Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Tablet, Oral:
Caduet: Amlodipine 5 mg and atorvastatin 10 mg, Amlodipine 2.5 mg and atorvastatin 40 mg [DSC], Amlodipine 2.5 mg and atorvastatin 20 mg [DSC], Amlodipine 2.5 mg and atorvastatin 10 mg [DSC], Amlodipine 5 mg and atorvastatin 20 mg, Amlodipine 5 mg and atorvastatin 40 mg, Amlodipine 5 mg and atorvastatin 80 mg
Caduet: Amlodipine 10 mg and atorvastatin 10 mg, Amlodipine 10 mg and atorvastatin 20 mg, Amlodipine 10 mg and atorvastatin 40 mg, Amlodipine 10 mg and atorvastatin 80 mg [contains fd&c blue #2 (indigotine)]
Generic: Amlodipine 10 mg and atorvastatin 10 mg, Amlodipine 10 mg and atorvastatin 20 mg, Amlodipine 10 mg and atorvastatin 40 mg, Amlodipine 10 mg and atorvastatin 80 mg, Amlodipine 2.5 mg and atorvastatin 10 mg, Amlodipine 2.5 mg and atorvastatin 20 mg, Amlodipine 2.5 mg and atorvastatin 40 mg, Amlodipine 5 mg and atorvastatin 10 mg, Amlodipine 5 mg and atorvastatin 20 mg, Amlodipine 5 mg and atorvastatin 40 mg, Amlodipine 5 mg and atorvastatin 80 mg
Pharmacology
Mechanism of Action
Amlodipine: Inhibits calcium ion from entering the “slow channels” or select voltage-sensitive areas of vascular smooth muscle and myocardium during depolarization, producing a relaxation of coronary vascular smooth muscle and coronary vasodilation; increases myocardial oxygen delivery in patients with vasospastic angina. Amlodipine directly acts on vascular smooth muscle to produce peripheral arterial vasodilation reducing peripheral vascular resistance and blood pressure.
Atorvastatin: Inhibitor of 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase, the rate limiting enzyme in cholesterol synthesis (reduces the production of mevalonic acid from HMG-CoA); this then results in a compensatory increase in the expression of LDL receptors on hepatocyte membranes and a stimulation of LDL catabolism. In addition to the ability of HMG-CoA reductase inhibitors to decrease levels of high-sensitivity C-reactive protein (hsCRP), they also possess pleiotropic properties including improved endothelial function, reduced inflammation at the site of the coronary plaque, inhibition of platelet aggregation, and anticoagulant effects (de Denus 2002; Ray 2005).
Use: Labeled Indications
Hypertension, dyslipidemia, angina, documented coronary artery disease, primary and secondary prevention of cardiovascular disease: For use when treatment with both amlodipine and atorvastatin is appropriate:
Amlodipine: Management of hypertension; treatment of symptomatic chronic stable angina, vasospastic angina (previously referred to as Prinzmetal or variant angina); to reduce the risk of hospitalization for angina and to reduce risk of coronary revascularization procedure due to angina with documented coronary artery disease (CAD)
Atorvastatin: Treatment of dyslipidemias (primary hypercholesterolemia [heterozygous familial and nonfamilial] and mixed dyslipidemia [Fredrickson type IIa and IIb], primary dysbetalipoproteinemia [Fredrickson type III], elevated serum TG levels [Fredrickson type IV] in adults; homozygous familial hypercholesterolemia [HoFH]; heterozygous familial hypercholesterolemia [HeFH] in patients 10 to 17 years of age); primary and secondary prevention of cardiovascular disease in adults
Contraindications
Hypersensitivity to amlodipine, atorvastatin, or any component of the formulation; active liver disease; unexplained persistent elevations of serum transaminases; pregnancy; breastfeeding
Canadian labeling: Additional contraindications (not in US labeling): Hypersensitivity to amlodipine, atorvastatin, or to other dihydropyridine calcium channel blockers; concurrent therapy with cyclosporine or glecaprevir/pibrentasvir; severe hypotension (systolic <90 mm Hg).
Dosage and Administration
Dosing: Adult
Note: Dose must be individualized; combination product may be used as initial therapy or substituted for individual components in patients currently maintained on both agents separately or in patients not adequately controlled with monotherapy (using one of the agents or an agent within same pharmacologic class).
Hypertension, dyslipidemia, angina, documented coronary artery disease, primary and secondary prevention of cardiovascular disease: Oral: Initial: Amlodipine 2.5 to 5 mg/atorvastatin 10 to 20 mg once daily; dose may be titrated after 1 to 2 weeks (amlodipine component) and after 2 to 4 weeks (atorvastatin component); maximum dose: amlodipine 10 mg/atorvastatin 80 mg once daily. Patients requiring >45% reduction in low-density lipoprotein cholesterol may be initiated with atorvastatin 40 mg once daily.
