Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Packet, Oral:
Zithromax: 1 g (3 ea, 10 ea) [cherry-banana flavor]
Generic: 1 g (3 ea, 10 ea)
Solution Reconstituted, Intravenous [preservative free]:
Zithromax: 500 mg (1 ea)
Generic: 500 mg (1 ea)
Suspension Reconstituted, Oral:
Zithromax: 100 mg/5 mL (15 mL) [cherry-vanilla-banana flavor]
Zithromax: 200 mg/5 mL (15 mL, 22.5 mL, 30 mL) [cherry flavor]
Zmax: 2 g (1 ea [DSC]) [cherry-banana flavor]
Generic: 100 mg/5 mL (15 mL); 200 mg/5 mL (15 mL, 22.5 mL, 30 mL)
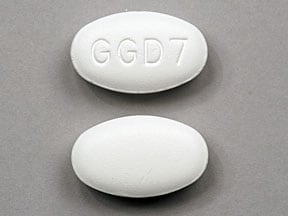
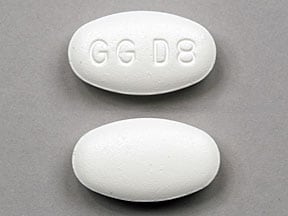
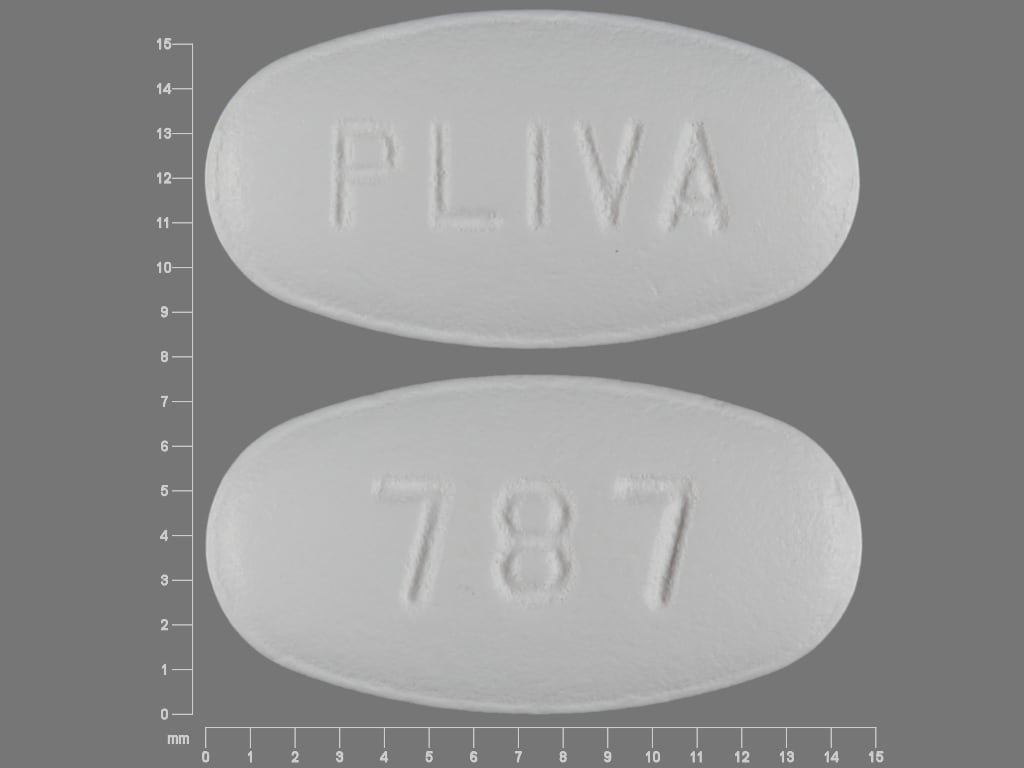
Tablet, Oral:
Zithromax: 250 mg, 500 mg, 600 mg
Zithromax Tri-Pak: 500 mg
Zithromax Z-Pak: 250 mg
Generic: 250 mg, 500 mg, 600 mg
Pharmacology
Mechanism of Action
Inhibits RNA-dependent protein synthesis at the chain elongation step; binds to the 50S ribosomal subunit resulting in blockage of transpeptidation
Pharmacokinetics/Pharmacodynamics
Absorption
Oral: Rapid from the GI tract
Distribution
Extensive tissue; distributes well into skin, lungs, sputum, tonsils, and cervix; penetration into CSF is poor; Vd: 31 to 33 L/kg
Metabolism
Hepatic to inactive metabolites
Excretion
Oral, IV: Biliary (major route 50%, unchanged); urine (6% to 14% unchanged)
Time to Peak
Oral: Serum: Immediate release: ~2 to 3 hours; Extended release: 3 to 5 hours
Half-Life Elimination
Terminal: Oral, IV: Infants and Children 4 months to 15 years: 54.5 hours; Adults: Immediate release: 68 to 72 hours; Extended release: 59 hours
Protein Binding
Concentration dependent and dependent on alpha1-acid glycoprotein concentrations: Oral, IV: 7% to 51%
Use in Specific Populations
Special Populations: Renal Function Impairment
Cmax and AUC increased 61% and 35%, respectively, in subjects with severe renal impairment.
Special Populations: Elderly
In elderly women, a higher Cmax was observed but there was no change in drug accumulation.
Use: Labeled Indications
Oral, IV:
Chancroid: Treatment of genital ulcer disease (in men) due to Haemophilus ducreyi (chancroid)
Chronic obstructive pulmonary disease, bacterial exacerbations: Treatment of acute bacterial exacerbations of chronic obstructive pulmonary disease (COPD) due to Haemophilus influenzae, Moraxella catarrhalis, or Streptococcus pneumoniae
Mycobacterium avium complex: Prevention of Mycobacterium avium complex (MAC) in patients with advanced HIV infection; treatment of disseminated MAC (in combination with ethambutol) in patients with advanced HIV infection
Otitis media, acute: Treatment of acute otitis media due to H. influenzae, M. catarrhalis, or S. pneumoniae
Pneumonia, community-acquired: Treatment of community-acquired pneumonia (CAP) due to Chlamydophila pneumoniae, H. influenzae, Legionella pneumophila, M. catarrhalis, Mycoplasma pneumoniae, or S. pneumoniae
Skin and skin structure infection, uncomplicated: Treatment of uncomplicated skin and skin structure infections due to Staphylococcus aureus, Streptococcus pyogenes, or Streptococcus agalactiae
Streptococcal pharyngitis (group A): Treatment of pharyngitis/tonsillitis due to S. pyogenes as an alternative to first-line therapy
Urethritis/cervicitis: Treatment of urethritis and cervicitis due to Chlamydia trachomatis or Neisseria gonorrhoeae
Use: Off Label
Acne vulgarisbyes
Data from controlled trials support the use of azithromycin in the treatment of acne vulgaris in adults with moderate to severe acne.
Based on the
Babesiosisbyes
Data from a prospective, nonblinded, randomized trial in patients with non-life-threatening babesiosis, support the use of azithromycin (in combination with atovaquone) for the treatment of this condition Krause 2000. Clinical experience also suggests the utility of azithromycin (in combination with atovaquone) for the treatment of immunocompetent patients with mild to moderate babesiosis Vannier 2012.
Based on the
Bronchiectasis (non-cystic fibrosis), prevention of pulmonary exacerbationsb
Data from a randomized, double-blind, placebo-controlled trial in patients with a diagnosis of bronchiectasis defined by high-resolution CT who had at least one pulmonary exacerbation requiring antibiotic treatment in the prior year support the use of azithromycin for the prevention of exacerbations in patients with non-cystic fibrosis bronchiectasis Wong 2012.
Bronchiolitis obliterans syndrome in lung transplant recipientscyes
Data from 2 retrospective observational studies, a prospective observational study, and several case series found that 30% to 83% of lung transplant patients with bronchiolitis obliterans syndrome (BOS) had improved lung function (increase in FEV1 of ≥10%) after receiving azithromycin treatment; however, in some studies, nonresponders experienced lung function decline Gottlieb 2008, Jain 2010, Meyer 2014, Vos 2010. Two of the observational studies found that lower mortality was seen in select patients (ie, early posttransplant or BOS stage 1) who received azithromycin treatment Jain 2010, Vos 2010.
