Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
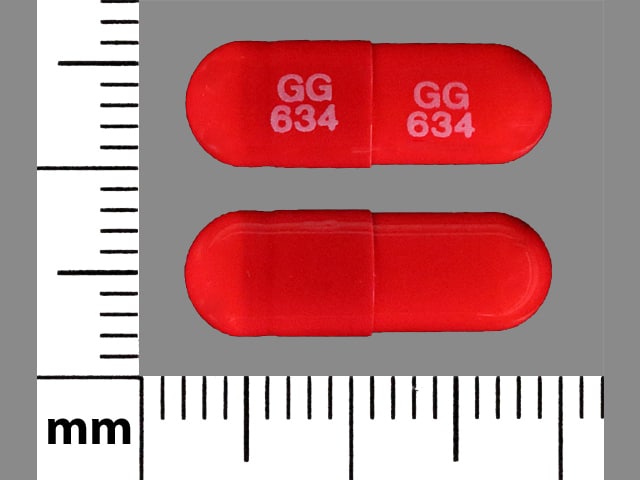
Capsule, Oral, as hydrochloride:
Generic: 100 mg
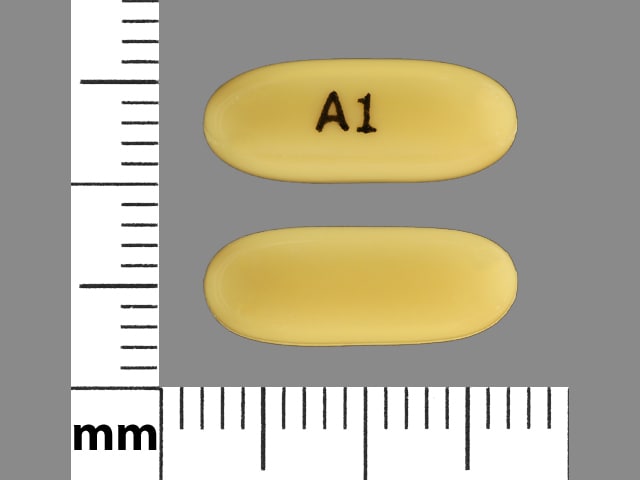
Capsule Extended Release 24 Hour, Oral, as hydrochloride [strength expressed as base]:
Gocovri: 68.5 mg, 137 mg
Syrup, Oral, as hydrochloride:
Generic: 50 mg/5 mL (10 mL, 473 mL)
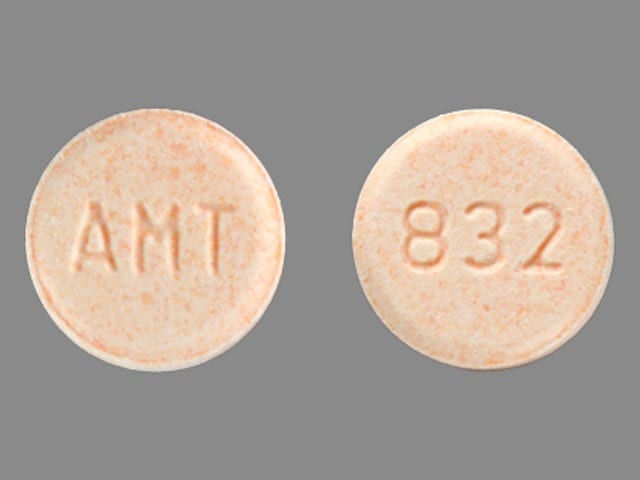
Tablet, Oral, as hydrochloride:
Generic: 100 mg
Tablet Extended Release 24 Hour, Oral, as hydrochloride [strength expressed as base]:
Osmolex ER: 129 mg [contains fd&c yellow #10 (quinoline yellow), fd&c yellow #6 (sunset yellow)]
Osmolex ER: 193 mg [contains fd&c blue #2 (indigotine), fd&c red #40, fd&c yellow #10 (quinoline yellow), fd&c yellow #6 (sunset yellow)]
Osmolex ER: 258 mg [contains brilliant blue fcf (fd&c blue #1), fd&c red #40, fd&c yellow #10 (quinoline yellow), fd&c yellow #6 (sunset yellow)]
Pharmacology
Mechanism of Action
Antiviral:
The mechanism of amantadine’s antiviral activity has not been fully elucidated. It appears to primarily prevent the release of infectious viral nucleic acid into the host cell by interfering with the transmembrane domain of the viral M2 protein. Amantadine is also known to prevent viral assembly during replication. Amantadine inhibits the replication of influenza A virus isolates from each of the subtypes (ie, H1N1, H2N2 and H3N2), but has very little or no activity against influenza B virus isolates.
