Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral:
Precose: 25 mg, 50 mg, 100 mg
Generic: 25 mg, 50 mg, 100 mg
Pharmacology
Mechanism of Action
Competitive inhibitor of pancreatic α-amylase and intestinal brush border α-glucosidases, resulting in delayed hydrolysis of ingested complex carbohydrates and disaccharides and absorption of glucose; dose-dependent reduction in postprandial serum insulin and glucose peaks; inhibits the metabolism of sucrose to glucose and fructose
Pharmacokinetics/Pharmacodynamics
Absorption
<2% as active drug, ~35% as metabolites
Metabolism
Exclusively via GI tract, principally by intestinal bacteria and digestive enzymes; 13 metabolites identified (major metabolites are sulfate, methyl, and glucuronide conjugates)
Excretion
Urine (~34% as inactive metabolites, <2% parent drug and active metabolite); feces (~51% as unabsorbed drug)
Time to Peak
Active drug: ~1 hour
Half-Life Elimination
~2 hours
Use in Specific Populations
Special Populations: Renal Function Impairment
In patients with CrCl <25 mL/minute/1.73 m2, the Cmax was ~5 times higher, and the AUC was 6 times larger.
Special Populations: Elderly
AUC and Cmax are approximately 1.5 times higher in the elderly.
Use: Labeled Indications
Diabetes mellitus, type 2: Adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus
Use: Off Label
Postprandial hyperinsulinemic hypoglycemia after gastric bypass surgeryc
Data from a few small, noncontrolled studies suggest acarbose may be helpful in reducing postprandial hypoglycemic events, glycemic variability, insulin secretion, and GLP-1 secretion in patients who experience postprandial hypoglycemia following Roux-en-Y gastric bypass (RYGB) Frankhouser 2013, Mordes 2015, Ritz 2012, Valderas 2012. Acarbose was used as adjunctive therapy to dietary modification that reduced the carbohydrate content of each meal and encouraged smaller, more frequent meals to achieve daily caloric intake Frankhouser 2013, Mordes 2015, Ritz 2012.
The American Society for Metabolic and Bariatric Surgery position statement on postprandial hyperinsulinemic hypoglycemia after bariatric surgery states that in patients refractory to dietary modification, pharmacotherapy (including acarbose) may be effective in treating hypoglycemic symptomology and should be attempted before considering surgical interventions Weisenburg 2017.
Contraindications
Hypersensitivity to acarbose or any component of the formulation; diabetic ketoacidosis; cirrhosis; inflammatory bowel disease, colonic ulceration, partial intestinal obstruction, patients predisposed to intestinal obstruction; chronic intestinal diseases associated with marked disorders of digestion or absorption; conditions that may deteriorate as a result of increased gas formation in the intestine
Dosage and Administration
Dosing: Adult
Diabetes mellitus, type 2: Note: Dosage must be individualized on the basis of effectiveness and tolerance. Oral: Initial dose: 25 mg 3 times daily with the first bite of each main meal (may also initiate at 25 mg once daily with gradual titration to 25 mg 3 times daily as tolerated); increase dose at 4- to 8-week intervals based on 1-hour postprandial glucose or glycosylated hemoglobin levels and tolerance until maintenance dose of 50 to 100 mg 3 times daily is reached (maximum dose: ≤60 kg: 50 mg 3 times daily; >60 kg: 100 mg 3 times daily)
Postprandial hyperinsulinemic hypoglycemia after gastric bypass surgery (off-label): Oral: 25 to 100 mg 3 times daily just prior to the start of each meal, or if more frequent meals may consider 25 to 50 mg up to 6 times daily. Administer in conjunction with dietary modifications aimed at reducing the glycemic index of each meal (Frankhouser 2013; Mordes 2015; Ritz 2012; Valderas 2012)
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Dosage must be individualized on the basis of effectiveness and tolerance.
Diabetes mellitus, type 2: Children ≥10 years and Adolescents: Very limited data available: Oral: Initial dose: 25 mg 3 times daily with the first bite of each main meal; may also initiate at 25 mg once daily with gradual titration to 25 mg 3 times daily as tolerated; then increase in 25 mg/dose increments in 2 to 4 week intervals as tolerated. Weight-based maximum dose: ≤60 kg: 50 mg/dose, >60 kg: 100 mg/dose. Clinical trials in pediatric patients are lacking; dosing based on expert reported clinical experience; overall dosing is similar to that used in adult patients (DeFronzo 1999; Jacobson-Dickman 2005; Kliegman 2016)
Dumping syndrome (reactive hypoglycemia) after Nissen fundoplication: Limited data available: Infants ≥4 months and young children who have failed nutritional manipulations: Oral: Initial dose: 12.5 to 25 mg before each bolus feeding of formula containing complex carbohydrates. Increase in 12.5 to 25 mg/dose increments until postprandial serum glucose stable (>60 mg/dL was used in clinical reports). Reported dose range: 12.5 to 100 mg/dose. Dosing based on a few small studies (total n=11). Acarbose was well tolerated in most patients; except a few patients experienced flatulence (De Cunto 2011; Ng 2001; Zung 2003).