Dosing: Geriatric
Refer to adult dosing. Initiate amlodipine at 2.5 mg once daily.
Administration
Administer with or without food.
Dietary Considerations
Before initiation of therapy with atorvastatin, patients should be placed on a standard cholesterol-lowering diet for 3 to 6 months and the diet should be continued during drug therapy.
Red yeast rice contains variable amounts of several compounds that are structurally similar to HMG-CoA reductase inhibitors, primarily monacolin K (or mevinolin) which is structurally identical to lovastatin; concurrent use of red yeast rice with HMG-CoA reductase inhibitors may increase the incidence of adverse and toxic effects (Lapi 2008; Smith 2003).
Storage
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F).
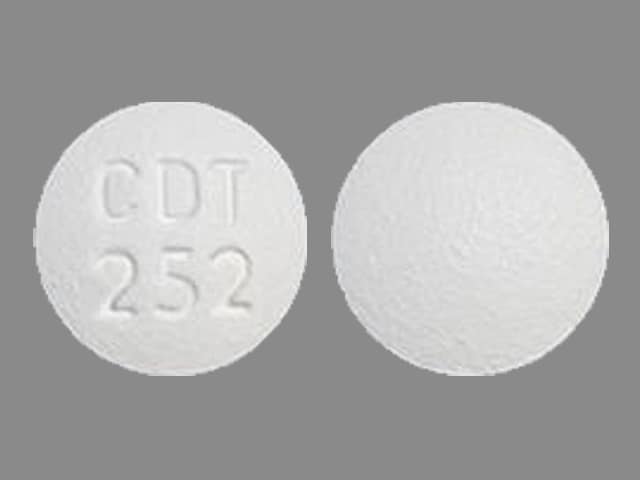
Amlodipine and Atorvastatin Images
Drug Interactions
Acipimox: May enhance the myopathic (rhabdomyolysis) effect of HMG-CoA Reductase Inhibitors (Statins). Monitor therapy
Alfuzosin: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Aliskiren: AtorvaSTATin may increase the serum concentration of Aliskiren. Monitor therapy
Alpha1-Blockers: May enhance the hypotensive effect of Calcium Channel Blockers. Monitor therapy
Amifostine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Amifostine. Management: When amifostine is used at chemotherapy doses, blood pressure lowering medications should be withheld for 24 hours prior to amifostine administration. If blood pressure lowering therapy cannot be withheld, amifostine should not be administered. Consider therapy modification
Amiodarone: May increase the serum concentration of AtorvaSTATin. Monitor therapy
Amphetamines: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Antihepaciviral Combination Products: May increase the serum concentration of AtorvaSTATin. Avoid combination
Antipsychotic Agents (Second Generation [Atypical]): Blood Pressure Lowering Agents may enhance the hypotensive effect of Antipsychotic Agents (Second Generation [Atypical]). Monitor therapy
Aprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
ARIPiprazole: CYP3A4 Inhibitors (Weak) may increase the serum concentration of ARIPiprazole. Management: Monitor for increased aripiprazole pharmacologic effects. Aripiprazole dose adjustments may or may not be required based on concomitant therapy and/or indication. Consult full interaction monograph for specific recommendations. Monitor therapy
Asunaprevir: May increase the serum concentration of HMG-CoA Reductase Inhibitors (Statins). Monitor therapy
Atosiban: Calcium Channel Blockers may enhance the adverse/toxic effect of Atosiban. Specifically, there may be an increased risk for pulmonary edema and/or dyspnea. Monitor therapy
Azithromycin (Systemic): May enhance the myopathic (rhabdomyolysis) effect of AtorvaSTATin. Monitor therapy
Barbiturates: May increase the metabolism of Calcium Channel Blockers. Management: Monitor for decreased therapeutic effects of calcium channel blockers with concomitant barbiturate therapy. Calcium channel blocker dose adjustments may be necessary. Nimodipine Canadian labeling contraindicates concomitant use with phenobarbital. Monitor therapy
Barbiturates: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Benperidol: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Bexarotene (Systemic): May decrease the serum concentration of AtorvaSTATin. Monitor therapy
Bezafibrate: May enhance the myopathic (rhabdomyolysis) effect of HMG-CoA Reductase Inhibitors (Statins). Bezafibrate may increase the serum concentration of HMG-CoA Reductase Inhibitors (Statins). More specifically, bezafibrate may increase the serum concentration of fluvastatin Management: Monitor patients closely for myopathy with concomitant use of bezafibrate and HMG-CoA reductase inhibitors. Concomitant use is contraindicated in patients predisposed to myopathy and alternative therapy should be considered. Consider therapy modification
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Brigatinib: May diminish the antihypertensive effect of Antihypertensive Agents. Brigatinib may enhance the bradycardic effect of Antihypertensive Agents. Monitor therapy
Brimonidine (Topical): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Bromperidol: Blood Pressure Lowering Agents may enhance the hypotensive effect of Bromperidol. Bromperidol may diminish the hypotensive effect of Blood Pressure Lowering Agents. Avoid combination
Calcium Channel Blockers (Nondihydropyridine): Calcium Channel Blockers (Dihydropyridine) may enhance the hypotensive effect of Calcium Channel Blockers (Nondihydropyridine). Calcium Channel Blockers (Nondihydropyridine) may increase the serum concentration of Calcium Channel Blockers (Dihydropyridine). Monitor therapy
Calcium Salts: May diminish the therapeutic effect of Calcium Channel Blockers. Monitor therapy
