Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
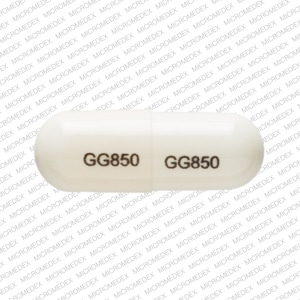
Capsule, Oral:
Generic: 250 mg [DSC], 500 mg
Solution Reconstituted, Injection, as sodium [strength expressed as base]:
Generic: 250 mg (1 ea [DSC]); 500 mg (1 ea [DSC]); 1 g (1 ea [DSC]); 2 g (1 ea [DSC])
Solution Reconstituted, Injection, as sodium [strength expressed as base, preservative free]:
Generic: 125 mg (1 ea); 250 mg (1 ea); 500 mg (1 ea); 1 g (1 ea); 2 g (1 ea)
Solution Reconstituted, Intravenous, as sodium [strength expressed as base, preservative free]:
Generic: 1 g (1 ea); 2 g (1 ea); 10 g (1 ea)
Suspension Reconstituted, Oral:
Generic: 125 mg/5 mL (100 mL [DSC], 200 mL [DSC]); 250 mg/5 mL (100 mL [DSC], 200 mL [DSC])
Pharmacology
Mechanism of Action
Inhibits bacterial cell wall synthesis by binding to one or more of the penicillin-binding proteins (PBPs) which in turn inhibits the final transpeptidation step of peptidoglycan synthesis in bacterial cell walls, thus inhibiting cell wall biosynthesis. Bacteria eventually lyse due to ongoing activity of cell wall autolytic enzymes (autolysins and murein hydrolases) while cell wall assembly is arrested.
Pharmacokinetics/Pharmacodynamics
Absorption
Oral: 50%
Distribution
Into bile; penetration into CSF occurs with inflamed meninges only
Excretion
Urine (∼90%, unchanged within 24 hours); feces
Time to Peak
Serum concentration: Oral: Within 1 to 2 hours
Half-Life Elimination
Neonates:
PNA 2 to 7 days: 4 hours
PNA 8 to 14 days: 2.8 hours
PNA 15 to 30 days: 1.7 hours
Children and Adults: 1 to 1.8 hours (Bergan 1978)
Anuric patients: 8 to 20 hours
Protein Binding
Neonates: 10%; Adults: 15% to 18%
Use: Labeled Indications
Oral:
GI tract infections: Treatment of GI tract infections caused by Shigella, Salmonella typhosa and other Salmonella, Escherichia coli, Proteus mirabilis, and enterococci. Note: Ampicillin is not recommended as a first-line agent for shigellosis, salmonellosis (nontyphoid), or Salmonella enterica species (typhoid fever) due to development of resistance (CDC 2014).
GU tract infections: Treatment of GU tract infections caused by E. coli, P. mirabilis, enterococci, Shigella, S. typhosa and other Salmonella, and nonpenicillinase-producing Neisseria gonorrhoeae. Note: Ampicillin is not recommended by the CDC as a first-line agent in the treatment of gonorrhea (CDC 2010).
Respiratory tract infections: Treatment of respiratory tract infections caused by nonpenicillinase-producing Haemophilus influenzae and staphylococci, and streptococci, including Streptococcus pneumoniae.
Injection:
Bloodstream infection: Treatment of bloodstream infection caused by susceptible gram-positive organisms, including Streptococcus species, penicillin G-susceptible staphylococci, and enterococci; gram-negative bloodstream infection caused by E. coli, P. mirabilis, and Salmonella species.
Endocarditis, treatment: Treatment of endocarditis caused by susceptible gram-positive organisms, including Streptococcus species, penicillin G-susceptible staphylococci, and enterococci.
