Boxed Warning
Abrupt withdrawal (injection):
Abrupt discontinuation of intrathecal baclofen, regardless of the cause, has resulted in sequelae that include high fever, altered mental status, exaggerated rebound spasticity, and muscle rigidity, which in rare cases has advanced to rhabdomyolysis, multiple organ-system failure, and death.
Prevention of abrupt discontinuation of intrathecal baclofen requires careful attention to programming and monitoring of the infusion system, refill scheduling and procedures, and pump alarms. Advise patients and caregivers of the importance of keeping scheduled refill visits and educate them on the early symptoms of baclofen withdrawal. Give special attention to patients at apparent risk (eg, spinal cord injuries at T-6 or above, communication difficulties, history of withdrawal symptoms from oral or intrathecal baclofen). Consult the technical manual of the implantable infusion system for additional postimplant clinician and patient information.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Solution, Intrathecal:
Gablofen: 40,000 mcg/20 mL (20 mL [DSC])
Generic: 10 mg/20 mL (20 mL); 40 mg/20 mL (20 mL); 20,000 mcg/20 mL (20 mL)
Solution, Intrathecal [preservative free]:
Gablofen: 10,000 mcg/20 mL (20 mL); 20,000 mcg/20 mL (20 mL) [antioxidant free]
Gablofen: 40,000 mcg/20 mL (20 mL)
Lioresal: 0.05 mg/mL (1 mL); 10 mg/20 mL (20 mL [DSC]); 10 mg/5 mL (5 mL [DSC]); 40 mg/20 mL (20 mL) [antioxidant free]
Lioresal: 10 mg/20 mL (20 mL); 10 mg/5 mL (5 mL) [antioxidant free, pyrogen free]
Solution, Oral:
Ozobax: 5 mg/5 mL (473 mL) [contains methylparaben, propylparaben; grape flavor]
Solution Prefilled Syringe, Intrathecal [preservative free]:
Gablofen: 50 mcg/mL (1 mL) [antioxidant free, latex free]
Gablofen: 50 mcg/mL (1 mL [DSC]); 10,000 mcg/20 mL (20 mL [DSC]); 40,000 mcg/20 mL (20 mL [DSC]); 20,000 mcg/20 mL (20 mL) [antioxidant free]
Gablofen: 10,000 mcg/20 mL (20 mL); 40,000 mcg/20 mL (20 mL) [antioxidant free, pyrogen free]
Tablet, Oral:
Generic: 5 mg, 10 mg, 20 mg
Pharmacology
Mechanism of Action
Inhibits the transmission of both monosynaptic and polysynaptic reflexes at the spinal cord level, possibly by hyperpolarization of primary afferent fiber terminals, with resultant relief of muscle spasticity
Pharmacokinetics/Pharmacodynamics
Absorption
Oral: Rapid; absorption from the GI tract is thought to be dose dependent; in pediatric patients (age range: 2 to 17 years) with cerebral palsy, absorption from GI tract highly variable and delayed (reported time lag: 0.59 ± 0.28 hours) (He 2014)
Distribution
Volume of distribution: Pediatric patients (age range: 2 to 17 years: Oral: Highly variable: 1.16 L/kg with 43.5% interindividual variability (He 2014)
Metabolism
Hepatic (15% of dose) (He 2014)
Excretion
Urine (>70% as unchanged drug) and feces (Brunton 2011)
Onset of Action
Intrathecal bolus: 30 minutes to 1 hour; Continuous infusion: 6 to 8 hours after infusion initiation
Peak effect: Intrathecal bolus: 4 hours (effects may last 4 to 8 hours); Continuous infusion: 24 to 48 hours
Time to Peak
Serum: Oral: 1 hour (0.5 to 4 hours) (Brunton 2011)
Half-Life Elimination
Oral:
Pediatric patients with cerebral palsy (age range: 2 to 17 years): 4.5 hours (He 2014)
Adults: Solution: 5.7 hours; Tablets: 3.75 ± 0.96 hours (Brunton 2011)
Intrathecal: CSF elimination half-life: 1.5 hours over the first 4 hours
Protein Binding
30%
Use: Labeled Indications
Spasticity:
Oral: Management of reversible spasticity associated with multiple sclerosis or spinal cord lesions
Intrathecal: Management of severe spasticity of spinal cord origin (eg, spinal cord injury, multiple sclerosis) or cerebral origin (eg, cerebral palsy, traumatic brain injury) in patients ≥4 years; may be considered as an alternative to destructive neurosurgical procedures.
Limitations of use: Patients should first respond to a screening dose of intrathecal baclofen prior to consideration for long term infusion via an implantable pump. For spasticity of spinal cord origin, chronic infusion via an implantable pump should be reserved for patients unresponsive to oral baclofen therapy, or those who experience intolerable CNS side effects at effective doses. Patients with spasticity due to traumatic brain injury should wait at least one year after the injury before consideration of long term intrathecal baclofen therapy.