CarBAMazepine: May increase the metabolism of Calcium Channel Blockers (Dihydropyridine). Management: Consider calcium channel blocker (CCB) dose adjustments or alternative therapy in patients receiving concomitant carbamazepine. Nimodipine Canadian labeling contraindicates concurrent use with carbamazepine. Consider therapy modification
Cimetidine: AtorvaSTATin may enhance the adverse/toxic effect of Cimetidine. Specifically, there is a theoretical potential for enhanced effects on reducing endogenous steroid activity. Monitor therapy
Ciprofibrate: May enhance the adverse/toxic effect of HMG-CoA Reductase Inhibitors (Statins). Management: Avoid the use of HMG-CoA reductase inhibitors and ciprofibrate if possible. If concomitant therapy is considered, benefits should be carefully weighed against the risks, and patients should be monitored closely for signs/symptoms of muscle toxicity. Consider therapy modification
Clarithromycin: May increase the serum concentration of AtorvaSTATin. Management: Limit atorvastatin to a maximum dose of 20 mg/day (for adults) when used with clarithromycin. If this combination is used, monitor patients more closely for evidence of atorvastatin toxicity. Consider therapy modification
Clofazimine: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Clopidogrel: Calcium Channel Blockers may diminish the therapeutic effect of Clopidogrel. Monitor therapy
Cobicistat: May increase the serum concentration of AtorvaSTATin. Management: Avoid the combined use of atorvastatin with atazanavir/cobicistat. Atorvastatin dose should not exceed 20 mg daily when combined with other cobicistat-containing regimens. Consider therapy modification
Colchicine: May enhance the myopathic (rhabdomyolysis) effect of HMG-CoA Reductase Inhibitors (Statins). Colchicine may increase the serum concentration of HMG-CoA Reductase Inhibitors (Statins). Consider therapy modification
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
CycloSPORINE (Systemic): May increase the serum concentration of AtorvaSTATin. Avoid combination
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May increase the metabolism of CYP3A4 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
CYP3A4 Inhibitors (Moderate): May increase the serum concentration of AmLODIPine. Monitor therapy
CYP3A4 Inhibitors (Strong): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Consider therapy modification
Cyproterone: May increase the serum concentration of HMG-CoA Reductase Inhibitors (Statins). Management: Avoid use of statins metabolized by CYP3A4 (eg, simvastatin) and consider avoiding fluvastatin as well in patients receiving high dose cyproterone (300 mg/day). Consider use of pravastatin, rosuvastatin, or pitavastatin if statin therapy is needed. Consider therapy modification
Dabigatran Etexilate: AtorvaSTATin may decrease the serum concentration of Dabigatran Etexilate. Monitor therapy
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Daclatasvir: May increase the serum concentration of HMG-CoA Reductase Inhibitors (Statins). Monitor therapy
Danazol: May increase the serum concentration of HMG-CoA Reductase Inhibitors (Statins). Management: Concurrent use of simvastatin with danazol is contraindicated. Do not exceed 20 mg per day of lovastatin if combined with danazol. Fluvastatin, pravastatin, and rosuvastatin may pose lower risk. Consider therapy modification
Dapoxetine: May enhance the orthostatic hypotensive effect of Calcium Channel Blockers. Monitor therapy
DAPTOmycin: HMG-CoA Reductase Inhibitors (Statins) may enhance the adverse/toxic effect of DAPTOmycin. Specifically, the risk of skeletal muscle toxicity may be increased. Management: Consider temporarily stopping HMG-CoA reductase inhibitor therapy prior to daptomycin. If used together, regular (i.e., at least weekly) monitoring of CPK concentrations is recommended. Consider therapy modification
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Dexmethylphenidate: May diminish the therapeutic effect of Antihypertensive Agents. Monitor therapy
Diazoxide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Digoxin: AtorvaSTATin may increase the serum concentration of Digoxin. Monitor therapy
DilTIAZem: AtorvaSTATin may increase the serum concentration of DilTIAZem. DilTIAZem may increase the serum concentration of AtorvaSTATin. Management: Consider using lower atorvastatin doses when used together with diltiazem. Consider therapy modification
Dofetilide: CYP3A4 Inhibitors (Weak) may increase the serum concentration of Dofetilide. Monitor therapy
Dronedarone: May increase the serum concentration of AtorvaSTATin. Monitor therapy
DULoxetine: Blood Pressure Lowering Agents may enhance the hypotensive effect of DULoxetine. Monitor therapy
Duvelisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Efavirenz: May decrease the serum concentration of AtorvaSTATin. Monitor therapy
