
What is obstructive sleep apnea?
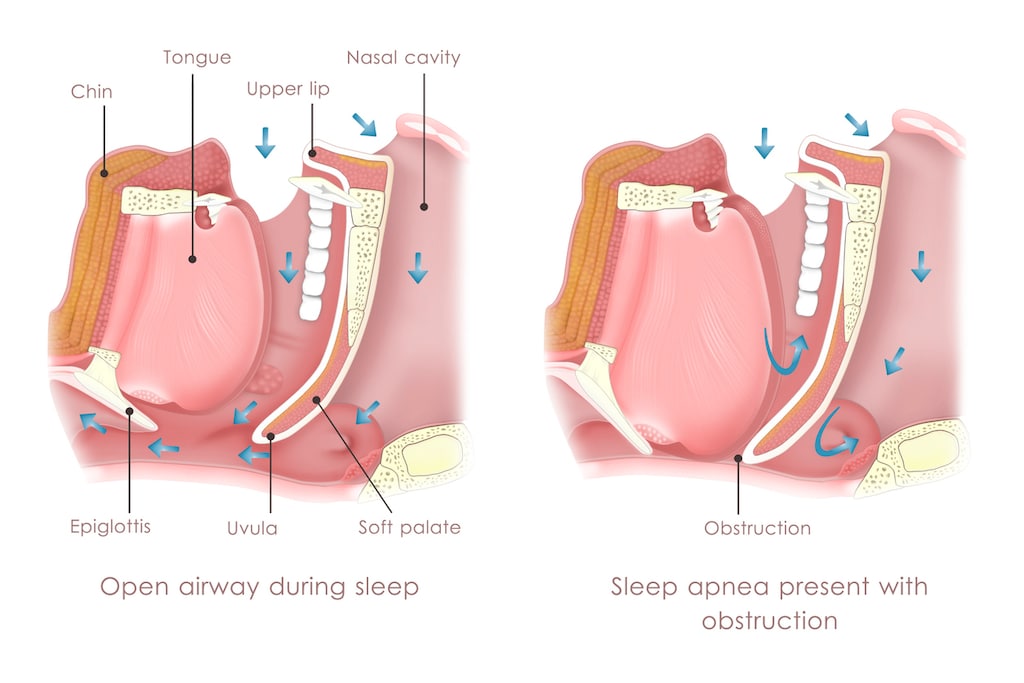
Obstructive sleep apnea (OSA) is a common breathing disorder that causes you to repeatedly stop breathing for 10 to 30 seconds at a time while you’re asleep. It is associated with complete or partial obstruction of your upper airway or throat.
Complete obstruction of your upper airway during sleep results in an episode of apnea - a pause in your breathing. A partial obstruction of your upper airway results in an episode of shallow breathing called hypopnea.
OSA is sometimes referred to as obstructive sleep apnea-hypopnea syndrome (OSAHS) when a person experiences frequent complete and partial blockages of their upper airway.
OSA is the most common type of sleep apnea. The other types of sleep apnea are central sleep apnea and complex sleep apnea.
What causes obstructive sleep apnea?
OSA is caused by the muscles in your throat relaxing so much during sleep that they allow your throat (pharynx) to become blocked.
During an apnea episode there is a decrease in muscle activity in the area of the throat behind the tongue which causes the soft tissues (tongue and soft palate) in the area to temporarily relax and obstruct your airway.
When your airway is obstructed it reduces or stops the flow of air to your lungs, which results in progressive asphyxia and reduced blood oxygen levels. This progressive asphyxia stimulates your breathing efforts and usually causes you to wake up.
What are the risk factors for obstructive sleep apnea?
A number of different factors can increase your risk of developing OSA, including your age, sex and weight.
Risk factors for OSA include:
- Anything that may narrow your upper airway:
- Large tonsils or adenoids - particularly in children
- Neck size (>17 inches in men, >16 inches in women)
- Large tongue
- Having a lower jaw that isn’t as long as your upper jaw (retrognathia)
- A narrow palate
- Obesity or being overweight
- A family history of OSA or snoring
- Men are two to three times more likely to have this condition than premenopausal women
- Older age - being in your 60s or 70s puts your at increased risk, but OSA can affect people of all ages including children
- Smoking
- Chronic nasal congestion
- Having certain conditions such as type 2 diabetes, high blood pressure, chronic lung disease including asthma, polycystic ovary syndrome (PCOS), hypothyroidism or pregnancy.
