Boxed Warning
Ischemic heart disease:
Following abrupt cessation of therapy with certain beta-blocking agents, exacerbations of angina pectoris and, in some cases, myocardial infarction (MI) have occurred. When discontinuing chronically administered metoprolol, particularly in patients with ischemic heart disease, gradually reduce the dosage over a period of 1 to 2 weeks and carefully monitor the patient. If angina markedly worsens or acute coronary insufficiency develops, reinstate metoprolol administration promptly, at least temporarily, and take other measures appropriate for the management of unstable angina. Warn patients against interruption or discontinuation of therapy without their health care provider's advice. Because coronary artery disease is common and may be unrecognized, it may be prudent not to discontinue metoprolol therapy abruptly, even in patients treated only for hypertension.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Capsule ER 24 Hour Sprinkle, Oral:
Kapspargo Sprinkle: 25 mg, 50 mg, 100 mg, 200 mg [contains corn starch]
Solution, Intravenous, as tartrate:
Generic: 5 mg/5 mL (5 mL)
Solution, Intravenous, as tartrate [preservative free]:
Generic: 5 mg/5 mL (5 mL)
Solution Cartridge, Intravenous, as tartrate:
Generic: 5 mg/5 mL (5 mL)
Tablet, Oral, as tartrate:
Lopressor: 50 mg [DSC]
Lopressor: 50 mg [scored]
Lopressor: 100 mg [scored; contains fd&c blue #2 aluminum lake]
Generic: 25 mg, 37.5 mg, 50 mg, 75 mg, 100 mg
Tablet Extended Release 24 Hour, Oral, as succinate:
Toprol XL: 25 mg
Toprol XL: 25 mg [DSC] [scored]
Toprol XL: 50 mg
Toprol XL: 50 mg [DSC] [scored]
Toprol XL: 100 mg
Toprol XL: 100 mg [DSC] [scored]
Toprol XL: 200 mg
Toprol XL: 200 mg [DSC] [scored]
Generic: 25 mg, 50 mg, 100 mg, 200 mg
Pharmacology
Mechanism of Action
Selective inhibitor of beta1-adrenergic receptors; competitively blocks beta1-receptors, with little or no effect on beta2-receptors at oral doses <100 mg (in adults); does not exhibit any membrane stabilizing or intrinsic sympathomimetic activity
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid and complete
Distribution
Vd: 3.2 to 5.6 L/kg; crosses the blood brain barrier; CSF concentrations are 78% of plasma concentrations
Metabolism
Extensively hepatic via CYP2D6; significant first-pass effect (~50%)
Excretion
Urine (95%, <5% to 10% as unchanged drug; increased to 30% to 40% in poor CYP2D6 metabolizers)
Onset of Action
Oral: Immediate release tablets: Within 1 hour; Peak effect: Oral: 1 to 2 hours (Regardh 1980); IV: 20 minutes (when infused over 10 minutes)
Duration of Action
Oral: Immediate release: Variable (dose-related; 50% reduction in maximum heart rate after single doses of 20, 50, and 100 mg occurred at 3.3, 5, and 6.4 hours, respectively), Extended release: ~24 hours
Half-Life Elimination
Neonates: 5 to 10 hours (Morselli 1989); Adults: 3 to 4 hours (7 to 9 hours in poor CYP2D6 metabolizers or hepatic impairment)
Protein Binding
~10% to 12% to albumin
Use in Specific Populations
Special Populations: Hepatic Function Impairment
Elimination half-life may be considerably prolonged, depending on severity.
Special Populations: Race
Poor CYP2D6 metabolizers (~8% Caucasians; ~2% other populations) have several-fold higher metoprolol plasma concentrations.
Use: Labeled Indications
Angina: Long-term treatment of angina pectoris.
Heart failure with reduced ejection fraction (HFrEF) (ER oral formulation): Treatment of stable, symptomatic (NYHA class II or III) heart failure of ischemic, hypertensive, or cardiomyopathic origin to reduce the rate of mortality plus hospitalization in patients already receiving ACE inhibitors, diuretics, and/or digoxin.
Hypertension: Management of hypertension. Note: Beta-blockers are not recommended as first-line therapy (ACC/AHA [Whelton 2017]).
Myocardial infarction: Treatment of hemodynamically stable acute myocardial infarction (MI) to reduce cardiovascular mortality (injection to be used in combination with metoprolol oral maintenance therapy).
Use: Off Label
Atrial fibrillation/flutteryes
Based on the 2014 American Heart Association/American College of Cardiology/Heart Rhythm Society (AHA/ACC/HRS) guideline for the management of patients with atrial fibrillation (AF), the use of beta-blockers, including metoprolol, for ventricular rate control in patients with paroxysmal, persistent, or permanent AF is effective and recommended.
Atrial fibrillation prevention after cardiac surgeryyes
Based on the American College of Cardiology Foundation/American Heart Association (ACCF/AHA) guideline for coronary artery bypass graft surgery, beta-blockers are recommended to help prevent postoperative atrial fibrillation.
Hypertrophic cardiomyopathyyes
Based on the American College of Cardiology Foundation/American Heart Association (ACCF/AHA) guideline for the diagnosis and treatment of hypertrophic cardiomyopathy, a beta blocker (eg, metoprolol) is an effective and recommended agent for the treatment of symptoms (eg, angina, dyspnea) in patients with obstructive or nonobstructive hypertrophic cardiomyopathy.
Marfan syndrome with aortic aneurysmyes
Based on the American College of Cardiology Foundation/American Heart Association/American Association for Thoracic Surgery (ACCF/AHA/AATS) guideline for the diagnosis and management of patients with thoracic aortic disease, a beta blocker (eg, metoprolol) is an effective and recommended agent to reduce the rate of aortic dilatation in patients with Marfan syndrome and aortic aneurysm, unless a contraindication exists.
Migraine prophylaxisbyes
Data from small, randomized, active-controlled trials support the use of metoprolol for prevention of migraines Diener 2001, Schellenberg 2008.