GI infections: Treatment of GI infections caused by S. typhi (typhoid fever), other Salmonella species, and Shigella species (dysentery). Note: Ampicillin is not recommended as a first-line agent for shigellosis, salmonellosis (nontyphoid), or S. enterica species (typhoid fever) due to development of resistance (CDC 2014).
Meningitis, bacterial: Treatment of bacterial meningitis caused by E. coli, group B streptococci, and other gram-negative bacteria (Neisseria meningitidis).
Respiratory tract infections: Treatment of respiratory tract infections caused by S. pneumoniae, Staphylococcus aureus (penicillinase and nonpenicillinase producing), H. influenzae, and group A beta-hemolytic streptococci.
Urinary tract infections: Treatment of urinary tract infections caused by E. coli and P. mirabilis.
Use: Off Label
Endocarditis, prophylaxis (dental or invasive respiratory tract procedures)yes
Based on the American Heart Association (AHA) guidelines for the prevention of infective endocarditis, ampicillin is effective and recommended for patients with certain cardiac conditions who are unable to take oral medication to provide prophylaxis against infective endocarditis associated with dental or respiratory tract procedures.
Intra-amniotic infection (chorioamnionitis)yes
Based on the American College of Obstetricians and Gynecologists (ACOG) guidelines on intrapartum management of intra-amniotic infection, ampicillin is an effective and recommended agent to treat intra-amniotic infection.
Osteomyelitis and/or discitis, treatmentyes
Based on the Infectious Diseases Society of America (IDSA) guidelines for the diagnosis and treatment of native vertebral osteomyelitis in adults, ampicillin is an effective and recommended agent for the treatment of native vertebral osteomyelitis due to penicillin-susceptible Enterococcus or Streptococcus species.
Peritonitis, treatment (peritoneal dialysis patients)yes
Based on the International Society for Peritoneal Dialysis peritonitis recommendations: 2016 update on prevention and treatment, intraperitoneal ampicillin is an effective and recommended agent as pathogen-directed therapy for peritonitis associated with peritoneal dialysis.
Postpartum endometritisc
Data from a limited number of patients studied suggest ampicillin may be beneficial for the treatment of postpartum endometritis Brumfield 2000.
Prosthetic joint infectionyes
Based on the IDSA guidelines for the diagnosis and management of prosthetic joint infection, ampicillin is an effective and recommended agent for the treatment of prosthetic joint infection with penicillin-susceptible Enterococcus spp.
Streptococcus (group B), maternal prophylaxis for prevention of neonatal diseaseyes
Based on the ACOG guidelines on prevention of group B streptococcal early-onset disease in newborns, ampicillin is an effective and recommended alternative agent at the onset of labor and until delivery in mothers colonized with group B streptococcus (neonatal prophylaxis).
Surgical prophylaxisyes
Based on the American Society of Health-System Pharmacists, IDSA, Surgical Infection Society, and Society of Healthcare Epidemiology of America guidelines for antimicrobial prophylaxis in surgery, ampicillin is an effective and recommended agent for perioperative surgical prophylaxis.
Tubo-ovarian abscessyes
Based on the Centers for Disease Control and Prevention sexually transmitted diseases treatment guidelines, ampicillin is an effective and recommended agent for the treatment of tubo-ovarian abscess.
Contraindications
Hypersensitivity (eg, anaphylaxis) to ampicillin, any component of the formulation, or other penicillins; infections caused by penicillinase-producing organisms
Dosage and Administration
Dosing: Adult
Note: For oral therapy, including oral step-down therapy after IV ampicillin, oral amoxicillin is usually preferred over oral ampicillin due to improved bioavailability and absorption (bioavailability 77% versus 39% to 54%, respectively) (Arancibia 1980; Bolme 1976). For ease of outpatient IV ampicillin administration, the total daily dose may be administered as a 24-hour continuous infusion (IDSA [Berbari 2015]; IDSA [Osmon 2013]; Lewis 2018; Ogawa 2014).
