Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Capsule, Oral:
Zovirax: 200 mg [DSC] [contains fd&c blue #2 (indigotine), parabens]
Generic: 200 mg
Solution, Intravenous, as sodium [strength expressed as base]:
Generic: 50 mg/mL (20 mL)
Solution, Intravenous, as sodium [strength expressed as base, preservative free]:
Generic: 50 mg/mL (10 mL, 20 mL)
Solution Reconstituted, Intravenous, as sodium [strength expressed as base]:
Generic: 500 mg (1 ea [DSC])
Suspension, Oral:
Zovirax: 200 mg/5 mL (473 mL) [contains methylparaben, propylparaben; banana flavor]
Generic: 200 mg/5 mL (473 mL)
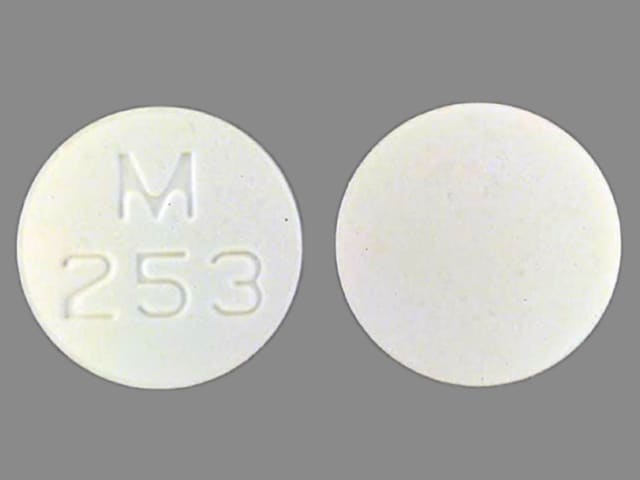
Tablet, Oral:
Zovirax: 400 mg
Zovirax: 800 mg [contains fd&c blue #2 (indigotine)]
Generic: 400 mg, 800 mg
Pharmacology
Mechanism of Action
Acyclovir is converted to acyclovir monophosphate by virus-specific thymidine kinase then further converted to acyclovir triphosphate by other cellular enzymes. Acyclovir triphosphate inhibits DNA synthesis and viral replication by competing with deoxyguanosine triphosphate for viral DNA polymerase and being incorporated into viral DNA.
Pharmacokinetics/Pharmacodynamics
Absorption
Oral: Poorly absorbed; absorption improves marginally with multiple small doses vs. one large daily dose (de Miranda 1983)
Distribution
Widely (eg, brain, kidney, lungs, liver, spleen, muscle, uterus, vagina, CSF) (de Miranda 1983; Laskin 1983); CSF acyclovir concentration is ~50% of plasma concentrations.
Vdss (Blum 1982; Laskin 1983; Spector 1981):
Neonates to 3 months of age: 28.8 L/1.73 m2
Children 1 to 2 years: 31.6 L/1.73 m2
Children 2 to 7 years: 42 L/1.73 m2
Adults: 0.8 L/kg (63.6 L)
Metabolism
Converted by viral enzymes to acyclovir monophosphate, and further converted to diphosphate then triphosphate (active form) by cellular enzymes
Excretion
Urine (62% to 91% as unchanged drug and metabolite)
Half-Life Elimination
Half-life elimination: Terminal: Neonates and Infants ≤3 months: 3.8 ± 1.19 hours; Infants >3 months to Children ≤12 years: 2.36 ± 0.97 hours; Adults: ~2.5 hours (with normal renal function); 20 hours (ESRD) (Gorlitsky 2017); Hemodialysis: ~5 hours
Protein Binding
9% to 33%
Use in Specific Populations
Special Populations: Renal Function Impairment
Total body clearance and half-life are dependent on renal function.
Use: Labeled Indications
Oral:
Herpes simplex virus (HSV), genital: Treatment of initial episodes and the management of recurrent episodes of genital herpes.
Herpes zoster (shingles): Acute treatment of herpes zoster (shingles).
Varicella (chickenpox): Treatment of varicella (chickenpox).
Injection:
Herpes simplex encephalitis: Treatment of herpes simplex encephalitis.
Herpes simplex virus (HSV), genital infection (severe): Treatment of severe initial clinical episodes of genital herpes in immunocompetent patients.
Herpes simplex virus (HSV), mucocutaneous infection in immunocompromised patients: Treatment of initial and recurrent mucosal and cutaneous herpes simplex (HSV-1 and HSV-2) in immunocompromised patients.
Herpes simplex virus (HSV), neonatal: Treatment of neonatal herpes infections.
Herpes zoster (shingles) in immunocompromised patients: Treatment of herpes zoster (shingles) in immunocompromised patients.
Use: Off Label
Bell palsy, new onsetbyes
There is insufficient evidence to recommend acyclovir for the treatment of Bell palsy. However, American Academy of Neurology (AAN) guidelines state that antivirals may, at best, provide a modest increase in recovery and may be reserved as an option.
Cytomegalovirus prevention in low-risk allogeneic hematopoietic cell transplant recipientsyes
Based on the American Society for Blood and Marrow Transplantation (ASBMT) and Infectious Diseases Society of America (IDSA) guidelines for preventing infectious complications among hematopoietic cell transplant recipients, acyclovir is recommended as an alternative agent to prevent cytomegalovirus (CMV) reactivation in low-risk allogeneic hematopoietic cell transplant (HCT) recipients.
Herpes simplex virus, esophagitisc
Clinical experience and case reports suggest the utility of acyclovir in the treatment of esophagitis due to herpes simplex virus (HSV) in immunocompetent or immunocompromised patients Bonis 2018, Canalejo 2010.
Herpes simplex virus, prevention in immunocompromised patientscyes
Based on the ASBMT/IDSA guidelines for preventing infectious complications among hematopoietic cell transplant recipients, acyclovir is an effective and recommended agent to prevent HSV reactivation (early and late) in HCT recipients.
