No woman wants to learn that she has breast cancer. But women who do receive this diagnosis can take some comfort in the advances that have been made over the past several decades.
Advanced tests can now reveal crucial details about a woman’s cancer that can help customize treatment. Treatments have fewer side effects. And today, your priorities and preferences are an important part of the conversation.
What is breast cancer?
Breast cancer is the uncontrolled growth of abnormal cells in the breast.
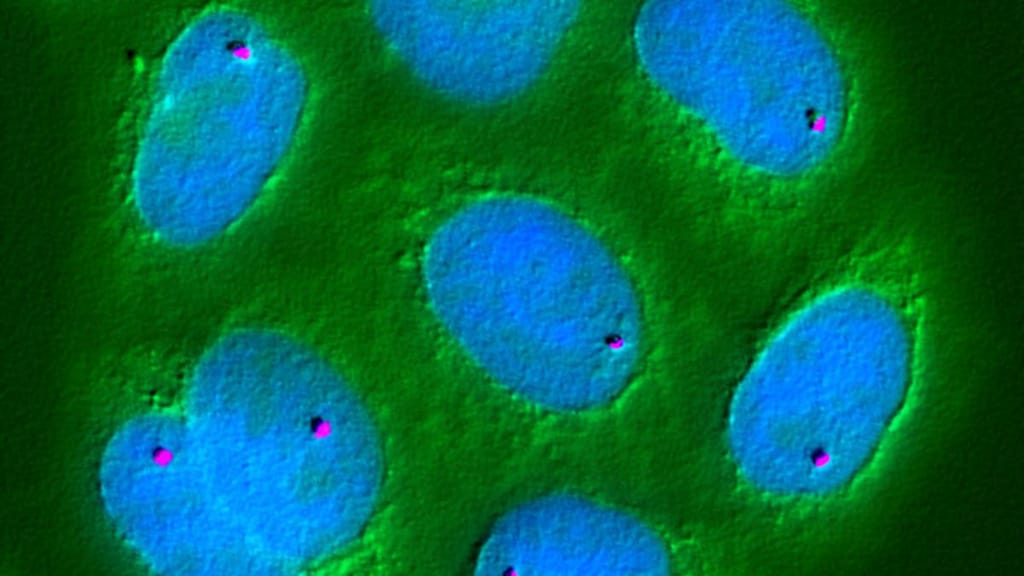
Cancer cells multiply faster then normal cells and don't die like normal cells. As more and more cancer cells build up, a lump forms. This is the primary tumor. Most tumors in the breast are carcinomas.
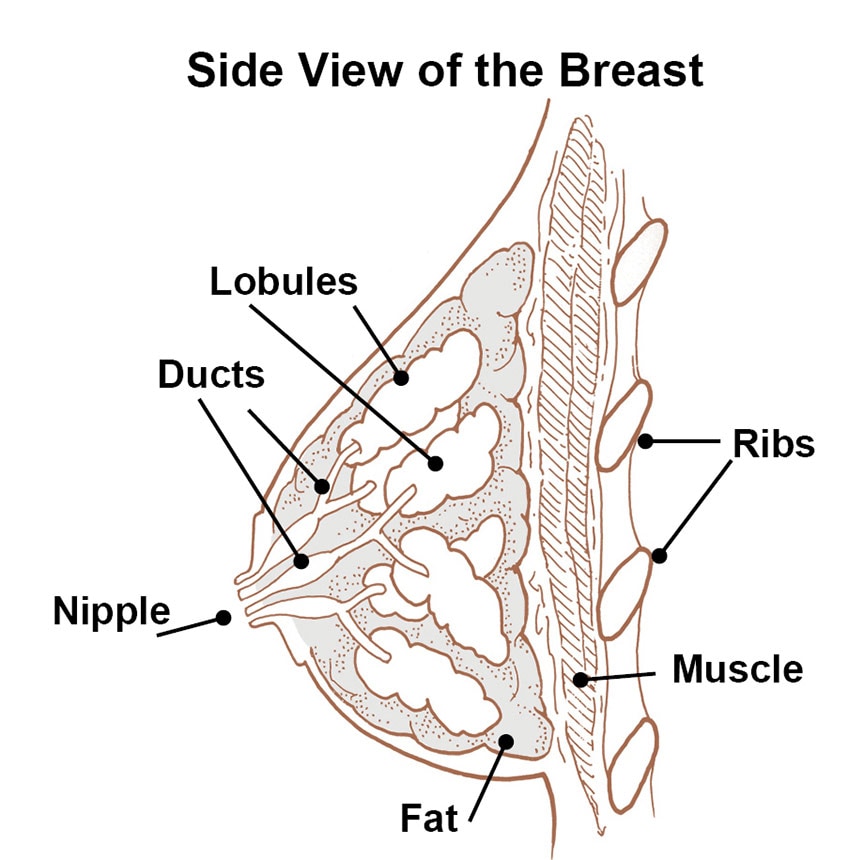
Most breast cancers start in the ducts. These are tiny tubes that carry milk from the lobules, where milk is made, to the nipple. Cancer can also start in the lobules or in non-glandular tissue.