Bloodstream infection:
Pathogen-directed therapy for Enterococcus spp.: IV: 2 g every 4 hours; use as part of an appropriate combination regimen in the setting of suspected endocarditis or critical illness (Graninger 1992; IDSA [Mermel 2009]; Murray 2019). Duration of therapy is 7 to 14 days for uncomplicated infection (ie, fever resolution within 72 hours and absence of metastatic focus of infection or endovascular hardware) (IDSA [Mermel 2009]). Some experts recommend a duration of 5 to 7 days for uncomplicated infection with rapid blood culture clearance (within 24 hours) and in the absence of metastatic infection (Murray 2019).
Pathogen-directed therapy for Listeria monocytogenes: IV: 2 g every 4 hours; use in combination with gentamicin for nonpregnant patients. Duration should be individualized based on patient factors, source and extent of infection, and clinical response, but ampicillin is usually continued for at least 14 to 21 days (Charlier 2017; Gelfand 2019; Hof 1997).
Endocarditis, prophylaxis (dental or invasive respiratory tract procedures) (alternative agent for patients unable to take oral therapy) (off-label use): IM, IV: 2 g as a single dose 30 to 60 minutes before procedure. Note: Only recommended for patients with cardiac conditions associated with the highest risk of an adverse outcome from endocarditis and who are undergoing a procedure likely to result in bacteremia with an organism that has the potential ability to cause endocarditis (AHA [Wilson 2007]).
Endocarditis, treatment:
Enterococcus faecalis, native or prosthetic valve (penicillin-susceptible): IV: 2 g every 4 hours as part of an appropriate combination regimen (eg, with ceftriaxone or gentamicin). Duration is usually 6 weeks; for patients with native valve endocarditis and symptoms <3 months, the combination of ampicillin and gentamicin can be given for 4 weeks. Note: Ampicillin plus ceftriaxone is the preferred regimen in patients with or at risk of renal insufficiency or with gentamicin resistance (AHA [Baddour 2015]; Fernández-Hidalgo 2013; Sexton 2019), and some experts favor this combination for all patients with native valve endocarditis (Sexton 2019).
HACEK organisms, native or prosthetic valve (ampicillin-susceptible) (off-label use): IV: 2 g every 4 hours for 4 weeks (native valve) or 6 weeks (prosthetic valve) (AHA [Baddour 2015]). Note: In vitro susceptibility should be confirmed prior to use.
Viridans group streptococci and Streptococcus gallolyticus (Streptococcus bovis) (alternative agent):
Native valve: Highly penicillin-susceptible (minimum inhibitory concentration [MIC] ≤0.12 mcg/mL): IV: 2 g every 4 hours for 4 weeks (AHA [Baddour 2015]).
Native valve: Relatively penicillin-resistant (MIC >0.12 to <0.5 mcg/mL): IV: 2 g every 4 hours for 4 weeks in combination with gentamicin for the first 2 weeks (AHA [Baddour 2015]).
Native valve: Penicillin-resistant (MIC ≥0.5 mcg/mL): IV: 2 g every 4 hours in combination with gentamicin. The duration of this regimen is not well established; infectious diseases consultation recommended (AHA [Baddour 2015]).
Prosthetic valve: Highly penicillin-susceptible (MIC ≤0.12 mcg/mL): IV: 2 g every 4 hours for 6 weeks (with or without concomitant gentamicin for the first 2 weeks) (AHA [Baddour 2015]).
Prosthetic valve: Relatively penicillin-resistant (MIC >0.12 to <0.5 mcg/mL) or fully penicillin-resistant (MIC ≥0.5 mcg/mL): IV: 2 g every 4 hours in combination with gentamicin for 6 weeks (AHA [Baddour 2015]). For relatively resistant strains, some experts prefer a shorter duration of the gentamicin component (≥2 weeks) (Karchmer 2019).