Based on the American Society of Clinical Oncology (ASCO) and IDSA guidelines for antimicrobial prophylaxis for adult patients with cancer-related immunosuppression, acyclovir is an effective and recommended agent to prevent HSV reactivation in patients undergoing leukemia induction therapy.
Clinical experience suggests the utility of acyclovir for prevention of HSV in seropositive solid organ transplant recipients who are not already receiving CMV prophylaxis Wilck 2013.
Herpes zoster ophthalmicusc
Clinical experience suggests the utility of IV acyclovir for the treatment of herpes zoster ophthalmicus in patients who are immunocompromised or require hospitalization for sight-threatening disease Albrecht 2018a.
Varicella zoster virus, acute retinal necrosiscyes
Based on the US Department of Health and Human Services (HHS) guidelines for the prevention and treatment of opportunistic infections in HIV-infected adults and adolescents, intravenous acyclovir is an effective and recommended agent in the management of varicella zoster virus (VZV) acute retinal necrosis (ARN) in immunocompromised patients (HIV-infected patients).
Clinical experience suggests the utility of intravenous acyclovir in the treatment of VZV ARN in immunocompetent patients Albrecht 2018b.
Varicella zoster virus, encephalitiscyes
Based on the IDSA clinical practice guideline for the management of encephalitis, intravenous acyclovir is recommended for the treatment of encephalitis caused by VZV.
Clinical experience suggests the use of intravenous acyclovir for the treatment of VZV encephalitis Chamizo 2016.
Varicella zoster virus, prevention in immunocompromised patientscyes
Based on the ASBMT/IDSA guidelines for preventing infectious complications among hematopoietic cell transplant recipients, acyclovir is an effective and recommended agent to prevent VZV reactivation in HCT recipients (allogeneic and autologous) who are VZV seropositive.
Clinical experience suggests the utility of acyclovir for the prevention of VZV in seropositive solid organ transplant recipients who are not already receiving CMV prophylaxis Pergam 2013.
Contraindications
Hypersensitivity to acyclovir, valacyclovir, or any component of the formulation
Dosage and Administration
Dosing: Adult
Bell palsy, new onset (adjunctive therapy) (alternative agent) (off-label use): Oral: 400 mg 5 times daily for 10 days in combination with corticosteroids; begin within 3 days of symptom onset. Note: Antiviral therapy alone is not recommended (AAN [Gronseth 2012]; AAO-HNSF [Baugh 2013]; Ronthal 2018); some experts only recommend addition of an antiviral to steroid therapy in patients with severe Bell palsy (de Almeida 2014).
Cytomegalovirus (CMV), prevention in low-risk allogeneic hematopoietic cell transplant (HCT) recipients (alternative agent) (off-label use): Note: Begin at engraftment and continue to day 100; requires close monitoring for CMV reactivation (due to weak activity); not for use in patients at high risk for CMV disease (ASBMT/IDSA [Tomblyn 2009]):
IV: 500 mg/m2/dose every 8 hours for up to 4 weeks or until hospital discharge, followed by oral therapy (ASBMT/IDSA [Tomblyn 2009]; Boeckh 2009; Ljungman 2002)
Oral: Following initial IV therapy: 800 mg 4 times daily (ASBMT/IDSA [Tomblyn 2009]; Boeckh 2009; Ljungman 2002)
Herpes simplex virus (HSV), central nervous system infection (encephalitis or meningitis): IV: 10 mg/kg/dose every 8 hours. Duration for encephalitis is 14 to 21 days and for meningitis is 10 to 14 days; treatment of encephalitis requires IV therapy while treatment of meningitis may include step-down oral antiviral therapy. Note: Empiric HSV therapy should be initiated in all patients with suspected encephalitis (IDSA [Tunkel 2008]; Tunkel 2018; Wilck 2013).
Herpes simplex virus, mucocutaneous infection:
Esophagitis (off-label use):
Immunocompetent patients: Oral: 400 mg 3 times daily or 200 mg 5 times daily for 7 to 10 days (Bonis 2018; Canalejo Castrillero 2010)
Immunocompromised patients: Oral: 400 mg 5 times daily for 14 to 21 days (Bonis 2018)
Patients with severe odynophagia or dysphagia: IV: 5 mg/kg/dose every 8 hours; patients who rapidly improve can be switched to an oral antiviral to complete a total of 7 to 14 days of therapy (Bonis 2018; Canalejo Castrillero 2010).
Genital:
Immunocompetent patients:
Treatment, initial episode:
Oral: 400 mg 3 times daily or 200 mg 5 times daily for 7 to 10 days; extend duration if lesions have not healed completely after 10 days (CDC [Workowski 2015]).
IV (for severe disease): 5 to 10 mg/kg/dose every 8 hours for 2 to 7 days, followed by oral acyclovir (or similar antiviral) to complete ≥10 days of therapy total (CDC [Workowski 2015])
Treatment, recurrent episode: Oral: 400 mg 3 times daily for 5 days or 800 mg twice daily for 5 days or 800 mg 3 times daily for 2 days. Note: Treatment is most effective when initiated during the prodrome or within 1 day of lesion onset (CDC [Workowski 2015]).
Suppressive therapy (eg, for severe and/or frequent recurrences): Oral: 400 mg twice daily. Note: Reassess need periodically (eg, annually) (CDC [Workowski 2015]).
Immunocompromised patients (including HIV-infected):
Treatment, initial or recurrent episode:
Oral: 400 mg 3 times daily for 5 to 10 days; extend treatment duration if lesions have not healed completely after 10 days (CDC [Workowski 2015]; HHS [OI adult 2018]; Wilck 2013).