Use: Off Label
Alcoholic liver disease (alcohol abstinence)byes
In a randomized, placebo-controlled study in patients with alcoholic liver disease, treatment with baclofen significantly improved the proportion of patients who achieved and maintained alcohol abstinence Addolorato 2007.
Based on the American College of Gastroenterology (ACG) for Alcoholic Liver Disease and American Association for the Study of Liver Diseases (AASLD) guidelines for the management of adult patients with ascites due to cirrhosis, baclofen may be used to reduce alcohol craving and consumption in patients with ascites due to alcoholic liver disease.
Gastroesophageal reflux diseaseb
Data from a meta-analysis and a controlled trial support the use of baclofen for gastroesophageal reflux disease (GERD); baclofen was associated with reductions in the number of reflux episodes and rate of transient lower esophageal sphincter relaxations in patients with GERD
Hiccups (singultus)b
Evidence from a limited number of small controlled and noncontrolled trials and several case reports suggests that baclofen may be effective in resolving or reducing symptoms in patients with chronic hiccups due to various causes. Baclofen may be a useful alternative when other treatments have failed
Nystagmusc
Inconsistent results have been reported with baclofen use for the treatment of nystagmus Averbuch-Heller 1997, Comer 2006, Dieterich 1991. It is unclear why some patients with nystagmus benefit from baclofen therapy and others do not. However, given the lack of a definitive symptomatic treatment for this disease, a therapeutic trial of baclofen may be warranted before more invasive or risky approaches such as botulinum toxin injections or surgery are attempted.
Trigeminal neuralgiacyes
Limited evidence from a small, double-blind, crossover trial suggests baclofen is beneficial for trigeminal neuralgia Fromm 1984.
Based on the European Academy of Neurology guideline on trigeminal neuralgia, baclofen is recommended based on limited evidence as monotherapy or as an adjunct for trigeminal neuralgia when first-line agents are not effective or tolerated EAN [Bendtsen 2019].
Contraindications
Hypersensitivity to baclofen or any component of the formulation
Intrathecal formulation: IV, IM, SubQ, or epidural administration
Dosage and Administration
Dosing: Adult
Spasticity:
Oral: Initial: 5 mg 3 times daily; may increase by 5 mg per dose every 3 days (ie, 5 mg 3 times daily for 3 days, then 10 mg 3 times daily for 3 days, etc.) until optimal response is reached. Do not exceed 80 mg daily (20 mg 4 times daily).
Intrathecal:
Screening dose: Initial: 50 mcg for 1 dose; following initial administration, observe patient for 4 to 8 hours. A positive response consists of a significant decrease in muscle tone and/or frequency and/or severity of spasms. If response is inadequate, may give 75 mcg as a second screening dose 24 hours after the first screening dose; observe patient for 4 to 8 hours. If response is still inadequate, may repeat a final screening dose of 100 mcg given 24 hours after the second screening dose. Patients not responding to screening dose of 100 mcg should not be considered for chronic infusion/implanted pump.
Dose titration following pump implant: After positive response to screening dose, a maintenance intrathecal infusion can be administered via an implanted intrathecal pump.
Initial total daily dose via pump: Double the screening dose that gave a positive response and administer over 24 hours, unless efficacy of the bolus dose was maintained for >8 hours, then infuse a dose equivalent to the screening dose over 24 hours. Do not increase dose in first 24 hours (to allow steady state to be achieved); thereafter, dosage adjustments may be made by increasing daily dose slowly by 10% to 30% (spasticity of spinal cord origin) or 5% to 15% (spasticity of cerebral origin) once every 24 hours until satisfactory response.
Maintenance: Daily dose may be increased 5% to 20% (maximum increase: 20%) (spasticity of cerebral origin) or by 10% to 40% (maximum increase: 40%) (spasticity of spinal cord origin). Dose may also be decreased 10% to 20% for adverse effects. Most patients have been adequately maintained on 90 mcg to 703 mcg daily (spasticity of cerebral origin) or 300 mcg to 800 mcg daily (spasticity of spinal cord origin). Experience with doses >1,000 mcg daily is limited.
Note: Dosage adjustments may be required often during the first few months of therapy to adjust for life style changes due to alleviation of spasticity. Maintain lowest dose that produces adequate response. Most patients require gradual increases over time to maintain optimal response. Sudden large requirements for a dose increase may indicate a catheter complication (eg, kink, dislodgement). Titrate dose to allow sufficient muscle tone and occasional spasms to optimize activities of daily living, support circulation, and possibly prevent DVT formation. Use extreme caution when filling the pump; follow manufacturer instructions carefully. 5% to 10% of patients receiving chronic therapy become refractory to dose adjustments; may consider a drug holiday (hospitalized patients only) with a gradual withdrawal over 2 to 4 weeks and use of alternative spasticity management methods. Following the drug holiday intrathecal baclofen may be resumed at the initial continuous infusion dose.
Alcoholic liver disease, alcohol abstinence (off-label use): Oral:
Initial: 5 mg 3 times daily for 3 days
Maintenance: May increase dose at a 3 to 5 day interval based on patient tolerance (ACG [Singal 2018]) to 10 mg 3 times daily (maximum: 15 mg 3 times daily) (AASLD [Runyon 2012]; ACG [Singal 2018]; Addolorato 2007).