The International Society for Heart and Lung Transplantation, American Thoracic Society, and European Respiratory Society (ISHLT/ATS/ERS) clinical practice guidelines for the diagnosis and management of BOS suggest a trial of azithromycin (continuous treatment for a minimum of 3 months) for lung transplant patients who experience a decline in FEV1 consistent with the onset of BOS.
Campylobacter infectioncyes
Data from a randomized, double-blind trial of patients with infectious diarrhea (64% with Campylobacter) suggest that azithromycin may be beneficial for the treatment of travelers' diarrhea caused by Campylobacter Tribble 2007.
Based on the American College of Gastroenterology (ACG) guideline for the diagnosis, treatment, and prevention of acute diarrheal infections in adults, the IDSA practice guidelines for the diagnosis and management of infectious diarrhea, and the US Department of Health and Human Services (HHS) guidelines for prevention and treatment of opportunistic infections in HIV-infected adults and adolescents, azithromycin is an effective and recommended treatment for patients with Campylobacter infection. Due to increased levels of resistance to fluoroquinolones, azithromycin may be a recommended first-line treatment, especially in regions with a high prevalence of Campylobacter (eg, Southeast Asia, India) or in geographical areas with suspected fluoroquinolone-resistant pathogens.
Cat scratch diseaseayes
Data from a prospective, randomized, double-blind, placebo-controlled trial in patients with cat scratch disease caused by Bartonella henselae support the use of azithromycin for the treatment of this condition Bass 1998.
Based on the IDSA guidelines for the diagnosis and management of skin and soft tissue infections (SSTIs), azithromycin is an effective and recommended treatment for cat scratch disease.
Cesarean delivery (intrapartum or after rupture of membranes), preoperative prophylaxisbyes
Data from a prospective, randomized, double-blind, placebo-controlled trial in patients undergoing unplanned cesarean delivery support the use of a single preoperative dose of azithromycin IV, in conjunction with standard preoperative antibiotics, to reduce the postpartum maternal infection rate Tita 2016.
Based on the American College of Obstetricians and Gynecologists guidelines for premature rupture of membranes, azithromycin may be used as an alternative or adjunctive prophylactic antibiotic in females undergoing unplanned cesarean delivery ACOG 199 2018.
Chlamydia trachomatis infection of the pharynxyes
Based on the CDC sexually transmitted diseases treatment guidelines, azithromycin is an effective and recommended agent in the treatment of Chlamydia trachomatis infection of the cervix, urethra, or pharynx.
Chlamydia trachomatis infection, expedited partner therapyyes
Based on the CDC sexually transmitted diseases treatment guidelines, azithromycin is an effective and recommended treatment of chlamydia in heterosexual partners of infected patients, unless prohibited by law.
Choleraa
Data from a prospective, double-blind, randomized trial support the use of azithromycin for the treatment of severe cholera in adults Saha 2006.
Chronic obstructive pulmonary disease, prevention of exacerbationsayes
Data from randomized, placebo-controlled trials support the use of azithromycin for prevention of chronic obstructive pulmonary disease (COPD) exacerbations Albert 2011, Uzun 2014.
Based on the European Respiratory Society/American Thoracic Society (ERS/ATS) guidelines for prevention of COPD exacerbations and the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines for the diagnosis, management, and prevention of chronic obstructive pulmonary disease, azithromycin is an effective and recommended agent to prevent COPD exacerbations.
Cystic fibrosis, anti-inflammatoryayes
Data from 3 randomized, double-blind trials support the use of azithromycin as an anti-inflammatory agent for patients with cystic fibrosis Equi 2002, Saiman 2003, Wolter 2002.
Based on the Cystic Fibrosis Foundation cystic fibrosis pulmonary guidelines on chronic medications for maintenance of lung heath, azithromycin is an effective and recommended agent to improve lung function and reduce exacerbations.
Endocarditis prophylaxis (dental or invasive respiratory tract procedure)yes
Based on the American Heart Association (AHA) guidelines for the prevention of infective endocarditis, azithromycin is an effective and recommended alternative for prophylaxis against infective endocarditis associated with dental procedures in patients with certain cardiac conditions who are allergic to penicillins or ampicillin.
Gonococcal infection, disseminated (arthritis, arthritis-dermatitis syndrome)yes
Based on the CDC sexually transmitted diseases treatment guidelines, azithromycin in combination with ceftriaxone is an effective and recommended treatment for patients with disseminated gonococcal infections including arthritis and arthritis-dermatitis syndrome.
Gonococcal infection, expedited partner therapyyes
Based on the CDC sexually transmitted diseases treatment guidelines, azithromycin in combination with cefixime is an effective and recommended treatment of gonorrhea in heterosexual partners of infected patients, unless prohibited by law.
Gonococcal infection, uncomplicated (infection of the rectum or pharynx; conjunctivitis)yes
Based on the CDC sexually transmitted diseases treatment guidelines, azithromycin in combination with ceftriaxone is an effective and recommended treatment for patients with uncomplicated gonococcal infections of the rectum or pharynx, or conjunctivitis.
Granuloma inguinale (donovanosis)yes
Based on the CDC sexually transmitted diseases treatment guidelines, azithromycin is an effective and recommended agent in the treatment of granuloma inguinale.
Lyme diseaseyes
Based on the IDSA guidelines for the clinical assessment, treatment and prevention of Lyme disease, human granulocytic anaplasmosis, and babesiosis, azithromycin is an effective and recommended alternative agent for the treatment of early localized or disseminated Lyme disease (erythema migrans or borrelial lymphocytoma) in patients who are unable to take or who are intolerant of tetracyclines, penicillins, or cephalosporins.
Mycobacterium abscessus infectionyes
Based on the ATS/IDSA guideline on the diagnosis, treatment, and prevention of nontuberculosis mycobacterial disease, the British Thoracic Society (BTS) guidelines for the management of nontuberculous mycobacterial pulmonary disease, and the US Cystic Fibrosis Foundation and European Cystic Fibrosis Society consensus recommendations for the management of nontuberculous mycobacteria in individuals with cystic fibrosis, azithromycin (in combination with other antimicrobials) is effective and recommended for the treatment of Mycobacterium abscessus pulmonary, skin, soft tissue, and bone infections.
Mycoplasma genitaliumcyes
A meta-analysis of controlled trials and observational studies supports the use of azithromycin in the management of Mycoplasma genitalium but notes that overall susceptibility to the drug appears to be decreasing, with cure rates of less than 70% reported since 2009 Lau 2015.
Pertussisyes
Based on the CDC guidelines on recommended antimicrobial agents for the treatment and postexposure prophylaxis of pertussis, azithromycin is effective and recommended for the treatment of pertussis.
Sexually transmitted infections, empiric treatment following sexual assaultyes
Based on the CDC sexually transmitted diseases treatment guidelines, azithromycin in combination with ceftriaxone (plus metronidazole or tinidazole) is a recommended regimen for empiric treatment of sexually transmitted infections following sexual assault.
Shigella infectionyes
Based on the World Health Organization (WHO) guidelines for the control of shigellosis and the IDSA practice guidelines for the diagnosis and management of infectious diarrhea, azithromycin, as an alternative to ciprofloxacin, may be used to treat this condition although there are limited data on efficacy.
Surgical prophylaxis, uterine evacuation (induced abortion or pregnancy loss)c
Clinical experience suggests the utility of azithromycin as an alternative agent as surgical prophylaxis for uterine evacuation Shih 2019.
Syphilis, primary and secondaryyes
Based on the CDC sexually transmitted diseases treatment guidelines, azithromycin is a recommended alternative treatment for primary and secondary syphilis in patients who are unable to receive penicillin or doxycycline. Note: Azithromycin should be used with caution, and should not be used to treat syphilis in patients with HIV, pregnant women, or in the men who have sex with men (MSM) population.
Travelers' diarrhea, empiric treatmentcyes
Data from a randomized, double-blind trial of patients with infectious diarrhea suggest that azithromycin may be beneficial for the treatment of travelers' diarrhea caused by Campylobacter Tribble 2007.