IV (for severe disease): 5 to 10 mg/kg/dose every 8 hours for 2 to 7 days, followed by oral acyclovir (or similar antiviral) once lesions begin to regress and continue for ≥10 days of therapy and until complete resolution (CDC [Workowski 2015]; HHS [OI adult 2018]).
Suppressive therapy (eg, for severe and/or frequent recurrences): Oral: 400 to 800 mg 2 to 3 times daily. Note: Reassess need periodically (eg, annually) (CDC [Workowski 2015]; HHS [OI adult 2018]).
Pregnant females:
Treatment, initial episode: Oral: 400 mg 3 times daily for 7 to 10 days; extend treatment duration if lesion has not healed completely after 10 days (ACOG 2007).
Treatment, recurrent episode (symptomatic): Oral: 400 mg 3 times daily or 800 mg twice daily for 5 days (ACOG 2007). Note: Some experts reserve treatment of recurrent episodes for patients with severe and/or frequent symptoms (Riley 2018).
Suppressive therapy, for patients with a genital HSV lesion anytime during pregnancy: Oral: 400 mg 3 times daily, beginning at 36 weeks' gestation and continued until the onset of labor (ACOG 2007; CDC [Workowski 2015]; Riley 2018). Note: Some experts offer suppressive therapy earlier than 36 weeks' gestation for women who have a first-episode lesion during the third trimester (Riley 2018).
Orolabial: Note: Initiate therapy at earliest symptom.
Immunocompetent and immunocompromised patients (including HIV-infected):
Treatment, initial or recurrent episode:
Oral: 400 mg 3 times daily for 5 to 10 days and until complete lesion resolution in immunocompromised patients (HHS [OI adult 2018]; Klein 2018; Wilck 2013)
IV (for severe disease in immunocompromised patients): 5 mg/kg/dose every 8 hours; switch to oral acyclovir (or similar antiviral) once lesions begin to regress and continue until complete resolution (HHS [OI adult 2018]; Wilck 2013).
Suppressive therapy (eg, for severe and/or frequent recurrences): Oral: 400 mg twice daily (HHS [OI adult 2018]; Rooney 1993). Note: Reassess need periodically (eg, annually) (HHS [adult OI 2018]).
Herpes simplex virus, prevention in immunocompromised patients (off-label use):
Seropositive HCT recipients (allogeneic or autologous) or seropositive patients undergoing leukemia induction chemotherapy:
IV: 250 mg/m2/dose every 12 hours (ASBMT/IDSA [Tomblyn 2009])
Oral: 400 to 800 mg twice daily (ASBMT/IDSA [Tomblyn 2009])
Note: Initiate with the chemotherapeutic or conditioning regimen and continue until recovery of WBC count and resolution of mucositis; duration may be extended in patients with frequent recurrences or graft-vs-host disease (ASBMT/IDSA [Tomblyn 2009]; ASCO/IDSA [Taplitz 2018]).
Solid organ transplant recipients (HSV-seropositive patients who do not require CMV prophylaxis): Oral: 400 to 800 mg twice daily for ≥1 month (Wilck 2013); some experts recommend continuing for 3 to 6 months after transplantation and during periods of lymphodepletion associated with treatment of rejection (Fishman 2018).
Herpes zoster (shingles), treatment:
Immunocompetent patients: Oral: 800 mg 5 times daily for 7 days (Pott Junior 2018; Shafran 2004). Initiate at earliest sign or symptom; treatment is most effective when initiated ≤72 hours after rash onset, but may initiate treatment >72 hours after rash onset if new lesions are continuing to appear (Cohen 1999).
Immunocompromised patients (including HIV-infected):
Acute localized dermatomal: Oral: 800 mg 5 times daily for 7 to 10 days; consider longer duration if lesions resolve slowly (HHS [OI adult 2018]; Pergam 2013).
Extensive cutaneous lesions or visceral involvement: IV: 10 to 15 mg/kg/dose every 8 hours (HHS [OI adult 2018]; Pergam 2013). When formation of new lesions has ceased and signs/symptoms of visceral infection are improving, switch to an oral antiviral to complete a total of 10 to 14 days of therapy (HHS [OI adult 2018]).
Herpes zoster ophthalmicus (off-label use): Immunocompromised patients or patients who require hospitalization for sight-threatening disease: IV: 10 mg/kg/dose every 8 hours for 7 days (Albrecht 2018a)
Varicella (chickenpox), treatment: Ideally initiate therapy within 24 hours of symptom onset, but may start later if the patient still has active lesions:
Immunocompetent patients with uncomplicated infection: Oral: 800 mg 5 times daily for ≥5 to 7 days and until all lesions have crusted (Albrecht 2018b; Arvin 1996; Wallace 1992)
Immunocompromised patients (including HIV-infected):
Severe or complicated infection: IV: 10 mg/kg/dose every 8 hours for 7 to 10 days (HHS [OI adult 2018]; Pergam 2013); some experts recommend up to 15 mg/kg/dose every 8 hours (HHS [OI adult 2018]). May switch to oral antiviral after defervescence if no evidence of visceral involvement; continue until all lesions have crusted (HHS [OI adult 2018]; Pergam 2013).
Uncomplicated infection: Oral: 800 mg 5 times daily for 5 to 7 days (HHS [OI adult 2018]); some experts recommend a minimum duration of 7 days, extending the course until all lesions have crusted (Albrecht 2018b; Pergam 2013).
Varicella zoster virus (VZV), acute retinal necrosis (off-label use): IV: 10 to 15 mg/kg/dose every 8 hours for 10 to 14 days, followed by ~6 weeks of valacyclovir (Albrecht 2018a; HHS [OI adult 2018]); in HIV-infected patients, intravitreal ganciclovir should be added (HHS [OI adult 2018]).