Gastroesophageal reflux disease (off-label use): Oral: 10 mg 4 times daily (Ciccaglione 2003)
Hiccups (off-label use): Oral: 5 to 10 mg 3 times daily (maximum: 75 mg daily in divided doses) (Guelaud 1995; Zhang 2014)
Nystagmus (off-label use): Oral: 5 mg 3 times daily; may increase at weekly intervals until optimal response is reached or intolerable adverse effects occur. Dosage range studied: 15 to 120 mg daily in divided doses (Cormer 2006; Dieterich 1991). Additional data may be necessary to further define the role of baclofen in the treatment of this condition.
Trigeminal neuralgia (off-label use): Oral: Initial: 5 to 10 mg 3 times daily (dose may be as low as 10 mg daily); may increase daily dose based on response and tolerability in increments of 10 mg every other day over 1 to 2 weeks up to 80 mg/day in 3 to 4 divided doses (Bajwa 2019; Fromm 1984; Steardo 1984).
Dosing: Geriatric
Oral: Refer to adult dosing; use with caution. If benefits are not observed, withdraw the drug slowly.
Dosing: Pediatric
Spasticity:
Oral: Note: Dose-related side effects (eg, sedation) may be minimized by slow titration; lower initial doses than described below (2.5 to 10 mg daily) may be used with subsequent titration to 8 hourly doses (Scheinberg 2006). There is limited published data in infants and children; the following is a compilation of small prospective studies (Goyal 2016; Milla 1977; Scheinberg 2006) and one large retrospective analysis of baclofen use in children (Lubsch 2006). Efficacy results variable (AAN [Delgado 2010]; Navarrete-Opazo 2016):
Infants ≥4 months and Children <2 years: Very limited data available: Oral: Usual dose: 10 to 20 mg/day in divided doses every 8 hours; begin at low end of range and titrate dose to patient response (Lubsch 2006); titration intervals of every 7 days have been used in pediatric patients ≥2 years (Goyal 2016; Scheinberg 2006). Maximum daily dose: 40 mg/day (Lubsch 2006). Dosing based on a retrospective study of 87 patients (age 9 ± 6 years; range: 0.4 to 23.5 years) with spasticity due to cerebral palsy or traumatic brain injury (Lubsch 2006). Note: To minimize dose-related side effects (eg, sedation), lower initial doses (eg, 2.5 mg once to 3 times daily) may be considered and has been reported in pediatric patients >2 years (Goyal 2016; Scheinberg 2006).
Children 2 to 7 years: Limited data available: Oral: Initial: 2.5 mg 3 times daily; titrate dose by 5 mg increments at weekly intervals to patient response; usual dose: 20 to 40 mg/day. Maximum daily dose: 60 mg/day (Goyal 2016; Lubsch 2006; Milla 1977; Scheinberg 2006). Note: Initial doses of 5 to 10 mg/day divided every 8 hours and more frequent titration intervals (ie, every 3 days) have also been described (Milla 1977).
Children ≥8 years and Adolescents: Limited data available in children <12 years: Oral: Initial: 5 mg 3 times daily; titrate dose to patient response at weekly intervals to usual dose of 30 to 40 mg/day; maximum daily dose: 60 mg/day (Goyal 2016; Lubsch 2006; Milla 1977; Scheinberg 2006); some patients ≥12 years may require every-6-hour dosing; usual maximum daily dose range: 60 to 80 mg/day. Note: Lower initial doses (5 to 10 mg/day) and more frequent titration intervals (every 3 days) have also been described (Milla 1977). Higher maximum daily doses (up to 200 mg/day) have been described in some patients in a retrospective review, usually the higher doses were needed over time (Lubsch 2006).
Intrathecal: Note: Dosage adjustments may be required often during the first few months of therapy to adjust for life style changes due to alleviation of spasticity. Maintain lowest dose that produces adequate response. Most patients require gradual increases over time to maintain optimal response. Sudden large requirements for a dose increase may indicate a catheter complication (eg, kink, dislodgement). Titrate dose to allow sufficient muscle tone and occasional spasms to optimize activities of daily living, support circulation, and possibly prevent DVT formation. Use extreme caution when filling the pump; follow manufacturer instructions carefully. With chronic therapy, 5% to 10% of patients will become refractory to dose adjustments; may consider a drug holiday (hospitalized patients only) with a gradual withdrawal over 2 to 4 weeks and use of alternative spasticity management methods. Following the drug holiday intrathecal baclofen may be resumed at the initial continuous infusion dose. Limited data available in children <4 years old, dosing for this age group based on expert consensus recommendations (Berweck 2014).
Screening dose:
Children <4 years: Limited data available: Intrathecal: Initial: 25 mcg; if response is inadequate, double the initial dose and administer 24 hours after the first dose (Berweck 2014).
