Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Suspension, Oral, as benzoate:
Katerzia: 1 mg/mL (150 mL) [contains polysorbate 80, sodium benzoate]
Tablet, Oral:
Norvasc: 10 mg
Generic: 10 mg
Tablet, Oral, as besylate:
Norvasc: 2.5 mg, 5 mg
Generic: 2.5 mg, 5 mg
Pharmacology
Mechanism of Action
Inhibits calcium ion from entering the “slow channels” or select voltage-sensitive areas of vascular smooth muscle and myocardium during depolarization, producing a relaxation of coronary vascular smooth muscle and coronary vasodilation; increases myocardial oxygen delivery in patients with vasospastic angina. Amlodipine directly acts on vascular smooth muscle to produce peripheral arterial vasodilation reducing peripheral vascular resistance and blood pressure.
Pharmacokinetics/Pharmacodynamics
Absorption
Well absorbed (Meredith 1992)
Distribution
Mean Vd:
Children >6 years: Similar to adults on a mg per kg basis; Note: Weight-adjusted Vd in younger children (<6 years of age) may be greater than in older children (Flynn 2006)
Adults: 21 L/kg (Scholz 1997)
Metabolism
Hepatic (~90%) to inactive metabolites
Excretion
Urine (10% of total dose as unchanged drug, 60% of total dose as metabolites)
Clearance: May be decreased in patients with hepatic insufficiency or moderate to severe heart failure; weight-adjusted clearance in children >6 years of age is similar to adults; Note: Weight-adjusted clearance in younger children (<6 years of age) may be greater than in older children (Flynn 2006)
Onset of Action
Antihypertensive effect: Significant reductions in blood pressure at 24 to 48 hours after first dose; slight increase in heart rate within 10 hours of administration may reflect some vasodilating activity (Donnelly 1993)
Time to Peak
Plasma: 6 to 12 hours
Duration of Action
Antihypertensive effect: At least 24 hours (Donnelly 1993); has been shown to extend to at least 72 hours when discontinued after 6 to 7 weeks of therapy (Biston 1999)
Half-Life Elimination
Terminal (biphasic): 30 to 50 hours; increased with hepatic dysfunction
Protein Binding
~93%
Use in Specific Populations
Special Populations: Hepatic Function Impairment
AUC may increase ~40% to 60%.
Special Populations: Elderly
AUC may increase ~40% to 60%.
Special Populations Note
Moderate to severe heart failure: AUC may increase ~40% to 60%.
Use: Labeled Indications
Angina: Treatment of symptomatic chronic stable angina; treatment of confirmed or suspected vasospastic angina (previously referred to as Prinzmetal or variant angina). May be used alone or in combination with other antianginal agents.
Hypertension: Management of hypertension in adults and children ≥6 years of age.
Use: Off Label
Raynaud phenomenonyes
Based on the European Society for Vascular Medicine guidelines for the diagnosis and management of Raynaud phenomenon, amlodipine is a reasonable alternative to nifedipine for the management of this condition.
Contraindications
Hypersensitivity to amlodipine or any component of the formulation.
Canadian labeling: Additional contraindications (not in US labeling): Hypersensitivity to other dihydropyridines; severe hypotension (systolic blood pressure <90 mm Hg); breastfeeding; hereditary fructose intolerance (oral solution); hyperglycerolemia or glycerol kinase deficiency (oral solution).
Dosage and Administration
Dosing: Adult
Angina:
Chronic stable angina (alternative agent):
Note: A beta-blocker is the preferred initial therapy; if there are ongoing symptoms on beta-blocker therapy, a long acting dihydropyridine calcium channel blocker (eg, amlodipine) may be added; amlodipine may also be used as an alternative therapy if there are contraindications or unacceptable adverse effects with beta-blockade (ACC/AHA [Fihn 2012]).
Oral: 5 to 10 mg once daily.
Vasospastic angina:
Note: May use alone or in combination with nitrates (ACC/AHA [Fihn 2012]).
Oral: 5 to 10 mg once daily.
Hypertension:
Note: For initial treatment in patients with blood pressure ≥20/10 mm Hg above goal, may be used in combination with another appropriate agent (eg, ACE inhibitor, ARB, or thiazide diuretic). For patients <20/10 mm Hg above goal, some experts recommend an initial trial of monotherapy; however, over time, many patients will require combination therapy (ACC/AHA [Whelton 2017]; Mann 2019).