Parkinson disease:
The exact mechanism of amantadine in the treatment of Parkinson disease and drug-induced extrapyramidal symptoms is not known. Data from early animal studies suggest that amantadine may have direct and indirect effects on dopamine neurons; however, recent studies have demonstrated that amantadine is a weak, noncompetitive NMDA receptor antagonist. Although amantadine has not been shown to possess direct anticholinergic activity, clinically, it exhibits anticholinergic-like side effects (dry mouth, urinary retention, and constipation).
Pharmacokinetics/Pharmacodynamics
Absorption
Well absorbed
Distribution
Vd: Normal: 3 to 8 L/kg; Renal failure: 5.1 ± 0.2 L/kg (Aoki 1988)
Metabolism
Not appreciable; small amounts of an acetyl metabolite identified
Excretion
Urine (80% to 90% unchanged) by glomerular filtration and tubular secretion
Onset of Action
Antidyskinetic: Within 48 hours
Time to Peak
Plasma: Extended-release capsule: 12 hours (mean; range: 6 to 20 hours); extended-release tablet: 7.5 hours (median; range: 5.5 to 12 hours); immediate release: 2 to 4 hours
Half-Life Elimination
Normal renal function: 16 ± 6 hours (9 to 31 hours); Healthy, older (≥60 years) males: 29 hours (range: 20 to 41 hours) (Aoki 1988); End-stage renal disease: 8 days
Protein Binding
Normal renal function: ~67%; Hemodialysis: ~59% (Aoki 1988)
Use in Specific Populations
Special Populations: Renal Function Impairment
Elimination half-life is increased 2- to 3-fold or greater when CrCl is less than 40 mL/minute/1.73 m2.
Special Populations: Elderly
Clearance is reduced.
Use: Labeled Indications
Drug-induced extrapyramidal symptoms (immediate release and extended-release tablet only): Treatment of drug-induced extrapyramidal symptoms.
Influenza A: Note: Due to high resistance rates, amantadine is no longer recommended for the treatment or prophylaxis of influenza A (CDC 2018; IDSA [Uyeki 2019]). Please refer to the current CDC recommendations.
Prophylaxis (immediate release only): Chemoprophylaxis against signs and symptoms of influenza A virus infection.
Treatment (immediate release only): Treatment of uncomplicated respiratory tract illness caused by influenza A virus strains.
Parkinson disease:
Extended release:
Capsule: Treatment of dyskinesia in patients with Parkinson disease receiving levodopa-based therapy, with or without concomitant dopaminergic medications.
Tablet: Treatment of Parkinson disease.
Immediate release: Treatment of idiopathic Parkinson disease (paralysis agitans), postencephalitic parkinsonism, parkinsonism in association with cerebral arteriosclerosis, and symptomatic parkinsonism, which may follow injury to the nervous system by carbon monoxide intoxication.
Use: Off Label
Chorea of Huntington diseasecyes
Data from a limited number of clinical trials suggest that amantadine may be beneficial for the treatment of chorea of Huntington disease. Additional data may be necessary to further define the role of amantadine in this condition O'Suilleabhain 2003, Verhagen 2002.
Based on the
Multiple sclerosis-related fatiguecyes
In a meta-analysis of trials evaluating the treatment of multiple sclerosis-related fatigue, the use of amantadine demonstrated variable results; nonpharmacological rehabilitation interventions were superior Asano 2014.
Based on the
Restless legs syndromec
Data from a limited number of patients in a noncontrolled trial suggest that amantadine may be beneficial for the treatment of restless legs syndrome Evidente 2000. Additional data may be necessary to further define the role of amantadine in this condition.
Based on the
Traumatic brain injurycyes
Data from a limited number of clinical trials suggest that amantadine may be beneficial for the treatment of neurobehavioral sequelae of traumatic brain injury Giacino 2012, Hammond 2014. Additional data may be necessary to further define the role of amantadine in this condition.
Based on the
Contraindications
Hypersensitivity to amantadine or any component of the formulation; end-stage renal disease (CrCl <15 mL/minute/1.73 m2) (extended release only).