Administration
Oral: Administer with the first bite of each main meal.
Storage
Store at <25°C (77°F). Protect from moisture.
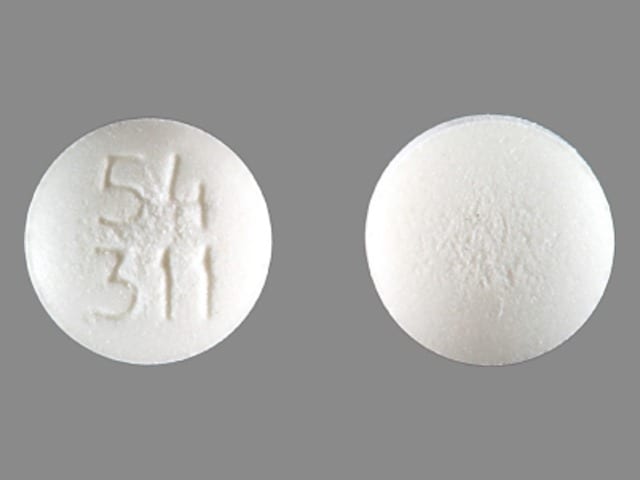
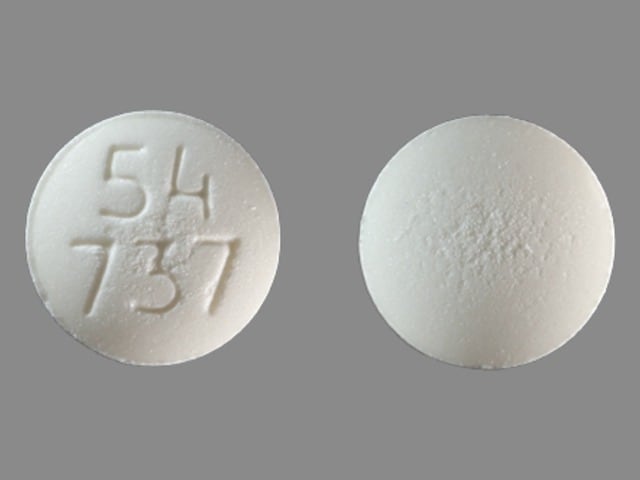
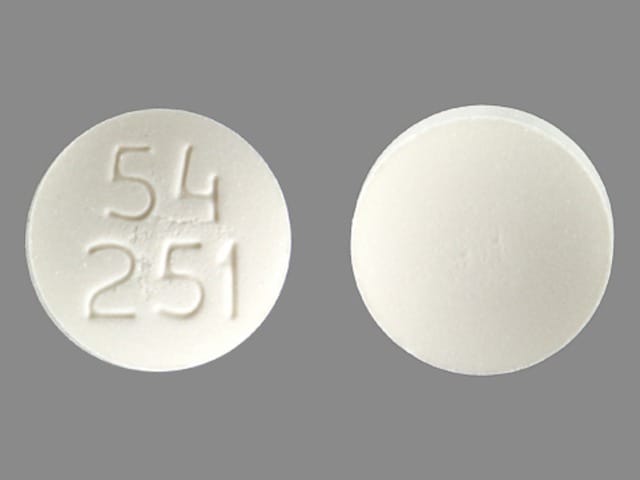
Acarbose Images
Drug Interactions
Alpha-Lipoic Acid: May enhance the hypoglycemic effect of Antidiabetic Agents. Monitor therapy
Androgens: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Exceptions: Danazol. Monitor therapy
Digoxin: Acarbose may decrease the serum concentration of Digoxin. Monitor therapy
Direct Acting Antiviral Agents (HCV): May enhance the hypoglycemic effect of Antidiabetic Agents. Monitor therapy
Guanethidine: May enhance the hypoglycemic effect of Antidiabetic Agents. Monitor therapy
Hyperglycemia-Associated Agents: May diminish the therapeutic effect of Antidiabetic Agents. Monitor therapy
Hypoglycemia-Associated Agents: Antidiabetic Agents may enhance the hypoglycemic effect of Hypoglycemia-Associated Agents. Monitor therapy
Maitake: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Monoamine Oxidase Inhibitors: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Neomycin: May enhance the adverse/toxic effect of Acarbose. Neomycin may decrease the metabolism of Acarbose. Monitor therapy
Pegvisomant: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Prothionamide: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Quinolones: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Quinolones may diminish the therapeutic effect of Blood Glucose Lowering Agents. Specifically, if an agent is being used to treat diabetes, loss of blood sugar control may occur with quinolone use. Monitor therapy
Ritodrine: May diminish the therapeutic effect of Antidiabetic Agents. Monitor therapy
Salicylates: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Selective Serotonin Reuptake Inhibitors: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Thiazide and Thiazide-Like Diuretics: May diminish the therapeutic effect of Antidiabetic Agents. Monitor therapy
Adverse Reactions
>10%: Gastrointestinal: Frequency and intensity of flatulence (74%) tend to abate with time; diarrhea (31%) and abdominal pain (19%) tend to return to pretreatment levels over time
1% to 10%: Hepatic: Increased serum transaminases (≤4%)
<1%, postmarketing, and/or case reports: Edema, erythema, hepatic injury, hepatitis, intestinal obstruction, jaundice, pneumatosis cystoides intestinalis, skin rash, thrombocytopenia, urticaria
Warnings/Precautions
Concerns related to adverse effects:
- Elevated serum transaminases: Treatment-emergent elevations of serum transaminases (AST and/or ALT) and hyperbilirubinemia may occur (dose-related). These elevations were asymptomatic, reversible, more common in females, and, in general, were not associated with other evidence of liver dysfunction. Fulminant hepatitis (may be fatal) has been reported. If elevations are observed, a reduction in dosage or withdrawal of therapy may be indicated, particularly if the elevations persist.