Elbasvir: May increase the serum concentration of AtorvaSTATin. Management: Limit the dose of atorvastatin to a maximum of 20 mg/day when used together with elbasvir and grazoprevir. Monitor closely for evidence of statin-related toxicities such as myalgia or myopathy. Consider therapy modification
Eltrombopag: May increase the serum concentration of OATP1B1/1B3 (SLCO1B1/1B3) Substrates. Monitor therapy
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Etravirine: May decrease the serum concentration of HMG-CoA Reductase Inhibitors (Statins). This applies to atorvastatin, lovastatin and simvastatin. Monitor therapy
Fenofibrate and Derivatives: May enhance the adverse/toxic effect of HMG-CoA Reductase Inhibitors (Statins). Monitor therapy
Flibanserin: CYP3A4 Inhibitors (Weak) may increase the serum concentration of Flibanserin. Monitor therapy
Fluconazole: May increase the serum concentration of AtorvaSTATin. Monitor therapy
Fosaprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosnetupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosphenytoin: May decrease the serum concentration of HMG-CoA Reductase Inhibitors (Statins). Consider therapy modification
Fosphenytoin: Calcium Channel Blockers may increase the serum concentration of Fosphenytoin. Management: Monitor for phenytoin toxicity with concomitant use of a calcium channel blocker (CCB) or decreased phenytoin effects with CCB discontinuation. Monitor for decreased CCB therapeutic effects. Nimodipine Canadian labeling contraindicates use with phenytoin. Consider therapy modification
Fusidic Acid (Systemic): May enhance the adverse/toxic effect of HMG-CoA Reductase Inhibitors (Statins). Specifically, the risk for muscle toxicities, including rhabdomyolysis may be significantly increased. Management: Avoid concurrent use whenever possible. Use is listed as contraindicated in product characteristic summaries in several countries, although UK labeling suggests that use could be considered under exceptional circumstances and with close supervision. Avoid combination
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Gemfibrozil: May enhance the myopathic (rhabdomyolysis) effect of AtorvaSTATin. Gemfibrozil may increase the serum concentration of AtorvaSTATin. Avoid combination
Glecaprevir and Pibrentasvir: May increase the serum concentration of AtorvaSTATin. Avoid combination
Grapefruit Juice: May increase the serum concentration of HMG-CoA Reductase Inhibitors (Statins). Management: Avoid concurrent use of GFJ with lovastatin or simvastatin. Avoid high quantities of GFJ with atorvastatin. Consider using a lower statin dose or a statin that is less likely to interact when possible. Consider therapy modification
Grazoprevir: May increase the serum concentration of AtorvaSTATin. Management: Limit the dose of atorvastatin to a maximum of 20 mg/day when used together with elbasvir and grazoprevir. Monitor closely for evidence of statin-related toxicities such as myalgia or myopathy. Consider therapy modification
Herbs (Hypertensive Properties): May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Herbs (Hypotensive Properties): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Hypotension-Associated Agents: Blood Pressure Lowering Agents may enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Istradefylline: May increase the serum concentration of AtorvaSTATin. Monitor therapy
Itraconazole: May increase the serum concentration of AtorvaSTATin. Management: Limit atorvastatin to a maximum adult dose of 20 mg/day in patients receiving itraconazole. Assess clinical response to ensure that the lowest necessary dose of atorvastatin is used. Consider use of fluva-, rosuva-, pitava-, or pravastatin when possible. Consider therapy modification
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Ketoconazole (Systemic): AtorvaSTATin may enhance the adverse/toxic effect of Ketoconazole (Systemic). Specifically, there is a theoretical potential for additive effects on reducing endogenous steroid concentrations. Ketoconazole (Systemic) may increase the serum concentration of AtorvaSTATin. Management: Administer ketoconazole with atorvastatin cautiously, and monitor for toxic effects of atorvastatin (e.g., myalgia, rhabdomyolysis, liver function test abnormalities). Consider use of fluva-, rosuva-, pitava-, or pravastatin when possible. Consider therapy modification
Lanthanum: HMG-CoA Reductase Inhibitors (Statins) may decrease the serum concentration of Lanthanum. Management: Administer HMG-CoA reductase inhibitors at least two hours before or after lanthanum. Consider therapy modification
Larotrectinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Ledipasvir: May enhance the adverse/toxic effect of AtorvaSTATin. Monitor therapy