Carcinomas can be invasive or noninvasive. Noninvasive breast cancers remain contained in one spot.
A noninvasive cancer in a milk duct is called ductal carcinoma in situ. One that arises in a milk lobule is known as lobular carcinoma in situ. Women with noninvasive breast cancer have an excellent prognosis.
Biopsy and surgery
Almost all women with breast cancer have surgery as their primary treatment.
After a biopsy, most women with breast cancer will need surgery. Sometimes the amount of breast tissue removed during a biopsy is sufficient, so that further surgery is not necessary. However, most often, women undergo either lumpectomy or mastectomy.
Lumpectomy:
Surgery to take out the tumor and a surrounding area of normal breast tissue. This is also known as breast-conserving surgery.
Mastectomy:
This surgery removes the entire breast.
Factors involved in choosing the right type of surgery for you include:
- the cancer’s stage and the characteristics of the cancer cells
- your age
- your overall health
- your priorities and preferences
- genetic testing, if performed
Checking lymph nodes
Surgery often requires removing nearby lymph nodes.
In many instances, women have nearby lymph nodes removed during lumpectomy or mastectomy to check them for cancer cells. When breast cancer does spread, the usual place is the lymph nodes under the arm. The first nodes that cancer cells reach are called sentinel nodes.
In a sentinel node biopsy, a surgeon removes a few of these nodes to check for cancer cells. While you are still in the operating room, the nodes are sent to the laboratory for examination under a microscope. If the sentinel nodes have cancer cells, your surgeon removes more nodes.
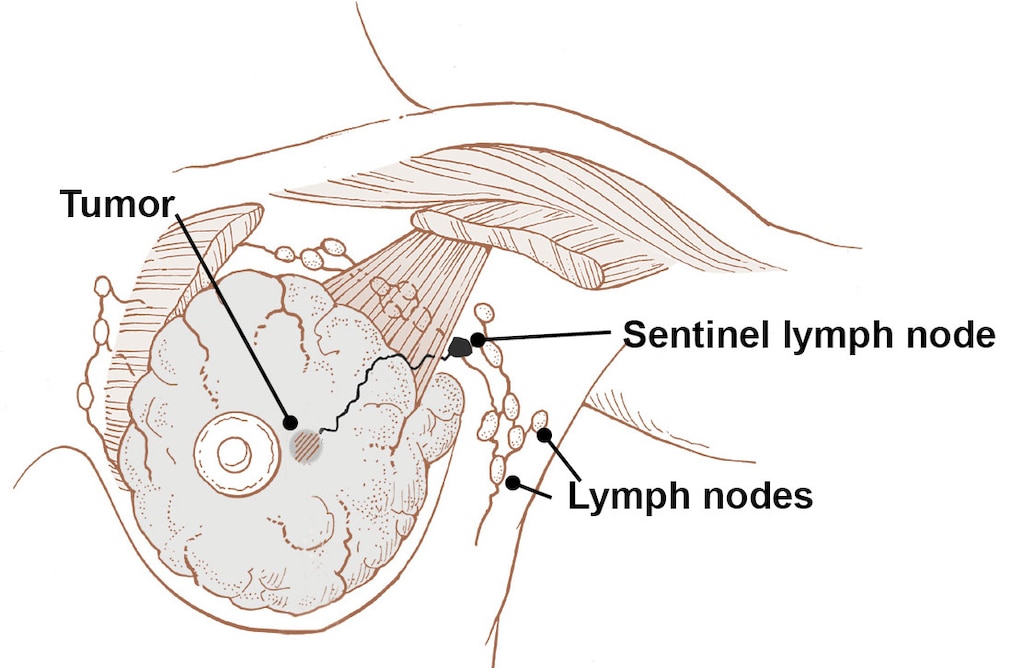
Cancer in the lymph nodes affects the treatment plan.
Tumor cell characteristics
Breast cancer cells have features that help guide treatment and prognosis.
A doctor called a pathologist examines the tumor under a microscope. He or she gives the tumor a grade, between 1 and 3, which describes how invasive the tumor is.
Grade 1 Tumors grow slowly and are least likely to spread.
Grade 3 Tumors grow quickly and are most likely to spread.