Intra-abdominal infection (off-label use): Empiric or pathogen-directed therapy for Enterococcus spp. in high-risk patients (eg, postoperative infection or healthcare-associated infection in patients with prior use of antibiotics that select for Enterococcus, immunocompromising condition, valvular heart disease, or prosthetic intravascular material):
IV: 2 g every 4 hours as part of an appropriate combination regimen (Barshak 2019; SIS [Mazuski 2017]). Total duration of therapy (which may include oral step-down therapy) is 4 to 7 days following adequate source control (SIS [Mazuski 2017]; SIS/IDSA [Solomkin 2010]); for infections managed without surgical or percutaneous intervention, a longer duration may be necessary (Barshak 2019).
Meningitis, bacterial: As a component of empiric therapy (community-acquired infections in immunocompetent patients >50 years of age and immunocompromised patients) or pathogen-directed therapy (eg, Haemophilus influenzae [beta-lactamase negative], L. monocytogenes, Neisseria meningitidis [penicillin MIC <0.1 mcg/mL], Streptococcus agalactiae, Streptococcus pneumoniae [penicillin MIC ≤0.06 mcg/mL], Enterococcus spp. [ampicillin-susceptible]):
IV: 2 g every 4 hours; for empiric therapy and for directed therapy for Enterococcus or Listeria, use as part of an appropriate combination regimen. Treatment duration is 7 to 21 days, depending on causative pathogen(s) and clinical response (IDSA [Tunkel 2004]; IDSA [Tunkel 2017]).
Osteomyelitis and/or discitis, treatment (off-label use): Pathogen-directed therapy for penicillin-susceptible Enterococcus or Streptococcus spp.: IV: 2 g every 4 hours or 12 g as a continuous infusion every 24 hours, generally for ≥6 weeks. Shorter courses are appropriate if the affected bone is completely resected (eg, by amputation) (IDSA [Berbari 2015]; Osmon 2019). For Enterococcus, some experts use with ceftriaxone in the setting of retained hardware (Osmon 2019).
Pelvic infections (off-label use):
Intra-amniotic infection (chorioamnionitis): IV: 2 g every 6 hours in combination with gentamicin. In females undergoing cesarean delivery, an anti-anaerobic agent should also be added. Continue regimen until vaginal delivery or for 1 dose after cesarean delivery (ACOG 2017). Note: Some experts recommend 1 additional dose after vaginal delivery and extension of antibiotics after cesarean delivery until patient is afebrile and asymptomatic ≥48 hours (Tita 2019).
Postpartum endometritis: Note: For patients known to be colonized with GBS (Chen 2019).
IV: 2 g every 6 hours in combination with clindamycin and gentamicin; treat until patient is clinically improved (no fundal tenderness) and afebrile for 24 to 48 hours (Brumfield 2000; Chen 2019).
Tubo-ovarian abscess: IV: 2 g every 6 hours in combination with clindamycin and gentamicin (Beigi 2019). After 24 to 48 hours of sustained clinical improvement, may transition to oral therapy to complete ≥14 days of treatment (CDC [Workowski 2015]).
Peritonitis, treatment (peritoneal dialysis patients) (off-label use): Note: Intraperitoneal administration is preferred to IV administration (ISPD [Li 2016]). Consider a 25% dose increase in patients with significant residual renal function (urine output >100 mL/day) (ISPD [Li 2010]; ISPD [Li 2016]; Mancini 2018; Szeto 2018).
Pathogen-directed therapy (eg, Enterococcus spp., Streptococcus spp.): Continuous (with every exchange): Intraperitoneal: 125 mg/L of dialysate with each exchange (ISPD [Li 2016]). Duration of therapy is ≥2 weeks for patients with adequate clinical response (Burkart 2019; ISPD [Li 2016]).