Based on the CDC Yellow Book, the ACG guideline for the diagnosis, treatment, and prevention of acute diarrheal infections in adults, and the IDSA practice guidelines for the diagnosis and management of infectious diarrhea, azithromycin is effective and recommended treatment for patients with travelers' diarrhea. Due to increased levels of resistance to fluoroquinolones, azithromycin may be a recommended first-line treatment, especially in regions with a high prevalence of Campylobacter (eg, Southeast Asia, India) or in geographical areas with suspected fluoroquinolone-resistant pathogens or enterotoxigenic Escherichia coli.
Contraindications
Hypersensitivity to azithromycin, erythromycin, other macrolide (eg, azalide or ketolide) antibiotics, or any component of the formulation; history of cholestatic jaundice/hepatic dysfunction associated with prior azithromycin use
Note: The manufacturer does not list concurrent use of pimozide as a contraindication; however, azithromycin is listed as a contraindication in the manufacturer's labeling for pimozide.
Dosage and Administration
Dosing: Adult
Note: Zmax suspension has been discontinued in the US for more than 1 year.
Note: Extended-release suspension (Zmax) is not interchangeable with immediate-release formulations. Use should be limited to approved indications. All doses are expressed as immediate-release azithromycin unless otherwise specified.
Acne vulgaris, inflammatory (moderate to severe) (off-label use):
Note: Use as an adjunct to topical acne therapy (AAD [Zaenglein 2016]).
Oral: Dosing regimens used in clinical trials have varied greatly. All trials used pulse-dosing regimens; regimens included: 500 mg once daily for 4 consecutive days per month for 3 consecutive months (Babaeinejad 2011; Parsad 2001) or 500 mg once daily for 3 days in the first week, followed by 500 mg once weekly until week 10 (Maleszka 2011) or 500 mg once daily for 3 consecutive days each week in month 1, followed by 500 mg once daily for 2 consecutive days each week in month 2, then 500 mg once daily for 1 day each week in month 3 (Kus 2005). The shortest possible duration should be used to minimize development of bacterial resistance; reevaluate at 3 to 4 months (AAD [Zaenglein 2016]).
Babesiosis (off-label use):
Mild to moderate disease: Oral: 500 mg on day 1, followed by 250 mg once daily in combination with atovaquone for 7 to 10 days in immunocompetent patients (IDSA [Wormser 2006]; Krause 2000; Vannier 2012); higher doses of azithromycin may be used in immunocompromised patients (600 to 1,000 mg daily) (IDSA [Wormser 2006]; Weiss 2001; Wormser 2010).
Severe disease: IV: 500 mg daily in combination with atovaquone for 7 to 10 days (Kletsova 2017; Sanchez 2016); a longer duration is needed for those at high risk for relapse (Krause 2008; Sanchez 2016; Vannier 2012). Note: May switch to oral azithromycin (at the same dose) following improvement on IV therapy (Sanchez 2016); when switching to oral treatment in immunocompromised patients, a higher dose (600 to 1,000 mg daily) has been used (IDSA [Wormser 2006]; Sanchez 2016; Weiss 2001).
Bronchiectasis (non-cystic fibrosis), prevention of pulmonary exacerbations (off-label use): Oral: 500 mg 3 times weekly (Wong 2012) or 250 mg once daily (Altenburg 2013). Note: Recommended for patients with ≥2 (Barker 2018) or ≥3 (ERS [Polverino 2017]) exacerbations per year; for those who do not have Pseudomonas aeruginosa infection, have P. aeruginosa but cannot take an inhaled antibiotic, or continue to have exacerbations despite an inhaled antibiotic. Patients should be screened for nontuberculous mycobacterial infection prior to treatment and azithromycin should not be given if present (ERS [Polverino 2017]).
Bronchiolitis obliterans syndrome in lung transplant recipients, treatment (off-label use): Oral: 250 mg daily for 5 days, followed by 250 mg 3 times weekly for at least a 3-month trial (ISHLT/ATS/ERS [Meyer 2014]); some experts continue indefinitely, regardless of response to therapy (Pilewski 2018). Note: When studied to prevent bronchiolitis obliterans syndrome in patients with hematologic malignancy who underwent allogeneic hematopoietic cell transplantation, rates of cancer relapse and mortality were increased among patients receiving long-term azithromycin, leading to early trial termination (Bergeron 2017; FDA Drug Safety Communication 2018).
Cat scratch disease (lymphadenitis) (off-label use): Oral: 500 mg as a single dose, then 250 mg once daily for 4 additional days (Bass 1998; IDSA [Stevens 2014]; Psarros 2012)
Cesarean delivery (intrapartum or after rupture of membranes), preoperative prophylaxis (off-label use): IV: 500 mg as a single dose 1 hour prior to surgical incision; use in combination with standard preoperative antibiotics (ACOG 199 2018; Tita 2016)
Chronic obstructive pulmonary disease (COPD):
Bacterial exacerbation, treatment: Oral: 500 mg in a single loading dose on day 1, followed by 250 mg once daily on days 2 to 5 (Castaldo 2003) or 500 mg once daily for 3 days (Swanson 2005). Note: Some experts reserve for use in patients with uncomplicated COPD (eg, age <65 years without major comorbidities, FEV1 >50% predicted, infrequent exacerbations) (Anzueto 2007; Sethi 2008).
Prevention of exacerbations (off-label use): Oral: 250 to 500 mg 3 times weekly (Berkhof 2013; Uzun 2014) or 250 mg once daily (Albert 2011)
Cystic fibrosis, anti-inflammatory (off-label use): Oral: 250 mg (<40 kg) or 500 mg (≥40 kg) 3 times weekly (Saiman 2003) or 250 mg once daily (Wolter 2002). Note: Patients should be screened for nontuberculous mycobacterial infection prior to treatment and azithromycin should not be given if present (Mogayzel 2013; Saiman 2003).
Diarrhea, infectious (off-label use):
Campylobacter infection: Oral: 1 g as a single dose or 500 mg once daily for 3 days (ACG [Riddle 2016]; Tribble 2007). If symptoms have not resolved after 24 hours following single-dose therapy, continue with 500 mg once daily for 2 more days (ACG [Riddle 2016]). For HIV-infected patients, 500 mg once daily for 5 days is recommended (HHS [OI adult] 2019). Note: Increased nausea may occur with the 1 g single-dose regimen (Tribble 2007), which may be reduced by administering azithromycin as 2 divided doses on the same day (CDC 2018; Riddle 2017).
Cholera (alternative agent): Oral: 1 g as a single dose (Saha 2006)
Shigella infection: Note: Confirm susceptibility if possible (Agha 2018; HHS [OI adult] 2019; WHO 2005). Oral: 500 mg once daily for 3 days (ACG [Riddle 2016]); 5 days of therapy should be given for Shigella dysenteriae type 1 infection or for patients with HIV coinfection (Agha 2018; HHS [OI adult] 2019).
Travelers' diarrhea, empiric treatment: Oral: 1 g as a single dose or 500 mg once daily for 3 days (ACG [Riddle 2016]; CDC 2018; Riddle 2017; Tribble 2007). If symptoms have not resolved after 24 hours following single-dose therapy, continue with 500 mg once daily for 2 more days. A 3-day course of 500 mg once daily is the preferred regimen for dysentery or febrile diarrhea (ACG [Riddle 2016]). Note: Most cases are self-limited and may not warrant antimicrobial therapy. Increased nausea may occur with the 1 g single-dose regimen (Tribble 2007), which may be reduced by administering azithromycin as 2 divided doses on the same day (CDC 2018; Riddle 2017).
Endocarditis prophylaxis, dental or invasive respiratory tract procedure (alternative agent for penicillin-allergic patients) (off-label use): Oral: 500 mg 30 to 60 minutes prior to procedure. Note: Only recommended for patients with cardiac conditions associated with the highest risk of an adverse outcome from endocarditis and who are undergoing a procedure likely to result in bacteremia with an organism that has the potential to cause endocarditis. (AHA [Wilson 2007]).