Dosage and Administration
Dosing: Adult
Influenza A treatment/prophylaxis: Note: Due to high resistance rates, amantadine is no longer recommended for the treatment or prophylaxis of influenza A (CDC 2018; IDSA [Uyeki 2019]). Please refer to the current CDC recommendations.
Influenza A treatment: Immediate release: Oral: 200 mg once daily or 100 mg twice daily (may be preferred to reduce CNS effects); Note: Initiate within 24 to 48 hours after onset of symptoms; continue for 24 to 48 hours after symptom resolution (duration of therapy is generally 5 days [CDC/ACIP 2011]).
Influenza A prophylaxis: Immediate release: Oral: 200 mg once daily or 100 mg twice daily (may be preferred to reduce CNS effects). Note: Continue prophylaxis throughout the peak influenza activity in the community or throughout the entire influenza season in patients who cannot be vaccinated. Development of immunity following vaccination takes ~2 weeks; amantadine therapy should be considered for high-risk patients from the time of vaccination until immunity has developed.
Drug-induced extrapyramidal symptoms:
Extended-release tablet: Oral: Initial: 129 mg once daily; may be increased in weekly intervals to a maximum dose of 322 mg/day.
Immediate release: Oral: 100 mg twice daily; may increase to 300 mg/day in divided doses, if needed
Parkinson disease:
Extended release:
Capsule (monotherapy or as an adjunct to dopaminergic medications): Oral: Initial: 137 mg once daily; after 1 week, increase to usual dose of 274 mg once daily.
Tablet: Oral: Initial: 129 mg once daily; may be increased in weekly intervals to a maximum dose of 322 mg/day.
Immediate release: Oral: Usual dose: 100 mg twice daily as monotherapy; may increase to 400 mg/day in divided doses, if needed, with close monitoring. Note: Patients with a serious concomitant illness or those receiving high doses of other antiparkinson drugs should be started at 100 mg once daily; may increase to 100 mg twice daily, if needed, after one to several weeks.
Chorea of Huntington disease (off-label use): Immediate release: Oral: 100 mg 3 to 4 times daily. Additional data may be necessary to further define the role of amantadine in this condition (Armstrong 2012; O'Suilleabhain 2003; Verhagen 2002).
Multiple sclerosis-related fatigue (off-label use): Immediate release: Oral: 100 mg twice daily. Additional data may be necessary to further define the role of amantadine in this condition (Ledinek 2013; Shaygannejad 2012).
Restless legs syndrome (off-label use): Immediate release: Oral: Initial: 100 mg daily; increase by 100 mg every 3 to 5 days based on response and tolerability up to 300 mg/day in 1 to 3 divided doses. Additional data may be necessary to further define the role of amantadine in this condition (Evidente 2000).
Traumatic brain injury (off-label use): Immediate release: Oral: Initial: 100 mg twice daily (morning and afternoon); may increase total daily dose by 100 mg every week based on response and tolerability up to 200 mg twice daily. Additional data may be necessary to further define the role of amantadine in this condition (Giacino 2012; Hammond 2014).
Discontinuation of therapy: Do not discontinue abruptly. For patients who have taken the extended-release capsule for more than 4 weeks, reduce dose by half for 1 week before discontinuing, if possible. Reduce the dose of the extended-release tablet gradually from higher doses to 129 mg/day for 1 to 2 weeks before discontinuing.
Dosing: Geriatric
Drug-induced extrapyramidal symptoms/Parkinson disease: Refer to adult dosing; some patients tolerate the immediate-release formulations better when administered in 2 divided daily doses (to avoid adverse neurologic reactions).
Influenza A treatment/prophylaxis: Immediate release: Oral: 100 mg once daily. Note: Due to issues of resistance, amantadine is no longer recommended for the treatment or prophylaxis of influenza A (CDC 2018; IDSA [Uyeki 2019]). Please refer to current CDC recommendations.
Discontinuation of therapy: Refer to adult dosing.
Dosing: Pediatric
Attention-deficit/hyperactivity disorder (ADHD): Limited data available: Oral: Immediate release: Children ≥5 years and Adolescents: Initial: 50 mg/day; titrate up at 4 to 7 day intervals in 50 mg increments to effect; reported range: 50 to 150 mg/day in divided doses 1 to 3 times daily (morning, noon, and 4 PM); maximum daily dose (weight-dependent): <30 kg: 100 mg/day; ≥30 kg: 150 mg/day (Donfrancecso 2007; Mohammadi 2010); dosing based on two small open-label trials (n=24, n=20; age range: 5 to 14 years) which suggested improvements in symptoms; the comparison trial with methylphenidate (n=40) showed both amantadine and methylphenidate yielded significant improvement in ADHD symptoms (50% reduction from baseline symptoms), with no significant differences in efficacy between the groups; more frequent side effects in the methylphenidate group (Mohammadi 2010).