Prosthetic joint infection (off-label use): Pathogen-directed therapy (eg, penicillin-susceptible Enterococcus spp. or Streptococcus spp.): IV: 2 g every 4 hours or 12 g continuous infusion every 24 hours. Duration varies, but is generally 4 to 6 weeks; for enterococcal infections, some experts use with ceftriaxone in the setting of retained hardware (Berbari 2019; IDSA [Osmon 2013]).
Streptococcus (group B), maternal prophylaxis for prevention of neonatal disease (alternative agent) (off-label use): Note: Prophylaxis is reserved for pregnant women with a positive group B Streptococcus (GBS) vaginal or rectal screen in late gestation; GBS bacteriuria during the current pregnancy; history of birth of an infant with early-onset GBS disease; and unknown GBS culture status with any of the following: birth <37 0/7 weeks' gestation, intrapartum fever, prolonged rupture of membranes, known GBS positive in a previous pregnancy, or intrapartum nucleic acid amplification testing positive for GBS (ACOG 2019).
IV: 2 g as a single dose at onset of labor or prelabor rupture of membranes, then 1 g every 4 hours until delivery (ACOG 2019).
Urinary tract infection: Note: Uncomplicated urinary tract infection (UTI) has traditionally been defined as infection in an otherwise healthy nonpregnant female with a normal urinary tract; UTI in other patient populations has been considered complicated. Some experts instead categorize UTI as either acute simple cystitis (mild infection limited to the bladder with no signs/symptoms of upper tract or systemic infection in a nonpregnant adult) or complicated UTI (pyelonephritis or cystitis symptoms with other signs/symptoms of systemic infection) (Hooton 2019a; Hooton 2019b; Hooton 2019c). Ampicillin is not recommended for empiric therapy given decreased efficacy compared to first-line agents and high prevalence of resistance (IDSA/ESCMID [Gupta 2011]).
Acute uncomplicated or simple cystitis due to Enterococcus spp.: Oral: 500 mg every 6 hours for 5 to 7 days (Hooton 2019a; Hooton 2019b; IDSA/ESCMID [Gupta 2011]; Shah 2018).
Acute pyelonephritis or other complicated urinary tract infection due to Enterococcus spp. (off label): IV: 1 to 2 g every 4 to 6 hours; can give with an aminoglycoside for critical illness (Cole 2015; Heintz 2010; IDSA/ESCMID [Gupta 2011]). Switch to an appropriate oral regimen once patient has improvement in symptoms. Duration of therapy depends on the antimicrobial chosen to complete the regimen and ranges from 5 to 14 days (Hooton 2019c).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
General dosing, susceptible infection (Bradley 2019; Red Book [AAP 2018]): Infants, Children, and Adolescents:
Mild to moderate infection:
Oral: 50 to 100 mg/kg/day divided every 6 hours; maximum daily dose: 2,000 mg/day.
IM, IV: 50 to 200 mg/kg/day divided every 6 hours; maximum daily dose: 8 g/day.
Severe infection (eg, meningitis, endocarditis): IM, IV: 300 to 400 mg/kg/day divided every 4 to 6 hours; maximum daily dose: 12 g/day.
Community-acquired pneumonia (CAP) (IDSA/PIDS [Bradley 2011]): Infants >3 months, Children, and Adolescents: Note: May consider addition of vancomycin or clindamycin to empiric therapy if community-acquired MRSA suspected. In children ≥5 years, a macrolide antibiotic should be added if atypical pneumonia cannot be ruled out.
Empiric treatment or S. pneumoniae (MICs for penicillin ≤2 mcg/mL) or H. influenzae (beta-lactamase negative) in fully immunized patients: IV: 150 to 200 mg/kg/day divided every 6 hours.
Group A Streptococcus: IV: 200 mg/kg/day divided every 6 hours.
S. pneumoniae (MICs for penicillin ≥4 mcg/mL): IV: 300 to 400 mg/kg/day divided every 6 hours.
Endocarditis:
Treatment: Children and Adolescents: IV: 200 to 300 mg/kg/day divided every 4 to 6 hours; maximum daily dose: 12 g/day; use in combination with other antibiotics for at least 4 weeks; some organisms may require longer duration (AHA [Baltimore 2015]).