What are the symptoms of obstructive sleep apnea?
OSA puts your body under stress and interferes with your ability to get a good night’s sleep. Sleep is important for our well-being and not getting enough quality sleep can result in a number of negative side effects.
Signs and symptoms of OSA include:
- Daytime sleepiness
- Loud snoring
- Insomnia and waking up frequently
- Temporarily stopping breathing during sleep (usually observed by another person)
- Nighttime restlessness
- Waking up at night accompanied by choking or gasping for air
- Waking up with a sore throat or dry mouth
- Fatigue or tiredness throughout the day
- Morning headaches
- Difficulty concentrating or a poor memory
- Mood changes, such as irritability or depression
- Night sweats
- Decreased libido
How is obstructive sleep apnea diagnosed?
To diagnose OSA your healthcare professional will begin by asking you about your medical history and carrying out a physical exam.
During this process you will be asked about your symptoms, such as how tired you feel during the day and how well you sleep. Your healthcare professional may also check your throat, mouth, nose, blood pressure, weight and neck circumference.
You may also be referred to a sleep specialist for further evaluation. Your sleep specialist may recommend an overnight sleep study - sometimes these are conducted at home and other times in a sleep lab.
Polysomnography is used during a sleep study to help diagnose OSA. Polysomnography involves using equipment to monitor the following while your sleep:
- Heart rate
- Airflow into and out of your lungs
- Breathing effort and rate
- Blood oxygen levels
- Brain activity
- Muscle activity
- Limb movement
- Eye movement
Monitoring may be carried out for a full night or part of the night. If during your lab-based sleep study a diagnosis of is made, you may be woken up and given a continuous positive airway pressure (CPAP) machine to try for the rest of the night.
You may also be referred to an Ear, Nose and Throat (ENT) specialist if large tonsils or another type of blockage is suspected of causing sleep apnea.
How is obstructive sleep apnea treated?
OSA can be effectively treated. The most appropriate treatment option for you will depend on the results of your diagnostic tests and your risk factors for the condition.
Lifestyle changes may be enough to help some people with mild symptoms. For those with moderate-to-severe symptoms, other treatments may also be necessary. Treatments for OSA include:
- Lifestyle changes. Lifestyle changes that can help to reduce the symptoms of OSA include:
- Weight loss
- Exercising regularly
- Stopping smoking
- Reducing the amount of alcohol you drink and avoiding alcohol before bed
- Avoiding sleeping on your back - sleeping aids, such as a PillowPositive, may be helpful to maintain an optimal sleep position. Sleeping upright may help some obese people with this condition.
- Avoiding sedative medications, such as sleeping pills and anxiety medications
- Using a decongestant or anti-allergy medication
- Continuous positive airway pressure (CPAP) therapy. CPAP therapy is the most popular treatment for OSA. In most cases it can offer immediate relief from sleep apnea symptoms.
CPAP therapy involves wearing a mask on your face while you sleep. The mask is connected to a machine that delivers pressurized air that is pushed into your throat to hold your airway open. - Nasal Expiratory Positive Airway Pressure (EPAP). EPAP is an alternative treatment for OSA that uses reusable or disposable valves that are attached to your nostrils. The valves help to increase airway resistance at the end of your breath out, which helps to hold your airway open as you breathe in.
- Oral appliances. Oral appliances or devices are available to help treat OSA. These are worn in the mouth and typically hold the jaw forward or stop the tongue from blocking the throat. Oral appliances are most often recommended in people with mild symptoms who are not overweight.
- Surgery. Surgery may be recommended to help treat OSA, including surgery to remove enlarged tonsils and adenoids for example.