Based on evidence-based guidelines for pharmacologic treatment for episodic migraine prevention in adults from the American Academy of Neurology and the American Headache Society, metoprolol is effective for migraine prevention in adults.
Supraventricular tachycardia (eg, atrioventricular nodal reentrant tachycardia, atrioventricular reentrant tachycardia, focal atrial tachycardia)yes
Based on the American College of Cardiology/American Heart Association/Heart Rhythm Society (ACC/AHA/HRS) guidelines for the management of adult patients with supraventricular tachycardia, the use of an oral or intravenous beta-blocker, including metoprolol, is effective and recommended for a variety of symptomatic supraventricular tachycardias (atrioventricular nodal reentrant tachycardia [AVNRT], atrioventricular reentrant tachycardia [AVRT], focal atrial tachycardia [AT], and multifocal atrial tachycardia [MAT]). In patients without pre-excitation, intravenous metoprolol is recommended for acute treatment in hemodynamically stable patients and oral metoprolol is recommended for ongoing management of symptomatic supraventricular tachycardias in patients who are not candidates for, or prefer not to undergo, catheter ablation. Intravenous or oral metoprolol may be useful for rate control in the acute treatment or ongoing management of hemodynamically stable patients with atrial flutter.
Thyrotoxicosisyes
Based on the American Thyroid Association guidelines for diagnosis and management of hyperthyroidism and other causes of thyrotoxicosis, beta-blockers, including metoprolol, are effective and recommended in the treatment of symptomatic thyrotoxicosis. Beta-blockers should also be considered in asymptomatic patients who are at increased risk of complications due to worsening hyperthyroidism.
Ventricular arrhythmiasyes
Based on the American Heart Association/American College of Cardiology/Heart Rhythm Society (AHA/ACC/HRS) guideline for management of patients with ventricular arrhythmias and prevention of sudden cardiac death, beta-blockers are effective for control of ventricular arrhythmias and ventricular premature beats.
Contraindications
Hypersensitivity to metoprolol, any component of the formulation, or other beta-blockers; second- or third-degree heart block
Note: Additional contraindications are formulation and/or indication specific.
Immediate-release tablets/injectable formulation:
Hypertension and angina (oral only): Sinus bradycardia; cardiogenic shock; overt heart failure; sick sinus syndrome; severe peripheral arterial circulatory disorders
Myocardial infarction (oral and injection): Severe sinus bradycardia (heart rate <45 beats/minute); significant first-degree heart block (P-R interval ≥0.24 seconds); systolic blood pressure <100 mm Hg; moderate to severe cardiac failure
Extended-release formulation: Severe bradycardia, cardiogenic shock; decompensated heart failure; sick sinus syndrome (except in patients with a functioning artificial pacemaker)
Documentation of allergenic cross-reactivity for beta-blockers is limited. However, because of similarities in chemical structure and/or pharmacologic actions, the possibility of cross-sensitivity cannot be ruled out with certainty.
Canadian labeling: Additional contraindications (not in US labeling): Cor pulmonale; untreated pheochromocytoma; asthma and other obstructive respiratory disease (injection only); concomitant use with anesthesia agents that cause myocardial depression
Dosage and Administration
Dosing: Adult
Angina: Note: For vasospastic angina, beta-blockers are not recommended; calcium channel blockers and nitrates are preferred in this situation. For nonvasospastic angina, guidelines recommend titrating dose to a resting heart rate of 55 to 60 beats per minute (ACCF/AHA [Fihn 2012]), while other experts recommend target of 60 to 70 beats per minute (Kannam 2019).
Immediate release (metoprolol tartrate): Oral: Initial: 50 mg twice daily; may increase dose at weekly intervals to desired effect; usual dosage range: 50 to 200 mg twice daily; maximum dose: 400 mg/day
Extended release (metoprolol succinate): Oral: Initial: 100 mg once daily; may increase dose at weekly intervals to desired effect; maximum dose: 400 mg/day
Note: For microvascular angina, some experts start with 50 mg/day (divided twice daily for the immediate-release formulation or once daily for the extended-release formulation) and increase to 100 to 200 mg/day as needed to control symptoms (Chaudhary 2018).
Atrial fibrillation/flutter (off-label use):
Acute ventricular rate control: IV: 2.5 to 5 mg over 2 minutes; repeat dose every 5 minutes as needed; maximum total dose: 15 mg. Note: Initiate cautiously in patients with concomitant heart failure. Avoid in patients with decompensated heart failure; electrical cardioversion preferred (AHA/ACC/HRS [January 2014]; AHA [Neumar 2010]).
Maintenance of ventricular rate control:
Immediate release (metoprolol tartrate): Oral: 25 to 100 mg twice daily (AHA/ACC/HRS [January 2014]). Note: More frequent dosing is appropriate in the acute setting while titrating to a maintenance dose.
Extended release (metoprolol succinate): Oral: 50 to 400 mg once daily (AHA/ACC/HRS [January 2014])
Atrial fibrillation prevention after cardiac surgery: Note: Initiate prior to surgery (preferentially at least 48 hours before) or postoperatively when hemodynamically stable. Continue therapy at least until the first postoperative visit in patients with no other indication for beta-blocker therapy (Lee 2018).
Immediate release (metoprolol tartrate): Oral: Initial: 25 to 50 mg twice daily; titrate based on daily evaluation of hemodynamic response to the maximally tolerated dose; maximum dose: 200 mg/day (Acikel 2008; Haghjoo 2007)
Extended release (metoprolol succinate): Oral: Initial: 50 mg once daily; titrate based on daily evaluation of hemodynamic response to the maximally tolerated dose; maximum dose: 200 mg/day (Ozaydin 2013)
Heart failure with reduced ejection fraction (HFrEF): Note: Initiate only in stable patients. In hospitalized patients, volume status should be optimized and IV diuretics, vasodilators, and inotropic agents successfully discontinued. Use caution when initiating in patients with NYHA class IV symptoms or recent HF exacerbation (particularly in those who required inotropes during their hospital course) (ACCF/AHA [Yancy 2013]; Meyer 2019).