Children ≥4 years and Adolescents: Intrathecal: Initial: 50 mcg (1 mL) for 1 dose; following initial administration, observe patient for 4 to 8 hours. A positive response consists of a significant decrease in muscle tone and/or frequency and/or severity of spasms. If response is inadequate, may give 75 mcg as a second screening dose 24 hours after the first screening dose; observe patient for 4 to 8 hours. If response is still inadequate, may repeat a final screening dose of 100 mcg given 24 hours after the second screening dose. Patients not responding to screening dose of 100 mcg should not be considered for chronic infusion/implanted pump. Note: A 25 mcg initial screening dose may be considered in very small pediatric patients.
Dose titration following pump implant: Children and Adolescents: After positive response to screening dose, a maintenance intrathecal infusion can be administered via an implanted intrathecal pump.
Initial total daily dose via pump: Children and Adolescents: Intrathecal: Double the screening dose that gave a positive response and administer over 24 hours, unless efficacy of the bolus dose was maintained for >8 hours, then infuse a dose equivalent to the screening dose over 24 hours. Do not increase dose in first 24 hours (to allow steady state to be achieved); thereafter, increase daily dose slowly by 5% to 15% once every 24 hours until satisfactory response is achieved; usual range: 50 to 100 mcg daily (Berweck 2014).
Titration to maintenance dose: Children ≥4 years and Adolescents: Intrathecal: Daily dose may be increased 5% to 20% (maximum increase: 20%); may also be decreased 10% to 20% for adverse effects.
Some experts have suggested the following titration parameters: Children and Adolescents (Berweck 2014): Intrathecal:
Inpatient titration: May adjust by 10% to 20% of dose (usual dose change is 50 mcg); maximum increment change: 100 mcg.
Outpatient titration: May adjust by 10% of daily dose (usual dose change is 25 mcg).
Usual maintenance dose: Children and Adolescents: Intrathecal: 100 to 2,000 mcg daily (Berweck 2014); the manufacturer provides the following:
Children 4 to 12 years: Intrathecal: 24 to 1,199 mcg daily (average: 274 mcg/day).
Children ≥12 years and Adolescents: Intrathecal: 90 to 703 mcg daily; daily doses have ranged from 22 to 1,400 mcg; experience with doses >1,000 mcg daily is limited.
Reconstitution
Intrathecal: Screening doses are a 50 mcg/mL concentration and only the 1 mL screening ampul or screening syringe (50 mcg/mL) is used; do not further dilute. Maintenance infusions for patients who require concentrations other than 500 mcg/mL, 1,000 mcg/mL, or 2,000 mcg/mL must be diluted with preservative-free sodium chloride.
Extemporaneously Prepared
Note: A baclofen suspension (1 mg/mL or 5 mg/mL) is commercially available as a compounding kit (First-Baclofen) and as a 1 mg/mL oral solution (Ozobax). Compounded oral suspension may be available in multiple concentrations (eg, up to 10 times more concentrated); use caution to avoid confusion; verify concentration.
5 mg/mL Oral Suspension (ASHP Standard Concentration) (ASHP 2017)
A 5 mg/mL oral suspension may be made with tablets. Crush thirty 20 mg tablets in a mortar and reduce to a fine powder. Add a small amount of glycerin and mix to a uniform paste. Mix while adding Simple Syrup, NF in incremental proportions to almost 120 mL; transfer to a calibrated bottle, rinse mortar with vehicle, and add a sufficient quantity of vehicle to make 120 mL. Label “shake well” and “refrigerate.” Stable for 35 days (Johnson 1993).
Johnson CE, Hart SM. Stability of an extemporaneously compounded baclofen oral liquid. Am J Hosp Pharm. 1993;50(11):2353-2355.8266961
10 mg/mL Oral Suspension: Note: Commercially available suspension is more dilute (eg, up to 10 times more dilute); use caution to avoid confusion; verify concentrations.
A 10 mg/mL oral suspension may be made with tablets. Crush one-hundred-twenty 10 mg tablets in a mortar and reduce to a fine powder. Add small portions (60 mL) of a 1:1 mixture of Ora-Sweet and Ora-Plus and mix to a uniform paste; mix while adding the vehicle in incremental proportions to almost 120 mL; transfer to a calibrated bottle, rinse mortar with vehicle, and add quantity of vehicle sufficient to make 120 mL. Label “shake well” and “refrigerate.” Stable for 60 days (Allen 1996).
Allen LV Jr, Erickson MA 3rd. Stability of baclofen, captopril, diltiazem hydrochloride, dipyridamole, and flecainide acetate in extemporaneously compounded oral liquids. Am J Health Syst Pharm. 1996;53(18):2179-2184.8879325
Administration
Intrathecal: For screening dosages, administer as a bolus injection (50 mcg/mL concentration) by barbotage into the subarachnoid space over at least 1 minute, followed by maintenance continuous infusion. Do not administer intrathecal formulation IV, IM, SubQ, or epidurally.
Oral: Administer without regards to meals.
Storage
Injection: Do not store above 30°C (86°F). Does not require refrigeration. Do not freeze or heat sterilize. Discard any unused solution.
Oral solution: Store refrigerated at 2°C to 8°C (36°F to 46°F). Dispense in a light-resistant container.