Oral: Initial: 2.5 to 5 mg once daily; titrate every 1 to 2 weeks as needed based on patient response; maximum: 10 mg/day (ACC/AHA [Whelton 2018]; Jamerson 2008); antihypertensive effect attenuates with higher doses and adverse effects may become more prominent (Mann 2019).
Raynaud phenomenon (off-label use): Oral: 5 mg once daily; if needed, increase dose gradually based on patient response and tolerability, usually once every 4 weeks, but not more frequently than once every 7 to 10 days; monitor blood pressure closely with each dose increase; maximum dose: 20 mg/day (ESVM [Belch 2017]; Wigley 2018).
Dosing: Geriatric
Dosing should start at the lower end of dosing range and be titrated to response due to possible increased incidence of hepatic, renal, or cardiac impairment. Elderly patients also show decreased clearance of amlodipine.
Chronic stable angina (alternative agent); vasospastic angina: Oral: Initial: 5 mg once daily.
Hypertension: Oral: Initial: 2.5 mg once daily.
Dosing: Pediatric
Hypertension: Oral:
Children 1 to 5 years: Limited data available: Note: A population pharmacokinetic study found that children <6 years of age had weight-adjusted clearance and Vd of amlodipine that were significantly greater than children ≥6 years of age. This may suggest the need for higher mg/kg/day doses in younger children (<6 years of age); however, the study included only a small number of younger children (n=11) (Flynn 2006). One retrospective pediatric study (n=55) that included only eight patients 1-6 years of age used initial doses of 0.05-0.1 mg/kg/day; doses were titrated upwards as needed; mean required dose was significantly higher in patients 1-6 years of age (0.3 ± 0.16 mg/kg/day) compared to older children (6 to 12 years: 0.16 ± 0.12 mg/kg/day; 12 to 20 years: 0.14 ± 0.1 mg/kg/day) (Flynn 2000a).
Children and Adolescents 6 to 17 years: 2.5 to 5 mg once daily; doses >5 mg daily have not been fully studied. In a randomized, placebo-controlled trial of amlodipine in children (n=268; mean age: 12.1 years; range: 6 to 16 years), a significant reduction in systolic blood pressure (compared to placebo) was observed in both the 2.5 mg once daily and the 5 mg once daily amlodipine groups. The authors recommend an initial dose of 0.06 mg/kg/day with a maximum dose of 0.34 mg/kg/day (not to exceed 10 mg/day) (Flynn 2004).
Extemporaneously Prepared
A 1 mg/mL oral suspension may be made with tablets and either a 1:1 mixture of simple syrup and 1% methylcellulose or a 1:1 mixture of Ora-Plus® and Ora-Sweet®. Crush fifty 5 mg tablets in a mortar and reduce to a fine powder. Add small portions of the chosen vehicle and mix to a uniform paste; mix while adding the vehicle in incremental proportions to almost 250 mL; transfer to a calibrated bottle, rinse mortar with vehicle, and add quantity of vehicle sufficient to make 250 mL. Label “shake well” and “refrigerate”. Stable for 56 days at room temperature or 91 days refrigerated.
Nahata MC, Morosco RS, and Hipple TF, "Stability of Amlodipine Besylate in Two Liquid Dosage Forms," J Am Pharm Assoc (Wash) 1999, 39(3):375-7.10363465
Administration
Oral: Administer without regard to meals.
Storage
Suspension: Store at 2°C to 8°C (36°F to 46°F); avoid freezing and excessive heat. Protect from light.
Tablets: Store at 15°C to 30°C (59°F to 86°F).
