Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Solution, Intravenous:
Generic: 250 mg/mL (20 mL)
Solution, Oral:
Amicar: 25% (236.5 mL) [contains edetate disodium, methylparaben, propylparaben, saccharin sodium; raspberry flavor]
Generic: 25% (236.5 mL)
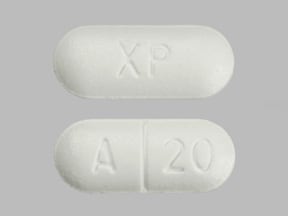
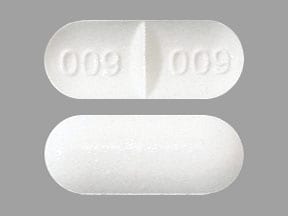
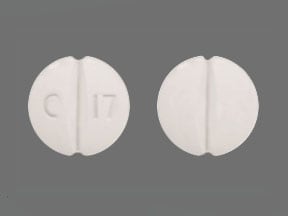
Tablet, Oral:
Amicar: 500 mg, 1000 mg [scored]
Generic: 500 mg, 1000 mg
Pharmacology
Mechanism of Action
Binds competitively to plasminogen; blocking the binding of plasminogen to fibrin and the subsequent conversion to plasmin, resulting in inhibition of fibrin degradation (fibrinolysis).
Pharmacokinetics/Pharmacodynamics
Distribution
Widely through intravascular and extravascular compartments; Vd: Oral: 23 L, IV: 30 L
Metabolism
Minimally hepatic
Excretion
Urine (65% as unchanged drug, 11% as metabolite)
Onset of Action
~1 to 72 hours
Time to Peak
Oral: 1.2 ± 0.45 hours
Half-Life Elimination
1 to 2 hours
Use: Labeled Indications
To enhance hemostasis when fibrinolysis contributes to bleeding (causes may include cardiac surgery, hematologic disorders, neoplastic disorders, abruptio placentae, hepatic cirrhosis, and urinary fibrinolysis)
Use: Off Label
Bleeding associated with dental procedures in patients on oral anticoagulant therapy (mouth rinse)c
Data from a limited number of patients studied suggest that aminocaproic acid may be beneficial for the prevention of bleeding associated with dental procedures in patients on oral anticoagulant therapy (mouth rinse) Souto 1996. Additional data may be necessary to further define the role of aminocaproic acid in this condition.
Bleeding (control) in severe thrombocytopeniac
Data from a limited number of patients studied (case series) in patients with amegakaryocytic thrombocytopenia and immune thrombocytopenia who were refractory to usual therapies suggests that aminocaproic acid may be beneficial for the control of bleeding associated with severe thrombocytopenia Bartholomew 1989, Gardner 1980. Additional data may be necessary to further define the role of aminocaproic acid in this condition.
Control of refractory bleeding associated with extracorporeal membrane oxygenationc
Data from a limited number of patients studied (cases series) suggests that the use of aminocaproic acid may be beneficial for the control of refractory bleeding in patients on extracorporeal membrane oxygenation (ECMO) Buckley 2016. Additional data may be necessary to further define the role of aminocaproic acid to control bleeding associated with ECMO.
Intracranial hemorrhage associated with thrombolytics (plasminogen-activator) (eg, alteplase, reteplase, or tenecteplase)yes
Based on the Neurocritical Care Society and the Society of Critical Care Medicine guideline for reversal of antithrombotics in intracranial hemorrhage, aminocaproic acid is suggested as a reversal agent for use in intracranial hemorrhage due to thrombolytics (plasminogen-activator) (eg, alteplase, reteplase, tenecteplase) in cases where cryoprecipitate (preferred therapy) is contraindicated or not available in a timely manner.
Oral bleeding (control) in congenital and acquired coagulation disordersc
Data from a limited number of clinical trials suggest that aminocaproic acid may be beneficial for the control of oral bleeding in congenital and acquire coagulation disorders Lucas 1981. Clinical experience also suggests the utility of aminocaproic acid in managing the treatment of oral bleeding in congenital and acquired coagulation disorders Mannucci 1998. Additional data may be necessary to further define the role of aminocaproic acid in this condition.
Perioperative bleeding (prevention) associated with cardiac surgerya
Data from three randomized, prospective, placebo-controlled studies supports the use of aminocaproic acid in the prevention of perioperative bleeding associated with cardiac surgery Fergusson 2008, Penta de Peppo 1995, Vander Salm 1996.