Lyme disease (erythema migrans or borrelial lymphocytoma) (alternative agent) (off-label use): Oral: 500 mg once daily for 7 to 10 days. Note: Use with caution and only when recommended agents cannot be used (due to decreased efficacy compared to other agents) (IDSA [Wormser 2006]).
Mycobacterial (nontuberculous) infection:
Mycobacterium avium complex (MAC) infection:
Disseminated disease in HIV-infected patients:
Treatment: Oral: 500 to 600 mg daily as part of a combination therapy regimen (HHS [OI adult] 2019).
Primary prophylaxis (patients with CD4 count <50 cells/mm3 who are not initiated on fully suppressive antiretroviral therapy [ART]): Oral: 1,200 mg once weekly (preferred) or 600 mg twice weekly; may discontinue prophylaxis when patient is initiated on effective ART (HHS [OI adult] 2019; IAS-USA [Saag 2018]).
Secondary prophylaxis: Oral: 500 to 600 mg daily as part of an appropriate combination regimen; may discontinue when patient has completed ≥12 months of therapy, has no signs/symptoms of MAC disease, and has sustained (>6 months) CD4 count >100 cells/mm3 in response to ART (HHS [OI adult] 2019).
Pulmonary disease (nodular/bronchiectatic disease) (off-label use): Oral: 500 to 600 mg 3 times weekly as part of an appropriate combination regimen; continue treatment until patient is culture negative on therapy for ≥1 year (ATS/IDSA [Griffith 2007]); some experts prefer 500 mg 3 times weekly due to improved tolerability (BTS [Haworth 2017]).
Pulmonary disease (severe nodular/bronchiectatic or cavitary disease) (off-label use): Oral: 250 to 500 mg once daily as part of an appropriate combination regimen (ATS/IDSA [Griffith 2007]; BTS [Haworth 2017]; Deshpande 2016; van Ingen 2012); continue treatment until patient is culture negative on therapy for ≥1 year (ATS/IDSA [Griffith 2007]; BTS [Haworth 2017]). Preliminary data suggest a relationship between peak concentration and clinical outcome among patients receiving daily therapy for pulmonary MAC (Jeong 2016); as such, some experts recommend checking levels and/or using higher doses of azithromycin (Kasperbauer 2018).
Pulmonary disease in patients with cystic fibrosis (off-label use): Oral: 250 to 500 mg once daily as part of an appropriate combination regimen; continue treatment until patient is culture negative on therapy for ≥1 year. Note: Intermittent dosing (3 times weekly) is not recommended for patients with cystic fibrosis (CFF/ECFS [Floto 2016]).
Mycobacterium abscessus infection (off-label use):
Note: Presence of inducible erm gene can result in decreased susceptibility even with a “susceptible” MIC result; perform susceptibility testing before and after ≥14 days of clarithromycin incubation to evaluate for the presence of an active erm gene, which may preclude use of azithromycin (CFF/ECFS [Floto 2016]; Griffith 2018).
Pulmonary, skin, soft tissue, or bone infection: Oral: 250 to 500 mg once daily as part of an appropriate combination regimen and continued for ≥6 to 12 months for pulmonary and bone infections, and ≥4 months for skin/soft tissue infections (ATS/IDSA [Griffith 2007]; CFF/ECFS [Floto 2016]; Griffith 2018). Note: Patients should be under the care of a clinician with expertise in managing mycobacterial infection.
Pertussis (off-label use): Oral: 500 mg on day 1, followed by 250 mg once daily on days 2 to 5 (CDC [Tiwari 2005]).
Pneumonia, community-acquired:
Note: For empiric therapy, may need to use in combination with other appropriate agents (depending on disease severity and/or risk factors for drug-resistant pathogens, particularly Streptococcus pneumoniae). Duration of therapy may vary based on disease severity and response to therapy. Patients should be afebrile for ≥48 hours and clinically stable prior to discontinuation (IDSA/ATS [Mandell 2007]).
Outpatient: Oral: 500 mg on day 1, followed by 250 mg once daily for 4 days or 500 mg once daily for 3 days (Amsden 1999; IDSA/ATS [Mandell 2007]; Schönwald 1991).
ER suspension (Zmax): 2 g as a single dose.
Inpatient: Oral, IV: 500 mg once daily for a minimum of 3 days (File 2019; IDSA/ATS [Mandell 2007]).
Sexually transmitted infections:
Cervicitis, empiric therapy: Oral: 1 g as a single dose, preferably under direct observation; give in combination with ceftriaxone if the patient is at high risk for gonorrhea, if follow-up is a concern, or if the local prevalence of gonorrhea is high (eg, >5%) (CDC [Workowski 2015]; Marrazzo 2018).
Chancroid (due to Haemophilus ducreyi): Oral: 1 g as a single dose. Note: Data are limited concerning efficacy in HIV infected patients (CDC [Workowski 2015]).
Chlamydia trachomatis infection of the cervix, urethra, or pharynx (off-label use [pharynx]): Oral: 1 g as a single dose, preferably under direct observation (CDC [Workowski 2015]).
Chlamydia trachomatis infection, expedited partner therapy (off-label use): Oral: 1 g as a single dose, preferably under direct observation. Note: Clinical evaluation and presumptive treatment is preferred for sexual partners of patients with chlamydia. Alternatively, expedited partner therapy for chlamydia can be used for heterosexual partners if the provider is concerned that the partner will otherwise not be promptly evaluated and treated; state laws regarding expedited partner therapy vary (CDC [Workowski 2015]).
Empiric treatment following sexual assault (off-label use): Oral: 1 g as a single dose in combination with ceftriaxone (plus metronidazole or tinidazole) (CDC [Workowski 2015]).
Gonococcal infection, disseminated (arthritis, arthritis-dermatitis) (off-label use): Oral: 1 g as a single dose in combination with ceftriaxone, preferably under direct observation (CDC [Workowski 2015]).
Gonococcal infection, expedited partner therapy (off-label use): Oral: 1 g as a single dose in combination with cefixime. Note: Clinical evaluation and presumptive treatment is preferred for sexual partners of patients with gonorrhea. Alternatively, expedited partner therapy for gonorrhea can be used for heterosexual partners if the provider is concerned that the partner will otherwise not be promptly evaluated and treated; state laws regarding expedited partner therapy vary (CDC [Workowski 2015]).
Gonococcal infection, uncomplicated (infection of the cervix, urethra, rectum, or pharynx; conjunctivitis): Oral:
Dual-therapy regimen (off-label): 1 g as a single dose in combination with ceftriaxone (CDC [Workowski 2015]).
Patients with severe cephalosporin allergy (off-label): 2 g as a single dose in combination with gemifloxacin (not available in the US) or gentamicin IM (CDC [Workowski 2015]). Note: Patients with pharyngeal infection treated with an alternative regimen should have a test-of-cure performed. Consult an infectious diseases specialist when treatment failure is suspected and report failures to the CDC through state and local health departments within 24 hours of diagnosis (CDC [Workowski 2015]).
Granuloma inguinale (donovanosis) (off-label use): Oral: 1 g once weekly or 500 mg once daily for ≥3 weeks and until lesions have healed. Note: If symptoms do not improve within the first few days of therapy, the addition of gentamicin may be considered (CDC [Workowski 2015]).
Mycoplasma genitalium (off-label use) (CDC [Workowski 2015]; Falk 2015): Oral:
Note: Azithromycin resistance is rapidly emerging; consider alternative therapy.
Single-dose regimen: 1 g as a single dose.
Extended-dose regimen: 500 mg on day 1, followed by 250 mg once daily on days 2 through 5.
Syphilis, primary and secondary (alternative agent for penicillin-allergic patients) (off-label use): Oral: 2 g as a single dose. Note: Limited data support the use of alternatives to penicillin; close serologic and clinical follow-up is warranted. Use only if no other options are available due to the potential for rapid emergence of macrolide resistance in Treponema pallidum and treatment failure; do not use to treat syphilis in patients with HIV, pregnant women, or the men who have sex with men (MSM) population (CDC [Workowski 2015]).
Urethritis, empiric therapy: Oral: 1 g as a single dose, preferably under direct observation; give in combination with ceftriaxone if there is microscopic evidence of gonococcal urethritis or if there is high clinical suspicion for gonococcal infection (Bachmann 2018; CDC [Workowski 2015]).