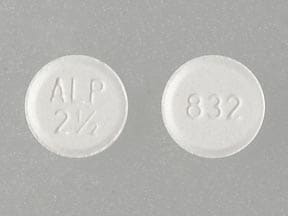
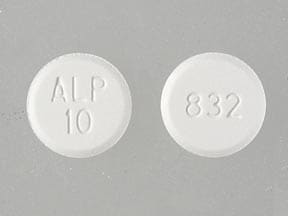
AmLODIPine Images
Drug Interactions
Alfuzosin: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Alpha1-Blockers: May enhance the hypotensive effect of Calcium Channel Blockers. Monitor therapy
Amifostine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Amifostine. Management: When amifostine is used at chemotherapy doses, blood pressure lowering medications should be withheld for 24 hours prior to amifostine administration. If blood pressure lowering therapy cannot be withheld, amifostine should not be administered. Consider therapy modification
Amphetamines: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Antifungal Agents (Azole Derivatives, Systemic): May enhance the adverse/toxic effect of Calcium Channel Blockers. Specifically, itraconazole may enhance the negative inotropic effects of verapamil or diltiazem. Antifungal Agents (Azole Derivatives, Systemic) may decrease the metabolism of Calcium Channel Blockers. Fluconazole and isavuconazonium likely exert weaker effects than other azoles and are addressed in separate monographs. Management: Concurrent use of felodipine or nisoldipine with itraconazole is specifically contraindicated. Frequent monitoring is warranted with any such combination; calcium channel blocker dose reductions may be required. Exceptions: Fluconazole; Isavuconazonium Sulfate. Consider therapy modification
Antihepaciviral Combination Products: May increase the serum concentration of AmLODIPine. Management: Reduce amlodipine dose by at least 50% and monitor for increased amlodipine effects (eg, hypotension) if an antihepaciviral combination product is initiated. Consider therapy modification
Antipsychotic Agents (Second Generation [Atypical]): Blood Pressure Lowering Agents may enhance the hypotensive effect of Antipsychotic Agents (Second Generation [Atypical]). Monitor therapy
Aprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
ARIPiprazole: CYP3A4 Inhibitors (Weak) may increase the serum concentration of ARIPiprazole. Management: Monitor for increased aripiprazole pharmacologic effects. Aripiprazole dose adjustments may or may not be required based on concomitant therapy and/or indication. Consult full interaction monograph for specific recommendations. Monitor therapy
Atosiban: Calcium Channel Blockers may enhance the adverse/toxic effect of Atosiban. Specifically, there may be an increased risk for pulmonary edema and/or dyspnea. Monitor therapy
Barbiturates: May increase the metabolism of Calcium Channel Blockers. Management: Monitor for decreased therapeutic effects of calcium channel blockers with concomitant barbiturate therapy. Calcium channel blocker dose adjustments may be necessary. Nimodipine Canadian labeling contraindicates concomitant use with phenobarbital. Monitor therapy
Barbiturates: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Benperidol: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Brigatinib: May diminish the antihypertensive effect of Antihypertensive Agents. Brigatinib may enhance the bradycardic effect of Antihypertensive Agents. Monitor therapy
Brimonidine (Topical): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Bromperidol: Blood Pressure Lowering Agents may enhance the hypotensive effect of Bromperidol. Bromperidol may diminish the hypotensive effect of Blood Pressure Lowering Agents. Avoid combination
Calcium Channel Blockers (Nondihydropyridine): Calcium Channel Blockers (Dihydropyridine) may enhance the hypotensive effect of Calcium Channel Blockers (Nondihydropyridine). Calcium Channel Blockers (Nondihydropyridine) may increase the serum concentration of Calcium Channel Blockers (Dihydropyridine). Monitor therapy
Calcium Salts: May diminish the therapeutic effect of Calcium Channel Blockers. Monitor therapy
CarBAMazepine: May increase the metabolism of Calcium Channel Blockers (Dihydropyridine). Management: Consider calcium channel blocker (CCB) dose adjustments or alternative therapy in patients receiving concomitant carbamazepine. Nimodipine Canadian labeling contraindicates concurrent use with carbamazepine. Consider therapy modification
Clofazimine: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Clopidogrel: Calcium Channel Blockers may diminish the therapeutic effect of Clopidogrel. Monitor therapy
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
CycloSPORINE (Systemic): Calcium Channel Blockers (Dihydropyridine) may increase the serum concentration of CycloSPORINE (Systemic). CycloSPORINE (Systemic) may increase the serum concentration of Calcium Channel Blockers (Dihydropyridine). Monitor therapy
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May increase the metabolism of CYP3A4 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
CYP3A4 Inhibitors (Moderate): May increase the serum concentration of AmLODIPine. Monitor therapy
CYP3A4 Inhibitors (Strong): May increase the serum concentration of AmLODIPine. Monitor therapy