Autism (hyperactivity, irritability): Very limited data available (Hosenbocus 2013): Oral: Immediate release: Children ≥5 years and Adolescents: Initial: 2.5 mg/kg/dose once daily for 1 week, then increase to 2.5 mg/kg/dose twice daily; maximum daily dose: 200 mg/day; dosing based on short-term (4-week) double-blind, placebo-controlled trial of 39 pediatric patients (treatment group, n=19) which showed improvement in clinician-rated behavioral and hyperactivity ratings (King 2001).
Influenza A treatment/prophylaxis: Note: Due to high resistance rates, amantadine is no longer recommended by the CDC for the treatment or prophylaxis of influenza A (CDC 2018; IDSA [Uyeki 2019]). Please refer to the current CDC recommendations. The following is based on the manufacturer's labeling and last applicable CDC guidelines (CDC/ACIP 2011): Oral: Immediate release:
Influenza A treatment:
1 to 9 years: 5 mg/kg/day in 2 divided doses (manufacturer's labeling: 4.4 to 8.8 mg/kg/day); maximum daily dose: 150 mg/day.
≥10 years and <40 kg: 5 mg/kg/day in 2 divided doses (CDC/ACIP 2011).
≥10 years and ≥40 kg: 100 mg twice daily (CDC/ACIP 2011).
Note: Initiate within 24 to 48 hours after onset of symptoms; continue for 24 to 48 hours after symptom resolution (duration of therapy is generally 3 to 5 days).
Influenza A prophylaxis: Refer to "Influenza A treatment" dosing.
Note: Continue prophylaxis throughout the peak influenza activity in the community or throughout the entire influenza season in patients who cannot be vaccinated. Development of immunity following vaccination takes ~2 weeks; amantadine therapy should be considered for high-risk patients from the time of vaccination until immunity has developed. For ages <9 years receiving influenza vaccine for the first time, amantadine prophylaxis should continue for 6 weeks (4 weeks after the first dose and 2 weeks after the second dose).
Multiple-sclerosis associated lassitude (fatigue): Limited data available (Beers 2005; Pohl 2007): Oral: Immediate release:
6 to <10 years or weight <40 kg: 2.5 mg/kg/dose twice daily; maximum daily dose: 150 mg/day.
≥10 years and weight ≥40 kg: 100 mg twice daily, may titrate dose to clinical response; maximum daily dose: 400 mg/day.
Traumatic brain injury (TBI): Limited data available: Oral: Immediate release:
Children ≥6 years and Adolescents <16 years: 4 to 6 mg/kg/day in 2 divided doses; maximum daily dose (age or weight dependent): If <10 years or <40 kg: 150 mg/day; if ≥10 years or ≥40 kg: 200 mg/day (Beers 2005; McMahon 2009). While total daily dose similar in trials, the reported dosing approaches and efficacy results are variable (eg, timing of therapy initiation, duration of study, outcome measures) (Williams 2007). In an open-label, case-controlled trial of 27 pediatric patients with TBI within the last 24 months prior to enrollment (n=17 amantadine treatment, n=10 controls), patients received 5 mg/kg/day for entire study period of 12 weeks; results showed improvement in behavior (parental report) and a subset analysis suggested therapy more effective on cognition for those with more recent injury (Beers 2005). In a double-blind, placebo-controlled crossover trial of seven pediatric patients (mean age: 12.7 years) with TBI within last 12 weeks prior to enrollment, therapy was initiated at 4 mg/kg/day up to 300 mg/day for 1 week, and increased to 6 mg/kg/day up to 400 mg/day for Weeks 2 and 3 of the study duration; improved consciousness observed during treatment period of study (McMahon 2009; Vargus-Adams 2010).
Adolescents ≥16 years: Initial: 100 mg twice daily for 14 days; on Week 3 increase to 150 mg twice daily; may further increase to 200 mg twice daily on Week 4 if needed; dosing based on a multicenter, double-blind, placebo-controlled trial of 184 patients (age range: 16 to 65 years; treatment group, n=87) which showed 4 weeks of amantadine therapy initiated at 4 to 16 weeks postinjury increased the rate of functional recovery (Giacino 2012).