Subarachnoid hemorrhagecyes
Current evidence suggests aminocaproic acid may be an effective option for prevention of rebleeding in patients with SAH, provided therapy does not continue past 72 hours after the event and there are no thromboembolic risk factors. Incidents of early rebleeding are often fatal and are a primary concern in SAH; however, thrombotic events also remain a serious concern because of a lack of data from adequately powered studies demonstrating the risk of adverse events. Other guideline recommendations to avoid rebleeding include tranexamic acid (another antifibrinolytic), a titratable agent to control hypertension (SBP less than 160 mm Hg), and surgical interventions, such as clipping or endovascular coiling.
Traumatic hyphemab
Data from one prospective, randomized, placebo-controlled, double-blind, multicenter study and one randomized, placebo-controlled study support the use of aminocaproic acid in the treatment of secondary hemorrhage after traumatic hyphema Crouch 1997, McGetrick 1983. Clinical experience also suggests the utility of aminocaproic acid in managing this condition Brandt 2001, Crouch 1999. Additional trials may be necessary to further define the role of aminocaproic acid in this condition.
Contraindications
Disseminated intravascular coagulation (without heparin); evidence of an active intravascular clotting process
Dosage and Administration
Dosing: Adult
Acute bleeding: Oral, IV: Loading dose: 4 to 5 g during the first hour, followed by 1 g/hour for 8 hours (or 1.25 g/hour using oral solution) or until bleeding controlled (maximum daily dose: 30 g)
Control of bleeding with severe thrombocytopenia (off-label use) (Bartholomew 1989, Gardner 1980):
Initial: IV: 100 mg/kg (maximum dose: 5 g) over 30 to 60 minutes
Maintenance: Oral, IV: 1 to 4 g every 4 to 8 hours or 1 g/hour (maximum daily dose: 24 g). Additional data may be necessary to further define the role of aminocaproic acid in the treatment of this condition.
Control of oral bleeding in congenital and acquired coagulation disorder (off-label use): Oral: 50 to 60 mg/kg every 4 hours (Mannucci 1998). Additional data may be necessary to further define the role of aminocaproic acid in the treatment of this condition.
Control of refractory bleeding associated with extracorporeal membrane oxygenation (off-label use): IV: 4 to 5 g loading dose; follow with an infusion of 1 to 1.25 g/hour until bleeding controlled (Buckley 2016). Additional data may be necessary to further define the role of aminocaproic acid in the treatment of this condition.
Intracranial hemorrhage associated with thrombolytics (plasminogen-activator) (eg, alteplase, reteplase, tenecteplase) (off-label use): IV: 4 to 5 g (as an alternative to cryoprecipitate); check fibrinogen levels after administration, if fibrinogen <150 mg/dL, cryoprecipitate is recommended (NCS/SCCM [Frontera 2016]).
Prevention of dental procedure bleeding in patients on oral anticoagulant therapy (off-label use): Oral rinse: Hold 4 g/10 mL in mouth for 2 minutes then spit out. Repeat every 6 hours for 2 days after procedure (Souto 1996). Concentration and frequency may vary by institution and product availability. Additional data may be necessary to further define the role of aminocaproic acid in the treatment of this condition.
Prevention of perioperative bleeding associated with cardiac surgery (off-label use): IV: Loading dose of 75 to 150 mg/kg (typically 5 to 10 g), followed by 10 to 15 mg/kg/hour (typically 1 g/hour); may add 2 to 2.5 g/L of cardiopulmonary bypass circuit priming solution (Gravlee 2008)
or
Loading dose of 10 g followed by 2 g/hour during surgery; no medication added to the bypass circuit (Fergusson 2008)
or
10 g over 20 to 30 minutes prior to skin incision, followed by 10 g after heparin administration then 10 g at discontinuation of cardiopulmonary bypass (Vander Salm1996)
Subarachnoid hemorrhage (off-label use): IV: Loading dose of 4 g followed by 1 g/hour infusion for up to 72 hours after SAH onset. Note: Discontinue infusion 4 hours prior to angiography or 2 hours prior to endovascular ablation of aneurysm (Diringer 2011; Starke 2008). Additional data may be necessary to further define the role of aminocaproic acid in the treatment of this condition.
