
Most people get mild headaches from time to time. But an unfortunate few get severe headaches on a regular basis.
Headaches shouldn’t ruin your life. Your doctor can help you find ways to relieve headache pain and help keep headaches from happening in the first place.
Types of headaches
Most headache sufferers have what doctors call “primary headaches,” including:
- Tension headache
- Cluster headache
- Migraine headache
That means the pain is just a headache, and not a sign of a more serious problem.
The most common primary headaches are tension headaches and migraines.
Most headaches are caused by stress, fatigue, hunger, hormonal changes, weather changes, or caffeine withdrawal.
Tension headaches
Tension headaches cause dull squeezing pain on both sides of the head. They are usually caused by:
- muscle tightness in the scalp or neck
- eyestrain
- poor posture

Over-the-counter pain relievers can ease the pain.
To prevent tension headaches, try not to skip meals, make sure you get enough sleep, and pace yourself to avoid fatigue.
Massage, relaxation techniques, biofeedback, and other ways to reduce stress can also help relieve tension headaches and sometimes prevent them.
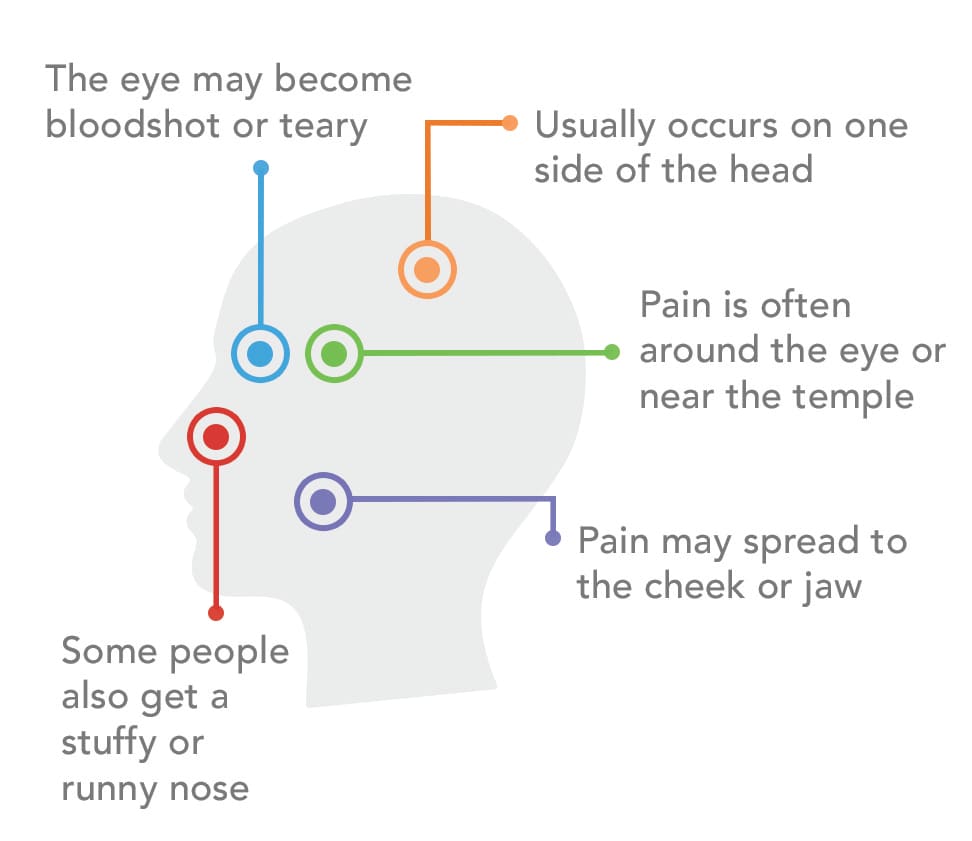
Cluster headaches
A less common kind of primary headache is a cluster headache.
Cluster headaches cause intense, sharp, penetrating pain.
Cluster headaches come in several attacks a day, for a week or longer. Headache-free periods occur between attacks.
Successful treatment of cluster headaches can take trial and error before finding the most effective plan.
Medications and avoiding triggers—things that start these headaches—are usually part of treatment.
Migraine headaches
Migraine headaches can completely disrupt a person’s day.
The word “migraine” comes from a Greek term meaning “half a head". That describes what many people feel: throbbing or pulsating pain on one side of the head.
The pain is often felt around the temple. Many people with migraines feel nauseous or vomit.