Tablets: Store at 20°C to 25°C (68°F to 77°F).
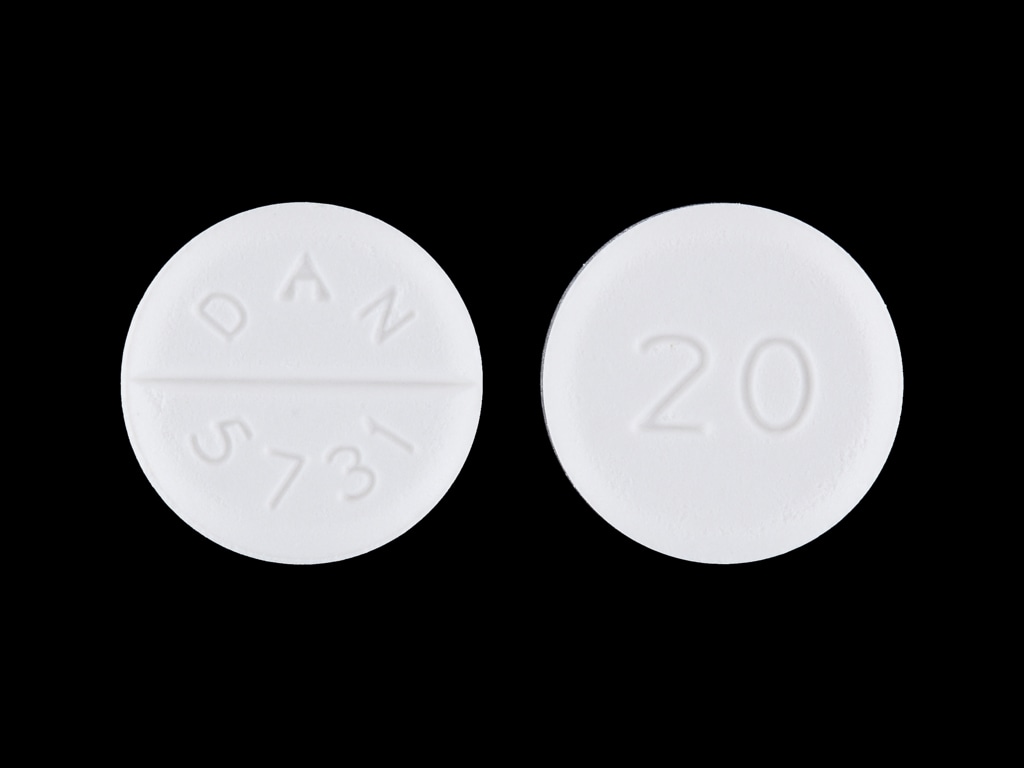
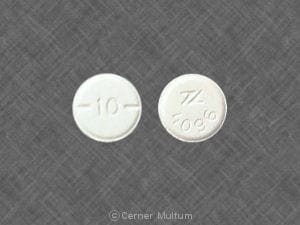
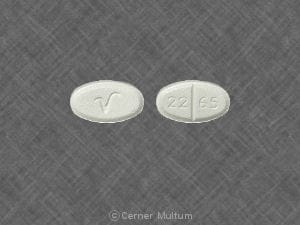
Baclofen Images
Drug Interactions
Alcohol (Ethyl): CNS Depressants may enhance the CNS depressant effect of Alcohol (Ethyl). Monitor therapy
Alizapride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Azelastine (Nasal): CNS Depressants may enhance the CNS depressant effect of Azelastine (Nasal). Avoid combination
Blonanserin: CNS Depressants may enhance the CNS depressant effect of Blonanserin. Consider therapy modification
Botulinum Toxin-Containing Products: Muscle Relaxants (Centrally Acting) may enhance the adverse/toxic effect of Botulinum Toxin-Containing Products. Specifically, the risk for increased muscle weakness may be enhanced. Monitor therapy
Brexanolone: CNS Depressants may enhance the CNS depressant effect of Brexanolone. Monitor therapy
Brimonidine (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromopride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromperidol: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Buprenorphine: CNS Depressants may enhance the CNS depressant effect of Buprenorphine. Management: Consider reduced doses of other CNS depressants, and avoiding such drugs in patients at high risk of buprenorphine overuse/self-injection. Initiate buprenorphine at lower doses in patients already receiving CNS depressants. Consider therapy modification
Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Cannabis: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Chlormethiazole: May enhance the CNS depressant effect of CNS Depressants. Management: Monitor closely for evidence of excessive CNS depression. The chlormethiazole labeling states that an appropriately reduced dose should be used if such a combination must be used. Consider therapy modification
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
CNS Depressants: May enhance the adverse/toxic effect of other CNS Depressants. Monitor therapy
Dimethindene (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Doxylamine: May enhance the CNS depressant effect of CNS Depressants. Management: The manufacturer of Diclegis (doxylamine/pyridoxine), intended for use in pregnancy, specifically states that use with other CNS depressants is not recommended. Monitor therapy
Dronabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Droperidol: May enhance the CNS depressant effect of CNS Depressants. Management: Consider dose reductions of droperidol or of other CNS agents (eg, opioids, barbiturates) with concomitant use. Exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Consider therapy modification
Esketamine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Flunitrazepam: CNS Depressants may enhance the CNS depressant effect of Flunitrazepam. Consider therapy modification
HYDROcodone: CNS Depressants may enhance the CNS depressant effect of HYDROcodone. Management: Avoid concomitant use of hydrocodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
HydrOXYzine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Kava Kava: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Lacidipine: Baclofen may enhance the hypotensive effect of Lacidipine. Monitor therapy
Lemborexant: May enhance the CNS depressant effect of CNS Depressants. Management: Dosage adjustments of lemborexant and of concomitant CNS depressants may be necessary when administered together because of potentially additive CNS depressant effects. Close monitoring for CNS depressant effects is necessary. Consider therapy modification
Lofexidine: May enhance the CNS depressant effect of CNS Depressants. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Magnesium Sulfate: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Methotrimeprazine: CNS Depressants may enhance the CNS depressant effect of Methotrimeprazine. Methotrimeprazine may enhance the CNS depressant effect of CNS Depressants. Management: Reduce adult dose of CNS depressant agents by 50% with initiation of concomitant methotrimeprazine therapy. Further CNS depressant dosage adjustments should be initiated only after clinically effective methotrimeprazine dose is established. Consider therapy modification