Pathologists also test cancer cells for:
- estrogen and progesterone hormone receptors
- the receptor protein known as HER2
- gene activity that provides clues about whether the cancer will spread or recur
Staging
The stage of the cancer also helps guide treatment and prognosis.
Staging usually happens after surgery and additional imaging tests. Your doctor will stage your breast cancer with a number between zero (0) and four (IV). In general, a lower stage number means less complicated treatment and a greater chance of cure.
The stage number is based on the following factors:
- the size of the primary breast tumor
- whether the cancer is invasive or noninvasive
- whether breast cancer cells have spread to any lymph nodes, and how many are involved
- whether the cancer has spread and formed tumors (metastases) in other organs, such as the liver or lungs
Hormone therapy
The number of hormone receptors on breast cancer cells determines whether hormone therapy will work. Receptors are like a cell’s antennae. They pick up signals from hormones, telling the cells to grow. If the cancer cells in your biopsy have many receptors for estrogen, they are estrogen-positive (ER+). Progesterone-positive (PR+) cells have many receptors for progesterone.
Hormone therapy will likely work for you if your breast cancer is either ER+ or PR+. This treatment “turns off” receptors. As a result, cancer cells don’t respond to hormones. The result is that the cancer grows more slowly or stops growing.
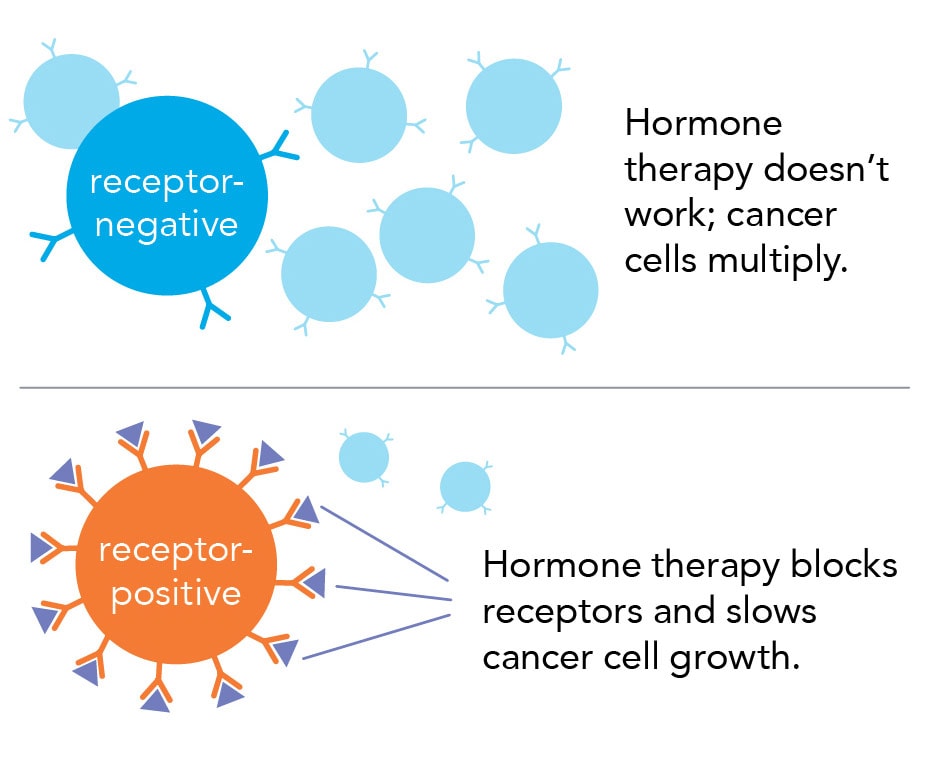
Women with hormone-receptor-positive breast cancer tend to have a better prognosis.
Radiation therapy
Radiation therapy uses high-energy rays to destroy cancer cells. Many women with invasive breast cancer receive radiation therapy. Usually it happens after surgery, but your doctor may also suggest it beforehand. Women almost always get radiation therapy after a lumpectomy. The goal is to kill any cancer cells left in or around the breast. It reduces the chance of cancer returning in the same breast.
Radiation may also be part of your treatment plan if you have a mastectomy or if cancer has spread to other parts of your body.
A type of radiation therapy called external beam radiation therapy (EBRT) is used most often to treat breast cancer. EBRT machines aim radiation at the outside of your body. The radiation goes through your skin to the tumor. Most women get EBRT 5 days a week for 5 to 7 weeks. It is done as outpatient treatment, so you don’t have to stay in the hospital.
If you’ve had surgery, you’ll need 3 to 4 weeks to heal before you start radiation therapy.