- Neuromuscular tongue muscle stimulator. eXciteOSA is a neuromuscular tongue muscle stimulator. It is a device you place in your mouth and use for 20 minutes during the day. It delivers a mild electric shock to help strengthen your tongue muscle so that it does not block your airway.
- Implantable nerve stimulator. Inspire Upper Airway Stimulation is an implantable nerve stimulator. It detects a person’s breathing pattern and uses mild nerve stimulation to maintain an open airway. A remote is used to turn the device on and off.
What is the prognosis for obstructive sleep apnea?
The prognosis for people with OSA is very good if it is properly managed and treated.
Left untreated this condition can become a serious, life threatening condition. Untreated OSA puts you at increased risk of:
- High blood pressure
- Cardiovascular disease, including heart attack and stroke
- Type 2 diabetes
- Death
The fatigue caused by this condition also puts you at increased risk of motor vehicle crashes and other accidents.
How is obstructive sleep apnea prevented?
The lifestyle changes used to help treat OSA can also be used to help prevent it. Try losing weight, exercising regularly, avoiding alcohol and stopping smoking. If you have a blocked or stuffy nose try a nasal decongestant or allergy medication. Getting a restful night’s sleep and avoiding sleep deprivation is also important.
Article references
- MedlinePlus. Obstructive sleep apnea. Available at: https://medlineplus.gov/genetics/condition/obstructive-sleep-apnea/. [Accessed March 25, 2022].
- Sleep Foundation. Hypopnea. March 11, 2022. Available at: https://www.sleepfoundation.org/sleep-apnea/hypopnea. [Accessed March 25, 2022].
- Spicuzza L, Caruso D, Di Maria G. Obstructive sleep apnoea syndrome and its management. Ther Adv Chronic Dis. 2015;6(5):273-285. doi:10.1177/2040622315590318.
- Perger E, Taranto-Montemurro L. Upper airway muscles: influence on obstructive sleep apnoea pathophysiology and pharmacological and technical treatment options, Current Opinion in Pulmonary Medicine: November 2021 - Volume 27 - Issue 6 - p 505-513. doi: 10.1097/MCP.0000000000000818.
- Rowley JA, Lareau S, Fahy BF, Garvey C, Sockrider M. What Is Obstructive Sleep Apnea in Adults?. Am J Respir Crit Care Med. 2017;196(1):P1-P2. doi:10.1164/rccm.1961P1.
- American Sleep Apnea Association. Obstructive Sleep Apnea. Available at: https://www.sleepapnea.org/learn/sleep-apnea/obstructive-sleep-apnea/. [Accessed March 25, 2022].
- Sleep Foundation. Obstructive Sleep Apnea. March 11, 2022. Available at: https://www.sleepfoundation.org/sleep-apnea/obstructive-sleep-apnea. [Accessed March 25, 2022].
- MedlinePlus. Polysomnography. Available at: https://medlineplus.gov/ency/article/003932.htm. [Accessed March, 2022].
- American Sleep Association (ASA). CPAP Treatment. Available at: https://www.sleepassociation.org/sleep-apnea/cpap-treatment/. [Accessed March 25, 2022].
- Lorenzi-Filho G, Almeida FR, Strollo PJ. Treating OSA: Current and emerging therapies beyond CPAP. Respirology. 2017;22(8):1500-1507. doi:10.1111/resp.13144.
- Baptista PM, Martínez Ruiz de Apodaca P, Carrasco M, et al. Daytime Neuromuscular Electrical Therapy of Tongue Muscles in Improving Snoring in Individuals with Primary Snoring and Mild Obstructive Sleep Apnea. J Clin Med. 2021;10(9):1883. Published 2021 Apr 27. doi:10.3390/jcm10091883.
- Food and Drug Administration (FDA). Inspire® Upper Airway Stimulation – P130008/S039. June 29, 2020. Available at: https://www.fda.gov/medical-devices/recently-approved-devices/inspirer-upper-airway-stimulation-p130008s039. [Accessed March 25, 2022].
- Medscape. Obstructive sleep apnea (OSA). Prognosis. September 15, 2020. Available at: https://emedicine.medscape.com/article/295807-overview#a6. [Accessed March 25, 2022].