Administration
Oral:
Extended-release capsule: Administer at bedtime with or without food. Swallow whole; do not crush, chew, or divide capsules. If needed, sprinkle entire contents on a small amount (teaspoonful) of soft food, such as applesauce, and administer immediately without chewing.
Extended-release tablet: Administer in the morning without regard to food. Swallow whole; do not crush, chew, or divide tablets.
Storage
Store at 20°C to 25°C (68°F to 77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Protect immediate-release capsules from moisture and exposure to light.
Amantadine Images
Drug Interactions
Alcohol (Ethyl): May enhance the CNS depressant effect of Amantadine. Alcohol may also cause dose-dumping for at least one extended-release amantadine product. Avoid combination
Alizapride: May diminish the therapeutic effect of Anti-Parkinson Agents (Dopamine Agonist). Avoid combination
Alkalinizing Agents: May increase the serum concentration of Amantadine. Monitor therapy
Amisulpride: May diminish the therapeutic effect of Anti-Parkinson Agents (Dopamine Agonist). Anti-Parkinson Agents (Dopamine Agonist) may diminish the therapeutic effect of Amisulpride. Avoid combination
Anticholinergic Agents: Amantadine may enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Antipsychotic Agents (First Generation [Typical]): May diminish the therapeutic effect of Anti-Parkinson Agents (Dopamine Agonist). Anti-Parkinson Agents (Dopamine Agonist) may diminish the therapeutic effect of Antipsychotic Agents (First Generation [Typical]). Management: Avoid concomitant therapy if possible and monitor for decreased effects of both agents when these combinations cannot be avoided. Atypical antipsychotics such as clozapine and quetiapine may be less likely to reduce the effects of anti-Parkinson agents. Consider therapy modification
Antipsychotic Agents (Second Generation [Atypical]): May diminish the therapeutic effect of Anti-Parkinson Agents (Dopamine Agonist). Management: Consider using an alternative antipsychotic agent when possible in patients with Parkinson disease. If an atypical antipsychotic is necessary, consider using clozapine or quetiapine, which may convey the lowest interaction risk. Consider therapy modification
Bromopride: May diminish the therapeutic effect of Anti-Parkinson Agents (Dopamine Agonist). Monitor therapy
BuPROPion: Anti-Parkinson Agents (Dopamine Agonist) may enhance the adverse/toxic effect of BuPROPion. Monitor therapy
Carbonic Anhydrase Inhibitors: May increase the serum concentration of Amantadine. Monitor therapy
Erdafitinib: May increase the serum concentration of OCT2 Substrates. Monitor therapy
Glycopyrrolate (Systemic): Amantadine may enhance the anticholinergic effect of Glycopyrrolate (Systemic). Monitor therapy
Influenza Virus Vaccine (Live/Attenuated): Antiviral Agents (Influenza A and B) may diminish the therapeutic effect of Influenza Virus Vaccine (Live/Attenuated). Management: Avoid anti-influenza antivirals during the period beginning 48 hours prior to and ending 2 weeks after live influenza virus vaccine administration. Consider therapy modification
Memantine: NMDA Receptor Antagonists may enhance the adverse/toxic effect of Memantine. Monitor therapy
Methylphenidate: May enhance the adverse/toxic effect of Anti-Parkinson Agents (Dopamine Agonist). Monitor therapy
Metoclopramide: May diminish the therapeutic effect of Anti-Parkinson Agents (Dopamine Agonist). Monitor therapy
Propiverine: May enhance the adverse/toxic effect of Amantadine. Monitor therapy
Solriamfetol: Anti-Parkinson Agents (Dopamine Agonist) may enhance the hypertensive effect of Solriamfetol. Monitor therapy
Sulpiride: May diminish the therapeutic effect of Anti-Parkinson Agents (Dopamine Agonist). Avoid combination
Tafenoquine: May increase the serum concentration of OCT2 Substrates. Management: Avoid use of OCT2 substrates with tafenoquine, and if the combination cannot be avoided, monitor closely for evidence of toxicity of the OCT2 substrate and consider a reduced dose of the OCT2 substrate according to that substrate's labeling. Consider therapy modification
Trimethoprim: May enhance the adverse/toxic effect of Amantadine. Specifically, the risk of myoclonus and/or delirium may be increased. Amantadine may increase the serum concentration of Trimethoprim. Trimethoprim may increase the serum concentration of Amantadine. Monitor therapy
Urinary Acidifying Agents: May decrease the serum concentration of Amantadine. Monitor therapy
Test Interactions
May interfere with urine detection of amphetamines/methamphetamines (false-positive).