Streptococcal pharyngitis (group A) (alternative agent for severely penicillin-allergic patients): Oral: 500 mg on day 1, followed by 250 mg once daily on days 2 through 5 (IDSA [Shulman 2012]) or 500 mg once daily for 3 days (Casey 2005).
Surgical prophylaxis, uterine evacuation (induced abortion or pregnancy loss) (alternative agent) (off-label use): Oral: 500 mg as a single dose 1 hour before the procedure (may be administered up to 12 hours before the procedure) (Shih 2019).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Zmax 2 g extended-release oral suspension has been discontinued in the US for more than 1 year.
Note: Extended-release suspension (Zmax) is not interchangeable with immediate-release formulations. All doses are expressed as immediate-release azithromycin unless otherwise specified.
General dosing, susceptible infection (Red Book [AAP] 2012): Infants, Children, and Adolescents:
Mild to moderate infection: Oral: 5 to 12 mg/kg/dose; typically administered as 10 to 12 mg/kg/dose on day 1 followed by 5 to 6 mg/kg once daily for remainder of treatment duration; usual maximum dose for the total course: 1,500 to 2,000 mg
Serious infection: IV: 10 mg/kg once daily; maximum dose: 500 mg/dose
Babesiosis: Infants, Children, and Adolescents: Oral: 10 mg/kg once on day 1 (maximum dose: 500 mg/dose), then 5 mg/kg once daily on days 2 to 10 (maximum dose: 250 mg/dose) in combination with atovaquone; longer duration of therapy may be necessary in some cases; in immunocompromised patients, higher doses (eg, adults: 600 to 1,000 mg daily) may be required (Red Book [AAP] 2012; IDSA [Wormser 2006])
Bartonellosis: Oral:
Cat scratch disease (B. henselae) with extensive lymphadenopathy (IDSA [Stevens] 2014): Non-HIV-exposed/-positive:
Infants, Children, and Adolescents ≤45 kg: 10 mg/kg once on day 1 (maximum dose: 500 mg/dose), followed by 5 mg/kg once daily on days 2 to 5 (maximum dose: 250 mg/dose)
Children and Adolescents >45 kg: 500 mg as a single dose on day 1, then 250 mg once daily for 4 additional days
Cutaneous bacillary angiomatosis (B. henselae or B. quintana): HIV- exposed/-positive: Infants, Children, and Adolescents: 5 to 12 mg/kg once daily; maximum dose: 600 mg/dose; usual treatment duration: 3 months (CDC 2009)
Chancroid (CDC 2010; Red Book [AAP] 2012): Oral:
<45 kg: 20 mg/kg as a single dose; maximum dose: 1,000 mg/dose
≥45 kg: 1,000 mg as a single dose
Chlamydial infections:
Cervicitis, urethritis (C. trachomatis): Children and Adolescents ≥45 kg: Oral: 1,000 mg as a single dose (CDC 2010; Red Book [AAP] 2012)
Conjunctivitis: Infants: Oral, IV: 20 mg/kg once daily for 3 days (Red Book [AAP] 2012)
Pneumonia, community-acquired (Bradley 2011): Infants >3 months, Children, and Adolescents:
Mild infection or step-down therapy: Oral: 10 mg/kg once on day 1 (maximum dose: 500 mg/dose) followed by 5 mg/kg once daily on days 2 to 5 (maximum dose: 250 mg/dose)
Severe infection: IV: 10 mg/ kg once daily for at least 2 days, then transition to oral route with a single daily dose of 5 mg/kg to complete course of therapy; maximum dose: 500 mg/dose
Cystic fibrosis; improve lung function, reduce exacerbation frequency: Limited data available; dosing regimen variable (Mogayzel 2013; Saiman 2003; Saiman 2010): Children ≥6 years and Adolescents: Oral:
18 to 35.9 kg: 250 mg three times weekly (Monday, Wednesday, Friday)
≥36 kg: 500 mg three times weekly (Monday, Wednesday, Friday)
Diarrhea, infectious:
Campylobacter: Infants, Children, and Adolescents: Oral: 10 mg/kg once daily for 3 days; maximum dose: 500 mg/dose (Red Book [AAP] 2012)
Shigellosis: Infants, Children, and Adolescents: Oral:
AAP Recommendation: 12 mg/kg once on day 1 (maximum dose: 500 mg/dose), followed by 6 mg/kg once daily on days 2 to 5 (maximum dose: 250 mg/dose) (Red Book [AAP] 2012)
Alternate dosing: 10 mg/kg once daily for 3 days (Dupont 2009; Mackell 2005); WHO Guidelines recommend up to 20 mg/kg/dose and in some cases, a wider range of duration of therapy (eg, 1 to 5 days) (WHO 2005)
Endocarditis; prophylaxis: Infants, Children, and Adolescents: Oral: 15 mg/kg/dose 30 to 60 minutes before procedure; maximum dose: 500 mg/dose (Wilson 2007)
Gonococcal infection; uncomplicated (cervicitis, urethritis, anorectal): Oral:
Children <45 kg: 20 mg/kg as a single dose; maximum dose: 1,000 mg/dose (Red Book [AAP] 2012)
Children > 8 years and ≥45 kg and Adolescents: 1,000 mg as a single dose (CDC 2012; Red Book [AAP] 2012)
Group A streptococcal infection; treatment of streptococcal tonsillopharyngitis:
Manufacturer's labeling and AHA recommendations: Infants, Children, and Adolescents: Oral: 12 mg/kg/dose once daily for 5 days; maximum dose: 500 mg/dose (AHA [Gerber 2009])
Alternate dosing:
IDSA recommendations: Note: Recommended as an alternative agent for group A streptococcal pharyngitis in penicillin-allergic patients. Infants, Children, and Adolescents: Oral: 12 mg/kg (maximum: 500 mg/dose) on day 1 followed by 6 mg/kg/dose (maximum: 250 mg/dose) once daily on days 2 through 5 (IDSA [Shulman 2012]).
