Boxed Warning
Fetal toxicity
When pregnancy is detected, discontinue aliskiren as soon as possible. Drugs that act directly on the renin-angiotensin system can cause injury and even death to the developing fetus.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral:
Tekturna: 150 mg, 300 mg
Generic: 150 mg, 300 mg
Pharmacology
Mechanism of Action
Decreases plasma renin activity and inhibits conversion of angiotensinogen to angiotensin I.
Pharmacokinetics/Pharmacodynamics
Absorption
Poor; absorption decreased by high-fat meal. Aliskiren is a substrate of P-glycoprotein; concurrent use of P-glycoprotein inhibitors may increase absorption.
Metabolism
Extent of metabolism unknown; in vitro studies indicate metabolism via CYP3A4
Excretion
Urine (~25% of absorbed dose excreted unchanged in urine); feces (unchanged via biliary excretion)
Onset of Action
Maximum antihypertensive effect: Within 2 weeks
Time to Peak
1 to 3 hours
Half-Life Elimination
~24 hours (range: 16 to 32 hours)
Use in Specific Populations
Special Populations: Elderly
AUC is increased in patients ≥65 years.
Use: Labeled Indications
Hypertension: Management of hypertension in adults and pediatric patients ≥6 years of age
Note: Not recommended for the initial treatment of hypertension (ACC/AHA [Whelton 2017]).
Contraindications
Hypersensitivity to aliskiren or any component of the formulation; concomitant use with an ACE inhibitor or ARB in patients with diabetes; children <2 years of age
Canadian labeling: Additional contraindications (not in US labeling): History of angioedema with aliskiren, ACE inhibitors, or ARBs; hereditary or idiopathic angioedema; pregnancy, breastfeeding; concomitant use with ACE inhibitors or ARBs in patients with GFR <60 mL/minute/1.73 m2
Dosage and Administration
Dosing: Adult
Hypertension (alternative agent): Initial: 150 mg once daily; may increase to 300 mg once daily (maximum: 300 mg/day) (ACC/AHA [Whelton 2017]).
Dosing: Geriatric
Refer to adult dosing. No initial dosage adjustment required.
Dosing: Pediatric
Note: Prior to initiation, correct hypovolemia and/or closely monitor volume status in patients on concurrent diuretics during treatment initiation.
Hypertension: Children ≥6 years of age weighing ≥20 kg and Adolescents: Oral: Oral tablets or pellets (if unable to swallow tablets):
20 kg to 50 kg: Initial: 75 mg once daily; if blood pressure not adequately controlled, may increase to 150 mg once daily; maximum daily dose: 150 mg/day
≥50 kg: Initial: 150 mg once daily; if blood pressure not adequately controlled, may increase to 300 mg once daily; maximum daily dose: 300 mg/day
Administration
Oral: Administer at the same time daily with or without a meal, but consistent administration with regards to meals is recommended; high-fat meal reduces absorption.
Oral pellets: For patients unable to swallow tablets, administer oral pellets by opening the dispensing capsule, emptying the entire contents onto a spoon, swallowing, and then following with milk (dairy or soy-based) or water immediately without chewing or crushing. Alternatively, may open the dispensing capsule and mix with ≥1 teaspoons of only vanilla pudding (milk or soy-based), vanilla ice cream (milk or soy-based), milk (dairy or soy-based), or water. Do not swallow the capsules or empty the contents of the capsule directly into the mouth. Do not chew or crush the capsule.
Storage
Store at 20°C to 25°C (68°F to 77°F); excursions are permitted to 15°C to 30°C (59°F to 86°F). Protect from moisture. Dispense blisters in the original container.