Lemborexant: CYP3A4 Inhibitors (Weak) may increase the serum concentration of Lemborexant. Management: The maximum recommended dosage of lemborexant is 5 mg, no more than once per night, when coadministered with weak CYP3A4 inhibitors. Consider therapy modification
Letermovir: May increase the serum concentration of AtorvaSTATin. Management: Limit the atorvastatin dose to 20 mg daily when combined with letermovir. When letermovir is coadministered with cyclosporine, the use of atorvastatin (at any dose) is not recommended. Consider therapy modification
Levodopa-Containing Products: Blood Pressure Lowering Agents may enhance the hypotensive effect of Levodopa-Containing Products. Monitor therapy
Lomitapide: May increase the serum concentration of AtorvaSTATin. AtorvaSTATin may increase the serum concentration of Lomitapide. Management: When the lomitapide dose is 10 mg daily or greater, reduce the lomitapide dose by 50% when combined with atorvastatin. No dose adjustment is required when the lomitapide dose is 5 mg daily. Consider therapy modification
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Lormetazepam: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Lovastatin: AmLODIPine may increase the serum concentration of Lovastatin. Monitor therapy
Macrolide Antibiotics: May decrease the metabolism of Calcium Channel Blockers. Management: Consider using a noninteracting macrolide. Felodipine Canadian labeling specifically recommends avoiding its use in combination with clarithromycin. Exceptions: Azithromycin (Systemic); Fidaxomicin; Roxithromycin; Spiramycin. Consider therapy modification
Magnesium Salts: Calcium Channel Blockers may enhance the adverse/toxic effect of Magnesium Salts. Magnesium Salts may enhance the hypotensive effect of Calcium Channel Blockers. Monitor therapy
Melatonin: May diminish the antihypertensive effect of Calcium Channel Blockers (Dihydropyridine). Monitor therapy
Methylphenidate: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Midazolam: AtorvaSTATin may increase the serum concentration of Midazolam. Monitor therapy
MiFEPRIStone: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Minimize doses of CYP3A4 substrates, and monitor for increased concentrations/toxicity, during and 2 weeks following treatment with mifepristone. Avoid cyclosporine, dihydroergotamine, ergotamine, fentanyl, pimozide, quinidine, sirolimus, and tacrolimus. Consider therapy modification
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Molsidomine: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Naftopidil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Netupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Neuromuscular-Blocking Agents (Nondepolarizing): Calcium Channel Blockers may enhance the neuromuscular-blocking effect of Neuromuscular-Blocking Agents (Nondepolarizing). Monitor therapy
Niacin: May enhance the adverse/toxic effect of HMG-CoA Reductase Inhibitors (Statins). Monitor therapy
Niacinamide: May enhance the adverse/toxic effect of HMG-CoA Reductase Inhibitors (Statins). Monitor therapy
Nicergoline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicorandil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
NiMODipine: CYP3A4 Inhibitors (Weak) may increase the serum concentration of NiMODipine. Monitor therapy
Nitroprusside: Blood Pressure Lowering Agents may enhance the hypotensive effect of Nitroprusside. Monitor therapy
Obinutuzumab: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Management: Consider temporarily withholding blood pressure lowering medications beginning 12 hours prior to obinutuzumab infusion and continuing until 1 hour after the end of the infusion. Consider therapy modification
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Pentoxifylline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Phenytoin: Calcium Channel Blockers may increase the serum concentration of Phenytoin. Phenytoin may decrease the serum concentration of Calcium Channel Blockers. Management: Avoid use of nimodipine or nifedipine with phenytoin. Monitor for phenytoin toxicity and/or decreased calcium channel blocker effects with any concurrent use. Consider therapy modification
Phenytoin: May decrease the serum concentration of HMG-CoA Reductase Inhibitors (Statins). Consider therapy modification
Pholcodine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Pholcodine. Monitor therapy
Phosphodiesterase 5 Inhibitors: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Pimozide: CYP3A4 Inhibitors (Weak) may increase the serum concentration of Pimozide. Avoid combination
Posaconazole: May increase the serum concentration of AtorvaSTATin. Avoid combination
Prostacyclin Analogues: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Protease Inhibitors: May increase the serum concentration of AtorvaSTATin. Management: See full monograph for recommended dose limits. Avoid atorvastatin with tipranavir/ritonavir. Consider therapy modification