Varicella zoster virus, encephalitis (off-label use): IV: 10 to 15 mg/kg/dose every 8 hours for 10 to 14 days (IDSA [Tunkel 2008])
Varicella zoster virus, prevention in immunocompromised patients (off-label use):
Seropositive HCT recipients (allogeneic and autologous): Oral: 800 mg twice daily (ASBMT/IDSA [Tomblyn 2009]; Boeckh 2006). Note: Initiate with the chemotherapeutic or conditioning regimen and continue for 1 year; may extend duration in patients requiring ongoing immunosuppression (some experts continue prophylaxis in these patients until 6 months after discontinuation of all systemic immunosuppression) (ASBMT/IDSA [Tomblyn 2009]).
Solid organ transplant recipients (VZV-seropositive patients who do not require CMV prophylaxis): Oral: 200 mg 3 to 5 times daily for 3 to 6 months after transplantation and during periods of lymphodepletion associated with treatment of rejection (Fishman 2018; Pergam 2013)
Dosing: Geriatric
Refer to adult dosing; use with caution.
Dosing: Pediatric
Note: Obese patients should be dosed using ideal body weight. Parenteral IV doses >15 mg/kg/dose or 500 mg/m2 may be associated with an increased risk of nephrotoxicity; close monitoring of renal function is recommended (Rao 2015).
CMV prophylaxis: Low-risk allogeneic hematopoietic stem cell transplant (HSCT) in seropositive recipient. Note: Begin at engraftment and continue to day 100; requires close monitoring for CMV reactivation (due to weak activity); not for use in patients at high risk for CMV disease (Tomblyn 2009):
Oral:
Infants, Children, and Adolescents <40 kg: 600 mg/m2/dose 4 times daily; maximum dose: 800 mg/dose
Children and Adolescents ≥40 kg: 800 mg 4 times daily
IV: Infants, Children, and Adolescents: 500 mg/m2/dose every 8 hours
Herpes zoster, acute retinal necrosis, treatment (HIV-exposed/-positive):
Initial treatment: IV: Note: Follow up IV therapy with oral acyclovir or valacyclovir maintenance therapy.
Infants: 10 to 15 mg/kg/dose every 8 hours for 10 to 14 days (DHHS [pediatric] 2013)
Children: 10 to 15 mg/kg/dose every 8 hours for 10 to 14 days (DHHS [pediatric] 2013)
Adolescents: 10 to 15 mg/kg/dose every 8 hours for 10 to 14 days (DHHS [adult] 2015)
Maintenance treatment; begin after 10- to 14-day course of IV acyclovir: Oral: Infants and Children: 20 mg/kg/dose 4 times daily for 4 to 6 weeks (DHHS [pediatric] 2013)
Herpes zoster (shingles), treatment:
Immunocompetent host:
Ambulatory therapy: Oral: Children ≥12 years and Adolescents: 800 mg every 4 hours (5 doses per day) for 5 to 7 days (Red Book [AAP 2015])
Hospitalized patient: IV:
Infants: 10 mg/kg/dose every 8 hours for 7 to 10 days (Red Book [AAP 2015])
Children and Adolescents: 500 mg/m2/dose every 8 hours for 7 to 10 days; some experts recommend 10 mg/kg/dose every 8 hours (Red Book [AAP 2015])
Immunocompromised host (non-HIV-exposed/-positive): IV: Infants, Children, and Adolescents: 10 mg/kg/dose every 8 hours for 7 to 10 days (Red Book [AAP 2015])
HIV-exposed/-positive:
Mild, uncomplicated disease and no or moderate immune suppression: Oral:
Infants and Children: 20 mg/kg/dose 4 times daily for 7 to 10 days; maximum dose: 800 mg/dose; consider longer course if resolution of lesions is slow (DHHS [pediatric] 2013)
Adolescents: 800 mg 5 times daily for 7 to 10 days, longer if lesions resolve slowly (DHHS [adult] 2015)
Severe immune suppression or complicated disease; trigeminal nerve involvement, extensive multidermatomal zoster or extensive cutaneous lesions or visceral involvement: IV:
Infants: 10 mg/kg/dose every 8 hours until resolution of cutaneous lesions and visceral disease clearly begins, then convert to oral therapy to complete a 10- to 14-day total course of therapy (DHHS [pediatric] 2013)
Children: 10 mg/kg/dose or 500 mg/m2/dose every 8 hours until resolution of cutaneous lesions and visceral disease clearly begins, then convert to oral therapy to complete a 10- to 14-day total course of therapy (DHHS [pediatric] 2013)
Adolescents: 10 to 15 mg/kg/dose every 8 hours until clinical improvement is evident, then convert to oral therapy to complete a 10- to 14-day total course of therapy (DHHS [adult] 2015)
HSV neonatal infection, treatment and suppressive therapy in very young infants (independent of HIV status):
Treatment (disseminated, CNS, or skin, eye, or mouth disease): Infants 1 to 3 months: IV: 20 mg/kg/dose every 8 hours; treatment duration: For cutaneous and mucous membrane infections (skin, eye, or mouth): 14 days; for CNS or disseminated infection: 21 days (AAP [Kimberlin 2013]; Bradley 2015; CDC [Workowski 2015]; DHHS [pediatric] 2013; Red Book [AAP 2015])
Chronic suppressive therapy following any neonatal HSV infection:
AAP Recommendation (low dose, 6-month course): Infants: Oral: 300 mg/m2/dose every 8 hours for 6 months; begin after completion of a 14- to 21-day-course of IV therapy dependent upon type of infection (AAP [Kimberlin 2013]; Kimberlin 2011; Red Book [AAP 2015])
Alternate dosing (high dose, 2-year course) in infants with disseminated or CNS infection (Tiffany 2005): Limited data available: Infants and Children <3 years: Oral: Begin after completion of a 21-day course of IV therapy; dosing based on a prospective trial of 16 consecutive neonates (GA: Premature: n=4; term=12; age at treatment: Neonate: n=14; PNA >30 days: n=1) following disseminated or CNS infection; pharmacokinetic data were used to determine dosing regimen to maintain serum acyclovir concentration above target of 2 to 3 mcg/mL; treatment was continued for 2 years in 14 of 16 patients; results showed normal neurodevelopmental outcomes in 69% and normal motor development in 70%; no untoward effects were reported during the study duration.