Prophylaxis: Note: AHA guidelines (Baltimore 2015) limit the use of prophylactic antibiotics to patients at the highest risk for infective endocarditis (IE) or adverse outcomes (eg, prosthetic heart valves, patients with previous IE, unrepaired cyanotic congenital heart disease, repaired congenital heart disease with prosthetic material or device during first 6 months after procedure, repaired congenital heart disease with residual defects at the site or adjacent to site of prosthetic patch or device, and heart transplant recipients with cardiac valvulopathy):
Dental or oral procedures or respiratory tract procedures (eg, tonsillectomy, adenoidectomy): Infants, Children, and Adolescents: IV, IM: 50 mg/kg within 30 to 60 minutes before procedure; maximum dose: 2,000 mg/dose. Intramuscular (IM) injections should be avoided in patients who are receiving anticoagulant therapy. In these circumstances, orally administered regimens should be used whenever possible. Intravenously (IV) administered antibiotics should be used for patients who are unable to tolerate or absorb oral medications (Wilson 2007).
Intra-abdominal infection, complicated: Infants, Children, and Adolescents: IV: 200 mg/kg/day divided every 6 hours; maximum single dose: 2,000 mg; maximize doses if undrained abdominal abscesses (IDSA [Solomkin 2010]).
Meningitis (including health care-associated meningitis and ventriculitis): Infants, Children, and Adolescents: IV: 300 to 400 mg/kg/day divided every 4 to 6 hours; maximum daily dose: 12 g/day (Bradley 2019; IDSA [Tunkel 2004]; IDSA [Tunkel 2017]; Red Book [AAP 2018]).
Peritonitis (CAPD) Limited data available: Infants, Children, and Adolescents: Intraperitoneal: 125 mg per liter of dialysate for 2 weeks (ISPD [Warady 2012]).
Surgical prophylaxis: Infants, Children, and Adolescents: IV: 50 mg/kg within 60 minutes prior to surgical incision; may repeat in 2 hours if lengthy procedure or excessive blood loss; maximum dose: 2,000 mg/dose (ASHP/IDSA [Bratzler 2013]; Red Book [AAP 2018]).
Reconstitution
IM: Dissolve contents of vial in sterile water for injection or bacteriostatic water for injection; final concentration for IM injection is 125 mg/mL or 250 mg/mL. Solutions for IM injection should be freshly prepared and used within 1 hour.
IV:
Direct IV use: Dissolve contents of 125 mg, 250 mg, or 500 mg vial in 5 mL SWFI or bacteriostatic water for injection. Alternatively, dissolve contents of 1 g or 2 g vial in 7.4 or 14.8 mL SWFI or bacteriostatic water for injection, respectively.
Intermittent infusion: Minimum volume: Concentration should not exceed 30 mg/mL due to concentration-dependent stability restrictions. Usual diluent: 500 mg/50 mL NS; 1 g/50 mL NS; 2 g/100 mL NS.
Administration
Administer around-the-clock to promote less variation in peak and trough serum levels.
Oral: Administer on an empty stomach with a full glass (8 oz) of water (ie, 30 minutes prior to or 2 hours after meals) to increase total absorption.
IM.: Inject deep IM into a large muscle mass
IV: Direct IV bolus: Administer over 3 to 5 minutes (125 to 500 mg) or over 10 to 15 minutes (1 to 2 g). More rapid infusion may cause seizures.
Infusion: Rapid infusion may cause seizures. Adjust rate of infusion so that the total dose is administered before admixture stability expires.
Dietary Considerations
Take on an empty stomach 30 minutes before or 2 hours after meals. Some products may contain sodium.
Storage
Oral:
Capsules: Store at 20°C to 25°C (68°F to 77°F).