Quinagolide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
QuiNIDine: Calcium Channel Blockers (Dihydropyridine) may decrease the serum concentration of QuiNIDine. Calcium Channel Blockers (Dihydropyridine) may increase the serum concentration of QuiNIDine. QuiNIDine may increase the serum concentration of Calcium Channel Blockers (Dihydropyridine). Monitor therapy
QuiNINE: May increase the serum concentration of HMG-CoA Reductase Inhibitors (Statins). Monitor therapy
Raltegravir: May enhance the myopathic (rhabdomyolysis) effect of HMG-CoA Reductase Inhibitors (Statins). Monitor therapy
Ranolazine: May increase the serum concentration of AtorvaSTATin. Monitor therapy
Red Yeast Rice: May enhance the adverse/toxic effect of HMG-CoA Reductase Inhibitors (Statins). Avoid combination
Repaglinide: HMG-CoA Reductase Inhibitors (Statins) may increase the serum concentration of Repaglinide. Monitor therapy
Rifamycin Derivatives: May decrease the serum concentration of Calcium Channel Blockers. This primarily affects oral forms of calcium channel blockers. Management: The labeling for some US and Canadian calcium channel blockers contraindicate use with rifampin, however recommendations vary. Consult appropriate labeling. Consider therapy modification
Rifamycin Derivatives: May decrease the serum concentration of HMG-CoA Reductase Inhibitors (Statins). Management: Consider use of noninteracting antilipemic agents (note: pitavastatin concentrations may increase with rifamycin treatment). Monitor for altered HMG-CoA reductase inhibitor effects. Rifabutin and fluvastatin, or possibly pravastatin, may pose lower risk. Consider therapy modification
Rupatadine: May enhance the adverse/toxic effect of HMG-CoA Reductase Inhibitors (Statins). Specifically, the risk for increased CPK and/or other muscle toxicities may be increased. Monitor therapy
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: May increase the serum concentration of AtorvaSTATin. Management: The maximum atorvastatin dose should not exceed 40 mg/day with concurrent use of simeprevir, and use of the lowest necessary atorvastatin dose is recommended. Consider therapy modification
Simvastatin: AmLODIPine may increase the serum concentration of Simvastatin. Management: Avoid the concurrent use of amlodipine with simvastatin when possible. If used together, avoid doses of simvastatin greater than 20 mg/day (for adults). Consider therapy modification
Sincalide: Drugs that Affect Gallbladder Function may diminish the therapeutic effect of Sincalide. Management: Consider discontinuing drugs that may affect gallbladder motility prior to the use of sincalide to stimulate gallbladder contraction. Consider therapy modification
Spironolactone: AtorvaSTATin may enhance the adverse/toxic effect of Spironolactone. Specifically, there is a theoretical potential for enhanced effects on reducing endogenous steroid activity. Monitor therapy
St John's Wort: May increase the metabolism of HMG-CoA Reductase Inhibitors (Statins). Management: Consider avoiding the concomitant administration of St Johns Wort with interacting HMG-CoA reductase inhibitors in order to avoid the potential for decreased antilipemic effects. Monitor for decreased effects during concomitant therapy. Consider therapy modification
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
Tacrolimus (Systemic): Calcium Channel Blockers (Dihydropyridine) may increase the serum concentration of Tacrolimus (Systemic). Monitor therapy
Telithromycin: May increase the serum concentration of AtorvaSTATin. Management: Consider limiting atorvastatin to a max (adult) dose of 20 mg/day when used with telithromycin. Although not a specific recommendation in atorvastatin labeling, this is consistent with dosing for other strong CYP3A4 inhibitors, including clarithromycin. Consider therapy modification
Teriflunomide: May increase the serum concentration of OATP1B1/1B3 (SLCO1B1/1B3) Substrates. Monitor therapy
Ticagrelor: May increase the serum concentration of AtorvaSTATin. Monitor therapy
Tipranavir: May increase the serum concentration of AtorvaSTATin. Avoid combination
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Tolvaptan: May increase the serum concentration of OATP1B1/1B3 (SLCO1B1/1B3) Substrates. Consider therapy modification
Trabectedin: HMG-CoA Reductase Inhibitors (Statins) may enhance the myopathic (rhabdomyolysis) effect of Trabectedin. Monitor therapy
Triazolam: CYP3A4 Inhibitors (Weak) may increase the serum concentration of Triazolam. Management: Consider triazolam dose reduction in patients receiving concomitant weak CYP3A4 inhibitors. Consider therapy modification