MetyroSINE: CNS Depressants may enhance the sedative effect of MetyroSINE. Monitor therapy
Minocycline (Systemic): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Nabilone: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Opioid Agonists: CNS Depressants may enhance the CNS depressant effect of Opioid Agonists. Management: Avoid concomitant use of opioid agonists and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Orphenadrine: CNS Depressants may enhance the CNS depressant effect of Orphenadrine. Avoid combination
Oxomemazine: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
OxyCODONE: CNS Depressants may enhance the CNS depressant effect of OxyCODONE. Management: Avoid concomitant use of oxycodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Paraldehyde: CNS Depressants may enhance the CNS depressant effect of Paraldehyde. Avoid combination
Perampanel: May enhance the CNS depressant effect of CNS Depressants. Management: Patients taking perampanel with any other drug that has CNS depressant activities should avoid complex and high-risk activities, particularly those such as driving that require alertness and coordination, until they have experience using the combination. Consider therapy modification
Piribedil: CNS Depressants may enhance the CNS depressant effect of Piribedil. Monitor therapy
Pramipexole: CNS Depressants may enhance the sedative effect of Pramipexole. Monitor therapy
ROPINIRole: CNS Depressants may enhance the sedative effect of ROPINIRole. Monitor therapy
Rotigotine: CNS Depressants may enhance the sedative effect of Rotigotine. Monitor therapy
Rufinamide: May enhance the adverse/toxic effect of CNS Depressants. Specifically, sleepiness and dizziness may be enhanced. Monitor therapy
Selective Serotonin Reuptake Inhibitors: CNS Depressants may enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk of psychomotor impairment may be enhanced. Monitor therapy
Sodium Oxybate: May enhance the CNS depressant effect of CNS Depressants. Management: Consider alternatives to combined use. When combined use is needed, consider minimizing doses of one or more drugs. Use of sodium oxybate with alcohol or sedative hypnotics is contraindicated. Consider therapy modification
Suvorexant: CNS Depressants may enhance the CNS depressant effect of Suvorexant. Management: Dose reduction of suvorexant and/or any other CNS depressant may be necessary. Use of suvorexant with alcohol is not recommended, and the use of suvorexant with any other drug to treat insomnia is not recommended. Consider therapy modification
Tapentadol: May enhance the CNS depressant effect of CNS Depressants. Management: Avoid concomitant use of tapentadol and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Tetrahydrocannabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Thalidomide: CNS Depressants may enhance the CNS depressant effect of Thalidomide. Avoid combination
Tolperisone: May enhance the adverse/toxic effect of Muscle Relaxants (Centrally Acting). Management: Monitor for increased sedation or CNS effects if tolperisone is combined with other centrally acting muscle relaxants. Consider decreasing the tolperisone dose if these agents are combined. Consider therapy modification
Trimeprazine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Urapidil: Baclofen may enhance the hypotensive effect of Urapidil. Monitor therapy
Zolpidem: CNS Depressants may enhance the CNS depressant effect of Zolpidem. Management: Reduce the Intermezzo brand sublingual zolpidem adult dose to 1.75 mg for men who are also receiving other CNS depressants. No such dose change is recommended for women. Avoid use with other CNS depressants at bedtime; avoid use with alcohol. Consider therapy modification
Adverse Reactions
>10%:
Central nervous system: Hypotonia (2% to 35%), drowsiness (6% to 21%), confusion (1% to 11%), headache (2% to 11%)
Gastrointestinal: Nausea (1% to 12%), vomiting (2% to 11%)
1% to 10%:
Cardiovascular: Hypotension (≤9%), peripheral edema (≤3%)
Central nervous system: Seizure (≤10%), dizziness (2% to 8%), insomnia (≤7%), paresthesia (≤7%), hypertonia (≤6%), pain (≤4%), speech disturbance (≤4%), depression (2%), coma (≤2%), abnormality in thinking (≤1%), agitation (≤1%), chills (≤1%)
