
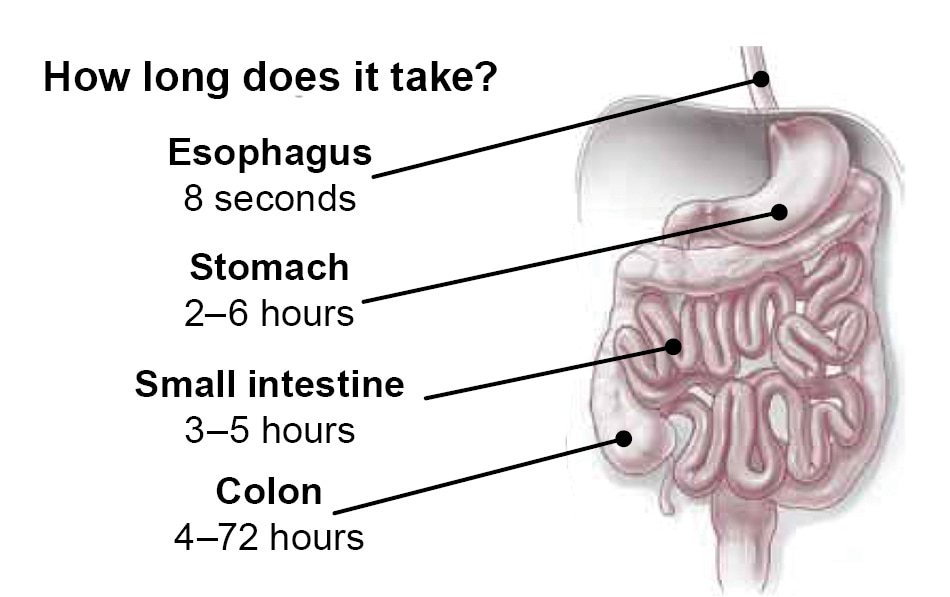
Most people have a fairly regular pattern of bowel movements.
When bowel movements occur less often than usual or when stool becomes hard, dry, and difficult to pass, that can be a sign of constipation. Often diet and lifestyle contribute to constipation. And while certain health problems also may lead to constipation, sometimes there is no clear cause. Fortunately, there are many things you can do to ease this common and uncomfortable problem and get your digestive system back on track.
What is constipation?
People mean different things when they talk about “constipation.”
Bowel habits vary greatly even among perfectly healthy people. “Normal” bowel movements can range from three times a day to three times a week.
Constipation means having fewer than three bowel movements a week, or often having trouble such as pain or straining when trying to pass stool.
When you can’t go to the bathroom for days on end, you feel bloated and miserable. Straining day after day can also lead to more serious problems, like hemorrhoids or even bulging (prolapse) of rectal tissue.
In most healthy adults, constipation improves gradually within a few weeks with increased fiber and fluids and regular exercise.
Symptoms of constipation
Constipation has a range of symptoms.
These include:
- fewer than three bowel movements per week
- straining hard to push out a bowel movement
- often needing to use enemas, laxatives, or suppositories
- small, hard, dry stools that are difficult or painful to pass
- feeling that your rectum is not empty after a bowel movement
It is usually a temporary annoyance and not a serious health problem. Tests usually aren’t needed. But severe constipation or constipation that lasts longer than three months (chronic constipation) can negatively affect the quality of a person’s life. In those cases, additional testing may be needed. Even then, no obvious cause may be found.
Occasionally, long-term constipation causes fecal impaction. That’s when the large intestine is blocked by a mass of stool that can’t be moved by normal intestinal movement. Fecal impaction can cause pain and vomiting and may require emergency treatment or hospitalization.
Common causes of constipation
Constipation is often related to diet or lifestyle.
- Lack of fiber: Fiber softens the stool and encourages proper bowel function. Many people don’t eat enough fiber.
- Lack of fluids: Getting enough fluids can help keep stools from becoming hard, dry, and difficult to pass. Aim for six to eight 8-ounce glasses of water each day. The liquids in fruits, soups, coffee, tea, stews, and solid foods count.
- Medication and supplements: Constipation is a side effect of many prescription and over-the-counter medications.
- Certain foods: Some people find foods such as dairy products or bananas constipating.
- Lack of exercise: Regular exercise promotes normal muscle contractions in the bowel wall and can help prevent constipation.
- Changes in routine: Travel, changes in your diet, and limited access to the bathroom can set off constipation.
- Ignoring the urge to go: Repeatedly putting off using the bathroom when you have the urge can lead to constipation.
Constipation due to health problems
An underlying health problem can trigger or contribute to constipation. For example:
- Underactive thyroid (hypothyroidism). When the thyroid gland doesn't produce enough thyroid hormone, metabolism slows. Constipation is a common symptom.
