Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
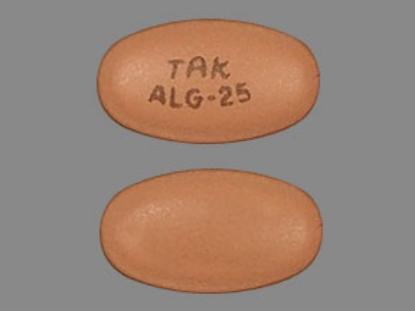
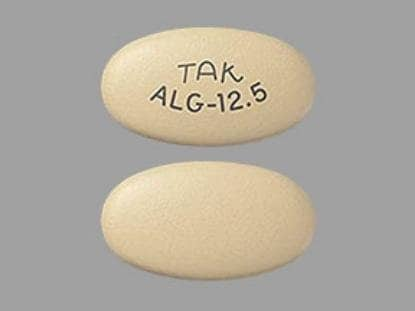
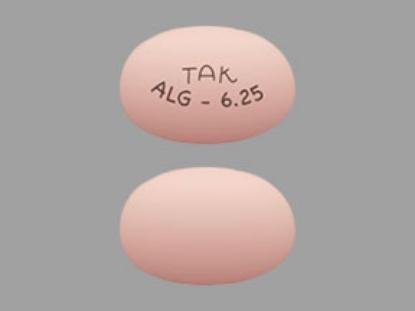
Tablet, Oral:
Nesina: 6.25 mg, 12.5 mg, 25 mg
Generic: 6.25 mg, 12.5 mg, 25 mg
Pharmacology
Mechanism of Action
Alogliptin inhibits dipeptidyl peptidase 4 (DPP-4) enzyme resulting in prolonged active incretin levels. Incretin hormones (eg, glucagon-like peptide-1 [GLP-1] and glucose-dependent insulinotropic polypeptide [GIP]) regulate glucose homeostasis by increasing insulin synthesis and release from pancreatic beta cells and decreasing glucagon secretion from pancreatic alpha cells. Decreased glucagon secretion results in decreased hepatic glucose production. Under normal physiologic circumstances, incretin hormones are released by the intestine throughout the day and levels are increased in response to a meal; incretin hormones are rapidly inactivated by the DPP-4 enzyme.
Pharmacokinetics/Pharmacodynamics
Absorption
Extensive (~100%) regardless of food intake
Distribution
417 L
Metabolism
Not extensively metabolized; minor metabolism via CYP2D6 and CYP3A4 suggested by in vitro studies (<7% of parent compound is transformed to active and inactive metabolites)
Excretion
Urine 76% (60% to 71% as unchanged drug); feces 13%
Time to Peak
~1 to 2 hours
Half-Life Elimination
~21 hours
Protein Binding
20%
Use in Specific Populations
Special Populations: Renal Function Impairment
AUC increased two-, three-, and four-fold in patients with moderate renal impairment, severe renal impairment, and end-stage renal disease, respectively.
Use: Labeled Indications
Diabetes mellitus, type 2: Management of adults with type 2 diabetes mellitus as an adjunct to diet and exercise as monotherapy or in combination therapy
Contraindications
History of serious hypersensitivity (eg, anaphylaxis, angioedema, severe cutaneous reactions) to alogliptin or any component of the formulation
Dosage and Administration
Dosing: Adult
Diabetes mellitus, type 2: Oral: 25 mg once daily
Concomitant use with insulin and/or insulin secretagogues (eg, sulfonylureas): Reduced dose of insulin and/or insulin secretagogues may be needed.
Dosing: Geriatric
Refer to adult dosing.
Administration
May be taken with or without food.
Dietary Considerations
Individualized medical nutrition therapy (MNT) based on ADA recommendations is an integral part of therapy.
Storage
Store at 25°C (77°F); excursions permitted between 15°C to 30°C (59°F to 86°F).