Extended release (metoprolol succinate): Oral: Initial: 12.5 to 25 mg once daily; up-titrate gradually (eg, doubling the dose every 2 or more weeks) to the maximum tolerated dose while monitoring for signs and symptoms of HF; maximum dose: 200 mg/day (ACCF/AHA [Yancy 2013]; ACC/AHA/HFSA [Yancy 2017]; MERIT-HF Study Group 1999)
Hypertension (alternative agent): Note: Not recommended in the absence of specific comorbidities (eg, ischemic heart disease, HFrEF, arrhythmia) (ACC/AHA [Whelton 2017]).
Immediate release (metoprolol tartrate): Oral: Initial: 50 mg twice daily; titrate at weekly (or longer) intervals as needed based on patient response; maximum dose: 400 mg/day; usual dosage range: 100 to 200 mg/day in 2 divided doses (ACC/AHA [Whelton 2017])
Extended release (metoprolol succinate): Oral: Initial: 25 to 100 mg once daily; titrate at weekly (or longer) intervals as needed based on patient response; maximum dose: 400 mg/day; usual dosage range: 50 to 200 mg once daily (ACC/AHA [Whelton 2017])
Migraine prophylaxis (off-label use): Immediate release (metoprolol tartrate): Oral: Initial: 25 mg twice daily; titrate slowly (eg, every 1 to 2 weeks) based on patient response and tolerability up to 200 mg/day in divided doses; maintain for at least 3 months before considering treatment failure (Bajwa 2018; Diener 2001; Pringsheim 2012; Schellenberg 2008).
Myocardial infarction, early treatment and secondary prevention: Note: An oral beta-blocker is recommended within the first 24 hours if there are no contraindications. Do not initiate metoprolol in patients with signs of heart failure, a low output state, increased risk of cardiogenic shock, or other contraindications for beta-blockade (eg, second- or third-degree heart block) (ACCF/AHA [O'Gara 2013]). Patients who did not receive a beta-blocker within 24 hours of myocardial infarction because of early contraindications should be subsequently reevaluated for secondary prevention. The optimal duration of therapy is unknown; some experts treat for a minimum of 3 years and use a longer duration for patients with high-risk features (eg, cardiogenic shock, heart failure, chronic kidney disease) at initial presentation (Rosenson 2018).
IV: Note: Small doses of IV metoprolol at the time of presentation may be considered for ST-elevation myocardial infarction (STEMI) patients with hypertension or ongoing ischemia if no contraindications exist. Initial: 5 mg; repeat dose every 5 minutes for up to 3 doses as needed based on heart rate and blood pressure; maximum total dose: 15 mg; begin oral therapy 15 to 30 minutes after the last IV dose (ACCF/AHA [O'Gara 2013]; Chen 2005; Rosenson 2018).
Oral:
Immediate release (metoprolol tartrate): Initial: 25 to 50 mg every 6 to 12 hours in the acute setting; some experts suggest a lower starting dose of 12.5 mg every 6 to 12 hours when concern for adverse effects remain; for outpatients, transition to twice-daily dosing of metoprolol tartrate (immediate release) or to daily metoprolol succinate (extended release); titrate dose based on heart rate and blood pressure as tolerated up to a maximum dose of 200 mg/day (ACCF/AHA [O'Gara 2013]; Rosenson 2018; Simons 2018).
Extended release (metoprolol succinate): Initial: 25 to 50 mg once daily is also recommended by some experts; titrate dose based on heart rate and blood pressure as tolerated up to 200 mg once daily (Rosenson 2018; Simons 2018).
Supraventricular tachycardia (eg, atrioventricular nodal reentrant tachycardia, atrioventricular reentrant tachycardia, focal atrial tachycardia) (off-label use):
Acute treatment: IV: 2.5 to 5 mg over 2 minutes; repeat dose every 5 minutes as needed; maximum total dose: 15 mg. Note: Initiate cautiously in patients with concomitant heart failure. Avoid in patients with decompensated heart failure; electrical cardioversion preferred (ACC/AHA/HRS [Page 2016]; AHA [Neumar 2010]).
Maintenance therapy:
Immediate release (metoprolol tartrate): Oral: Initial: 25 mg twice daily; maximum dose: 400 mg/day (ACC/AHA/HRS [Page 2016])
Extended release (metoprolol succinate): Oral: Initial: 50 mg once daily; maximum dose: 400 mg/day (ACC/AHA/HRS [Page 2016])
Thyrotoxicosis (off-label use): Immediate release (metoprolol tartrate): Oral: 25 to 50 mg every 8 to 12 hours; may also consider administering an equivalent dose of the once-daily extended-release formulation (metoprolol succinate) (Ross 2016).
Ventricular arrhythmias (off-label use):
Sustained ventricular tachycardia (VT), incessant VT, or electric storm (hemodynamically stable): Note: Beta-blockers are generally administered in addition to an antiarrhythmic drug (eg, amiodarone) for these indications. A beta-blocker is also used to reduce shocks in patients who receive an implantable cardioverter defibrillator for these indications (AHA/ACC/HRS [Al-Khatib 2017]); propranolol may be the preferred beta-blocker in these situations (Chatzidou 2018).
Acute ventricular tachycardia (eg, sustained VT):IV: 5 mg every 5 minutes up to 3 doses (AHA/ACC/HRS [Al-Khatib 2017])
Prevention of ventricular arrhythmias:
Immediate release (metoprolol tartrate): Oral: Initial: 12.5 to 25 mg twice daily; increase as needed based on patient response; maximum dose: 200 mg/day in 2 or 3 divided doses (Kettering 2002; Kuck 2000; Seidl 1998)
Extended release (metoprolol succinate): Oral: 25 to 100 mg 1 to 2 times daily (AHA/ACC/HRS [Al-Khatib 2017])
Nonsustained VT or ventricular premature beats, symptomatic: Note: Unless there are other indications for a beta-blocker (eg, prior MI or heart failure), use the lowest dose that alleviates symptoms.