- Nerve or intestinal muscle disorders. Faulty nerve signals to the intestine or abnormal muscle activity in the intestine can slow the movement of stool. Diabetes and multiple sclerosis are examples of such disorders.
- Abdominal surgery. After an operation, the intestines are usually much less active than normal. This effect may last several days or more.
- Irritable bowel syndrome. This condition is marked by alternating periods of constipation and diarrhea, and abdominal cramping, pain, or bloating.
- General anesthesia and prolonged bed rest. These can also cause constipation.
If you have constipation along with any one of the following symptoms, call your doctor right away: blood in your stool, weight loss, worsening abdominal pain, severe abdominal swelling, fever, or weakness. These may be signs of a potentially serious problem such as an intestinal blockage, inflammatory bowel disease, or colon cancer.
Treatments
Fend off constipation with diet
Getting enough fiber and fluids can help.
Fiber is the non-digestible part of plant-based foods. There are two kinds, and you need them both.
- Soluble fiber from foods such as legumes, oats, and apples dissolves into a gel-like substance that helps the bowels hold on to water, bulking up the stool.
- Insoluble fiber from foods such as whole grains and most vegetables does not dissolve as it moves through your digestive tract. This increases stool bulk and helps move it along.
If your diet has been low in fiber, and then you start adding fiber, it can make you feel bloated and gassy. To avoid this, start slowly. Try eating five more grams of fiber each week until you reach your goal. Be sure to drink plenty of fluids as well.
| Recommended Daily Fiber Intake | |
|---|---|
| Men younger than 50 | 38 grams |
| Women younger than 50 | 25 grams |
| Men older than 50 | 30 grams |
| Women older than 50 | 21 grams |
| Source: Food and Nutrition Board, Institute of Medicine | |
Adding fiber to your diet
Start by eating more fruits, vegetables, and whole grains.
These easy tips can help:
- Toss some berries on your breakfast cereal.
- Include vegetables in each meal. Sauté with a little olive oil, steam, grill, or enjoy them raw.
- Snack on baby carrots and celery sticks dipped in hummus, or an apple with peanut butter.
- Cook with beans. Add them to your soups and pasta dishes, or try them on a salad.
- Choose whole-grain breads (100% whole wheat) and whole-wheat pasta, and brown rice.
Read labels carefully.
Good sources of fiber contain 5 grams or more per serving. Keep in mind that the amount of fiber listed is based on the serving size, not the entire package.
Laxatives
Using laxatives wisely can help when diet and lifestyle changes don't.
Some laxatives work by drawing water into the stool to soften it and make it easier to pass. Others stimulate bowel contractions.
Talk with your doctor about which laxative is safest for you, and how long you should use it. Always use laxatives exactly as directed.
These laxatives are taken by mouth:
- Bulk-forming laxatives. These contain fiber and draw water into stool. It may take a few days to get results.
- Osmotic and saline laxatives. These hold water in the stool and increase bowel movements. Common side effects include gas, bloating, and nausea.
- Stimulant laxatives. These trigger contractions in the bowels that push stool along.
- Emollient laxatives. These are called “stool softeners.” Mineral oil can block absorption of some vitamins. There are safer, more effective options.
Other treatments
Certain treatments should be used with caution.
Laxatives also come in the form of suppositories or enemas that are inserted into the rectum. These tend to work more quickly, but most people find them unpleasant to use. Avoid "natural" constipation remedies. Their ingredients, effectiveness, and safety may not be well studied.
You can buy prepackaged enemas containing sodium phosphate/biphosphate at your local drugstore. Your doctor may suggest trying one if other laxatives don't help. If so, follow your doctor's instructions carefully. These enemas should not be used more than once a day and can be dangerous for people with kidney or heart disease. Never use a "homemade" enema solution.
When diet and lifestyle changes and other treatments don't provide relief for severe or chronic constipation, your doctor may recommend a prescription medicine. This may be a prescription laxative or an oral medicine (pill) that is used for certain types of constipation.
Constipation and IBS
Constipation can be a symptom of irritable bowel syndrome.
Cramping, abdominal pain, bloating, diarrhea, and constipation can make life miserable. If you experience a combination of these symptoms for three or more months, you might have a condition called irritable bowel syndrome (IBS).
The cause of IBS is unknown. The bowels simply don't work the way they should: sometimes they’re overactive, and sometimes they’re underactive.
Some people with IBS have mildly annoying symptoms that come and go.
Others deal with such severe daily bowel problems that IBS affects their ability to work, sleep, and enjoy life.
For some people, dietary changes, such as cutting back on insoluble fiber or dairy, may improve symptoms. Probiotics also can help.
When constipation is the primary symptom of IBS (also called constipation-predominant IBS), increasing fiber intake and getting plenty of fluids are the first treatments.
Your doctor may also recommend a prescription laxative or other medication to help restore regular bowel movements.
Crohn’s disease and constipation
Symptoms may overlap with IBS, but these conditions are not the same.