Adverse Reactions
>10%:
Cardiovascular: Orthostatic hypotension (≤29%; may be more common in men), presyncope (≤29%), syncope (≤29%), peripheral edema (1% to 16%)
Central nervous system: Dizziness (≤29%), delusions (≤25%), hallucination (≤25%), illusion (≤25%), paranoia (≤25%), falling (13%)
Gastrointestinal: Xerostomia (1% to 16%; may be more common in women), constipation (1% to 13%)
1% to 10%:
Cardiovascular: Livedo reticularis (1% to 6%; may be more common in women)
Central nervous system: Insomnia (5% to 10%), anxiety (1% to 7%), depression (1% to 6%), headache (1% to 6%), abnormal dreams (1% to 5%; may be more common in women), agitation (1% to 5%), ataxia (1% to 5%; may be more common in men and adults ≥65 years old), confusion (1% to 5%), drowsiness (1% to 5%), fatigue (1% to 5%), irritability (1% to 5%), nervousness (1% to 5%), dyschromia (3%), dystonia (3%), apathy (2%), suicidal ideation (≤2%)
Gastrointestinal: Nausea (5% to 10%; may be more common in women), decreased appetite (6%), anorexia (1% to 5%), diarrhea (1% to 5%), vomiting (3%)
Genitourinary: Urinary tract infection (10%), benign prostatic hypertrophy (6%)
Hematologic & oncologic: Bruise (6%)
Neuromuscular & skeletal: Joint swelling (3%), muscle spasm (3%)
Ophthalmic: Blurred vision (4%), cataract (3%; may be more common in women), xerophthalmia (3%)
Respiratory: Dry nose (1% to 5%), cough (3%)
<1%, postmarketing, and/or case reports: Abnormal gait, abnormality in thinking, acute respiratory tract failure, aggressive behavior, agranulocytosis, amnesia, anaphylaxis, cardiac arrhythmia (including malignant arrhythmias), cardiac failure, coma, corneal edema, decreased libido, decreased visual acuity, delirium, diaphoresis, dysphagia, dyspnea, eczema, edema, EEG pattern changes, euphoria, fever, hyperkinesia, hypersensitivity reaction, hypertension, hypertonia, hypokinesia, hypotension, impulse control disorder, increased blood urea nitrogen, increased creatine phosphokinase, increased gamma-glutamyl transferase, increased lactate dehydrogenase, increased libido, increased serum alkaline phosphatase, increased serum ALT, increased serum AST, increased serum bilirubin, increased serum creatinine, keratitis, leukocytosis, leukopenia, mania, mydriasis, neuroleptic malignant syndrome (associated with dosage reduction or abrupt withdrawal of amantadine), neutropenia, oculogyric crisis, optic nerve palsy, paresthesia, pathological gambling, pruritus, psychosis, pulmonary edema, seizure, skin photosensitivity, skin rash, slurred speech, stupor, tachycardia, tachypnea, tremor, urinary retention, visual disturbance (including punctate subepithelial or other corneal opacity), weakness
Warnings/Precautions
Concerns related to adverse effects:
- CNS depression: May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks that require mental alertness (eg, operating machinery or driving). Patients taking amantadine for Parkinson disease have reported falling asleep while engaged in activities of daily living, sometimes without warning. Patients with a concomitant sleep disorder may be at a greater risk. There is insufficient information that dose reduction will eliminate episodes of falling asleep or daytime somnolence.
- Impulse control disorders: Dopamine agonists used for Parkinson disease or restless legs syndrome have been associated with compulsive behaviors and/or loss of impulse control, which has manifested as pathological gambling, libido increases (hypersexuality), urges to spend money, and/or binge eating. Causality has not been established, and controversy exists as to whether this phenomenon is related to the underlying disease, prior behaviors/addictions, and/or drug therapy. Dose reduction or discontinuation of therapy has been reported to reverse these behaviors in some, but not all cases.
- Melanoma: Risk for melanoma development is increased in Parkinson disease patients; drug causation or factors contributing to risk have not been established. Patients should be monitored closely and periodic skin examinations should be performed.