Immediate release (metoprolol tartrate): Oral: 50 to 200 mg/day in 2 or 3 divided doses (Zimetbaum 2018)
Extended release (metoprolol succinate): Oral: 25 to 100 mg 1 to 2 times daily (AHA/ACC/HRS [Al-Khatib 2017])
Switching dosage forms:
Switching from immediate release (metoprolol tartrate) to extended release (metoprolol succinate): The same total daily dose of metoprolol should be used. Metoprolol tartrate is typically administered in 2 to 3 divided daily doses and metoprolol succinate is administered once daily.
Switching between oral and intravenous dosage forms: In most cases, equivalent beta-blocking effect is achieved when a 2.5:1 (Oral:IV) ratio is used. However, in one bioavailability study of healthy volunteers (N=5), the range of Oral:IV conversion ratios was approximately 2:1 to 5:1 (Regrdh 1974). Therefore, patient variability may exist and a specific ratio may not apply to all patients, especially if comorbid conditions are present. The estimated equivalent IV total daily dose should be divided into 4 equal doses. For example, if a patient is receiving a chronic oral dose of metoprolol tartrate 25 mg twice daily (total daily dose of 50 mg), this could translate to a range of 2.5 mg IV every 6 hours (based on a 5:1 ratio) to 5 mg IV every 6 hours (based on a 2.5:1 ratio). Recognizing that patients receiving larger chronic oral doses should not automatically be converted to a large IV dose, consideration should be given to further reducing the initial IV dose and basing subsequent doses on the clinical response (Huckleberry 2003).
Dosing: Geriatric
Refer to adult dosing. In the management of hypertension, consider lower initial doses and titrate to response (Aronow 2011).
Dosing: Pediatric
Note: Dose should be individualized based on patient response.
Heart failure (dilated cardiomyopathy): Limited data available: Children and Adolescents: Oral: Immediate release (metoprolol tartrate): Initial: 0.1 to 0.2 mg/kg/dose twice daily, may increase slowly (usually every 2 weeks) as needed up to 1 mg/kg/day; maximum daily dose: 2 mg/kg/day or 200 mg/day, whichever is less (Kliegman 2011; Park 2014; Shaddy 1999). Dosing based on a multicenter, open-label trial in 15 pediatric patients (age range: 2.5 to 15 years, mean: 8.6 ± 1.3 years) with dilated cardiomyopathy with heart failure that failed to show improvement in left ventricular function on conventional therapy; after 23 months of metoprolol, significant increases in ejection fraction (mean: 41.1%) and fractional shortening (mean: 23.3%) were observed; the reported mean maximum daily dose was 1.1 ± 0.1 mg/kg/day (range: 0.5 to 2.3 mg/kg/day) (Shaddy 1999).
Hypertension: Note: Guidelines do not recommend beta-blockers as initial therapy in pediatric patients; beta-blockers should be reserved for use in patients who have contraindications to preferred agents or after ≥2 preferred agents have failed in patients with hypertension and chronic kidney disease, proteinuria, or diabetes mellitus (AAP [Flynn 2017]).
Immediate-release tablets (metoprolol tartrate): Children and Adolescents ≤17 years: Oral: Initial: 0.5 to 1 mg/kg/dose (maximum initial dose: 25 mg/dose) twice daily; adjust dose based on patient response; maximum daily dose: 6 mg/kg/day or 200 mg/day, whichever is less (NHBPEP [Falkner 2004]; NHLBI [Kavey 2011])
Extended-release sprinkle capsules or tablets (metoprolol succinate): Children ≥6 years and Adolescents: Oral: Initial: 1 mg/kg/dose once daily (maximum initial dose: 50 mg/dose); adjust dose based on patient response; maximum daily dose: 2 mg/kg/day or 200 mg/day, whichever is less; higher doses have not been studied.
Syncope, vagal: Limited data available: Children ≥7 years and Adolescents:
Tilt-table test: IV: 0.1 to 0.2 mg/kg; maximum dose: 10 mg/dose (Muller 1993, O'Marcaigh 1994)
Chronic treatment: Oral: Immediate release (metoprolol tartrate): 0.5 to 1 mg/kg/dose two times daily; maximum daily dose: 6 mg/kg/day (Kliegman 2011; Muller 1993; O'Marcaigh 1994). Dosing based on two studies: In one study, oral metoprolol was initiated at doses of 0.8 to 2.8 mg/kg/day in 15 patients (8 to 20 years of age) after showing response to tilt-table testing. During follow up, a total of 6 patients discontinued therapy due to recurrent syncope or adverse events including irritability/moodiness, severe depression, and severe nausea (dose ranged in this group from 1.6 to 2.8 mg/kg/day) (Muller 1993); in another study, oral doses of 1 to 2 mg/kg/day, rounded to the nearest 25 mg/day and divided into 2 doses daily were used in 19 patients (7 to 18 years of age) with unexplained syncope; the mean effective dose was 1.5 mg/kg/day (O'Marcaigh 1994).
Extemporaneously Prepared
10 mg/mL Oral Suspension (ASHP Standard Concentration) (ASHP 2017)
A 10 mg/mL oral suspension may be made with metoprolol tartrate tablets and one of three different vehicles (cherry syrup; a 1:1 mixture of Ora-Sweet and Ora-Plus; or a 1:1 mixture of Ora-Sweet SF and Ora-Plus). Crush twelve 100 mg tablets in a mortar and reduce to a fine powder. Add 20 mL of the chosen vehicle and mix to a uniform paste; mix while adding the vehicle in incremental proportions to almost 120 mL; transfer to a calibrated bottle, rinse mortar with vehicle, and add quantity of vehicle sufficient to make 120 mL. Label "shake well" and "protect from light". Stable for 60 days.
Allen LV Jr and Erickson MA 3rd, "Stability of Labetalol Hydrochloride, Metoprolol Tartrate, Verapamil Hydrochloride, and Spironolactone With Hydrochlorothiazide in Extemporaneously Compounded Oral Liquids," Am J Health Syst Pharm, 1996, 53(19):2304-9.8893069
Administration
Oral:
Immediate release (metoprolol tartrate): Administer with or immediately following meals.