Three-day regimen: Limited data available: Children and Adolescents: Oral: 20 mg/kg/dose once daily for 3 days; maximum dose: 1,000 mg/dose (Cohen 2004; O'Doherty 1996)
Meningococcal disease, chemoprophylaxis of high-risk contacts: Infants, Children, and Adolescents: Oral: 10 mg/kg as a single dose; maximum dose: 500 mg/dose; Note: Not routinely recommended; may consider if fluoroquinolone resistance detected (Red Book [AAP] 2012)
Mycobacterium avium complex (MAC) infection (HIV-exposed/-positive):
Infants and Children (DHHS [pediatric] 2013): Oral:
Treatment: 10 to 12 mg/kg once daily in combination with ethambutol, with or without rifabutin; maximum dose: 500 mg/dose; treatment duration at least 12 months; dependent upon clinical response
Primary prevention of first episode: Preferred: 20 mg/kg once weekly (maximum dose: 1,200 mg/dose) or alternatively, 5 mg/kg once daily (maximum dose: 250 mg/dose)
Secondary prevention of recurring episodes: 5 mg/kg once daily in combination with ethambutol, with or without rifabutin; maximum dose: 250 mg/dose
Adolescents (DHHS [adult] 2013): Oral:
Treatment: 500 to 600 mg daily in combination with ethambutol
Primary prophylaxis: 1,200 mg once weekly or alternatively, 600 mg twice weekly
Secondary prophylaxis: 500 to 600 mg daily in combination with ethambutol
Otitis media, acute (AOM): Infants ≥6 months, Children, and Adolescents: Oral: Note: Due to increased S pneumonia and H. influenzae resistance, azithromycin is not routinely recommended as a treatment option (AAP [Lieberthal 2013])
Single-dose regimen: 30 mg/kg as a single dose; maximum dose: 1,500 mg/dose; if patient vomits within 30 minutes of dose, repeat dosing has been administered although limited data available on safety
Three-day regimen: 10 mg/kg once daily for 3 days; maximum dose: 500 mg/dose
Five-day regimen: 10 mg/kg once on day 1 (maximum dose: 500 mg/dose), followed by 5 mg/kg (maximum dose: 250 mg/dose) once daily on days 2 to 5
Peritonitis (peritoneal dialysis), prophylaxis for patients receiving peritoneal dialysis who require dental procedures: Infants, Children, and Adolescents: Oral: 15 mg/kg administered 30 to 60 minutes before dental procedure; maximum dose: 500 mg/dose (Warady [ISPD 2012])
Pertussis (CDC 2005; Red Book [AAP] 2012): Oral, IV:
Infants 1 to 5 months: 10 mg/kg/dose once daily for 5 days
Infants ≥6 months, Children, and Adolescents: 10 mg/kg once on day 1 (maximum dose: 500 mg/dose), followed by 5 mg/kg once daily on days 2 to 5 (maximum dose: 250 mg/dose)
Pneumonia, community-acquired (excluding mycobacterial [mycoplasma pneumoniae] and chlamydial infections):
Oral:
Immediate release: Infants >3 months, Children, and Adolescents: 10 mg/kg once on day 1 (maximum dose: 500 mg/dose), followed by 5 mg/kg (maximum dose: 250 mg/dose) once daily on days 2 to 5 (Bradley 2011)
Extended-release oral suspension (Zmax): Infants ≥6 months, Children, and Adolescents: 60 mg/kg as a single dose; maximum dose: 2,000 mg/dose
IV: Infants >3 months, Children, and Adolescents: 10 mg/kg once daily for at least 2 days, follow IV therapy by the oral route with a single daily dose of 5 mg/kg to complete a 5-day course of therapy; maximum dose: 500 mg/dose (Bradley 2011)
Pneumonia, community acquired; mycoplasma pneumoniae, or chlamydial infection (Bradley 2011): Infants >3 months, Children, and Adolescents:
Mild infection or step-down therapy: Oral: 10 mg/kg once on day 1 (maximum dose: 500 mg/dose) followed by 5 mg/kg once daily on days 2 to 5 (maximum dose: 250 mg/dose)
Severe infection: IV: 10 mg/kg once daily for at least 2 days (maximum dose: 500 mg/dose), then transition to oral route with a single daily dose of 5 mg/kg to complete course of therapy (maximum dose: 250 mg/dose)
Rhinosinusitis, bacterial: Oral: Infants ≥6 months, Children, and Adolescents: 10 mg/kg once daily for 3 days; maximum dose: 500 mg/dose; Note: Although FDA approved, macrolides are not recommended for empiric therapy due to high rates of resistance (Chow 2012).
Sexual victimization, prophylaxis: Oral: Note: Use in combination with cefixime or ceftriaxone and completion of hepatitis B virus immunization; also consider prophylaxis for trichomoniasis and bacterial vaginosis (CDC 2010; Red Book [AAP] 2012).
Children <45 kg: 20 mg/kg as a single dose
Children ≥45 kg and Adolescents: 1,000 mg as a single dose
Toxoplasma gondii, encephalitis (HIV-exposed/-positive); treatment and prevention: Oral: Adolescents: 900 to 1,200 mg once daily in combination with pyrimethamine/leucovorin; treatment duration: 6 weeks or longer if extensive disease or incomplete response at 6 weeks (DHHS [adult] 2013)
Reconstitution
Injection (Zithromax): Prepare initial solution by adding 4.8 mL of sterile water for injection to the 500 mg vial (resulting concentration: 100 mg/mL). Use of a standard syringe is recommended due to the vacuum in the vial (which may draw additional solution through an automated syringe).
The initial solution should be further diluted to a concentration of 1 mg/mL (500 mL) to 2 mg/mL (250 mL) in NS, D5W, or LR.
Administration
IV: Infuse over 1 hour (2 mg/ml infusion) or over 3 hours (1 mg/ml infusion). Not for IM or IV bolus administration.
Oral: Immediate release suspension and tablet may be taken without regard to food; extended release suspension should be taken on an empty stomach (at least 1 hour before or 2 hours following a meal), within 12 hours of reconstitution.
Dietary Considerations
Some products may contain sodium and/or sucrose.
Oral suspension, immediate release, may be administered with or without food.
Oral suspension, extended release, should be taken on an empty stomach (at least 1 hour before or 2 hours following a meal).
Tablet may be administered with food to decrease GI effects.
Storage
Injection (Zithromax): Store intact vials of injection at room temperature. Reconstituted solution is stable for 24 hours when stored below 30°C (86°F). The diluted solution D5W, D5LR, D51/4NS, D51/3NS, D51/2NS (with or without 20 mEq/L KCl), Normosol-M in D5, Normosol-R in D5, LR, NS, or 1/2NS is stable for 24 hours at or below room temperature (30°C [86°F]) and for 7 days if stored under refrigeration (5°C [41°F]).
Suspension, immediate release (Zithromax): Store dry powder below 30°C (86°F). Store reconstituted suspension at 5°C to 30°C (41°F to 86°F) and use within 10 days.
Suspension, extended release (Zmax): Store dry powder ≤30°C (86°F). Following reconstitution, store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F); do not refrigerate or freeze. Should be consumed within 12 hours following reconstitution.
Tablet (Zithromax): Store between 15°C to 30°C (59°F to 86°F).
Azithromycin (Systemic) Images
Drug Interactions
Afatinib: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Afatinib. Management: Reduce afatinib by 10 mg if not tolerated. Some non-US labeling recommends avoiding combination if possible. If used, administer the P-gp inhibitor simultaneously with or after the dose of afatinib. Consider therapy modification
AtorvaSTATin: Azithromycin (Systemic) may enhance the myopathic (rhabdomyolysis) effect of AtorvaSTATin. Monitor therapy
BCG (Intravesical): Antibiotics may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCG Vaccine (Immunization): Antibiotics may diminish the therapeutic effect of BCG Vaccine (Immunization). Monitor therapy
Betrixaban: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Betrixaban. Management: Decrease the adult betrixaban dose to an initial single dose of 80 mg followed by 40 mg once daily if combined with a P-glycoprotein inhibitor. Consider therapy modification
Bilastine: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Bilastine. Management: Consider alternatives when possible; bilastine should be avoided in patients with moderate to severe renal insufficiency who are receiving p-glycoprotein inhibitors. Consider therapy modification
Brentuximab Vedotin: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Brentuximab Vedotin. Specifically, concentrations of the active monomethyl auristatin E (MMAE) component may be increased. Monitor therapy
Cardiac Glycosides: Macrolide Antibiotics may increase the serum concentration of Cardiac Glycosides. Monitor therapy
Celiprolol: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Celiprolol. Monitor therapy
Chloroquine: QT-prolonging Miscellaneous Agents (Moderate Risk) may enhance the QTc-prolonging effect of Chloroquine. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Cholera Vaccine: Antibiotics may diminish the therapeutic effect of Cholera Vaccine. Management: Avoid cholera vaccine in patients receiving systemic antibiotics, and within 14 days following the use of oral or parenteral antibiotics. Avoid combination
Clofazimine: QT-prolonging Miscellaneous Agents (Moderate Risk) may enhance the QTc-prolonging effect of Clofazimine. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Colchicine: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Colchicine. Colchicine distribution into certain tissues (e.g., brain) may also be increased. Management: Colchicine is contraindicated in patients with impaired renal or hepatic function who are also receiving a p-glycoprotein inhibitor. In those with normal renal and hepatic function, reduce colchicine dose as directed. See full monograph for details. Consider therapy modification