Traumatic hyphema (off-label use): Oral: 50 mg/kg/dose every 4 hours (maximum daily dose: 30 g) for 5 days (Brandt 2001; Crouch 1999)
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Control of hemorrhage (oral, epistaxis, menorrhagia) in hemophilic patients, adjunct treatment: Limited data available: Infants, Children, and Adolescents: Oral: 50-100 mg/kg/dose every 6 hours; maximum daily dose: 24 g/day (Acharya, 2011)
Control of mucosal bleeding in thrombocytopenia/platelet dysfunction: Limited data available: Infants, Children, and Adolescents: Oral, IV: 50-100 mg/kg/dose every 6 hours; maximum daily dose: 24 g/day (Bussel, 2011; Lipton, 2011)
Hematuria (gross; upper tract), refractory: Limited data available: Children ≥11 years and Adolescents: Oral: 100 mg/kg/dose every 6 hours; continue for 2 days beyond resolution of hematuria; dosing based on case series (n=4) which showed hematuria resolution within 2-7 days; risks and benefits must be weighed prior to use (Kaye, 2010)
Prevention of bleeding associated with dental procedures in hemophilic patients: Limited data available: Infants, Children, and Adolescents: Oral: 50-100 mg/kg/dose every 6 hours; maximum daily dose: 24 g/day; used in conjunction with DDAVP or factor replacement therapy; continue for up to 7 days or until mucosal healing is complete (Acharya, 2011)
Prevention of bleeding associated with extracorporeal membrane oxygenation (ECMO), high-bleeding risk patients: Limited data available: Infants, Children, and Adolescents: IV: 100 mg/kg prior to or immediately after cannulation, followed by 25-30 mg/kg/hour for up to 72 hours; target activated clotting time (ACT) range during therapy of 180-200 seconds has been used (Downard, 2003; Horwitz, 1998; Wilson, 1993); variable results; patients requiring surgery just prior to or while on ECMO seem to benefit most
Prevention of perioperative bleeding associated with cardiac surgery: Limited data available:
Infants and Children <2 years: Dosing regimens variable: IV: In the largest trial (n=120, all patients <20 kg), a dose of 75 mg/kg was administered at the beginning and end of cardiopulmonary bypass (CPB), and 75 mg/100 mL was added to the CPB priming fluid (Martin, 2011a). Another study group in two separate trials (n=110, age range: 2 months to 14 years) used a 100 mg/kg dose after induction, during CPB pump priming, and when weaning CPB (over 3 hours) for a total of three doses (Chauhan, 2000; Chauhan, 2004).
Children ≥2 years and Adolescents: IV: 100 mg/kg after induction, during CPB pump priming, and when weaning CPB (over 3 hours) for a total of 3 doses; regimen used in two separate trials (n=110, age range: 2 months to 14 years) (Chauhan, 2000; Chauhan, 2004)
Prevention of perioperative bleeding associated with spinal surgery (eg, idiopathic scoliosis): Limited data available: Children ≥11 years and Adolescents: IV: 100 mg/kg (maximum dose: 5 g) administered over 15-20 minutes after induction, followed by a continuous IV infusion of 10 mg/kg/hour for the remainder of the surgery; discontinued at time of wound closure (Florentino-Pineda, 2001; Florentino-Pineda, 2004)
Traumatic hyphema: Limited data available: Infants, Children, and Adolescents: Oral: 50-100 mg/kg/dose every 4 hours for 5 days; maximum daily dose: 30 g/day (Brandt, 2001; Crouch, 1999; Teboul, 1995)
Reconstitution
Dilute IV solution in D5W, 0.9% sodium chloride, or Ringer's injection.
Administration
Rapid IV injection (IVP) of undiluted solution is not recommended due to possible hypotension, bradycardia, and arrhythmia.
IV: May administer loading dose over 15-60 minutes depending on indication; a continuous infusion may be necessary.
Storage
Store intact vials, tablets, and syrup at 20°C to 25°C (68°F to 77°F). Do not freeze. Solutions diluted for IV use in D5W or NS to concentrations of 10 to 100 mg/mL are stable at 4°C (39°F) and 23°C (73°F) for 7 days (Zhang 1997).
Aminocaproic Acid Images
Drug Interactions
Anti-inhibitor Coagulant Complex (Human): Antifibrinolytic Agents may enhance the thrombogenic effect of Anti-inhibitor Coagulant Complex (Human). Avoid combination
Factor IX Complex (Human) [(Factors II, IX, X)]: Aminocaproic Acid may enhance the adverse/toxic effect of Factor IX Complex (Human) [(Factors II, IX, X)]. Specifically, use of this combination may increase the risk of thrombosis. Avoid combination
Tretinoin (Systemic): May enhance the thrombogenic effect of Antifibrinolytic Agents. Monitor therapy
Adverse Reactions
Frequency not defined.