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dapoxetine: May enhance the orthostatic hypotensive effect of Calcium Channel Blockers. Monitor therapy
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Dexmethylphenidate: May diminish the therapeutic effect of Antihypertensive Agents. Monitor therapy
Diazoxide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Dofetilide: CYP3A4 Inhibitors (Weak) may increase the serum concentration of Dofetilide. Monitor therapy
DULoxetine: Blood Pressure Lowering Agents may enhance the hypotensive effect of DULoxetine. Monitor therapy
Duvelisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Efavirenz: May decrease the serum concentration of Calcium Channel Blockers. Monitor therapy
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Flibanserin: CYP3A4 Inhibitors (Weak) may increase the serum concentration of Flibanserin. Monitor therapy
Fluconazole: May increase the serum concentration of Calcium Channel Blockers. Monitor therapy
Fosaprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosnetupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosphenytoin: Calcium Channel Blockers may increase the serum concentration of Fosphenytoin. Management: Monitor for phenytoin toxicity with concomitant use of a calcium channel blocker (CCB) or decreased phenytoin effects with CCB discontinuation. Monitor for decreased CCB therapeutic effects. Nimodipine Canadian labeling contraindicates use with phenytoin. Consider therapy modification
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Herbs (Hypertensive Properties): May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Herbs (Hypotensive Properties): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Hypotension-Associated Agents: Blood Pressure Lowering Agents may enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Larotrectinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Lemborexant: CYP3A4 Inhibitors (Weak) may increase the serum concentration of Lemborexant. Management: The maximum recommended dosage of lemborexant is 5 mg, no more than once per night, when coadministered with weak CYP3A4 inhibitors. Consider therapy modification
Levodopa-Containing Products: Blood Pressure Lowering Agents may enhance the hypotensive effect of Levodopa-Containing Products. Monitor therapy
Lomitapide: CYP3A4 Inhibitors (Weak) may increase the serum concentration of Lomitapide. Management: Patients on lomitapide 5 mg/day may continue that dose. Patients taking lomitapide 10 mg/day or more should decrease the lomitapide dose by half. The lomitapide dose may then be titrated up to a max adult dose of 30 mg/day. Consider therapy modification
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Lormetazepam: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Lovastatin: AmLODIPine may increase the serum concentration of Lovastatin. Monitor therapy
Macrolide Antibiotics: May decrease the metabolism of Calcium Channel Blockers. Management: Consider using a noninteracting macrolide. Felodipine Canadian labeling specifically recommends avoiding its use in combination with clarithromycin. Exceptions: Azithromycin (Systemic); Fidaxomicin; Roxithromycin; Spiramycin. Consider therapy modification
Magnesium Salts: Calcium Channel Blockers may enhance the adverse/toxic effect of Magnesium Salts. Magnesium Salts may enhance the hypotensive effect of Calcium Channel Blockers. Monitor therapy
Melatonin: May diminish the antihypertensive effect of Calcium Channel Blockers (Dihydropyridine). Monitor therapy
Methylphenidate: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
MiFEPRIStone: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Minimize doses of CYP3A4 substrates, and monitor for increased concentrations/toxicity, during and 2 weeks following treatment with mifepristone. Avoid cyclosporine, dihydroergotamine, ergotamine, fentanyl, pimozide, quinidine, sirolimus, and tacrolimus. Consider therapy modification
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Molsidomine: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Naftopidil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Netupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Neuromuscular-Blocking Agents (Nondepolarizing): Calcium Channel Blockers may enhance the neuromuscular-blocking effect of Neuromuscular-Blocking Agents (Nondepolarizing). Monitor therapy
Nicergoline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicorandil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
NiMODipine: CYP3A4 Inhibitors (Weak) may increase the serum concentration of NiMODipine. Monitor therapy
Nitroprusside: Blood Pressure Lowering Agents may enhance the hypotensive effect of Nitroprusside. Monitor therapy
Obinutuzumab: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Management: Consider temporarily withholding blood pressure lowering medications beginning 12 hours prior to obinutuzumab infusion and continuing until 1 hour after the end of the infusion. Consider therapy modification