Alogliptin Images
Drug Interactions
Alpha-Lipoic Acid: May enhance the hypoglycemic effect of Antidiabetic Agents. Monitor therapy
Androgens: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Exceptions: Danazol. Monitor therapy
Angiotensin-Converting Enzyme Inhibitors: Dipeptidyl Peptidase-IV Inhibitors may enhance the adverse/toxic effect of Angiotensin-Converting Enzyme Inhibitors. Specifically, the risk of angioedema may be increased. Monitor therapy
Direct Acting Antiviral Agents (HCV): May enhance the hypoglycemic effect of Antidiabetic Agents. Monitor therapy
Guanethidine: May enhance the hypoglycemic effect of Antidiabetic Agents. Monitor therapy
Hyperglycemia-Associated Agents: May diminish the therapeutic effect of Antidiabetic Agents. Monitor therapy
Hypoglycemia-Associated Agents: Antidiabetic Agents may enhance the hypoglycemic effect of Hypoglycemia-Associated Agents. Monitor therapy
Insulins: Dipeptidyl Peptidase-IV Inhibitors may enhance the hypoglycemic effect of Insulins. Management: Consider a decrease in insulin dose when initiating therapy with a dipeptidyl peptidase-IV inhibitor and monitor patients for hypoglycemia. Consider therapy modification
Maitake: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Monoamine Oxidase Inhibitors: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Pegvisomant: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Prothionamide: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Quinolones: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Quinolones may diminish the therapeutic effect of Blood Glucose Lowering Agents. Specifically, if an agent is being used to treat diabetes, loss of blood sugar control may occur with quinolone use. Monitor therapy
Ritodrine: May diminish the therapeutic effect of Antidiabetic Agents. Monitor therapy
Salicylates: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Selective Serotonin Reuptake Inhibitors: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Sulfonylureas: Dipeptidyl Peptidase-IV Inhibitors may enhance the hypoglycemic effect of Sulfonylureas. Management: Consider a decrease in sulfonylurea dose when initiating therapy with a dipeptidyl peptidase-IV inhibitor and monitor patients for hypoglycemia. Consider therapy modification
Thiazide and Thiazide-Like Diuretics: May diminish the therapeutic effect of Antidiabetic Agents. Monitor therapy
Adverse Reactions
1% to 10%:
Central nervous system: Headache (4%)
Renal: Renal function abnormality (3%), decreased creatinine clearance (2%)
Respiratory: Nasopharyngitis (5%), upper respiratory tract infection (5%)
<1%, postmarketing, and/or case reports: Acute pancreatitis, anaphylaxis, angioedema, bullous pemphigoid, constipation, diarrhea, hepatic failure, hypersensitivity reaction, increased liver enzymes, intestinal obstruction, nausea, rhabdomyolysis, severe arthralgia, severe dermatological reaction, skin rash, Stevens-Johnson syndrome, urticaria
Warnings/Precautions
Concerns related to adverse effects:
- Arthralgia: Severe and disabling arthralgia has been reported with DPP-4 inhibitor use; onset may occur within one day to years after treatment initiation and may resolve with discontinuation of therapy. Some patients may experience a recurrence of symptoms if DPP-4 inhibitor therapy resumed. Discontinue use if severe joint pain results from DPP-4 inhibitor therapy.
- Bullous pemphigoid: DPP-4 inhibitor use has been associated with development of bullous pemphigoid; cases have typically resolved with topical or systemic immunosuppressive therapy and discontinuation of DPP-4 inhibitor therapy. Advise patients to report development of blisters or erosions. Discontinue therapy if bullous pemphigoid is suspected and consider referral to a dermatologist.
- Hepatotoxicity: Cases of fatal and nonfatal hepatic failure have been reported in postmarketing surveillance. Baseline liver function tests (serum transaminases) are recommended to rule out underlying liver diseases. Use with caution in patients with abnormal serum transaminases. Monitor and promptly evaluate serum transaminase levels in patients with symptoms of hepatic injury (eg, fatigue, anorexia, jaundice, dark urine, and/or abdominal pain). In patients with clinically significant transaminase elevations and/or persistent or worsening elevations, alogliptin therapy should be interrupted. Therapy should only be resumed with caution in patients where an alternative cause of transaminase elevations has been determined.