Extended release (metoprolol succinate): According to the manufacturer, it is preferable to administer with or immediately following meals; however, may also administer without regard to meals (Tangeman 2003; van den Berg 1990; Wikstrand 2003). May divide tablets in half; do not crush or chew.
Sprinkle capsule: May be swallowed whole or the capsule may be opened and contents sprinkled on a small amount (1 teaspoonful) of soft food (eg, applesauce, pudding, or yogurt) to be used within 60 minutes (do not store for future use).
Nasogastric tube administration: Open capsule and add contents to an all plastic oral tip syringe; add 15 mL of water. Gently shake the syringe for ~10 seconds. Immediately deliver mixture through a ≥12 French nasogastric tube. No granules should remain in the syringe; rinse syringe with additional water if necessary.
IV: May administer undiluted by rapid infusion (IV push) over 1 minute for acute treatment. May also be administered by slow infusion (ie, 5 to 10 mg of metoprolol in 50 mL of fluid) over ~30 to 60 minutes during less urgent situations (eg, substitution for oral metoprolol).
Storage
Injection: Store at 20°C to 25°C (68°F to 77°F). Do not freeze; protect from light.
Sprinkle capsules: Store at 20°C to 25°C (68°F to 77°F).
Tablet: Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Protect from moisture.
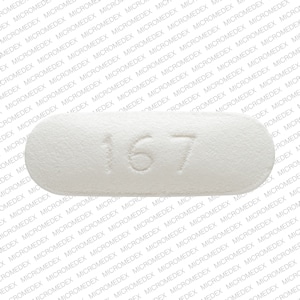
Metoprolol Images
Drug Interactions
Abiraterone Acetate: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Management: Avoid concurrent use of abiraterone with CYP2D6 substrates that have a narrow therapeutic index whenever possible. When concurrent use is not avoidable, monitor patients closely for signs/symptoms of toxicity. Consider therapy modification
Acetylcholinesterase Inhibitors: May enhance the bradycardic effect of Beta-Blockers. Monitor therapy
Ajmaline: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Alfuzosin: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Alpha1-Blockers: Beta-Blockers may enhance the orthostatic hypotensive effect of Alpha1-Blockers. The risk associated with ophthalmic products is probably less than systemic products. Monitor therapy
Alpha2-Agonists: May enhance the AV-blocking effect of Beta-Blockers. Sinus node dysfunction may also be enhanced. Beta-Blockers may enhance the rebound hypertensive effect of Alpha2-Agonists. This effect can occur when the Alpha2-Agonist is abruptly withdrawn. Management: Closely monitor heart rate during treatment with a beta blocker and clonidine. Withdraw beta blockers several days before clonidine withdrawal when possible, and monitor blood pressure closely. Recommendations for other alpha2-agonists are unavailable. Exceptions: Apraclonidine. Consider therapy modification
Amifostine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Amifostine. Management: When amifostine is used at chemotherapy doses, blood pressure lowering medications should be withheld for 24 hours prior to amifostine administration. If blood pressure lowering therapy cannot be withheld, amifostine should not be administered. Consider therapy modification
Aminoquinolines (Antimalarial): May decrease the metabolism of Beta-Blockers. Monitor therapy
Amiodarone: May enhance the bradycardic effect of Beta-Blockers. Possibly to the point of cardiac arrest. Amiodarone may increase the serum concentration of Beta-Blockers. Monitor therapy
Amphetamines: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Antipsychotic Agents (Phenothiazines): May enhance the hypotensive effect of Beta-Blockers. Beta-Blockers may decrease the metabolism of Antipsychotic Agents (Phenothiazines). Antipsychotic Agents (Phenothiazines) may decrease the metabolism of Beta-Blockers. Monitor therapy
Antipsychotic Agents (Second Generation [Atypical]): Blood Pressure Lowering Agents may enhance the hypotensive effect of Antipsychotic Agents (Second Generation [Atypical]). Monitor therapy
Asunaprevir: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Consider therapy modification
Barbiturates: May decrease the serum concentration of Beta-Blockers. Monitor therapy
Barbiturates: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Benperidol: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Beta2-Agonists: Beta-Blockers (Beta1 Selective) may diminish the bronchodilatory effect of Beta2-Agonists. Of particular concern with nonselective beta-blockers or higher doses of the beta1 selective beta-blockers. Monitor therapy
Bradycardia-Causing Agents: May enhance the bradycardic effect of other Bradycardia-Causing Agents. Monitor therapy
Brigatinib: May diminish the antihypertensive effect of Antihypertensive Agents. Brigatinib may enhance the bradycardic effect of Antihypertensive Agents. Monitor therapy
Brimonidine (Topical): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Bromperidol: Blood Pressure Lowering Agents may enhance the hypotensive effect of Bromperidol. Bromperidol may diminish the hypotensive effect of Blood Pressure Lowering Agents. Avoid combination
Bupivacaine: Beta-Blockers may increase the serum concentration of Bupivacaine. Monitor therapy
Calcium Channel Blockers (Nondihydropyridine): May enhance the hypotensive effect of Beta-Blockers. Bradycardia and signs of heart failure have also been reported. Calcium Channel Blockers (Nondihydropyridine) may increase the serum concentration of Beta-Blockers. Exceptions: Bepridil. Monitor therapy
Cardiac Glycosides: Beta-Blockers may enhance the bradycardic effect of Cardiac Glycosides. Monitor therapy
Ceritinib: Bradycardia-Causing Agents may enhance the bradycardic effect of Ceritinib. Management: If this combination cannot be avoided, monitor patients for evidence of symptomatic bradycardia, and closely monitor blood pressure and heart rate during therapy. Exceptions are discussed in separate monographs. Consider therapy modification
Cholinergic Agonists: Beta-Blockers may enhance the adverse/toxic effect of Cholinergic Agonists. Of particular concern are the potential for cardiac conduction abnormalities and bronchoconstriction. Monitor therapy
CloBAZam: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Cobicistat: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
CYP2D6 Inhibitors (Moderate): May increase the serum concentration of Metoprolol. Monitor therapy
CYP2D6 Inhibitors (Strong): May increase the serum concentration of Metoprolol. Monitor therapy