CycloSPORINE (Systemic): Azithromycin (Systemic) may increase the serum concentration of CycloSPORINE (Systemic). Monitor therapy
Dabigatran Etexilate: P-glycoprotein/ABCB1 Inhibitors may increase serum concentrations of the active metabolite(s) of Dabigatran Etexilate. Monitor therapy
Domperidone: QT-prolonging Agents (Moderate Risk) may enhance the QTc-prolonging effect of Domperidone. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
DOXOrubicin (Conventional): P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of DOXOrubicin (Conventional). Management: Seek alternatives to P-glycoprotein inhibitors in patients treated with doxorubicin whenever possible. One U.S. manufacturer (Pfizer Inc.) recommends that these combinations be avoided. Consider therapy modification
Edoxaban: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Edoxaban. Management: See full monograph for details. Reduced doses are recommended for patients receiving edoxaban for venous thromboembolism in combination with certain P-gp inhibitors. Similar dose adjustment is not recommended for edoxaban use in atrial fibrillation. Consider therapy modification
Everolimus: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Everolimus. Monitor therapy
Fexinidazole [INT]: May enhance the QTc-prolonging effect of QT-prolonging Agents (Moderate Risk). Avoid combination
Gadobenate Dimeglumine: QT-prolonging Miscellaneous Agents (Moderate Risk) may enhance the QTc-prolonging effect of Gadobenate Dimeglumine. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Halofantrine: QT-prolonging Miscellaneous Agents (Moderate Risk) may enhance the QTc-prolonging effect of Halofantrine. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Haloperidol: QT-prolonging Miscellaneous Agents (Moderate Risk) may enhance the QTc-prolonging effect of Haloperidol. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Inotuzumab Ozogamicin: QT-prolonging Miscellaneous Agents (Moderate Risk) may enhance the QTc-prolonging effect of Inotuzumab Ozogamicin. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Ivermectin (Systemic): Azithromycin (Systemic) may increase the serum concentration of Ivermectin (Systemic). Monitor therapy
Lactobacillus and Estriol: Antibiotics may diminish the therapeutic effect of Lactobacillus and Estriol. Monitor therapy
Larotrectinib: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Larotrectinib. Monitor therapy
Lefamulin: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Lefamulin. Management: Avoid concomitant use of lefamulin tablets with P-glycoprotein/ABCB1 inhibitors. If concomitant use is required, monitor for lefamulin adverse effects. Consider therapy modification
Lofexidine: QT-prolonging Miscellaneous Agents (Moderate Risk) may enhance the QTc-prolonging effect of Lofexidine. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Lovastatin: Azithromycin (Systemic) may enhance the myopathic (rhabdomyolysis) effect of Lovastatin. Monitor therapy
Midostaurin: QT-prolonging Miscellaneous Agents (Moderate Risk) may enhance the QTc-prolonging effect of Midostaurin. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Mizolastine: Macrolide Antibiotics may increase the serum concentration of Mizolastine. Avoid combination
Naldemedine: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Naldemedine. Monitor therapy
Naloxegol: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Naloxegol. Monitor therapy
Nelfinavir: May increase the serum concentration of Azithromycin (Systemic). Monitor therapy
Ondansetron: QT-prolonging Miscellaneous Agents (Moderate Risk) may enhance the QTc-prolonging effect of Ondansetron. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
PAZOPanib: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of PAZOPanib. Avoid combination
Pentamidine (Systemic): QT-prolonging Miscellaneous Agents (Moderate Risk) may enhance the QTc-prolonging effect of Pentamidine (Systemic). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
P-glycoprotein/ABCB1 Substrates: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inhibitors may also enhance the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Exceptions: Loperamide. Monitor therapy
Pimozide: May enhance the QTc-prolonging effect of QT-prolonging Agents (Moderate Risk). Avoid combination
Piperaquine: QT-prolonging Miscellaneous Agents (Moderate Risk) may enhance the QTc-prolonging effect of Piperaquine. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Probucol: QT-prolonging Miscellaneous Agents (Moderate Risk) may enhance the QTc-prolonging effect of Probucol. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Prucalopride: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Prucalopride. Monitor therapy
QT-prolonging Agents (Highest Risk): May enhance the QTc-prolonging effect of Azithromycin (Systemic). Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Consider therapy modification
QT-prolonging Antidepressants (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Miscellaneous Agents (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Antipsychotics (Moderate Risk): QT-prolonging Miscellaneous Agents (Moderate Risk) may enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Pimozide. Monitor therapy
QT-prolonging Class IC Antiarrhythmics (Moderate Risk): QT-prolonging Miscellaneous Agents (Moderate Risk) may enhance the QTc-prolonging effect of QT-prolonging Class IC Antiarrhythmics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Kinase Inhibitors (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Miscellaneous Agents (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Miscellaneous Agents (Moderate Risk). QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of QT-prolonging Miscellaneous Agents (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Quinolone Antibiotics (Moderate Risk): QT-prolonging Miscellaneous Agents (Moderate Risk) may enhance the QTc-prolonging effect of QT-prolonging Quinolone Antibiotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Strong CYP3A4 Inhibitors (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Miscellaneous Agents (Moderate Risk). QT-prolonging Strong CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of QT-prolonging Miscellaneous Agents (Moderate Risk). Avoid combination
Ranolazine: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Ranolazine. Monitor therapy
RifAXIMin: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of RifAXIMin. Monitor therapy
Silodosin: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Silodosin. Monitor therapy
Simvastatin: Azithromycin (Systemic) may enhance the myopathic (rhabdomyolysis) effect of Simvastatin. Monitor therapy
Sincalide: Drugs that Affect Gallbladder Function may diminish the therapeutic effect of Sincalide. Management: Consider discontinuing drugs that may affect gallbladder motility prior to the use of sincalide to stimulate gallbladder contraction. Consider therapy modification
Sodium Picosulfate: Antibiotics may diminish the therapeutic effect of Sodium Picosulfate. Management: Consider using an alternative product for bowel cleansing prior to a colonoscopy in patients who have recently used or are concurrently using an antibiotic. Consider therapy modification
Sodium Stibogluconate: QT-prolonging Miscellaneous Agents (Moderate Risk) may enhance the QTc-prolonging effect of Sodium Stibogluconate. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Tacrolimus (Systemic): Azithromycin (Systemic) may increase the serum concentration of Tacrolimus (Systemic). Monitor therapy
Tacrolimus (Topical): Macrolide Antibiotics may increase the serum concentration of Tacrolimus (Topical). Monitor therapy
Talazoparib: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Talazoparib. Management: These listed exceptions are discussed in detail in separate interaction monographs. Monitor therapy
Tegaserod: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Tegaserod. Monitor therapy
Topotecan: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Topotecan. Avoid combination
Toremifene: Azithromycin (Systemic) may enhance the QTc-prolonging effect of Toremifene. Monitor therapy
Typhoid Vaccine: Antibiotics may diminish the therapeutic effect of Typhoid Vaccine. Only the live attenuated Ty21a strain is affected. Management: Vaccination with live attenuated typhoid vaccine (Ty21a) should be avoided in patients being treated with systemic antibacterial agents. Use of this vaccine should be postponed until at least 3 days after cessation of antibacterial agents. Consider therapy modification
Ubrogepant: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Ubrogepant. Management: Use an initial ubrogepant dose of 50 mg and second dose (if needed) of 50 mg when used with a P-gp inhibitor. Consider therapy modification
VinCRIStine (Liposomal): P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of VinCRIStine (Liposomal). Avoid combination
Vitamin K Antagonists (eg, warfarin): Macrolide Antibiotics may increase the serum concentration of Vitamin K Antagonists. Monitor therapy
Adverse Reactions
