
Your bladder is a hollow, muscular organ that stores urine. Bladder cancer is the uncontrolled growth of abnormal cells in the bladder.
Treatment often involves surgery. Depending on other factors, such as how far the cancer has spread, you may need additional treatments.
People who have had bladder cancer continue to have an increased risk of developing new or recurrent cancers in and around the bladder. That’s why continued, close monitoring is so important.
What is bladder cancer?
Bladder cancer is the uncontrolled growth of abnormal cells in the bladder.
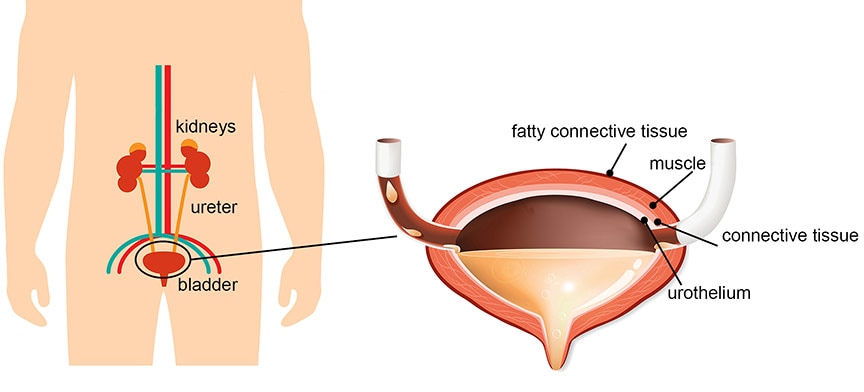
Your bladder is a hollow, balloon-shaped organ in the pelvis. Its job is to store urine before it leaves the body. Urine is made by the kidneys and transported to the bladder through tubes called ureters. When you urinate, the bladder muscles contract, forcing urine out of the bladder through a tube called the urethra.
The bladder wall is made up of four main layers:
- The innermost lining. This is called the urothelium or the transitional epithelium.
- A thin layer of connective tissue, blood vessels, and nerves.
- A thick layer of muscle.
- A layer of fatty connective tissue. This tissue separates the bladder from nearby organs.
Bladder cancer usually begins when cells in the innermost layer of the bladder start to grow uncontrollably. As more cancer cells develop, they can form a tumor, spread through additional layers of the bladder wall, and spread to other parts of the body.
Types of bladder cancer
Most bladder cancers begin in the innermost lining of the bladder.
They are called urothelial cancers, or transitional cell cancers (TCCs).
Invasive vs. non-invasive bladder cancer
Bladder cancers can be described by how far they have invaded into the wall of the bladder.
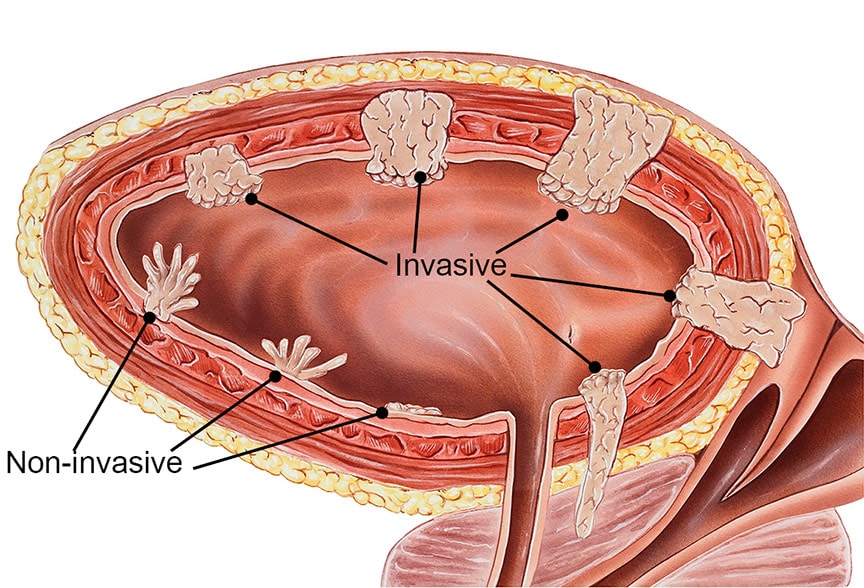
- Non-invasive (superficial) cancers are confined to the inner bladder lining. They have not grown into the deeper layers. Many bladder cancers are discovered before they have spread past the inner lining.