Dermatologic: Pruritus (4%), urticaria (≤1%)
Gastrointestinal: Constipation (≤6%), sialorrhea (≤3%), xerostomia (≤3%), diarrhea (≤2%)
Genitourinary: Urinary retention (≤8%), urinary frequency (≤6%), difficulty in micturition (2%), impotence (≤2%), urinary incontinence (≤2%)
Neuromuscular & skeletal: Asthenia (≤2%), back pain (≤2%), tremor (≤1%)
Ophthalmic: Amblyopia (≤2%)
Respiratory: Hypoventilation (≤4%), pneumonia (≤2%), dyspnea (≤1%)
Miscellaneous: Accidental injury (≤4%)
<1%, postmarketing, and/or case reports: Abdominal pain, accommodation disturbance, akathisia, albuminuria, alopecia, amnesia, ankle edema, anorexia, anxiety, apnea, ataxia, blurred vision, bradycardia, carcinoma, chest pain, contact dermatitis, decreased libido, deep vein thrombophlebitis, dehydration, dermal ulcer, diaphoresis, diplopia, dysarthria, dysautonomia, dysgeusia, dysphagia, dystonia, dysuria, epilepsy, erectile dysfunction, euphoria, excitement, facial edema, fecal incontinence, fever, gastrointestinal hemorrhage, hallucination, hematuria, hyperglycemia, hyperhidrosis, hypertension, hyperventilation, hypothermia, hysteria, inhibited ejaculation, intestinal obstruction, leukocytosis, loss of postural reflex, malaise, miosis, muscle rigidity, myalgia, mydriasis, nasal congestion, nephrolithiasis, nocturia, nystagmus disorder, occult blood in stools, oliguria, opisthotonus, orgasm disturbance, pallor, palpitations, paranoid ideation, personality disorder, petechial rash, priapism, pulmonary embolism, scoliosis, scoliosis progression, sedated state, sexual disorder, skin rash, slurred speech, strabismus, suicidal ideation, syncope, taste disorder, tinnitus, tongue irritation, vaginitis, vasodilation, weight gain, weight loss
Warnings/Precautions
Concerns related to adverse effects:
- CNS depression: May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks which require mental alertness (eg, operating machinery or driving).
- Intrathecal mass: Cases (most from pharmacy compounded preparations) of intrathecal mass formation at the implanted catheter tip have been reported; patients may experience worsening or return of spasticity, pain, inadequate response to dose adjustments, and/or neurological deficit/dysfunction. Neurosurgical evaluation and/or an appropriate imaging study should be considered if a mass is suspected.
- Urinary retention: May cause acute urinary retention (may be related to underlying disease); use with caution in patients with urinary obstruction.
Disease-related concerns:
- Autonomic dysreflexia: Use with caution in patients with a history of autonomic dysreflexia; presence of nociceptive stimuli or abrupt baclofen withdrawal may cause an autonomic dysreflexic episode.
- Gastrointestinal disorders: Use with caution in patients with peptic ulcer disease, decreased GI motility, and/or gastrointestinal obstructive disorders.
- Psychiatric disease: Use with caution in patients with psychotic disorders, schizophrenia, or confusional states; may cause exacerbation of condition.
- Renal impairment: Use with caution in patients with renal impairment; baclofen is eliminated primarily unchanged via the kidneys. Multiple cases describing neurotoxicity due to oral baclofen accumulation in adult patients with varying levels of renal impairment have been reported in the literature. In patients with renal impairment, initiation of oral baclofen at lower doses and/or extended intervals has been suggested (Aisen 1994; Chen 1997; Chou 2006; El-Husseini 2011; Peces 1998; Su 2009; Vlavonu 2014).
- Respiratory disease: Use with caution in patients with respiratory disease.
- Seizure disorder: Loss of seizure control has been reported in patients treated with baclofen; use with caution and monitor patients with a history of seizure disorder.
Special populations:
- Elderly: Use with caution in elderly patients; may be more sensitive to adverse CNS effects, especially at higher doses.
- Neonates: Neonatal withdrawal symptoms (eg, increased muscle tone, jitteriness, tremor, seizure), beginning hours to days after delivery, have been reported in neonates born to mothers treated with baclofen throughout pregnancy.