Crohn’s disease occurs when the immune system mistakenly attacks the digestive tract. The main symptoms of Crohn’s disease include:
- abdominal cramps
- fever
- fatigue
- loss of appetite
- weight loss
- watery diarrhea
- the feeling that you need to have a bowel movement when you don’t (this may involve straining, pain, and cramping)
- constipation
Some people with Crohn’s disease need iron or calcium supplements, which also can contribute to constipation.
There is no cure for Crohn’s disease. But changes to the diet along with certain medications can help. If you have Crohn’s disease and experience constipation, be sure to get your doctor’s advice before treating yourself.
Constipation from drugs and supplements
Some over-the-counter and prescription drugs, as well as some dietary supplements, cause constipation.
These include:
- iron supplements and vitamins with iron
- calcium supplements
- antacids that contain aluminum
- antidepressants
- narcotic painkillers
- muscle relaxants
- some blood pressure drugs
- some prescription drugs used to treat seizure disorders, Parkinson’s disease, and overactive bladder
Talk with your doctor if you use any of these medications and are suffering from constipation. There may be other options available that are not constipating.
Painkillers and constipation
Constipation is a significant side effect of opioid (narcotic) painkillers.
Opioid pain relievers work by attaching to certain receptors that control pain. Most of these receptors are in the brain and central nervous system, but some are found in the bowels.
When the opioid pain relievers latch on to those receptors, they slow the wave of contractions, known as peristalsis, that pushes stool toward the anus. Extra water is absorbed out of the stool sitting in the bowel. This leaves stools dry and hard. The result is constipation.
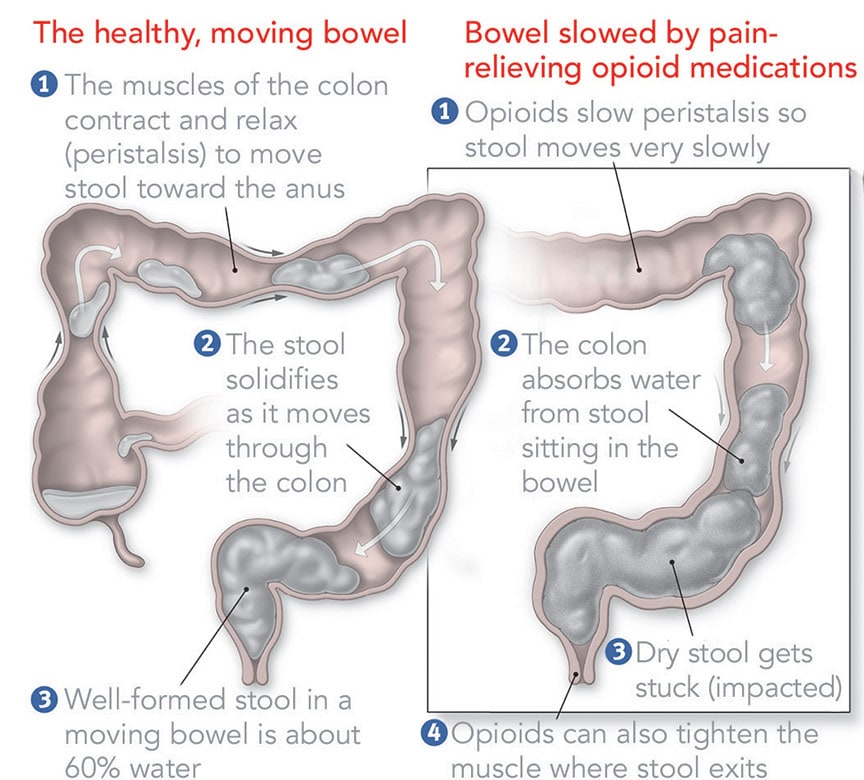
If your doctor prescribes a narcotic pain reliever, ask about ways to prevent constipation before you start taking the medicine.
As you’ve seen constipation is uncomfortable for you, and it can be difficult to pinpoint a cause. A healthy lifestyle, with exercise and nutritious food—especially fiber and fluids—will go a long way toward keeping constipation at bay.
Talk with your doctor
Whether this is your first visit or a follow-up, ask your doctor:
- Is my constipation a sign of an underlying health problem?
- What steps can I take to treat it on my own?
- Should I be eating more of certain foods?
- Are there foods I should avoid?
- Should I take fiber supplements?
- Should I try over-the-counter laxatives or stool softeners?
Your doctor may want to know:
- Is this the first time you’ve experienced constipation?
- When did it start and how long has it lasted?
- Do you take any over-the-counter medications or supplements? If so, which ones?
- What have you tried to relieve constipation (laxatives, stool softeners, diet)?
- Do you use laxatives regularly?
- Have you had other symptoms such as fever, unintended weight loss, or bleeding during bowel movements?