Initial dosing: 400 mg twice daily; approximate dose: 1,200 to 1,600 mg/m2/dose twice daily
Maintenance dosing: Note: Approximate doses for patients born at term:
Infants 1 to <5 months: 400 mg twice daily
Infants 5 to <9 months: 600 mg twice daily
Infants and Children 9 to <15 months: 800 mg twice daily
Children 15 to 24 months: 1,000 mg twice daily
Note: In the trial, serum acyclovir concentrations were evaluated to assess adequacy of dosing to maintain serum concentrations above the target of 2 to 3 mcg/mL. Samples were collected 1 hour after a witnessed dose; if the acyclovir serum concentration approached or was below the target, the dose was increased to the next greater 200 mg increment. Maximum dose: 1,200 mg. Serum concentrations were evaluated every 3 months; in order to limit the phlebotomy losses, follow-up serum concentrations were not evaluated outside of routine monitoring.
HSV encephalitis, treatment:
Infants and Children 3 months to <12 years:
Non-HIV-exposed/-positive: IV: 10 to 15 mg/kg/dose every 8 hours for 14 to 21 days. Note: Due to increased risk of neurotoxicity and nephrotoxicity, higher doses (20 mg/kg) are not recommended (Red Book [AAP 2015]).
HIV-exposed/-positive: IV: 10 mg/kg/dose every 8 hours for 21 days; higher doses (up to 20 mg/kg) may be necessary (DHHS [pediatric] 2013)
Children ≥12 years and Adolescents (independent of HIV status): IV: 10 mg/kg/dose every 8 hours for 14 to 21 days (Red Book [AAP 2015)]
HSV genital infection:
First infection, mild to moderate:
Non-HIV-exposed/-positive:
Children <12 years: Oral: 40 to 80 mg/kg/day divided in 3 to 4 doses per day for 5 to 10 days; maximum daily dose: 1,200 mg/day (Bradley 2015; Red Book [AAP 2015])
Children and Adolescents ≥12 years: Oral: 200 mg every 4 hours while awake (5 times daily) or 400 mg 3 times daily for 7 to 10 days; treatment can be extended beyond 10 days if healing is not complete (CDC [Workowski 2015]; Red Book [AAP 2015])
HIV-exposed/-positive:
Children: Oral: 20 mg/kg/dose 3 times daily for 7 to 10 days; maximum dose: 400 mg/dose (DHHS [pediatric] 2013)
Adolescents: Oral: 400 mg 3 times daily for 5 to 14 days (DHHS [adult] 2015)
First infection, severe (independent of HIV status): IV: Children and Adolescents ≥12 years: 5 mg/kg/dose every 8 hours for 5 to 7 days or 5 to 10 mg/kg/dose every 8 hours for 2 to 7 days, followed with oral therapy to complete at least 10 days of therapy (CDC [Workowski 2015]; Red Book [AAP 2015])
Recurrent infection:
Children <12 years (independent of HIV status): Oral: 20 mg/kg/dose 3 times daily for 5 days; maximum dose: 400 mg/dose (Bradley 2015; DHHS [pediatric] 2013)
Children and Adolescents ≥12 years:
Non-HIV-exposed/-positive: Oral: 200 mg every 4 hours while awake (5 times daily) for 5 days, or 400 mg 3 times daily for 5 days, or 800 mg twice daily for 5 days or 800 mg 3 times daily for 2 days (CDC [Workowski 2015]; Red Book [AAP 2015])
HIV-exposed/-positive: Adolescents: Oral: 400 mg 3 times daily for 5 to 14 days (DHHS [adult] 2015)
Suppression, chronic:
Non-HIV-exposed/-positive:
Children <12 years: Limited data available: Oral: 20 mg/kg/dose twice daily; maximum dose: 400 mg/dose (Bradley 2015)
Children and Adolescents ≥12 years: Oral: 400 mg twice daily; reassess therapy after 12 months (CDC [Workowski 2015]; Red Book [AAP 2015])
HIV-exposed/-positive:
Infants and Children: Oral: 20 mg/kg/dose twice daily; maximum dose: 800 mg/dose (DHHS [pediatric] 2013)
Adolescents: Oral: 400 mg twice daily (DHHS [adult] 2015)
HSV gingivostomatitis:
Non-HIV-exposed/-positive: Primary infection:
AAP recommendations: Children and Adolescents: Oral: 20 mg/kg/dose 4 times daily for 5 to 7 days; usual maximum dose: 200 mg/dose, others have reported higher (400 mg/dose) (Bradley 2015; Cernik 2008; Red Book [AAP 2015])
Alternate dosing: Infants ≥10 months, Children, and Adolescents: Oral: 15 mg/kg/dose five times daily for 7 days; maximum dose: 200 mg/dose (Amir 1997; Balfour 1999); dosing based on a placebo controlled trial in children 1 to 6 years of age (n=72, treatment group: n=31); results showed when treatment started within 72 hours of symptom onset a shorter duration of symptoms and viral shedding was observed (Amir 1997)
HIV-exposed/-positive (DHHS [pediatric] 2013):
Mild, symptomatic: Oral: Infants and Children: 20 mg/kg/dose 4 times daily for 7 to 10 days; maximum dose: 400 mg/dose
Moderate to severe, symptomatic: IV: Infants and Children: 5 to 10 mg/kg/dose every 8 hours; switch to oral therapy once lesions begin to regress
HSV, herpes labialis (cold sore) (HIV-exposed/-positive): Treatment:
Infants and Children: Oral: 20 mg/kg/dose 4 times daily for 5 days; maximum dose: 400 mg/dose (DHHS [pediatric] 2013)
Adolescents: Oral: 400 mg 3 times daily for 5 to 10 days (DHHS [adult] 2015)