Bright lights and loud noises can worsen the pain. The average migraine lasts four to twelve hours, though they can be shorter or longer. Common migraine symptoms include:
- Throbbing pain
- Visual blank spots
- Sparkling or flashing lights
- Light sensitivity
- Increased pain in response to noise
- Fatigue
- Nausea
- Nervousness or anxiety
Migraines seem to run in families. They may be caused by overactivity in certain brain cells.
Diagnosis
Brain scans, such as CT scans, MRIs, and brain wave tests, usually aren’t needed for people whose symptoms strongly suggest a tension, migraine, or cluster headache.
Migraine relief
For some people, over-the-counter pain relievers knock out migraine pain. Some of these products are specifically made to treat migraines.
Some simple steps to ease migraine pain include:
- applying heat or cold to your head, neck, or face
- drinking coffee or other caffeinated beverages
- resting in a quiet, dark room
- massaging the scalp, or other body areas
Many migraine sufferers need prescription medications to relieve pain, nausea, and vomiting.
These work best if taken at the first sign of an attack. Some prescription medications, if taken every day, can help prevent migraines from starting.
Some people feel completely wiped out for a day or two after an attack.
Preventing migraines
In many people with migraines, headaches are set off by triggers. Some common triggers include:
- Fatigue
- Travel
- Alcohol
- Weather
- Food
- Caffeine
Some people get migraines after eating certain foods, food additives or drinks. The list below includes some common migraine triggers from these categories:
- monosodium glutamate (MSG)
- nitrates (in cured meats)
- nuts and peanut butter
- onions
- peas
- pork
- red wine
- sour cream
- vinegar
- yogurt
- avocados
- bananas
- beans
- cheeses, aged and unpasteurized foods
- chicken livers
- chocolate
- citrus fruits
- fermented, pickled, or marinated foods herring
To identify your headache triggers, try to answer these questions:
- What were you doing when the migraine started?
- Was the migraine mild, moderate, or severe, and how long did it last?
- If you’re a woman, at what part of your menstrual cycle did it occur?
- Were you stressed that day?
- Were you physically active when it began?
- When did you last eat?
Identify and avoid your triggers, get enough sleep, eat well, exercise regularly, and manage stress to reduce migraines.
Keep a headache diary
Keeping a headache diary (when they happen and possible triggers) helps you and your doctor understand and treat headaches.
| About Your Headache | First Episode | Second Episode | Third Episode |
| Date/Day of the week | |||
| Time of onset | |||
| Time of resolution | |||
| Warning signs | |||
| Location(s) of the pain | |||
| Type of pain | |||
| Intensity of pain (scale 1-10) | |||
| Additional symptoms | |||
| Activities at time of onset | |||
| Time of last prior meal at onset | |||
| Most recent food/drink at onset | |||
| Medication(s) taken for headache | |||
| Response to medications | |||
| Other actions taken for relief | |||
| Response to other actions | |||
| Last menstrual period (start/end) | |||
| Medications for other conditions |
Rebound headaches
Prescription and over-the-counter pain relievers sometimes can set off a cycle of headache pain:
- You take a pain reliever for your headache.
- As it wears off, your headache pain returns.
- You take another dose of pain reliever.
- As that dose wears off, your headache pain returns.
If you suffer from headaches and find that you’re getting them more and more often, you may be dealing with something called medication overuse headaches, also known as rebound headaches.
The same prescription and over-the-counter medications that you take to make headache pain go away may be triggering headaches.
Treating rebound headaches
No one knows exactly what causes rebound headaches.
One possibility is that taking pain relievers often makes the nervous system more sensitive to pain.
When the pain medicine wears off, the slightest thing can set off a new headache.
Getting rid of rebound headaches isn’t easy. It usually means that you have to go off all headache medicines, which of course leads to pain.
Your doctor can tell you how to taper the drugs causing the problem. She or he may also be able to suggest other medication you can take for a short time during the withdrawal period.
Most rebound headaches improve once the medication is stopped.
Talk with your doctor
Whether this is your first visit or a follow-up, ask these questions for your doctor:
- How often do you get headaches?
- Do headaches run in your family?
- When did they start?
- Has the pain changed?
- How long do they last?
- Do they interfere with your work and family?
- Have you noticed any triggers?
- What stops your headache pain?
- How often do you take medications?
- What is the pain like?
Tell your doctor about any side effects from your medications.
When to call your doctor
- You get a sudden, severe headache that feels like a blow to the head
- You have a severe headache along with fever, nausea, vomiting, shortness of breath, weakness anywhere in your body, confusion, double vision, or a stiff neck
- You have the “worst” headache of your life
- You get a severe headache when you rarely, or never, get headaches
- A headache starts after a head injury