Oral suspension: Store dry powder at 20°C to 25°C (68°F to 77°F). Once reconstituted, oral suspension is stable for 14 days under refrigeration.
IV:
Store intact vials at 20°C to 25°C (68°F to 77°F).
Solutions for IM or direct IV should be used within 1 hour.
Stability of parenteral admixture in NS at 25°C (77°F) is 8 hours (concentrations up to 30 mg/mL) and at 4°C (39°F) is 24 hours (concentration of 30 mg/mL) or 48 hours (concentrations up to 20 mg/mL). Protect from freezing.
Ampicillin Images
Drug Interactions
Acemetacin: May increase the serum concentration of Penicillins. Monitor therapy
Allopurinol: May enhance the potential for allergic or hypersensitivity reactions to Ampicillin. Monitor therapy
Atenolol: Ampicillin may decrease the bioavailability of Atenolol. Monitor therapy
BCG (Intravesical): Antibiotics may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCG Vaccine (Immunization): Antibiotics may diminish the therapeutic effect of BCG Vaccine (Immunization). Monitor therapy
Chloroquine: May decrease the serum concentration of Ampicillin. Management: Chloroquine prescribing information recommends separating administration of ampicillin and chloroquine by at least 2 hours to minimize any potential negative impact of chloroquine on ampicillin bioavailability. Consider therapy modification
Cholera Vaccine: Antibiotics may diminish the therapeutic effect of Cholera Vaccine. Management: Avoid cholera vaccine in patients receiving systemic antibiotics, and within 14 days following the use of oral or parenteral antibiotics. Avoid combination
Dichlorphenamide: Penicillins may enhance the hypokalemic effect of Dichlorphenamide. Monitor therapy
Lactobacillus and Estriol: Antibiotics may diminish the therapeutic effect of Lactobacillus and Estriol. Monitor therapy
Lanthanum: May decrease the serum concentration of Ampicillin. Management: Administer oral ampicillin at least two hours before or after lanthanum. Consider therapy modification
Methotrexate: Penicillins may increase the serum concentration of Methotrexate. Monitor therapy
Mycophenolate: Penicillins may decrease serum concentrations of the active metabolite(s) of Mycophenolate. This effect appears to be the result of impaired enterohepatic recirculation. Monitor therapy
Probenecid: May increase the serum concentration of Penicillins. Monitor therapy
Sodium Picosulfate: Antibiotics may diminish the therapeutic effect of Sodium Picosulfate. Management: Consider using an alternative product for bowel cleansing prior to a colonoscopy in patients who have recently used or are concurrently using an antibiotic. Consider therapy modification
Tetracyclines: May diminish the therapeutic effect of Penicillins. Monitor therapy
Typhoid Vaccine: Antibiotics may diminish the therapeutic effect of Typhoid Vaccine. Only the live attenuated Ty21a strain is affected. Management: Vaccination with live attenuated typhoid vaccine (Ty21a) should be avoided in patients being treated with systemic antibacterial agents. Use of this vaccine should be postponed until at least 3 days after cessation of antibacterial agents. Consider therapy modification
Vitamin K Antagonists (eg, warfarin): Penicillins may enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Test Interactions
May interfere with urinary glucose tests using cupric sulfate (Benedict's solution, Clinitest®)
Some penicillin derivatives may accelerate the degradation of aminoglycosides in vitro, leading to a potential underestimation of aminoglycoside serum concentration.
Adverse Reactions
Frequency not defined.
Central nervous system: Brain disease (penicillin-induced), glossalgia, seizure, sore mouth
Dermatologic: Erythema multiforme, exfoliative dermatitis, skin rash, urticaria
Note: Appearance of a rash should be carefully evaluated to differentiate (if possible) nonallergic ampicillin rash from hypersensitivity reaction. Incidence is higher in patients with viral infection, Salmonella infection, lymphocytic leukemia, or patients that have hyperuricemia.