- Pediatric: Intrathecal: Children should be of sufficient body mass to accommodate the implantable pump for chronic infusion.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Other warnings/precautions:
- Abrupt withdrawal: [US Boxed Warning]: Abrupt withdrawal of intrathecal baclofen, regardless of the cause, has resulted in sequelae (hyperpyrexia, altered mental status, exaggerated rebound spasticity, and muscle rigidity, which, in rare cases, has advanced to rhabdomyolysis), multiple organ-system failure, and death. Prevention of abrupt discontinuation requires careful attention to programming and monitoring of infusion system, refill scheduling and procedures, and pump alarms. Advise patients and caregivers of the importance of keeping scheduled refill visits and educate them on the early symptoms of baclofen withdrawal. Give special attention to patients at apparent risk (eg, spinal cord injuries at T-6 or above, communication difficulties, history of withdrawal symptoms from oral or intrathecal baclofen). Consult the technical manual of the implantable infusion system for additional postimplant clinician and patient information. In most cases, symptoms of withdrawal (eg, return of baseline spasticity, hypotension, paresthesia, pruritus) appear within hours to a few days following interruption of therapy. Priapism may develop or recur if treatment with intrathecal baclofen is interrupted. Clinically, the advanced intrathecal baclofen withdrawal syndrome may resemble autonomic dysreflexia, infection (sepsis), malignant hyperthermia, neuroleptic-malignant syndrome, or other conditions associated with a hypermetabolic state or widespread rhabdomyolysis. Suggested treatment for intrathecal baclofen withdrawal is restoration of intrathecal baclofen at or near the same dosage as before therapy was interrupted. Abrupt withdrawal of oral therapy has been associated with altered mental status, exaggerated rebound spasticity, hallucinations, high fever, muscle rigidity, and seizures, rarely leading to rhabdomyolysis, multi-organ system failure, and death. Gradual dose reductions (over ~1 to 2 weeks) are recommended in the absence of severe adverse reactions.
- Appropriate use: Intrathecal: For use only in an FDA-approved implantable pump for intrathecal baclofen administration; health care providers should be experienced with chronic intrathecal infusion therapy and resuscitative equipment should be readily available. Ensure patient is infection-free and then evaluate patient's response to bolus intrathecal injection (screening phase) prior to implanting pump. Monitor closely during the initial phase of pump use and when adjusting the dosing rate and/or the concentration in the reservoir. Educate patients and caregivers on proper home care of the pump and insertion site. Use extreme caution when filling an implantable pump; pumps should only be refilled through the reservoir refill septum. Inadvertent injection into the subcutaneous tissue can occur if the reservoir refill septum is not properly accessed. Some pumps are equipped with a catheter access port that allows direct access to the intrathecal catheter; direct injection into this catheter access port or inadvertent injection into the subcutaneous tissue may cause a life-threatening overdose. Except in overdose related emergencies, intrathecal baclofen should be reduced slowly if discontinuation is necessary.
- Appropriate use: Oral: Efficacy of oral baclofen has not been established in patients with Parkinson disease or cerebral palsy; therefore, use is not recommended. Use caution in patients with a history of stroke; poor tolerability to baclofen without significant benefit has been observed. Not indicated for spasticity associated with rheumatic disorders. Use with caution when spasticity is utilized to sustain upright posture and balance in locomotion, or when spasticity is necessary to obtain increased function.
- Overdose: Intrathecal use: Monitor closely for signs and symptoms of overdose which may appear suddenly or insidiously, especially during the initial screening and dose-titration phase of treatment, and during reintroduction of therapy after a period of interruption. Signs/symptoms of overdose may include drowsiness, dizziness, somnolence, hypothermia, respiratory depression, seizures, rostral progression of hypotonia and loss of consciousness progressing to coma. If overdose is suspected, patient should be evaluated immediately in a hospital setting and the pump reservoir emptied.
Monitoring Parameters
Regular electroencephalogram (EEG) in patients with epilepsy (loss of seizure control has been reported).
Pregnancy
Pregnancy Considerations
Late-onset neonatal withdrawal may occur following in utero exposure. Feeding difficulties, high-pitched cry, hyperthermia, hypertonicity, loose stools, tremors, and seizures have been reported in newborns following maternal use of oral baclofen throughout pregnancy (Duncan 2013; Freeman 2016; Ratnayaka 2001). Use of intrathecal baclofen in pregnant females has been described (Dalton 2008; Hara 2018; Méndez-Lucena 2016; Tandon 2010). Maternal plasma concentrations following administration of intrathecal baclofen are significantly less than those with oral doses; exposure to the fetus is expected to be limited and adverse neonatal events have not been noted in available reports (Morton 2009).
Patient Education
What is this drug used for?
- It is used to relax muscles.
- It is used to treat spasms in patients with MS (multiple sclerosis) or spinal cord disease.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Trouble sleeping
- Loss of strength and energy
- Fatigue
- Nausea
- Headache
- Constipation
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Withdrawal like high fever, mental changes, increased spasm, or stiff muscles
- Severe dizziness
- Passing out
- Confusion
- Behavioral changes
- Seizures
- Vision changes
- Chest pain
- Muscle pain
- Muscle weakness
- Stiff muscles
- Burning or numbness feeling
- Trouble breathing
- Slow breathing
- Shallow breathing
- Unable to pass urine
- Change in amount of urine passed
- Blood in the urine
- Mood changes
- Sensing things that seem real but are not
- Abnormal movements
- Twitching
- Change in balance
- Trouble swallowing
- Trouble speaking
- Involuntary eye movements
- Abnormal heartbeat
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.