Ubrogepant: CYP3A4 Inhibitors (Weak) may increase the serum concentration of Ubrogepant. Management: In patients taking weak CYP3A4 inhibitors, the initial and second dose (if needed) of ubrogepant should be limited to 50 mg. Consider therapy modification
Velpatasvir: May increase the serum concentration of AtorvaSTATin. Monitor therapy
Verapamil: AtorvaSTATin may increase the serum concentration of Verapamil. Verapamil may increase the serum concentration of AtorvaSTATin. Management: Consider using lower atorvastatin doses when used together with verapamil. Consider therapy modification
Voriconazole: May increase the serum concentration of AtorvaSTATin. Management: Monitor for toxic effects of atorvastatin (e.g., myalgia, rhabdomyolysis, liver function test abnormalities) during concomitant treatment, and reduce atorvastatin dose when possible. Consider use of fluva-, rosuva-, pitava-, or pravastatin when possible. Consider therapy modification
Voxilaprevir: May increase the serum concentration of HMG-CoA Reductase Inhibitors (Statins). Management: Use the lowest statin dose possible if combined with voxilaprevir and monitor patients for increased statin effects/toxicities. Avoid concomitant use of voxilaprevir with rosuvastatin or pitavastatin, and limit pravastatin doses to 40 mg daily. Consider therapy modification
Yohimbine: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Adverse Reactions
See individual agents.
Warnings/Precautions
Concerns related to adverse effects:
- Angina/myocardial infarction: Increased angina and/or myocardial infarction (MI) has occurred with initiation or dosage titration of dihydropyridine calcium channel blockers. Reflex tachycardia may occur resulting in angina and/or MI in patients with obstructive coronary disease especially in the absence of concurrent beta-blockade.
- Diabetes mellitus: Increases in HbA1c and fasting blood glucose have been reported.
- Hepatotoxicity: Persistent elevations in serum transaminases have been reported; upon dose reduction, drug interruption, or discontinuation, transaminase levels returned to or near pretreatment levels. Postmarketing reports of fatal and nonfatal hepatic failure with atorvastatin have been reported and are rare. If serious hepatotoxicity with clinical symptoms and/or hyperbilirubinemia or jaundice occurs during treatment, interrupt therapy promptly. If an alternate etiology is not identified, do not restart atorvastatin. Liver enzyme tests should be obtained at baseline and as clinically indicated if signs/symptoms of liver injury occur. Ethanol may enhance the potential of adverse hepatic effects; instruct patients to avoid excessive ethanol consumption.
- Hypotension/syncope: Symptomatic hypotension with or without syncope can rarely occur with amlodipine; blood pressure must be lowered at a rate appropriate for the patient's clinical condition.
- Myopathy/rhabdomyolysis: Rhabdomyolysis with acute renal failure secondary to myoglobinuria and/or myopathy has been reported; patients should be monitored closely. This risk is dose-related and is increased with concurrent use of CYP3A4 inhibitors; if concurrent use is warranted, consider lower starting and maintenance doses of atorvastatin. Use caution in patients with inadequately treated hypothyroidism and those taking other drugs associated with myopathy (eg, colchicine); these patients are predisposed to myopathy. Immune-mediated necrotizing myopathy associated with HMG-CoA reductase inhibitors use has also been reported. Patients should be instructed to report unexplained muscle pain, tenderness, weakness, or brown urine, particularly if accompanied by malaise or fever. Discontinue therapy if markedly elevated CPK levels occur or if myopathy is suspected/diagnosed.
- Peripheral edema: The most common side effect of amlodipine is peripheral edema (dose dependent); occurs within 2 to 3 weeks of starting therapy.
Disease-related concerns:
- Aortic stenosis: Use amlodipine with extreme caution in patients with severe aortic stenosis; may reduce coronary perfusion resulting in ischemia.
- Hepatic impairment and/or ethanol use: Use atorvastatin with caution in patients who consume large amounts of ethanol or have a history of liver disease; use is contraindicated in patients with active liver disease or unexplained persistent elevations of serum transaminases. Use amlodipine with caution in patients with hepatic impairment; may require lower starting dose; titrate slowly in patients with severe hepatic impairment.
- Hypertrophic cardiomyopathy with outflow tract obstruction: Use amlodipine with caution in patients with hypertrophic cardiomyopathy and outflow tract obstruction since reduction in afterload may worsen symptoms associated with this condition (ACCF/AHA [Gersh 2011]).
- Renal impairment: Use atorvastatin with caution in patients with renal impairment; these patients are predisposed to myopathy.