Cardiovascular: Arrhythmia, bradycardia, edema, hypotension, intracranial hypertension, peripheral ischemia, syncope, thrombosis
Central nervous system: Confusion, delirium, dizziness, fatigue, hallucinations, headache, malaise, seizure, stroke
Dermatologic: Rash, pruritus
Gastrointestinal: Abdominal pain, anorexia, cramps, diarrhea, GI irritation, nausea, vomiting
Genitourinary: Dry ejaculation
Hematologic: Agranulocytosis, bleeding time increased, leukopenia, thrombocytopenia
Local: Injection site necrosis, injection site pain, injection site reactions
Neuromuscular & skeletal: CPK increased, myalgia, myositis, myopathy, rhabdomyolysis (rare), weakness
Ophthalmic: Vision decreased, watery eyes
Otic: Tinnitus
Renal: BUN increased, intrarenal obstruction (glomerular capillary thrombosis), myoglobinuria (rare), renal failure (rare)
Respiratory: Dyspnea, nasal congestion, pulmonary embolism
Miscellaneous: Allergic reaction, anaphylactoid reaction, anaphylaxis
Postmarketing and/or case reports: Hepatic lesion, hyperkalemia, myocardial lesion
Warnings/Precautions
Concerns related to adverse effects:
- Intrarenal obstruction: May occur secondary to glomerular capillary thrombosis or clots in the renal pelvis and ureters; do not use in hematuria of upper urinary tract origin unless possible benefits outweigh risks.
- Skeletal muscle weakness: Ranging from mild myalgias and fatigue to severe myopathy with rhabdomyolysis and acute renal failure has been reported with prolonged use. Monitor CPK; discontinue treatment with a rise in CPK.
Disease-related concerns:
- Renal impairment: Use with caution in patients with renal impairment; may accumulate.
Concurrent drug therapy issues:
- Blood products: Do not administer with factor IX complex concentrates or anti-inhibitor coagulant complexes; may increase risk for thrombosis.
Dosage form specific issues:
- Benzyl alcohol and derivatives: Some dosage forms may contain benzyl alcohol; large amounts of benzyl alcohol (≥99 mg/kg/day) have been associated with a potentially fatal toxicity (“gasping syndrome”) in neonates; the “gasping syndrome” consists of metabolic acidosis, respiratory distress, gasping respirations, CNS dysfunction (including convulsions, intracranial hemorrhage), hypotension and cardiovascular collapse (AAP ["Inactive" 1997]; CDC, 1982); some data suggests that benzoate displaces bilirubin from protein binding sites (Ahlfors, 2001); avoid or use dosage forms containing benzyl alcohol with caution in neonates. See manufacturer’s labeling.
Other warnings/precautions:
- Appropriate use: Do not administer without a definite diagnosis of laboratory findings indicative of hyperfibrinolysis. Inhibition of fibrinolysis may promote clotting or thrombosis; more likely due to the presence of DIC.
- IV administration: Avoid rapid IV administration; may induce hypotension, bradycardia, or arrhythmia; rapid injection of undiluted solution is not recommended.
Monitoring Parameters
Fibrinogen, fibrin split products, creatine phosphokinase (with long-term therapy), BUN, creatinine
Pregnancy
Pregnancy Risk Factor
C
Pregnancy Considerations
Animal reproduction studies have not been conducted.
Patient Education
What is this drug used for?
- It is used to treat or prevent bleeding.
Frequently reported side effects of this drug
- Nausea
- Vomiting
- Abdominal pain
- Diarrhea
- Loss of strength and energy
- Stuffy nose
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Severe cerebrovascular disease like change in strength on one side is greater than the other, difficulty speaking or thinking, change in balance, or vision changes.
- DVT like edema, warmth, numbness, change in color, or pain in the extremities.
- Abnormal heartbeat
- Slow heartbeat
- Bruising
- Bleeding
- Unable to pass urine
- Change in amount of urine passed
- Muscle pain
- Muscle weakness
- Edema
- Seizures
- Passing out
- Severe dizziness
- Sensing things that seem real but are not
- Confusion
- Chest pain
- Coughing up blood
- Shortness of breath
- Chills
- Sore throat
- Severe headache
- Vision changes
- Noise or ringing in the ears
- Severe injection site pain or irritation
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Patient should consult prescriber for additional questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.