- Hypoglycemia: Hypoglycemia is unlikely to occur with acarbose monotherapy but may occur with combination therapy (eg, sulfonylureas, insulin, metformin). In patients taking acarbose, oral glucose (dextrose) should be used instead of sucrose (cane sugar) in the treatment of mild-to-moderate hypoglycemia since the hydrolysis of sucrose to glucose and fructose is inhibited by acarbose.
Disease-related concerns:
- Hepatic impairment: Use with caution in patients with hepatic impairment.
- Renal impairment: Not recommended in patients with significant impairment (serum creatinine >2 mg/dL or CrCl <25 mL/minute/1.73 m2).
- Stress-related states: It may be necessary to discontinue acarbose and administer insulin if the patient is exposed to stress (ie, fever, trauma, infection, surgery).
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Other warnings/precautions:
- Appropriate use: Diet: Increased intake of sucrose (cane sugar) and food that contains sucrose during treatment can lead to GI symptoms (eg, flatulence and bloating), loose stools, and occasionally diarrhea. If a diabetic diet is not followed, the GI side effects may be intensified. If severe symptoms develop in spite of adherence to a diabetic diet, temporarily or permanently reduce dose.
- Patient education: Diabetes self-management education (DSME) is essential to maximize the effectiveness of therapy.
Monitoring Parameters
Postprandial glucose, hemoglobin A1c (at least twice yearly in patients who have stable glycemic control and are meeting treatment goals; quarterly in patients not meeting treatment goals or with therapy change [ADA 2019]), serum creatinine; serum transaminase levels every 3 months during the first year of treatment and periodically thereafter.
Pregnancy
Pregnancy Risk Factor
B
Pregnancy Considerations
Information related to the use of acarbose in pregnancy is limited (Bertini 2005; Narayanan 2016). Less than 2% of an oral dose of acarbose is absorbed systemically, which should limit fetal exposure.
Poorly controlled diabetes during pregnancy can be associated with an increased risk of adverse maternal and fetal outcomes, including diabetic ketoacidosis, preeclampsia, spontaneous abortion, preterm delivery, delivery complications, major birth defects, stillbirth, and macrosomia (ACOG 201 2018). To prevent adverse outcomes, prior to conception and throughout pregnancy, maternal blood glucose and HbA1c should be kept as close to target goals as possible but without causing significant hypoglycemia (ADA 2020; Blumer 2013).
Agents other than acarbose are currently recommended to treat diabetes mellitus in pregnancy (ADA 2020).
Patient Education
What is this drug used for?
- It is used to lower blood sugar in patients with high blood sugar (diabetes).
Frequently reported side effects of this drug
- Abdominal pain
- Passing gas
- Diarrhea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Low blood sugar like dizziness, headache, fatigue, feeling weak, shaking, fast heartbeat, confusion, increased hunger, or sweating
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin or eyes
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.