- Stroke: Patients with recent stroke or transient ischemic attack receiving long-term therapy with high-dose (ie, 80 mg/day) atorvastatin may be at increased risk for hemorrhagic stroke (SPARCL Investigators, 2006). A subsequent post-hoc analysis demonstrated that patients with lacunar or hemorrhagic stroke may be at higher risk of hemorrhagic stroke; however, this finding was determined to be hypothesis generating. The overall benefit of treatment with atorvastatin (ie, reduced risk of stroke and cardiovascular events) in this population seems to outweigh the increased risk of hemorrhagic stroke if one truly exists (Goldstein 2008).
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information
Special populations:
- Elderly: Use atorvastatin with caution in patients with advanced age, these patients are predisposed to myopathy.
- Surgical patients: The manufacturer recommends temporary discontinuation for elective major surgery, acute medical or surgical conditions, or in any patient experiencing an acute, serious condition suggestive of a myopathy or having a risk factor predisposing to rhabdomyolysis (eg, sepsis, hypotension, trauma, uncontrolled seizures, severe metabolic, endocrine, or electrolyte disorders). Based on current research and clinical guidelines, HMG-CoA reductase inhibitors should be continued in the perioperative period for noncardiac and cardiac surgery (ACC/AHA [Fleisher 2014]; ACC/AHA [Hillis 2011]). Perioperative discontinuation of statin therapy is associated with an increased risk of cardiac morbidity and mortality.
Other warnings/precautions:
- Appropriate use: Secondary causes of hyperlipidemia should be ruled out prior to therapy with atorvastatin. Atorvastatin has not been studied when the primary lipid abnormality is chylomicron elevation (Fredrickson types I and V).
- Titration: Dosage titration of amlodipine should occur after 7 to 14 days on a given dose.
Monitoring Parameters
Amlodipine: Blood pressure, heart rate
Atorvastatin:
2013 ACC/AHA Blood Cholesterol Guideline recommendations (ACC/AHA [Stone 2013]):
Lipid panel (total cholesterol, HDL, LDL, triglycerides): Baseline lipid panel; fasting lipid profile within 4 to 12 weeks after initiation or dose adjustment and every 3 to 12 months (as clinically indicated) thereafter. If 2 consecutive LDL levels are <40 mg/dL, consider decreasing the dose.
Hepatic transaminase levels: Baseline measurement of hepatic transaminase levels (ie, ALT); measure hepatic function if symptoms suggest hepatotoxicity (eg, unusual fatigue or weakness, loss of appetite, abdominal pain, dark-colored urine or yellowing of skin or sclera) during therapy.
CPK: CPK should not be routinely measured. Baseline CPK measurement is reasonable for some individuals (eg, family history of statin intolerance or muscle disease, clinical presentation, concomitant drug therapy that may increase risk of myopathy). May measure CPK in any patient with symptoms suggestive of myopathy (pain, tenderness, stiffness, cramping, weakness, or generalized fatigue).
Evaluate for new-onset diabetes mellitus during therapy; if diabetes develops, continue statin therapy and encourage adherence to a heart-healthy diet, physical activity, a healthy body weight, and tobacco cessation.
If patient develops a confusional state or memory impairment, may evaluate patient for nonstatin causes (eg, exposure to other drugs), systemic and neuropsychiatric causes, and the possibility of adverse effects associated with statin therapy.
Manufacturer's labeling: Liver enzyme tests at baseline and repeated when clinically indicated. Measure CPK when myopathy is being considered or may measure CPK periodically in high risk patients (eg, drug-drug interaction). Upon initiation or titration, lipid panel should be analyzed within 2 to 4 weeks.
Pregnancy
Pregnancy Considerations
Use is contraindicated in pregnancy.
Effective contraception should be used during treatment in females of reproductive potential.
See individual agents for additional information.
Patient Education
What is this drug used for?
- It is used to treat high blood pressure.
- It is used to lower bad cholesterol and raise good cholesterol (HDL).
- It is used to lower triglycerides.
- It is used to treat some types of chest pain (angina).
- It is used to lower the chance of heart attack, stroke, and death in some people.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Diarrhea
- Joint pain
- Nausea
- Stuffy nose
- Loss of strength and energy
- Painful extremities
- Sore throat
- Trouble sleeping
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Urinary tract infection like blood in the urine, burning or painful urination, passing a lot of urine, fever, lower abdominal pain, or pelvic pain
- Severe dizziness
- Passing out
- Shortness of breath
- Excessive weight gain
- Swelling of arms or legs
- Chest pain
- Muscle pain
- Muscle weakness
- Stiff muscles
- Tremors
- Abnormal movements
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin
- Severe cerebrovascular disease like change in strength on one side is greater than the other, trouble speaking or thinking, change in balance, or vision changes
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.