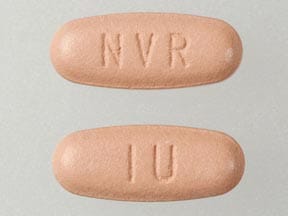
Aliskiren Images
Drug Interactions
Alfuzosin: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Amifostine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Amifostine. Management: When amifostine is used at chemotherapy doses, blood pressure lowering medications should be withheld for 24 hours prior to amifostine administration. If blood pressure lowering therapy cannot be withheld, amifostine should not be administered. Consider therapy modification
Amphetamines: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Angiotensin II Receptor Blockers: Aliskiren may enhance the hyperkalemic effect of Angiotensin II Receptor Blockers. Aliskiren may enhance the hypotensive effect of Angiotensin II Receptor Blockers. Aliskiren may enhance the nephrotoxic effect of Angiotensin II Receptor Blockers. Management: Aliskiren use with ACEIs or ARBs in patients with diabetes is contraindicated. Combined use in other patients should be avoided, particularly when CrCl is less than 60 mL/min. If combined, monitor potassium, creatinine, and blood pressure closely. Consider therapy modification
Angiotensin-Converting Enzyme Inhibitors: Aliskiren may enhance the hyperkalemic effect of Angiotensin-Converting Enzyme Inhibitors. Aliskiren may enhance the hypotensive effect of Angiotensin-Converting Enzyme Inhibitors. Aliskiren may enhance the nephrotoxic effect of Angiotensin-Converting Enzyme Inhibitors. Management: Aliskiren use with ACEIs or ARBs in patients with diabetes is contraindicated. Combined use in other patients should be avoided, particularly when CrCl is less than 60 mL/min. If combined, monitor potassium, creatinine, and blood pressure closely. Consider therapy modification
Antipsychotic Agents (Second Generation [Atypical]): Blood Pressure Lowering Agents may enhance the hypotensive effect of Antipsychotic Agents (Second Generation [Atypical]). Monitor therapy
AtorvaSTATin: May increase the serum concentration of Aliskiren. Monitor therapy
Barbiturates: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Benperidol: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Brigatinib: May diminish the antihypertensive effect of Antihypertensive Agents. Brigatinib may enhance the bradycardic effect of Antihypertensive Agents. Monitor therapy
Brimonidine (Topical): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Bromperidol: Blood Pressure Lowering Agents may enhance the hypotensive effect of Bromperidol. Bromperidol may diminish the hypotensive effect of Blood Pressure Lowering Agents. Avoid combination
CycloSPORINE (Systemic): May increase the serum concentration of Aliskiren. Avoid combination
Dexmethylphenidate: May diminish the therapeutic effect of Antihypertensive Agents. Monitor therapy
Diazoxide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Drospirenone: May enhance the hyperkalemic effect of Aliskiren. Monitor therapy
DULoxetine: Blood Pressure Lowering Agents may enhance the hypotensive effect of DULoxetine. Monitor therapy
Erdafitinib: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Furosemide: Aliskiren may decrease the serum concentration of Furosemide. Monitor therapy
Grapefruit Juice: May decrease the serum concentration of Aliskiren. Management: Avoid concomitant use of aliskiren and grapefruit juice. Separation of aliskiren and grapefruit juice administration by several hours may reduce the chance for interaction. Monitor for decreased aliskiren levels/effects. Consider therapy modification
Heparin: May enhance the hyperkalemic effect of Aliskiren. Monitor therapy
Heparins (Low Molecular Weight): May enhance the hyperkalemic effect of Aliskiren. Monitor therapy
Herbs (Hypertensive Properties): May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Herbs (Hypotensive Properties): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Hypotension-Associated Agents: Blood Pressure Lowering Agents may enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Itraconazole: May increase the serum concentration of Aliskiren. Avoid combination
Ketoconazole (Systemic): May increase the serum concentration of Aliskiren. Monitor therapy
Lasmiditan: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Avoid combination
Levodopa-Containing Products: Blood Pressure Lowering Agents may enhance the hypotensive effect of Levodopa-Containing Products. Monitor therapy
Lormetazepam: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Lumacaftor and Ivacaftor: May decrease the serum concentration of P-glycoprotein/ABCB1 Substrates. Lumacaftor and Ivacaftor may increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Methylphenidate: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Molsidomine: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Naftopidil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicergoline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicorandil: May enhance the hyperkalemic effect of Aliskiren. Monitor therapy
Nitroprusside: Blood Pressure Lowering Agents may enhance the hypotensive effect of Nitroprusside. Monitor therapy
Nonsteroidal Anti-Inflammatory Agents: May diminish the antihypertensive effect of Aliskiren. Nonsteroidal Anti-Inflammatory Agents may enhance the nephrotoxic effect of Aliskiren. Management: Monitor renal function periodically in patients receiving aliskiren and any nonsteroidal anti-inflammatory agent. Patients at elevated risk of renal dysfunction include those who are elderly, are volume depleted, or have pre-existing renal dysfunction. Monitor therapy
Obinutuzumab: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Management: Consider temporarily withholding blood pressure lowering medications beginning 12 hours prior to obinutuzumab infusion and continuing until 1 hour after the end of the infusion. Consider therapy modification
Pentoxifylline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
P-glycoprotein/ABCB1 Inducers: May decrease the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inducers may also further limit the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Monitor therapy
P-glycoprotein/ABCB1 Inhibitors: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inhibitors may also enhance the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Monitor therapy
Pholcodine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Pholcodine. Monitor therapy
Phosphodiesterase 5 Inhibitors: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Potassium Salts: May enhance the hyperkalemic effect of Aliskiren. Monitor therapy
Prostacyclin Analogues: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Quinagolide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Ranolazine: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Verapamil: May increase the serum concentration of Aliskiren. Monitor therapy
Yohimbine: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Test Interactions
May lead to false-positive or false-negative aldosterone/renin ratio (ARR) (Funder 2016)
Adverse Reactions
1% to 10%:
Dermatologic: Skin rash (1%)
Gastrointestinal: Diarrhea (2%)
Neuromuscular & skeletal: Increased creatine phosphokinase (>300% increase: 1%)
Renal: Increased blood urea nitrogen (≤7%), increased serum creatinine (≤7%)
Respiratory: Cough (1%)
<1%, postmarketing, and/or case reports: Abdominal pain, anaphylaxis, anemia, angioedema, decreased hematocrit, decreased hemoglobin, dyspepsia, erythema, gastroesophageal reflux disease, gout, hepatic insufficiency, hyperkalemia, hyponatremia, increased liver enzymes, increased uric acid, myositis, nausea, nephrolithiasis, periorbital edema, peripheral edema, pruritus, rhabdomyolysis, seizure, severe hypotension, Stevens-Johnson syndrome, tonic-clonic seizures, toxic epidermal necrolysis, urticaria, vomiting
Warnings/Precautions
Concerns related to adverse effects:
- Hyperkalemia: May occur; risk increased in patients with renal impairment or diabetes, or concomitant use with ACE inhibitors, ARBs, NSAIDs, potassium-sparing diuretics, potassium supplements, and/or potassium-containing salts.