- Psychosis: Visual and auditory hallucinations, delusions, illusions, and paranoia were reported in clinical trials; monitor for the occurrence of these symptoms especially at initiation and after dose increases. Use is not recommended in patients with preexisting psychotic disorders.
- Suicidal ideation/depression: There have been reports of suicidal ideation/attempt and depression in patients with and without a history of psychiatric illness. May exacerbate mental problems in patients with a history of mental illness.
Disease-related concerns:
- Cardiovascular disease: Use with caution in patients with heart failure, peripheral edema, or orthostatic hypotension; dizziness, syncope, orthostatic hypotension, presyncope, postural dizziness, and hypotension have been reported in clinical trials. Dosage reduction may be required.
- Eczema: Use with caution in patients with a history of recurrent and eczematoid dermatitis.
- Glaucoma: Avoid in untreated angle closure glaucoma.
- Hepatic impairment: Use with caution in patients with hepatic impairment; rarely, reversible elevations in transaminases have been reported.
- Renal impairment: Use with caution in patients with renal impairment; dosage reduction recommended. Use of the extended-release products is contraindicated in end-stage renal disease (CrCl <15 mL/minute/1.73 m2).
- Seizure disorder: Use with caution in patients with a history of seizure disorder.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Elderly: Use with caution in the elderly; may be more susceptible to CNS effects (using 2 divided daily doses of immediate-release products may minimize this effect). These patients may require dosage reductions.
Dosage form specific issues:
- Propylene glycol: Some dosage forms may contain propylene glycol; large amounts are potentially toxic and have been associated hyperosmolality, lactic acidosis, seizures and respiratory depression; use caution (AAP 1997; Zar 2007).
Other warnings/precautions:
- Tolerance: Tolerance has also been reported with long-term use (Zubenko 1984).
- Withdrawal syndrome: A symptom complex resembling neuroleptic malignant syndrome (elevated temperature, muscular rigidity, altered consciousness, and autonomic instability) with no other obvious cause has been reported in association with rapid dose reduction, withdrawal of, or changes in drugs that increased central dopaminergic dose. Abrupt discontinuation of amantadine may cause agitation, anxiety, delirium, delusions, depression, hallucinations, paranoia, parkinsonian crisis, slurred speech, or stupor. Upon discontinuation of amantadine therapy, gradually taper dose.
Monitoring Parameters
Renal function (baseline and as clinically indicated), mental status including psychosis, hallucinations, depression and suicidality, dizziness, blood pressure, and orthostasis (as clinically indicated)
Pregnancy
Pregnancy Risk Factor
C
Pregnancy Considerations
Adverse events have been observed in animal reproduction studies and teratogenic events have been observed in humans (case reports) (Seier 2017).
When treatment for Parkinson disease is needed, agents other than amantadine are recommended in pregnant women (Seier 2017).
Untreated influenza infection is associated with an increased risk of adverse events to the fetus and an increased risk of complications or death to the mother. Other agents are currently recommended for the treatment or prophylaxis influenza in pregnant women and women up to 2 weeks postpartum. Appropriate antiviral agents are currently recommended as an adjunct to vaccination and should not be used as a substitute for vaccination in pregnant women (CDC 2011; CDC 2014).
Patient Education
What is this drug used for?
- It is used to treat or prevent the flu.
- It is used to treat Parkinson's disease and side effects caused by some other drugs.
- It may be given for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Dry mouth
- Constipation
- Lack of appetite
- Abnormal dreams
- Dry nose
- Diarrhea
- Loss of strength and energy
- Tablet shell in stool
- Nausea
- Headache
- Anxiety
- Trouble sleeping
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Confusion
- Severe dizziness
- Passing out
- Sensing things that seem real but are not
- Seizures
- Shortness of breath
- Excessive weight gain
- Swelling of arms or legs
- Difficult urination
- Blurred vision
- Uncontrollable urges
- Change in balance
- Falls
- Depression like thoughts of suicide, anxiety, emotional instability, agitation, irritability, panic attacks, mood changes, behavioral changes, or confusion
- Skin growths
- Mole changes
- Urinary tract infection like blood in the urine, burning or painful urination, passing a lot of urine, fever, lower abdominal pain, or pelvic pain.
- Narcolepsy
- Severe fatigue
- Neuroleptic malignant syndrome like fever, muscle cramps or stiffness, dizziness, severe headache, confusion, change in thinking, fast heartbeat, abnormal heartbeat, or sweating a lot.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.