HSV, herpes labialis (cold sore) recurrent, chronic suppressive therapy: Immunocompetent Children and Adolescents: Oral: 10 mg/kg/dose 3 times daily; maximum daily dose: 1,000 mg/day; reevaluate after 12 months (Red Book [AAP 2015])
HSV mucocutaneous infection:
Immunocompetent host: Infants, Children, and Adolescents:
Treatment (Bradley 2015):
IV: 5 mg/kg/dose every 8 hours
Oral: 20 mg/kg/dose 4 times daily for 5 to 7 days; maximum dose: 800 mg/dose
Suppression, chronic: Limited data available; no pediatric data; some experts recommend oral 20 mg/kg/dose 2 to 3 times daily for 6 to 12 months, then reevaluate need; maximum dose: 400 mg/dose (Bradley 2015)
Immunocompromised host:
Treatment:
IV:
Infants and Children: 10 mg/kg/dose every 8 hours for 7 to 14 days (Red Book [AAP 2015])
Adolescents: 5 to 10 mg/kg/dose every 8 hours; change to oral therapy after lesions begin to regress (DHHS [adult] 2015; Red Book [AAP 2015])
Oral: Children ≥2 years and Adolescents: 1,000 mg/day in 3 to 5 divided doses for 7 to 14 days; some suggest the maximum daily dose should not exceed 80 mg/kg/day (Red Book 2009; Red Book [AAP 2015])
Suppression, chronic (cutaneous, ocular) episodes:
Infants and Children (HIV-exposed/-positive): Oral: 20 mg/kg/dose twice daily; maximum dose: 800 mg/dose; reassess after 12 months (DHHS [pediatric] 2013)
Children 12 years of age (non-HIV-exposed/-positive): Prevention of ocular episodes: Oral: 400 mg twice daily; reassess at 12 months (Red Book [AAP 2015])
Adolescents (independent of HIV status): Oral: 400 mg twice daily; reassess at 12 months (DHHS [adult] 2015; Red Book [AAP 2015])
HSV progressive or disseminated infection, treatment (immunocompromised host):
Non-HIV-exposed/-positive: Infants, Children, and Adolescents: IV: 10 mg/kg/dose every 8 hours for 7 to 14 days (Red Book [AAP 2015])
HIV-exposed/-positive: Infants, Children, and Adolescents: IV: 10 mg/kg/dose every 8 hours for 21 days; higher doses (up to 20 mg/kg/dose) may be used in children <12 years of age (DHHS [pediatric] 2013; Red Book [AAP 2015])
HSV, acute retinal necrosis, treatment (HIV-exposed/-positive): Children (DHHS [pediatric] 2013):
Initial treatment: IV: 10 to 15 mg/kg/dose every 8 hours for 10 to 14 days. Note: Follow up IV therapy with oral acyclovir or valacyclovir maintenance therapy.
Maintenance treatment: Begin after 10- to 14-day course of IV acyclovir: Oral: 20 mg/kg/dose 4 times daily for 4 to 6 weeks
HSV prophylaxis; immunocompromised hosts, seropositive:
Hematopoietic stem cell transplant (HSCT) in seropositive recipient (Tomblyn 2009):
Prevention of early reactivation: Note: Begin at conditioning and continue until engraftment or resolution of mucositis; whichever is longer (~30 days post-HSCT)
Infants, Children, and Adolescents <40 kg:
IV: 250 mg/m2/dose every 8 hours or 125 mg/m2/dose every 6 hours; maximum daily dose: 80 mg/kg/day
Oral: 60 to 90 mg/kg/day in 2 to 3 divided doses; maximum dose: 800 mg/dose twice daily
Children and Adolescents ≥40 kg:
IV: 250 mg/m2/dose every 12 hours
Oral: 400 to 800 mg twice daily
Prevention of late reactivation: Note: Treatment during first year after HSCT.
Infants, Children, and Adolescents <40 kg: Oral: 60 to 90 mg/kg/day in 2 to 3 divided doses; maximum daily dose: 800 mg twice daily
Children and Adolescents ≥40 kg: Oral: 800 mg twice daily
Other immunocompromised hosts who are HSV seropositive:
IV: Infants, Children, and Adolescents: 5 mg/kg/dose every 8 hours during period of risk (Red Book [AAP 2015])
Oral: Children ≥2 years and Adolescents: 200 mg every 4 hours while awake (5 doses daily) or 200 mg every 8 hours; administer during periods of risk (Red Book [AAP 2015])
Varicella (chickenpox) or Herpes zoster (shingles), prophylaxis
Hematopoietic stem cell transplant (HSCT): Prophylaxis of disease reactivation: Note: Continue therapy for 1 year after HSCT (Tomblyn 2009):
Infants, Children, and Adolescents <40 kg: Oral: 60 to 80 mg/kg/day in 2 to 3 divided doses
Children and Adolescents ≥40 kg: Oral: 800 mg twice daily
HIV-exposed/-positive: Limited data available: Note: Consider use if >96 hours postexposure or if VZV-immune globulin is not available; begin therapy 7 to 10 days after exposure; some experts begin therapy at first appearance of rash (DHHS [pediatric] 2013).
Infants and Children: Oral: 20 mg/kg/dose 4 times daily for 7 days; maximum dose: 800 mg/dose (DHHS [pediatric] 2013)
Adolescents: Oral: 800 mg 5 times daily for 5 to 7 days (DHHS [adult] 2015)
Other immunocompromised hosts: Infants, Children, and Adolescents: Oral: 20 mg/kg/dose 4 times daily for 7 days; maximum dose: 800 mg/dose. Note: Consider use if VZV-immune globulin or IVIG is not available; begin therapy 7 to 10 days after exposure (Red Book [AAP] 2015).