- Hypersensitivity: Anaphylaxis and angioedema have been reported. Since the effect of aliskiren on bradykinin levels is unknown, the risk of kinin-mediated etiologies of angioedema occurring is also unknown. Use with caution in any patient with a history of angioedema (of any etiology) as angioedema, some cases necessitating hospitalization and intubation, has been observed with aliskiren use. Discontinue immediately following the occurrence of anaphylaxis or angioedema; do not readminister. Prolonged frequent monitoring may be required especially if tongue, glottis, or larynx are involved as they are associated with airway obstruction. Patients with a history of airway surgery may have a higher risk of airway obstruction. Early, aggressive, and appropriate management is critical.
- Hypotension: During the initiation of therapy, symptomatic hypotension may occur, particularly in volume or salt-depleted patients or with concomitant use of other agents acting on the renin-angiotensin-aldosterone system. Prior to initiation, correct hypovolemia or salt depletion, or closely monitor during treatment initiation. If hypotension does occur, this is not a contraindication for further use; once blood pressure has been stabilized, aliskiren usually can be continued without difficulty.
- Renal effects: Changes in renal function, including acute renal failure, may occur; risk is increased in patients with renal artery stenosis, severe heart failure, post-myocardial infarction, volume depletion, or patients receiving ARB, ACEI or NSAIDs. Consider withholding or discontinuing therapy in patients who develop a clinically significant decrease in renal function.
Disease-related concerns:
- Diabetes: Use in patients with diabetes has demonstrated an increased incidence of renal impairment, hypotension, and hyperkalemia; use is contraindicated in patients with diabetes who are taking an ACE inhibitor or ARB.
- Renal impairment: Use with caution in patients with renal impairment; risk of developing acute renal failure and hyperkalemia is increased. Avoid concomitant use with an ACE inhibitor or ARB in patients with CrCl <60 mL/minute.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Pregnancy: [US Boxed Warning]: Drugs that act on the renin-angiotensin system can cause injury and death to the developing fetus. Discontinue as soon as possible once pregnancy is detected.
Monitoring Parameters
Blood pressure; serum potassium, BUN, serum creatinine
The 2017 Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults (ACC/AHA [Whelton 2017]):
Confirmed hypertension and known CVD or 10-year ASCVD risk ≥10%: Target blood pressure <130/80 mm Hg is recommended
Confirmed hypertension without markers of increased ASCVD risk: Target blood pressure <130/80 mm Hg may be reasonable
Pregnancy
Pregnancy Considerations
[US Boxed Warning]: Drugs that act on the renin-angiotensin system can cause injury and death to the developing fetus. Discontinue as soon as possible once pregnancy is detected. The use of drugs which act on the renin-angiotensin system are associated with oligohydramnios. Oligohydramnios, due to decreased fetal renal function, may lead to fetal lung hypoplasia and skeletal malformations. Use is also associated with anuria, hypotension, renal failure, skull hypoplasia, and death in the fetus/neonate. The exposed fetus should be monitored for fetal growth, amniotic fluid volume, and organ formation. Infants exposed in utero should be monitored for hyperkalemia, hypotension, and oliguria.
Patient Education
What is this drug used for?
- It is used to treat high blood pressure.
Frequently reported side effects of this drug
- Diarrhea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Kidney problems like unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain.
- High potassium like abnormal heartbeat, confusion, dizziness, passing out, weakness, shortness of breath, numbness or tingling feeling.
- Low sodium like headache, trouble focusing, trouble with memory, confusion, weakness, seizures, or change in balance.
- Dizziness
- Passing out
- Abdominal pain
- Vomiting
- Trouble swallowing
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.