>10%: Gastrointestinal: Loose stools (≤14%; single-dose regimens tend to be associated with increased incidence), vomiting (children, single-dose regimens tend to be associated with increased incidence: 1% to 14%; adults: ≤2%; adults, single 2 g dose: 1% to 7%), diarrhea (2% to 9%; single-dose regimens 4% to 14%), nausea (≤7%; high single-dose regimens 4% to 18%)
1% to 10%:
Cardiovascular: Chest pain (≤1%), palpitations (≤1%)
Central nervous system: Dizziness (≤1%), drowsiness (≤1%), fatigue (≤1%), headache (≤1%), vertigo (≤1%)
Dermatologic: Skin rash (≤5%; single-dose regimens tend to be associated with increased incidence), dermatitis (children: ≤2%), pruritus (≤2%), skin photosensitivity (≤1%)
Endocrine & metabolic: Increased lactate dehydrogenase (1% to 3%), increased gamma-glutamyl transferase (1% to 2%), increased serum potassium (1% to 2%), decreased serum bicarbonate (adults: ≥1%), decreased serum glucose (adults: >1%)
Gastrointestinal: Abdominal pain (1% to 7%; single-dose regimens tend to be associated with increased incidence), anorexia (≤2%), dysgeusia (≤1%), dyspepsia (≤1%), flatulence (≤1%), gastritis (≤1%), melena (adults, multiple-dose regimens: ≤1%), mucositis (≤1%), oral candidiasis (≤1%)
Genitourinary: Vaginitis (≤3%), genital candidiasis (adults, multiple-dose regimens: ≤1%)
Hematologic & oncologic: Decrease in absolute neutrophil count (children: 15% to 16%; 500 to 1,500 cells/mm3), decreased hematocrit (adults: >1%), decreased hemoglobin (adults: >1%), increased neutrophils (adults: >1%), thrombocythemia (adults: >1%), change in neutrophil count (children: ≥1%), eosinophilia (≥1%), lymphocytopenia (≥1%)
Hepatic: Increased serum ALT (≤6%), increased serum AST (≤6%), increased serum bilirubin (≤3%), cholestatic jaundice (≤1%)
Local (adults with IV administration): Pain at injection site (7%), local inflammation (3%)
Neuromuscular & skeletal: Increased creatine phosphokinase (1% to 2%)
Renal: Increased serum creatinine (≤6%), increased blood urea nitrogen (≤1%), nephritis (adults, multiple-dose regimens: ≤1%)
Respiratory: Bronchospasm (≤1%)
Miscellaneous: Fever (children: (≤2%)
<1%, postmarketing, and/or case reports: Abnormal stools, acute generalized exanthematous pustulosis, acute renal failure, ageusia, aggressive behavior, agitation, alteration in sodium, altered sense of smell, altered serum glucose, anaphylaxis, anemia, angioedema, anosmia, anxiety, arthralgia, asthma, basophilia, bronchitis, cardiac arrhythmia, chills, Clostridioides (formerly Clostridium) difficile-associated diarrhea, conjunctivitis (children), constipation, convulsions, cough, deafness, decreased serum potassium (children), decreased serum sodium, diaphoresis, DRESS syndrome, dyspnea, dysuria, eczema, edema, emotional lability, enteritis, erythema multiforme, exacerbation of myasthenia gravis, facial edema, flu-like symptoms, fungal dermatitis, fungal infection, gastrointestinal disease, hearing loss, hepatic failure, hepatic insufficiency, hepatic necrosis, hepatitis, hepatotoxicity (idiosyncratic) (Chalasani 2014), hostility, hyperactivity, hyperkinesia, hypersensitivity reaction, hypotension, increased monocytes, increased serum alkaline phosphatase, increased serum bicarbonate, increased serum glucose, increased serum phosphate, interstitial nephritis, insomnia, irritability, jaundice, Lambert-Eaton syndrome, leukopenia, maculopapular rash, malaise, nervousness, neutropenia, otitis media, pain, pancreatitis, paresthesia, pharyngitis, pleural effusion, prolonged Q-T interval on ECG, pseudomembranous colitis, pyloric stenosis, pyloric stenosis (infantile hypertrophic), rhinitis, seizure, Stevens-Johnson syndrome, syncope, thrombocytopenia, tinnitus, tongue discoloration, torsades de pointes toxic epidermal necrolysis, urticaria, ventricular tachycardia, vesiculobullous dermatitis, weakness
Warnings/Precautions
Concerns related to adverse effects:
- Hypersensitivity reactions: Allergic reactions (eg, angioedema, anaphylaxis, Stevens-Johnson syndrome, toxic epidermal necrolysis and drug reaction with eosinophilia and systemic symptoms [DRESS]) have been reported (rare), including fatalities; reappearance of allergic reaction may occur shortly after discontinuation of symptomatic treatment without further azithromycin exposure.
- Altered cardiac conduction: Macrolides (especially erythromycin) have been associated with rare QTc prolongation and ventricular arrhythmias, including torsades de pointes; consider avoiding use in patients with prolonged QT interval, congenital long QT syndrome, history of torsades de pointes, bradyarrhythmias, uncorrected hypokalemia or hypomagnesemia, clinically significant bradycardia, uncompensated heart failure, or concurrent use of Class IA (eg, quinidine, procainamide) or Class III (eg, amiodarone, dofetilide, sotalol) antiarrhythmic agents or other drugs known to prolong the QT interval.
- Cardiac risk: A retrospective cohort study done in Tennessee Medicaid patients demonstrated an increased cardiac risk with azithromycin relative to amoxicillin or ciprofloxacin, and similar risk compared to levofloxacin; notably, increased cardiac mortality (an estimated 47 additional deaths per 1 million 5-day courses of treatment compared to amoxicillin) was associated with higher baseline cardiovascular risk (Ray 2012); however, these data may not be generalizable to the population as a whole (Ray 1989). In another retrospective population study of US veterans, azithromycin was shown to significantly increase the risk of mortality and arrhythmia on days 1 to 5, but not on days 6 to 10 after dispensing the prescription (Rao 2014). In contrast, 2 additional large retrospective cohort studies did not demonstrate an increased risk of cardiovascular events, including all-cause mortality or cardiovascular death (Svanstrom 2013, Mortensen 2014). The implications of these data have yet to be determined.
- Superinfection: Prolonged use may result in fungal or bacterial superinfection, including C. difficile-associated diarrhea (CDAD); CDAD has been observed >2 months postantibiotic treatment.
Disease-related concerns:
- Bronchiolitis obliterans: When studied to prevent bronchiolitis obliterans syndrome in patients with hematologic malignancy who underwent allogeneic hematopoietic cell transplantation, rates of cancer relapse and mortality were increased among patients receiving long-term azithromycin, leading to early trial termination (Bergeron 2017; FDA Drug Safety Communication 2018).
- Gonorrhea/syphilis: May mask or delay symptoms of incubating gonorrhea or syphilis, so appropriate culture and susceptibility tests should be performed prior to initiating a treatment regimen.
- Hepatic impairment: Use with caution in patients with preexisting liver disease; hepatocellular and/or cholestatic hepatitis (with or without jaundice), hepatic necrosis, failure, and death have occurred. Discontinue immediately if symptoms of hepatitis occur (malaise, nausea, vomiting, abdominal colic, fever).
- Myasthenia gravis: Use with caution in patients with myasthenia gravis; exacerbation and new onset of symptoms have occurred.
- Renal impairment: Use with caution in patients with severe renal impairment (GFR <10 mL/minute); increased gastrointestinal adverse effects may occur.
Special populations:
- Infants: Use of azithromycin in neonates and infants (treatment up to 42 days of life) has been associated with infantile hypertrophic pyloric stenosis (IHPS); observe for non-bilious vomiting or irritability with feeding (Eberly 2015).
Dosage form specific issues:
- Oral suspensions: Immediate release and extended release suspensions are not interchangeable.
Monitoring Parameters
Liver function tests, CBC with differential
Pregnancy
Pregnancy Considerations
Azithromycin crosses the placenta (Ramsey 2003).
The maternal serum half-life of azithromycin is unchanged in early pregnancy and decreased at term; however, high concentrations of azithromycin are sustained in the myometrium and adipose tissue (Fischer 2012; Ramsey 2003).
Azithromycin may be used as an alternative or adjunctive prophylactic antibiotic in females undergoing unplanned cesarean delivery (ACOG 199 2018). Azithromycin is recommended for the treatment of several infections, including chlamydia, gonococcal infections, and Mycobacterium avium complex in pregnant patients (consult current guidelines) (CDC [Workowski 2015]; HHS [OI adult] 2019). Azithromycin may also be used in certain situations prior to vaginal delivery in females at high risk for endocarditis (ACOG 199 2018).
Patient Education
What is this drug used for?
- It is used to treat or prevent bacterial infections.
Frequently reported side effects of this drug
- Abdominal pain
- Diarrhea
- Headache
- Nausea
- Vomiting
- Injection site pain
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Fast heartbeat
- Abnormal heartbeat
- Trouble hearing
- Chest pain
- Swollen glands
- Vision changes
- Dizziness
- Passing out
- Myasthenia grave like muscle weakness, difficulty chewing, difficulty swallowing, difficulty breathing, droopy eyelids, blurred vision, or double vision.
- Clostridioides (formerly Clostridium) difficile-associated diarrhea like abdominal pain or cramps, severe diarrhea or watery stools, or bloody stools.
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.