Varicella (chickenpox), treatment: Begin treatment within the first 24 hours of rash onset:
Immunocompetent host:
Ambulatory therapy: Oral: Children ≥2 years and Adolescents: 20 mg/kg/dose 4 times daily for 5 days; maximum daily dose: 3,200 mg/day (Red Book [AAP 2015])
Hospitalized patient: IV: Infants, Children, and Adolescents: 10 mg/kg/dose or 500 mg/m2/dose every 8 hours for 7 to 14 days (Bradley 2015; Red Book [AAP 2015]); some experts recommend 15 to 20 mg/kg/dose for severe disseminated or CNS infection (Bradley 2015)
Immunocompromised host (non-HIV-exposed/-positive): IV:
Infants: 10 mg/kg/dose every 8 hours for 7 to 10 days (Red Book [AAP 2015])
Children and Adolescents: 500 mg/m2/dose every 8 hours for 7 to 10 days; some experts recommend 10 mg/kg/dose every 8 hours (Red Book [AAP 2015])
HIV-exposed/-positive:
Mild, uncomplicated disease and no or moderate immune suppression: Oral:
Infants and Children: 20 mg/kg/dose 4 times daily for 7 to 10 days and until no new lesions for 48 hours; maximum dose: 800 mg/dose (DHHS [pediatric] 2013)
Adolescents: 800 mg 5 times daily for 5 to 7 days (DHHS [adult] 2015)
Severe, complicated disease or severe immune suppression: IV:
Infants: 10 mg/kg/dose every 8 hours for 7 to 10 days and until no new lesions for 48 hours (DHHS [pediatric] 2013)
Children: 10 mg/kg/dose or 500 mg/m2/dose every 8 hours for 7 to 10 days or until no new lesions for 48 hours (DHHS [pediatric] 2013)
Adolescents: 10 to 15 mg/kg/dose every 8 hours for 7 to 10 days; may convert to oral therapy after defervescence and if no evidence of visceral involvement is evident (DHHS [adult] 2015)
Dosing: Obesity
IV: In obese patients, acyclovir IV has been dosed using ideal body weight (IBW) to avoid overdosing and subsequent toxicity. However, in a pharmacokinetic study using a single acyclovir IV dose, morbidly obese patients (BMI ≥ 40 kg/m2) dosed using IBW had lower systemic exposures compared to normal weight subjects dosed using actual body weight (exposure based on AUC, Cmax, and T > IC50 [time the drug concentration remains above the 50% inhibitory concentration]) (Turner 2016). Therefore, to avoid potentially underdosing obese patients who are severely ill (eg, HSV encephalitis), some clinicians use adjusted body weight (AjBW) to determine the IV dose (AjBW=IBW + [0.4 x (actual body weight-IBW)]) (Wong 2017), although this approach has not been evaluated in clinical studies.
Reconstitution
Powder for injection: Reconstitute acyclovir 500 mg powder with SWFI 10 mL (final concentration 50 mg/mL); do not use bacteriostatic water containing benzyl alcohol or parabens.
For intravenous infusion, dilute reconstituted powder for injection or solution for injection in D5W or NS to a final concentration ≤7 mg/mL. Concentrations >10 mg/mL increase the risk of phlebitis.
Administration
Oral: Administer with or without food.
IV: Avoid rapid infusion; infuse over 1 hour to prevent renal damage; maintain adequate hydration of patient; check for phlebitis and rotate infusion sites. Do not administer IM or SubQ. Acyclovir IV is an irritant (depending on concentration); avoid extravasation.
Dietary Considerations
Some products may contain sodium.
Storage
Capsule, oral suspension, tablet: Store at controlled room temperature of 15°C to 25°C (59°F to 77°F); protect capsule and tablet from moisture.
Powder for injection: Store undiluted vials at 15°C to 25°C (59°F to 77°F). Following reconstitution (final concentration 50 mg/mL), solution is stable for 12 hours at room temperature.
Solution for injection: Store solution at 20°C to 25°C (68°F to 77°F).
Do not refrigerate reconstituted solutions or solutions diluted for infusion as they may precipitate. Once diluted for infusion with NS or D5W, use within 24 hours.
Acyclovir (Systemic) Images
Drug Interactions
Cladribine: Agents that Undergo Intracellular Phosphorylation may diminish the therapeutic effect of Cladribine. Avoid combination
CloZAPine: CYP1A2 Inhibitors (Weak) may increase the serum concentration of CloZAPine. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Foscarnet: May enhance the nephrotoxic effect of Acyclovir-Valacyclovir. Avoid combination
Mycophenolate: Acyclovir-Valacyclovir may increase the serum concentration of Mycophenolate. Mycophenolate may increase the serum concentration of Acyclovir-Valacyclovir. Monitor therapy
Talimogene Laherparepvec: Antiherpetic Antivirals may diminish the therapeutic effect of Talimogene Laherparepvec. Monitor therapy
Tenofovir Products: Acyclovir-Valacyclovir may increase the serum concentration of Tenofovir Products. Tenofovir Products may increase the serum concentration of Acyclovir-Valacyclovir. Monitor therapy
Theophylline Derivatives: CYP1A2 Inhibitors (Weak) may increase the serum concentration of Theophylline Derivatives. Exceptions: Dyphylline. Monitor therapy
TiZANidine: CYP1A2 Inhibitors (Weak) may increase the serum concentration of TiZANidine. Management: Avoid these combinations when possible. If combined use is necessary, initiate tizanidine at an adult dose of 2 mg and increase in 2 to 4 mg increments based on patient response. Monitor for increased effects of tizanidine, including adverse reactions. Consider therapy modification
Varicella Virus Vaccine: Acyclovir-Valacyclovir may diminish the therapeutic effect of Varicella Virus Vaccine. Management: When possible, avoid use of acyclovir or valacyclovir within the 24 hours prior to administration of the varicella vaccine, and avoid use of these antiviral agents for 14 days after vaccination. Avoid combination
Zidovudine: Acyclovir-Valacyclovir may enhance the CNS depressant effect of Zidovudine. Monitor therapy
Zoster Vaccine (Live/Attenuated): Acyclovir-Valacyclovir may diminish the therapeutic effect of Zoster Vaccine (Live/Attenuated). Management: When possible, discontinue antiviral agents with anti-zoster activity (i.e., acyclovir, valacyclovir, famciclovir) for at least 24 hours prior to and 14 days after receiving a live attenuated zoster vaccine. Avoid combination
Adverse Reactions
As reported with IV administration, unless otherwise noted.