Gastrointestinal: Diarrhea, enterocolitis, glossitis, melanoglossia, nausea, oral candidiasis, pseudomembranous colitis, stomatitis, vomiting
Hematologic & oncologic: Agranulocytosis, anemia, eosinophilia, hemolytic anemia, immune thrombocytopenia, leukopenia
Hepatic: Increased serum AST
Hypersensitivity: Anaphylaxis
Immunologic: Serum sickness-like reaction
Renal: Interstitial nephritis (rare)
Respiratory: Stridor
Miscellaneous: Fever
<1%, postmarketing, and/or case reports: Dysgeusia (Syed 2016)
Warnings/Precautions
Concerns related to adverse effects:
- Hypersensitivity/anaphylactoid reactions: Serious and occasionally severe or fatal hypersensitivity (anaphylactoid) reactions have been reported in patients on penicillin therapy, especially with a history of beta-lactam hypersensitivity or a history of sensitivity to multiple allergens. Serious anaphylactoid reactions require emergency treatment and airway management. Appropriate treatments must be readily available.
- Rash: Appearance of a rash should be carefully evaluated to differentiate a nonallergic ampicillin rash from a hypersensitivity reaction; rash occurs in 5% to 10% of children and is a generalized dull red, maculopapular rash, generally appearing 3 to 14 days after the start of therapy. It normally begins on the trunk and spreads over most of the body. It may be most intense at pressure areas, elbows, and knees.
- Superinfection: Prolonged use may result in fungal or bacterial superinfection, including Clostridioides (formerly Clostridium) difficile-associated diarrhea (CDAD) and pseudomembranous colitis; CDAD has been observed >2 months postantibiotic treatment.
Disease-related concerns:
- Infectious mononucleosis: A high percentage of patients with infectious mononucleosis have developed rash during therapy; ampicillin-class antibiotics not recommended in these patients. Rash (generalized maculopapular and pruritic) usually appears 7 to 10 days after initiation and usually resolves within a week of discontinuation. It is not known whether these patients are truly allergic to ampicillin
- Renal impairment: Use with caution in patients with renal impairment; dosage adjustment recommended.
Monitoring Parameters
With prolonged therapy, monitor renal, hepatic, and hematologic function periodically; observe signs and symptoms of anaphylaxis during first dose
Pregnancy
Pregnancy Risk Factor
B
Pregnancy Considerations
Ampicillin crosses the placenta, providing detectable concentrations in the cord serum and amniotic fluid (Bolognese 1968; Fisher 1967; MacAulay 1966).
Maternal use of ampicillin has generally not resulted in an increased risk of birth defects (Aselton 1985; Czeizel 2001b; Heinonen 1977; Jick 1981; Puhó 2007).
Due to pregnancy-induced physiologic changes, the pharmacokinetics of ampicillin may be altered; dose adjustments may be needed. Although oral absorption is not altered during pregnancy, oral ampicillin is poorly absorbed during labor (Philipson 1977; Philipson 1978; Wasz-Höckert 1970).
Ampicillin is recommended for use in pregnant women for the management of preterm prelabor rupture of membranes (PROM) and is an option for the prevention of early-onset group B streptococcal (GBS) disease in newborns. Ampicillin may also be used in certain situations prior to vaginal delivery in women at high risk for endocarditis (ACOG 188 2018; ACOG 199 2018; ACOG 782 2019).
Patient Education
What is this drug used for?
- It is used to treat bacterial infections.
Frequently reported side effects of this drug
- Nausea
- Vomiting
- Diarrhea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Severe loss of strength and energy
- Bruising
- Bleeding
- Chills
- Sore throat
- Black, hairy tongue
- Mouth irritation
- Mouth sores
- Seizures
- Clostridium difficile (C. diff)-associated diarrhea like abdominal pain or cramps, severe diarrhea or watery stools, or bloody stools.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.