- Hypersensitivity reactions: Rare hypersensitivity reactions, including anaphylaxis, angioedema, and/or severe dermatologic reactions such as Stevens-Johnson syndrome, have been reported in postmarketing surveillance; discontinue if signs/symptoms of hypersensitivity reactions occur. Use with caution if patient has experienced angioedema with other DPP-4 inhibitor use.
- Pancreatitis: Cases of acute pancreatitis have been reported with use. Monitor for signs/symptoms of pancreatitis; discontinue use immediately if pancreatitis is suspected and initiate appropriate management. Use with caution in patients with a history of pancreatitis as it is not known if this population is at greater risk.
Disease-related concerns:
- Bariatric surgery:
– Altered absorption: Absorption may be altered given the anatomic and transit changes created by gastric bypass and sleeve gastrectomy surgery (Mechanick 2013; Melissas 2013).
– Glucagon-like peptide-1 exposure and therapeutic efficacy: Closely monitor for signs and symptoms of pancreatitis; gastric bypass and sleeve gastrectomy may increase endogenous secretion of glucagon-like peptide-1 (Korner 2009; Peterli 2012). A single-dose, placebo-controlled study evaluated short-term therapy (4 weeks) with sitagliptin in gastric bypass patients having persistent or recurrent type 2 diabetes and found it to be well tolerated and provided a small but significant reduction in postprandial blood glucose (Shah 2018).
- Heart failure: In a multi-center, randomized, double-blind, placebo-controlled cardiovascular outcome trial of patients with type 2 diabetes and recent acute coronary syndrome, the overall incidence of hospitalization for heart failure (HF) was slightly greater in the alogliptin arm compared to placebo (3.9% vs 3.3%), but this difference was not statistically significant. In patients without a history of HF, the incidence of hospitalization for HF was greater with alogliptin than placebo (2.2% vs 1.3%), a difference that reached statistical significance. (Zannad 2015). The ADA suggests DPP-4 inhibitors (except saxagliptin) may be considered in patients with HF (ADA 2019).
- Hepatic impairment: Use with caution in patients with hepatic dysfunction.
- Renal impairment: Use with caution in patients with moderate-to-severe renal dysfunction and end-stage renal disease (ESRD) requiring hemodialysis; dosing adjustment required.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Other warnings/precautions:
- Appropriate use: Not indicated for use in patients with type 1 diabetes mellitus or with diabetic ketoacidosis (DKA).
- Patient education: Diabetes self-management education (DSME) is essential to maximize the effectiveness of therapy.
Monitoring Parameters
HbA1c (at least twice yearly in patients who have stable glycemic control and are meeting treatment goals; quarterly in patients not meeting treatment goals or with therapy change [ADA 2019]), serum glucose; renal function prior to initiation and periodically during treatment; baseline liver function tests and then as clinically indicated; signs/symptoms of pancreatitis; signs/symptoms of heart failure
Pregnancy
Pregnancy Considerations
Poorly controlled diabetes during pregnancy can be associated with an increased risk of adverse maternal and fetal outcomes, including diabetic ketoacidosis, preeclampsia, spontaneous abortion, preterm delivery, delivery complications, major birth defects, stillbirth, and macrosomia (ACOG 201 2018). To prevent adverse outcomes, prior to conception and throughout pregnancy, maternal blood glucose and HbA1c should be kept as close to target goals as possible but without causing significant hypoglycemia (ADA 2020; Blumer 2013).
Agents other than alogliptin are currently recommended to treat diabetes mellitus in pregnancy (ADA 2020).
Patient Education
What is this drug used for?
- It is used to lower blood sugar in patients with high blood sugar (diabetes).
Frequently reported side effects of this drug
- Common cold symptoms
- Sore throat
- Stuffy nose
- Runny nose
- Headache
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Severe joint pain
- Persistent joint pain
- Skin blisters
- Skin breakdown
- Heart problems like cough or shortness of breath that is new or worse, swelling of the ankles or legs, abnormal heartbeat, weight gain of more than five pounds in 24 hours, dizziness, or passing out
- Low blood sugar like dizziness, headache, fatigue, feeling weak, shaking, a fast heartbeat, confusion, hunger, or sweating
- Pancreatitis like severe abdominal pain, severe back pain, severe nausea, or vomiting
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.