>10%:
Central nervous system: Malaise (oral: 12%)
Hematologic & oncologic: Decrease in absolute neutrophil count (neonates: 3% to 16%), decreased hemoglobin (neonates: 13%)
1% to 10%:
Central nervous system: Headache (oral: ≤2%)
Dermatologic: Pruritus (2%), skin rash (2%), urticaria (2%)
Gastrointestinal: Nausea (oral and IV: ≤7%), vomiting (oral and IV: ≤7%), diarrhea (oral: 2% to 3%; IV: <1%)
Hematologic & oncologic: Thrombocytopenia (neonates: 5% to 10%; children, adolescents, and adults: <1%)
Hepatic: Increased serum bilirubin (neonates, grades 3/4: 4%), increased serum transaminases (1% to 2%)
Local: Inflammation at injection site (≤9%), injection site phlebitis (≤9%)
Renal: Increased blood urea nitrogen (5% to 10%), increased serum creatinine (5% to 10%)
<1%, postmarketing, and/or case reports (all routes): Abdominal pain, aggressive behavior, agitation, alopecia, anaphylaxis, anemia, angioedema, anorexia, ataxia, coma, confusion, delirium, disseminated intravascular coagulation, dizziness, drowsiness, dysarthria, encephalopathy, erythema multiforme, fatigue, fever, gastrointestinal distress, hallucination, hematuria, hemolysis, hepatitis, hyperbilirubinemia, hypersensitivity angiitis, hypotension, impaired consciousness, increased liver enzymes, jaundice, leukocytosis, leukopenia, lymphadenopathy, myalgia, neutropenia, neutrophilia, obtundation, pain, paresthesia, peripheral edema, psychosis, renal failure syndrome, renal pain, seizure, skin photosensitivity, Stevens-Johnson syndrome, thrombocythemia, toxic epidermal necrolysis, tremor, visual disturbance
Warnings/Precautions
Concerns related to adverse effects:
- CNS effects: Neurotoxicity (eg, tremor/myoclonus, confusion, agitation, lethargy, hallucination, impaired consciousness) has been reported; risk may be increased with higher doses and in patients with renal failure. Monitor patients for signs/symptoms of neurotoxicity; ensure appropriate dosage reductions in patients with renal impairment (Chowdhury 2016).
- Extravasation: Acyclovir IV is an irritant (depending on concentration); avoid extravasation.
- Renal effects: Renal failure (sometimes fatal) has been reported. Dehydration, preexisting renal disease, and nephrotoxic drugs increase risk; ensure patient is adequately hydrated during oral or IV therapy.
- Thrombotic microangiopathy: Has been reported in immunocompromised patients receiving acyclovir.
Disease-related concerns:
- Renal impairment: Use with caution; dosage adjustment recommended. Neurotoxicity may be more common in patients with renal impairment (Chowdhury 2016).
- Varicella: Appropriate use: For maximum benefit, treatment should begin within 24 hours of appearance of rash; oral route not recommended for routine use in otherwise healthy children with varicella but may be effective in patients at increased risk of moderate-to-severe infection (>12 years of age, chronic cutaneous or pulmonary disorders, long-term salicylate therapy, corticosteroid therapy).
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Dosage form specific issues:
- Injection: Use IV preparation with caution in patients with underlying neurologic abnormalities, serious hepatic or electrolyte abnormalities, or substantial hypoxia. Encephalopathic changes characterized by lethargy, obtundation, confusion, hallucination, tremors, agitation, seizure, or coma have been observed in patients receiving IV acyclovir.
Other warnings/precautions:
- Adequate hydration: Maintain adequate hydration during oral or IV therapy.
Monitoring Parameters
Urinalysis, BUN, serum creatinine, urine output; liver enzymes, CBC; monitor for neurotoxicity and nephrotoxicity in pediatric patients when using high dose therapy; neutrophil count at least twice weekly in neonates receiving acyclovir 60 mg/kg/day IV. Monitor infusion site.
Pregnancy
Pregnancy Considerations
Acyclovir has been shown to cross the human placenta (Henderson 1992).
Results from a pregnancy registry, established in 1984 and closed in 1999, did not find an increase in the number of birth defects with exposure to acyclovir when compared to those expected in the general population. However, due to the small size of the registry and lack of long-term data, the manufacturer recommends using during pregnancy with caution and only when clearly needed. Acyclovir is recommended for the treatment of genital herpes in pregnant patients (ACOG 2007; CDC [Workowski 2015]).
Patient Education
What is this drug used for?
- It is used to treat herpes infections.
- It is used to treat shingles.
- It is used to treat chickenpox.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Nausea
- Vomiting
- Loss of strength and energy
- Injection site irritation
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Behavioral changes
- Mood changes
- Confusion
- Sensing things that seem real but are not
- Seizures
- Tremors
- Kidney problems like unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain.
- Thrombotic thrombocytopenic purpura/hemolytic uremic syndrome like bruising or bleeding; severe loss of strength and energy; dark urine or yellow skin; pale skin; change in the amount of urine passed; vision changes; change in strength on one side is greater than the other; difficulty speaking or thinking; change in balance; or fever.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.