Dacomitinib: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Management: Avoid concurrent use of dacomitinib with CYP2D6 subtrates that have a narrow therapeutic index. Consider therapy modification
Darunavir: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Dexmethylphenidate: May diminish the therapeutic effect of Antihypertensive Agents. Monitor therapy
Diazoxide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Dipyridamole: May enhance the bradycardic effect of Beta-Blockers. Monitor therapy
Disopyramide: May enhance the bradycardic effect of Beta-Blockers. Beta-Blockers may enhance the negative inotropic effect of Disopyramide. Monitor therapy
Dronedarone: May enhance the bradycardic effect of Beta-Blockers. Dronedarone may increase the serum concentration of Beta-Blockers. This likely applies only to those agents that are metabolized by CYP2D6. Management: Use lower initial beta-blocker doses; adequate tolerance of the combination, based on ECG findings, should be confirmed prior to any increase in beta-blocker dose. Consider therapy modification
DULoxetine: Blood Pressure Lowering Agents may enhance the hypotensive effect of DULoxetine. Monitor therapy
EPINEPHrine (Nasal): Beta-Blockers (Beta1 Selective) may diminish the therapeutic effect of EPINEPHrine (Nasal). Monitor therapy
EPINEPHrine (Oral Inhalation): Beta-Blockers (Beta1 Selective) may diminish the therapeutic effect of EPINEPHrine (Oral Inhalation). Monitor therapy
Epinephrine (Racemic): Beta-Blockers (Beta1 Selective) may diminish the therapeutic effect of Epinephrine (Racemic). Monitor therapy
EPINEPHrine (Systemic): Beta-Blockers (Beta1 Selective) may diminish the therapeutic effect of EPINEPHrine (Systemic). Monitor therapy
Ergot Derivatives: Beta-Blockers may enhance the vasoconstricting effect of Ergot Derivatives. Exceptions: Nicergoline. Consider therapy modification
Fexinidazole [INT]: Bradycardia-Causing Agents may enhance the arrhythmogenic effect of Fexinidazole [INT]. Avoid combination
Fingolimod: Beta-Blockers may enhance the bradycardic effect of Fingolimod. Management: Avoid the concomitant use of fingolimod and beta-blockers if possible. If coadministration is necessary, patients should have overnight continuous ECG monitoring conducted after the first dose of fingolimod. Monitor patients for bradycardia. Consider therapy modification
Floctafenine: May enhance the adverse/toxic effect of Beta-Blockers. Avoid combination
Grass Pollen Allergen Extract (5 Grass Extract): Beta-Blockers may enhance the adverse/toxic effect of Grass Pollen Allergen Extract (5 Grass Extract). More specifically, Beta-Blockers may inhibit the ability to effectively treat severe allergic reactions to Grass Pollen Allergen Extract (5 Grass Extract) with epinephrine. Some other effects of epinephrine may be unaffected or even enhanced (e.g., vasoconstriction) during treatment with Beta-Blockers. Consider therapy modification
Herbs (Hypertensive Properties): May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Herbs (Hypotensive Properties): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Hypotension-Associated Agents: Blood Pressure Lowering Agents may enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Imatinib: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Insulins: Beta-Blockers may enhance the hypoglycemic effect of Insulins. Monitor therapy
Ivabradine: Bradycardia-Causing Agents may enhance the bradycardic effect of Ivabradine. Monitor therapy
Lacosamide: Bradycardia-Causing Agents may enhance the AV-blocking effect of Lacosamide. Monitor therapy
Lercanidipine: May enhance the hypotensive effect of Metoprolol. Metoprolol may decrease the serum concentration of Lercanidipine. Monitor therapy
Levodopa-Containing Products: Blood Pressure Lowering Agents may enhance the hypotensive effect of Levodopa-Containing Products. Monitor therapy
Lidocaine (Systemic): Beta-Blockers may increase the serum concentration of Lidocaine (Systemic). Monitor therapy
Lidocaine (Topical): Beta-Blockers may increase the serum concentration of Lidocaine (Topical). Monitor therapy
Lormetazepam: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Lumefantrine: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Mepivacaine: Beta-Blockers may increase the serum concentration of Mepivacaine. Monitor therapy
Methacholine: Beta-Blockers may enhance the adverse/toxic effect of Methacholine. Monitor therapy
Methoxyflurane: May enhance the hypotensive effect of Beta-Blockers. Monitor therapy
Methylphenidate: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Midodrine: May enhance the bradycardic effect of Bradycardia-Causing Agents. Monitor therapy
Mirabegron: May diminish the antihypertensive effect of Metoprolol. Mirabegron may increase the serum concentration of Metoprolol. Monitor therapy
Molsidomine: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Naftopidil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicergoline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicorandil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
NIFEdipine: May enhance the hypotensive effect of Beta-Blockers. NIFEdipine may enhance the negative inotropic effect of Beta-Blockers. Monitor therapy
Nitroprusside: Blood Pressure Lowering Agents may enhance the hypotensive effect of Nitroprusside. Monitor therapy
Nonsteroidal Anti-Inflammatory Agents: May diminish the antihypertensive effect of Beta-Blockers. Monitor therapy
Obinutuzumab: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Management: Consider temporarily withholding blood pressure lowering medications beginning 12 hours prior to obinutuzumab infusion and continuing until 1 hour after the end of the infusion. Consider therapy modification
Opioids (Anilidopiperidine): May enhance the bradycardic effect of Beta-Blockers. Opioids (Anilidopiperidine) may enhance the hypotensive effect of Beta-Blockers. Monitor therapy
Panobinostat: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Peginterferon Alfa-2b: May decrease the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Peginterferon Alfa-2b may increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Pentoxifylline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Perhexiline: CYP2D6 Substrates (High risk with Inhibitors) may increase the serum concentration of Perhexiline. Perhexiline may increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Pholcodine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Pholcodine. Monitor therapy