- Invasive cancers have grown through the lining of the bladder and invaded the muscle wall of the bladder. They may also have spread to nearby organs.
Other types of cancer can also start in the bladder. But they are much less common than urothelial cancer.
Symptoms
Many people with bladder cancer have no symptoms.
The diagnosis is often made when red blood cells are detected in a urine sample. People with bladder cancer may not see blood in their urine because there is often not enough blood to change the urine color. Rather, small amounts of blood are found when a urine test is done because of other symptoms or as part of a general medical check-up.
When symptoms of bladder cancer do occur, they include:
- pink, red, or rust-colored urine, caused by the presence of many red blood cells
- painful urination, or a burning sensation when urinating
- more frequent urination
- feeling as if you need to urinate right away, even when your bladder is not full
- trouble urinating, or a weak urine stream
Diagnosis
The main test when looking for bladder cancer is cystoscopy.
First, however, your doctor will review your medical history, symptoms, and risk factors, and will examine you.
Your doctor will order laboratory tests. These will include urine and blood tests. Your doctor may send the urine sample for cytology, a test that can detect cancer cells.
Cystoscopy
- If your doctor suspects bladder cancer, he or she will recommend a cystoscopy. During this procedure, the doctor inserts a cystoscope through your urethra, into your bladder.
- A cystoscope is a thin tube with a light and a lens or small video camera on the end. Your doctor looks for abnormal spots inside your bladder.
- If areas of the bladder lining appear abnormal, your doctor will take one or more biopsies through the cystoscope. This means your doctor will cut out small pieces of tissue to be examined under a microscope to look for cancer cells. If possible, your doctor will remove the entire abnormal area during cystoscopy.
- You may also need additional tests to determine if the cancer has spread.
Grading and staging bladder cancer
A cancer’s grade and stage describe the cancer’s aggressiveness and how far it has spread.
These are two of the most important factors your doctor will consider when deciding on your course of treatment.
Grade
The tumor grade is an estimate of how likely the cancer is to grow and spread rapidly. It is based on how your cancer cells look under a microscope.
Low-grade cancers look more like normal bladder tissue. They have a lower chance of spreading than high- grade and are rarely life-threatening. Low-grade tumors usually have a good prognosis, or outlook. However, they do tend to recur and need to be removed repeatedly.
High-grade bladder cancers contain very abnormal-looking cells. They are more likely to grow into the bladder wall, spread quickly, and become life-threatening.
Stage
A cancer’s stage describes whether and how far it has spread, which is another important factor in predicting a person’s prognosis. Treatment options vary depending on the stage.
There are several different staging systems used to describe how far a cancer has spread. The staging system most often used for bladder cancer is the American Joint Committee on Cancer (AJCC)TNM system. It is based on three key pieces of information:
T: Describes how far the primary tumor has grown into the bladder wall and whether it has grown into nearby tissues.
N: Indicates whether cancer has spread to lymph nodes near the bladder. Lymph nodes are small collections of immune system cells. Cancers often spread to lymph nodes first.
M: Indicates whether the cancer has spread (metastasized) to distant sites. This includes other organs or lymph nodes that are not near the bladder.
Numbers or other letters appear after T, N, and M when describing a person’s bladder cancer. They provide more details about each of these factors. Higher numbers mean the cancer is more advanced.
Treatment overview
You will need to consider several factors when weighing your treatment options.
These include the benefits, risks, and possible side effects of treatment. You should also understand the goal of each treatment option. Will it cure your cancer? Extend your life? Or simply relieve your symptoms?
Primary treatment options for bladder cancer are:
- surgery
- intravesical therapy
- chemotherapy
- radiation therapy
These treatments may be used alone or in combination. Surgery is almost always part of the treatment plan for bladder cancer.
Your doctor will consider the stage and grade of your cancer when selecting a treatment plan.
Other important considerations should include:
- your age and expected life span
- your treatment goals and priorities
- any other serious health conditions you have
- possible side effects
Surgical treatment of bladder cancer
Surgery is part of the treatment plan for most cases of bladder cancer.
The type of surgery you have will depend on how far your cancer has spread.
Transurethral resection (TURBT)
TURBT is a procedure that removes cancerous tissue or tumors from the bladder. During the procedure, a cystoscope is inserted into the bladder through the urethra. The doctor uses a wire loop at the end of the cystoscope to remove cancerous tissues or tumors. Your doctor may burn away any remaining cancer or destroy it using a high-energy laser.