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Pentoxifylline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Phenytoin: Calcium Channel Blockers may increase the serum concentration of Phenytoin. Phenytoin may decrease the serum concentration of Calcium Channel Blockers. Management: Avoid use of nimodipine or nifedipine with phenytoin. Monitor for phenytoin toxicity and/or decreased calcium channel blocker effects with any concurrent use. Consider therapy modification
Pholcodine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Pholcodine. Monitor therapy
Phosphodiesterase 5 Inhibitors: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Pimozide: CYP3A4 Inhibitors (Weak) may increase the serum concentration of Pimozide. Avoid combination
Prostacyclin Analogues: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Quinagolide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
QuiNIDine: Calcium Channel Blockers (Dihydropyridine) may decrease the serum concentration of QuiNIDine. Calcium Channel Blockers (Dihydropyridine) may increase the serum concentration of QuiNIDine. QuiNIDine may increase the serum concentration of Calcium Channel Blockers (Dihydropyridine). Monitor therapy
Rifamycin Derivatives: May decrease the serum concentration of Calcium Channel Blockers. This primarily affects oral forms of calcium channel blockers. Management: The labeling for some US and Canadian calcium channel blockers contraindicate use with rifampin, however recommendations vary. Consult appropriate labeling. Consider therapy modification
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Simvastatin: AmLODIPine may increase the serum concentration of Simvastatin. Management: Avoid the concurrent use of amlodipine with simvastatin when possible. If used together, avoid doses of simvastatin greater than 20 mg/day (for adults). Consider therapy modification
Sincalide: Drugs that Affect Gallbladder Function may diminish the therapeutic effect of Sincalide. Management: Consider discontinuing drugs that may affect gallbladder motility prior to the use of sincalide to stimulate gallbladder contraction. Consider therapy modification
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
Tacrolimus (Systemic): Calcium Channel Blockers (Dihydropyridine) may increase the serum concentration of Tacrolimus (Systemic). Monitor therapy
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Triazolam: CYP3A4 Inhibitors (Weak) may increase the serum concentration of Triazolam. Management: Consider triazolam dose reduction in patients receiving concomitant weak CYP3A4 inhibitors. Consider therapy modification
Ubrogepant: CYP3A4 Inhibitors (Weak) may increase the serum concentration of Ubrogepant. Management: In patients taking weak CYP3A4 inhibitors, the initial and second dose (if needed) of ubrogepant should be limited to 50 mg. Consider therapy modification
Yohimbine: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Test Interactions
May lead to false-negative aldosterone/renin ratio (ARR) (Funder 2016).
Adverse Reactions
>10%:
Cardiovascular: Peripheral edema (2% to 11% dose related; female 15%; male 6%; HF patients 27% to 28% [Packer 1996; Packer 2013])
Respiratory: Pulmonary edema (HF patients 7% to 15% [Packer 1996; Packer 2013])
1% to 10%:
Cardiovascular: Palpitations (≤5%, dose related), flushing (≤3%, dose related, more frequent in females)
Central nervous system: Fatigue (5%), dizziness (1% to 3%, dose related), male sexual disorder (≤2%), drowsiness (1%)
Dermatologic: Pruritus (≤2%), skin rash (≤2%)
Gastrointestinal: Nausea (3%), abdominal pain (2%)
Neuromuscular & skeletal: Muscle cramps (≤2%), weakness (≤2%)
Respiratory: Dyspnea (≤2%)
<1%, postmarketing, and/or case reports: Abnormal dreams, acute interstitial nephritis (Ejaz 2000), angioedema, anorexia, anxiety, arthralgia, atrial fibrillation, back pain, bradycardia, cardiac arrhythmia, chest pain, cholestasis, conjunctivitis, constipation, depersonalization, depression, diaphoresis, diarrhea, difficulty in micturition, diplopia, dysphagia, epistaxis, erythema multiforme, erythematous rash, exfoliative dermatitis, extrapyramidal reaction, eye pain, female sexual disorder, flatulence, gingival hyperplasia, gynecomastia, hepatitis, hot flash, hyperglycemia, hypersensitivity angiitis, hypersensitivity reaction, hypoesthesia, increased serum transaminases, increased thirst, insomnia, jaundice, leukopenia, maculopapular rash, malaise, myalgia, nervousness, nocturia, nonthrombocytopenic purpura, orthostatic hypotension, osteoarthritis, pain, pancreatitis, paresthesia, peripheral ischemia, peripheral neuropathy, phototoxicity, purpura, rigors, syncope, tachycardia, thrombocytopenia, tinnitus, tremor, urinary frequency, vasculitis, ventricular tachycardia, vertigo, visual disturbance, vomiting, weight gain, weight loss, xerostomia
Warnings/Precautions
Concerns related to adverse effects:
- Angina/MI: Increased angina and/or MI have occurred with initiation or dosage titration of dihydropyridine calcium channel blockers. Reflex tachycardia may occur resulting in angina and/or MI in patients with obstructive coronary disease, especially in the absence of concurrent beta-blockade.