Phosphodiesterase 5 Inhibitors: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Propafenone: May increase the serum concentration of Beta-Blockers. Propafenone possesses some independent beta blocking activity. Monitor therapy
Prostacyclin Analogues: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Quinagolide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
QuiNINE: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Regorafenib: May enhance the bradycardic effect of Beta-Blockers. Monitor therapy
Reserpine: May enhance the hypotensive effect of Beta-Blockers. Monitor therapy
Rifamycin Derivatives: May decrease the serum concentration of Beta-Blockers. Exceptions: Rifabutin. Monitor therapy
Rivastigmine: May enhance the bradycardic effect of Beta-Blockers. Avoid combination
Ruxolitinib: May enhance the bradycardic effect of Bradycardia-Causing Agents. Management: Ruxolitinib Canadian product labeling recommends avoiding use with bradycardia-causing agents to the extent possible. Monitor therapy
Selective Serotonin Reuptake Inhibitors: May increase the serum concentration of Beta-Blockers. Exceptions: Citalopram; Escitalopram; FluvoxaMINE. Monitor therapy
Siponimod: Bradycardia-Causing Agents may enhance the bradycardic effect of Siponimod. Management: Avoid coadministration of siponimod with drugs that may cause bradycardia. Consider therapy modification
Sulfonylureas: Beta-Blockers may enhance the hypoglycemic effect of Sulfonylureas. Cardioselective beta-blockers (eg, acebutolol, atenolol, metoprolol, and penbutolol) may be safer than nonselective beta-blockers. All beta-blockers appear to mask tachycardia as an initial symptom of hypoglycemia. Ophthalmic beta-blockers are probably associated with lower risk than systemic agents. Monitor therapy
Terlipressin: May enhance the bradycardic effect of Bradycardia-Causing Agents. Monitor therapy
Theophylline Derivatives: Beta-Blockers (Beta1 Selective) may diminish the bronchodilatory effect of Theophylline Derivatives. Management: Monitor for reduced theophylline efficacy during concomitant use with any beta-blocker. Beta-1 selective agents are less likely to antagonize theophylline than nonselective agents, but selectivity may be lost at higher doses. Monitor therapy
Tofacitinib: May enhance the bradycardic effect of Bradycardia-Causing Agents. Monitor therapy
Yohimbine: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Adverse Reactions
Frequency not always defined.
Cardiovascular: Hypotension (1% to 27%), bradycardia (2% to 16%), first degree atrioventricular block (5%), arterial insufficiency (usually Raynaud type: 1%), cardiac failure (1%), cerebrovascular accident (1%), cold extremities (1%), palpitations (1%), peripheral edema (1%), claudication
Central nervous system: Dizziness (2% to 10%), fatigue (1% to 10%), depression (>2% to 5%), vertigo (≤2%), confusion, disturbed sleep, hallucination, headache, insomnia, nightmares, temporary amnesia
Dermatology: Pruritus (5%), skin rash (>2% to 5%), exacerbation of psoriasis, skin photosensitivity
Endocrine & metabolic: Decreased libido, unstable diabetes
Gastrointestinal: Diarrhea (>2% to 5%), constipation (1%), flatulence (1%), heartburn (1%), stomach pain (1%), xerostomia (1%), nausea (≤1%), vomiting
Neuromuscular & skeletal: Musculoskeletal pain
Ophthalmic: Blurred vision, visual disturbance
Otic: Tinnitus
Respiratory: Dyspnea (≤3%), bronchospasm (1%), wheezing (1%), rhinitis
Miscellaneous: Accidental injury (1%)
<1%, postmarketing and/or case reports: Abdominal pain, agranulocytosis, alopecia (reversible), anxiety, arthralgia, arthritis, chest pain, decreased HDL cholesterol, diaphoresis, drowsiness, dry eye syndrome, gangrene of skin or other tissue, hepatic insufficiency, hepatitis, impotence, increased lactate dehydrogenase, increased serum alkaline phosphatase, increased serum transaminases, increased serum triglycerides, jaundice, nervousness, paresthesia, Peyronie's disease, retroperitoneal fibrosis, syncope, taste disorder, weight gain
Warnings/Precautions
Concerns related to adverse events:
- Anaphylactic reactions: Use caution with history of severe anaphylaxis to allergens; patients taking beta-blockers may become more sensitive to repeated allergen challenges. Treatment of anaphylaxis (eg, epinephrine) in patients taking beta-blockers may be ineffective or promote undesirable effects.
- Atrioventricular (AV) block: Metoprolol commonly produces mild first-degree heart block. Metoprolol may also produce severe first-, second-, or third-degree heart block. Patients with acute myocardial infarction (especially right ventricular myocardial infarction) have a high risk of developing heart block of varying degrees. If severe heart block occurs, metoprolol should be discontinued and measures to increase heart rate should be employed.
- Bradycardia: Bradycardia, including sinus pause, heart block, and cardiac arrest, may occur. Patients with first-degree AV block, sinus node dysfunction, or conduction disorders may be at increased risk. Monitor heart rate and rhythm; if severe bradycardia occurs, reduce dose or discontinue therapy.
- CNS depression: May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks that require mental alertness (eg, operating machinery, driving).
- Hypotension: Symptomatic hypotension may occur with use.
Disease-related concerns:
- Bronchospastic disease: In general, patients with bronchospastic disease should not receive beta-blockers; however, metoprolol, with B1 selectivity, has been used cautiously with close monitoring.
- Conduction abnormality: Consider preexisting conditions such as sick sinus syndrome before initiating.
- Diabetes: Use with caution in patients with diabetes mellitus; may potentiate hypoglycemia and/or mask signs and symptoms.
- Heart failure: Use with caution in patients with compensated heart failure; monitor for a worsening of heart failure (only the ER formulation is indicated for use in heart failure). May need to increase diuretics and wait until clinically stable to advance dose to target.
- Hepatic impairment: Use with caution in patients with hepatic impairment.
- Myasthenia gravis: Use beta-blockers with caution in patients with myasthenia gravis.