Radiation side effects
Radiation technology has greatly improved in the last few decades.
Your team can pinpoint exactly where you need radiation and the most effective dose to use. These advances mean that as little skin as possible is exposed to radiation, and at the lowest effective dose.
Still, you may have some side effects. The most common ones include:
- a feeling of heaviness in the breast, or swelling that may take 6 to 12 months to completely go away
- skin irritation in the area getting radiation, including burning, redness, sensitivity, and dryness
- mild fatigue, which usually improves 1 to 2 months after treatment ends
Ask your team which of these side effects you’re most likely to have, when they’ll appear, and what you can do to ease them.
Chemotherapy
Chemotherapy uses a combination of drugs to kill cancer cells.
Many different chemotherapy drugs are available to treat breast cancer. The specific drugs you need will depend on your particular cancer.
Chemotherapy may be used:
- Before surgery, to shrink a large tumor. This may allow for breast-conserving surgery instead of a mastectomy.
- After surgery, to kill any cancer cells that have escaped from the primary tumor. This approach also helps keep cancer from recurring.
- To treat cancer that has already spread beyond your breast. In this case, chemotherapy may be your primary treatment instead of surgery.
- To kill breast cancers that are not ER+, PR+, or HER2+.
Chemotherapy treatment cycles
Most often, you get chemotherapy drugs intravenously (through a vein). You will get this treatment in a hospital, but as an outpatient. You will receive the chemotherapy for several days or weeks in a row. Then you’ll have a rest period of several days or weeks. The time between the first day of one chemotherapy treatment and the first day of the next treatment is called a cycle. The length of chemotherapy treatment varies.
Side effects of chemotherapy
The duration of your treatment cycles, the drugs you take, and their dosages also affect which side effects you’ll most likely have and their severity.
Common side effects include:
- loss of appetite
- bruising or bleeding easily
- fatigue
- hair loss
- more frequent infections
- lack of menstrual periods
- nausea and vomiting
Ask your doctor what you can do to minimize these side effects.
Targeted therapy
Targeted therapy is a treatment choice for women with cancer that is HER2-positive (HER2+). These are women whose cancer cells contain more HER2 proteins than normal.
Cancer cells with many HER2 proteins are more likely to grow more quickly. HER2+ breast cancer is also more likely to spread to other parts of the body. The good news, though, is that being HER2+ means targeted therapy can help. Targeted therapy uses her2 inhibitors to hunt down and kill cells with too much HER2.
Targeted therapy works differently to thanchemotherapy, but it’s common to get both types of drugs. You may even get them on the same day.
Your breast’s shape after surgery
You may want to have reconstructive plastic surgery to restore your breast’s shape after surgery.
After mastectomy
The new breast may be made with:
- Implants—these are breast-shaped bags filled with saline or silicone
- Flaps—these are formed from tissue from your belly, buttocks, or shoulder
- Implants and flaps together
Your nipple is usually recreated from tissue on your breast, but less commonly it may be recreated using tissue from you vulva or thigh. The tissue that becomes you nipple may be darkened with a tattoo to look more natural.
Discuss your choices and any potential risks early in the treatment process. You may be able to have reconstruction done during your mastectomy. Or you may decide to have it later.
After lumpectomy
If you’re having a lumpectomy, your surgeon may be able to shift breast tissue around to replace the lost volume and shape. If you’re not satisfied with the results, you can talk with a plastic surgeon about breast revision surgery.
Lifestyle changes to prevent recurrence
Here are some things you can do to help prevent cancer from coming back.
Follow a healthy lifestyle:
- maintain a healthy weight
- eat a diet loaded with fruits and vegetables
- exercise regularly
- avoid alcohol—but if you do drink, limit yourself to no more than one drink per day; taking a folic acid supplement may also help offset the alcohol risk
- don’t smoke
If your cancer cells are positive for hormone receptors, talk to your doctor about hormone therapy. Women who take it for five or more years reduce their chances of recurrence.
A diagnosis of breast cancer is never good, but advances in testing and treatments are the best yet. With fewer side effects and more choices, your priorities and preferences can now be considered when making recommendations for your treatment.
Talk with your doctor
Depending on your personal situation, here are some questions to consider:
Initial questions
- Do I definitely have breast cancer?
- Which kind of breast cancer do i have? Is it just in one spot, or has it spread?
- What tests do I need? What will they tell us?
Considering treatment options
- Will I need surgery? What are the choices? Which is the right option for me?
- Will I need hormone therapy, chemotherapy, or radiation therapy?
- Should I expect side effects? If yes, how can I best manage them?
At follow-up visits, ask:
- Is the treatment working as expected?
- Are any changes to my original treatment plan needed?