- Hypotension: Symptomatic hypotension can occur; acute hypotension upon initiation is unlikely due to the gradual onset of action. Blood pressure must be lowered at a rate appropriate for the patient's clinical condition.
- Peripheral edema: The most common side effect is peripheral edema; occurs within 2 to 3 weeks of starting therapy.
Disease-related concerns:
- Aortic stenosis: Use amlodipine with extreme caution in patients with severe aortic stenosis; may reduce coronary perfusion resulting in ischemia.
- Heart failure: With the exception of amlodipine, calcium channel blockers should be avoided whenever possible in patients with heart failure with reduced ejection fraction (HFrEF). Amlodipine may be used for the treatment of hypertension or ischemic heart disease in patients with HFrEF, but has no effect on functional status or mortality (ACCF/AHA [Yancy 2013]).
- Hepatic impairment: Use with caution in patients with hepatic impairment; may require lower starting dose; titrate slowly in patients with severe hepatic impairment.
- Hypertrophic cardiomyopathy (HCM) with outflow tract obstruction: Use amlodipine with caution in patients with HCM and outflow tract obstruction since reduction in afterload may worsen symptoms associated with this condition (ACCF/AHA [Gersh 2011]).
Special populations:
- Elderly: Initiate at a lower dose in the elderly.
Other warnings/precautions:
- Titration: Peak antihypertensive effect is delayed; dosage titration should occur after 7 to 14 days on a given dose.
Monitoring Parameters
Heart rate, blood pressure
Hypertension: The 2017 Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults (ACC/AHA [Whelton 2017]):
Confirmed hypertension and known CVD or 10-year atherosclerotic cardiovascular disease (ASCVD) risk ≥10%: Target blood pressure <130/80 mm Hg is recommended.
Confirmed hypertension without markers of increased ASCVD risk: Target blood pressure <130/80 mm Hg may be reasonable.
Diabetes and hypertension: The American Diabetes Association (ADA) guidelines (ADA 2019):
Patients 18 to 65 years of age, without ASCVD, and 10-year ASCVD risk <15%: Target blood pressure <140/90 mm Hg is recommended.
Patients 18 to 65 years of age and known ASCVD or 10-year ASCVD risk >15%: Target blood pressure <130/80 mm Hg may be appropriate if it can be safely attained.
Patients >65 years of age (healthy or complex/intermediate health): Target blood pressure <140/90 mm Hg is recommended.
Patients >65 years of age (very complex/poor health): Target blood pressure <150/90 mm Hg is recommended.
Pregnancy
Pregnancy Considerations
Amlodipine crosses the placenta. Cord blood concentrations were ~40% of maternal serum at delivery, and concentrations in the newborn were below the limit of quantification (<0.1 ng/mL) when measured in eight infants within 48 hours of delivery (Morgan 2017; Morgan 2018).
Due to pregnancy-induced pharmacologic changes, amlodipine pharmacokinetics may be altered immediately postpartum (Morgan 2018; Naito 2015b).
Chronic maternal hypertension may increase the risk of birth defects, low birth weight, preterm delivery, stillbirth, and neonatal death. Actual fetal/neonatal risks may be related to duration and severity of maternal hypertension. Untreated hypertension may also increase the risks of adverse maternal outcomes, including gestational diabetes, myocardial infarction, preeclampsia, stroke, and delivery complications (ACOG 203 2019).
Calcium channel blockers may be used to treat hypertension in pregnant women; however, agents other than amlodipine are more commonly used (ACOG 203 2019; ESC [Regitz-Zagrosek 2018]). Females with preexisting hypertension may continue their medication during pregnancy unless contraindications exist (ESC [Regitz-Zagrosek 2018]).
Patient Education
What is this drug used for?
- It is used to treat high blood pressure.
- It is used to treat some types of chest pain (angina).
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Fatigue
- Loss of strength and energy
- Flushing
.• Nausea
- Abdominal pain
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Severe dizziness
- Passing out
- Chest pain
- Fast heartbeat
- Abnormal heartbeat
- Stiff muscles
- Tremors
- Abnormal movements
- Swelling of arms or legs
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.