Cystectomy
If bladder cancer is invasive, or if non-invasive tumors return repeatedly, all or part of the bladder may need to be removed. This operation is called a cystectomy.
The cancer is removed along with part of the bladder wall. This surgery may be done if the cancer has invaded the muscle layer but is small and confined to one place.
A radical cystectomy removes the entire bladder and nearby lymph nodes. This surgery will affect how you urinate, and it can have sexual side effects as well.
Other treatment options
Other treatments may be used alone, in combination, or together with surgery. They include intravesical therapy, chemotherapy, and radiation therapy.
Intravesical therapy
In intravesical therapy, medication is placed directly inside the bladder. This therapy is most effective when cancer is confined to the bladder’s innermost lining.
Immunotherapy drugs may be used for intravesical therapy. They cause the body’s own immune system to attack the cancer cells. Or, a doctor may place chemotherapy drugs directly into the bladder to kill cancer cells.
Systemic chemotherapy
Chemotherapy uses drugs to kill cancer cells. So-called systemic chemotherapy may be given by mouth or through a vein and can kill cancer cells throughout the body.
Systemic chemotherapy can be used:
- before surgery, to try to shrink a large tumor. This allows the tumor to be removed more easily and lowers the chance the cancer will come back
- after surgery or radiation therapy, to kill any remaining cancer cells
- in combination with radiation therapy, to help the radiation work better
- as the main treatment for advanced bladder cancers
Radiation therapy
Radiation therapy uses high-energy radiation to kill cancer cells. When used to treat bladder cancer, it is usually done with external beam radiation therapy, which works by focusing radiation from a source outside of the body onto the site of the cancer.
Radiation therapy can be used:
- after surgery that doesn’t remove the entire bladder
- as an alternative treatment for people who can’t have surgery
- in combination with chemotherapy
- as part of the initial treatment for advanced bladder cancer
- to help prevent or treat symptoms caused by advanced bladder cancer
All cancer treatments can cause unpleasant side effects. If you experience side effects talk to your doctor or health care team. They can help you find ways to ease your discomfort.
Reconstructive surgery after bladder removal
If your entire bladder is surgically removed, you will need another way to store and remove urine from your body.
Different types of reconstructive surgery can be done. For example:
- A piece of intestine is removed and used to make a passageway from the ureters to the front of the abdomen. Urine flows from the kidneys through the ureters and into the passageway. A small bag placed over an opening in the abdomen collects the urine.
- A piece of intestine is removed and used to make a pouch that is attached to the ureters. Urine is stored in the pouch, which must be emptied several times a day. There is no bag outside the body.
- The surgeon creates a new bladder from a piece of intestine. The new bladder is connected to the ureters and the urethra. The person can urinate normally.
Reducing the risk of recurrence
People who have had bladder cancer remain at risk for it coming back.
Bladder cancer can start to grow again at the site where it started. Or new bladder cancers can develop.
The following steps may help to reduce your risk of another bladder cancer.
Follow up with your doctor. Anyone who has had bladder cancer should be closely monitored for the rest of their life. Ask your doctor when and how often you need follow-up appointments and tests.
Don’t smoke. Smoking may cause up to half of all bladder cancers. It also increases the risk of many other cancers.
Drink plenty of water. Drinking lots of fluids, particularly water, might lower the risk of bladder cancer.
Live a healthy lifestyle. These steps may help reduce the risk of cancer, as well as the occurrence of other medical conditions:
- Achieve and maintain a healthy weight
- Be physically active
- Eat a healthy, plant-based diet
- Limit alcohol
Researchers are studying whether certain foods, vitamins, minerals, dietary supplements, medications, or vaccines can reduce the risk of bladder cancer coming back, or of developing a second bladder cancer.
You can reduce your risk of new or recurrent cancers with close monitoring by your primary care physician and oncologist. Keep all suggested follow-up appointments and report any changes in your health immediately.
Talk to your doctor
Here are some questions you can ask your doctor before, during, and after treatment.
Ask your doctor:
- What type of bladder cancer do I have?
- Is my cancer aggressive?
- Is my cancer just in the lining of the bladder? If not, how far has it spread?
- What are my treatment options?
- Which treatment do you recommend?
- How will we know if the treatment is working?
- Will the treatment cure my cancer?
- What are the chances that my cancer will come back?
- What can I do to help prevent my cancer from returning?
Tell your doctor...
- If you are experiencing side effects from your treatment
- Before you try any complementary or alternative therapies