- Peripheral vascular disease (PVD) and Raynaud disease: May precipitate or aggravate symptoms of arterial insufficiency in patients with PVD and Raynaud disease. Use with caution and monitor for progression of arterial obstruction.
- Pheochromocytoma (untreated): Adequate alpha-blockade is required prior to use of any beta-blocker.
- Prinzmetal variant angina: Beta-blockers without alpha1-adrenergic receptor blocking activity should be avoided in patients with Prinzmetal variant angina because unopposed alpha1-adrenergic receptors mediate coronary vasoconstriction and can worsen anginal symptoms (Mayer 1998).
- Psoriasis: Beta-blocker use has been associated with induction or exacerbation of psoriasis, but cause and effect have not been firmly established.
- Supraventricular tachycardia (SVT): If antidromic atrioventricular reentrant tachycardia (AVRT) or pre-excited atrial fibrillation is suspected, avoid AV node-specific blocking drugs (eg, adenosine, diltiazem, verapamil, digoxin, beta-blockers). For these types of SVT enhanced antegrade conduction from atria to ventricles may occur through an accessory pathway leading to ventricular arrhythmias if the AV node is blocked. It is safe to use AV node-specific blocking drugs for orthodromic AVRT because antegrade conduction occurs through the AV node and only retrograde conduction (from ventricles to atria) occurs through the accessory pathway.
- Thyroid disease: May mask signs of hyperthyroidism (eg, tachycardia). If hyperthyroidism is suspected, carefully manage and monitor; abrupt withdrawal may exacerbate symptoms of hyperthyroidism or precipitate thyroid storm. Alterations in thyroid function tests may be observed.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Dosage form specific issues:
- Switching dosage forms: The conversion ratio for immediate release (metoprolol tartrate) and extended release (metoprolol succinate) is 1:1, therefore the same total daily dose of metoprolol should be used when switching formulations. However, metoprolol tartrate is typically administered in 2 to 3 divided daily doses and metoprolol succinate is administered once daily.
Special populations:
- Elderly: Bradycardia may be observed more frequently in elderly patients (>65 years of age); dosage reductions may be necessary.
Other warnings/precautions:
- Abrupt withdrawal: [US Boxed Warning]: Beta-blocker therapy should not be withdrawn abruptly (particularly in patients with CAD), but gradually tapered over 1 to 2 weeks to avoid acute tachycardia, hypertension, and/or ischemia. Severe exacerbation of angina, ventricular arrhythmias, and myocardial infarction (MI) have been reported following abrupt withdrawal of beta-blocker therapy. Temporary but prompt resumption of beta-blocker therapy may be indicated with worsening of angina or acute coronary insufficiency.
- Major surgery: Chronic beta-blocker therapy should not be routinely withdrawn prior to major surgery.
Monitoring Parameters
Acute cardiac treatment: Monitor ECG, heart rate, and blood pressure with IV administration; heart rate, rhythm, and blood pressure with oral administration.
IV use in a nonemergency situation: Necessary monitoring for surgical patients who are unable to take oral beta-blockers (because of prolonged ileus) has not been defined. Some institutions require monitoring of baseline and postinfusion heart rate and blood pressure when a patient's response to beta-blockade has not been characterized (ie, the patient's initial dose or following a change in dose). Consult individual institutional policies and procedures.
Hypertension: The 2017 Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults (ACC/AHA [Whelton 2017]):
Confirmed hypertension and known CVD or 10-year ASCVD risk ≥10%: Target blood pressure <130/80 mm Hg is recommended.
Confirmed hypertension without markers of increased ASCVD risk: Target blood pressure <130/80 mm Hg may be reasonable.
Pregnancy
Pregnancy Considerations
Metoprolol and the metabolite alpha-hydroxymetoprolol cross the placenta (Lindeberg 1987; Ryu 2016).
Exposure to beta-blockers during pregnancy may increase the risk for adverse events in the neonate. If maternal use of a beta-blocker is needed, fetal growth should be monitored during pregnancy and the newborn should be monitored for 48 hours after delivery for bradycardia, hypoglycemia, and respiratory depression (ESC [Regitz-Zagrosek 2018]).
Chronic maternal hypertension is also associated with adverse events in the fetus/infant. Chronic maternal hypertension may increase the risk of birth defects, low birth weight, premature delivery, stillbirth, and neonatal death. Actual fetal/neonatal risks may be related to duration and severity of maternal hypertension. Untreated chronic hypertension may also increase the risks of adverse maternal outcomes, including gestational diabetes, preeclampsia, delivery complications, stroke, and myocardial infarction (ACOG 203 2019).
The pharmacokinetics of metoprolol may be changed during pregnancy; the degree of changes may be dependent upon maternal CYP2D6 genotype (Ryu 2016).
When treatment of hypertension in pregnancy is indicated, beta-blockers may be used. Specific recommendations vary by guideline but use of metoprolol may be considered (ACOG 203 2019; ESC [Regitz-Zagrosek 2018]; Magee 2014). Females with preexisting hypertension may continue their medication during pregnancy unless contraindications exist (ESC [Regitz-Zagrosek 2018]). Metoprolol may be used for the treatment of maternal ventricular arrhythmias, atrial fibrillation/atrial flutter, or supraventricular tachycardia during pregnancy; consult current guidelines for specific recommendations (ACC/AHA/HRS [Page 2016]; ESC [Regitz-Zagrosek 2018]). Use of metoprolol may be considered if migraine prophylaxis is needed in a pregnant woman (Pringsheim 2012).
Patient Education
What is this drug used for?
- It is used to treat high blood pressure.
- It is used to treat chest pain or pressure.
- It is used to treat heart failure (weak heart).
- It is used after a heart attack to help prevent future heart attacks and lengthen life.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Diarrhea
- Fatigue
- Loss of strength and energy
- Nausea
- Vomiting
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Depression
- Severe dizziness
- Passing out
- Chest pain
- Abnormal heartbeat
- Slow heartbeat
- Shortness of breath
- Excessive weight gain
- Swelling of arms or legs
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.