Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Tablet, Oral, as hydrochloride:
Regimex: 25 mg [DSC]
Generic: 25 mg, 50 mg
Pharmacology
Mechanism of Action
Benzphetamine is a sympathomimetic amine with pharmacologic properties similar to the amphetamines. The mechanism of action in reducing appetite appears to be secondary to CNS effects, including stimulation of the hypothalamus to release norepinephrine.
Use: Labeled Indications
Obesity (short-term): Management of exogenous obesity as a short-term adjunct (a few weeks) in a regimen of weight reduction based on caloric restriction in patients with an initial body mass index (BMI) of 30 kg/m2 or higher who have not responded to appropriate weight reducing regimen (diet and/or exercise) alone.
Contraindications
Hypersensitivity or idiosyncrasy to benzphetamine, other sympathomimetic amines, or any component of the formulation; advanced arteriosclerosis, symptomatic cardiovascular disease, moderate-to-severe hypertension; hyperthyroidism; glaucoma; agitated states, history of drug abuse; during or within 14 days following MAO inhibitor therapy, concurrent use with other CNS stimulants; women who are or may become pregnant
Dosage and Administration
Dosing: Adult
Obesity (short-term): Oral: Initial: 25 to 50 mg once daily; may increase to 25 to 50 mg 1 to 3 times daily based on response
Dosing: Geriatric
Refer to adult dosing; use with caution starting at the low end of the dosage range.
Dosing: Pediatric
Obesity (short-term): Children ≥12 years and Adolescents: Refer to adult dosing.
Administration
Administer midmorning or midafternoon (for single daily dose) based on patient’s eating habits; avoid late afternoon administration if possible.
Dietary Considerations
Most effective when combined with a low calorie diet and behavior modification counseling.
Storage
Store at 20°C to 25°C (68°F to 77°F).
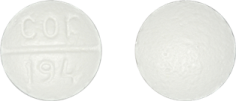
Benzphetamine Images
Drug Interactions
Acebrophylline: May enhance the stimulatory effect of CNS Stimulants. Avoid combination
Alkalinizing Agents: May decrease the excretion of Amphetamines. Management: Consider alternatives to using amphetamines and alkalinizing agents in combination. If these agents must be used together, patients should be monitored closely for excessive amphetamine effects. Consider therapy modification
Amifampridine: Agents With Seizure Threshold Lowering Potential may enhance the neuroexcitatory and/or seizure-potentiating effect of Amifampridine. Monitor therapy
Ammonium Chloride: May decrease the serum concentration of Amphetamines. This effect is likely due to an enhanced excretion of amphetamines in the urine. Monitor therapy
Antacids: May decrease the excretion of Amphetamines. Monitor therapy
Antihistamines: Amphetamines may diminish the sedative effect of Antihistamines. Monitor therapy
Antihypertensive Agents: Amphetamines may diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Antipsychotic Agents: May diminish the stimulatory effect of Amphetamines. Monitor therapy
Ascorbic Acid: May decrease the serum concentration of Amphetamines. Monitor therapy
AtoMOXetine: May enhance the hypertensive effect of Sympathomimetics. AtoMOXetine may enhance the tachycardic effect of Sympathomimetics. Monitor therapy
BuPROPion: May enhance the neuroexcitatory and/or seizure-potentiating effect of Agents With Seizure Threshold Lowering Potential. Monitor therapy
Cannabinoid-Containing Products: May enhance the tachycardic effect of Sympathomimetics. Exceptions: Cannabidiol. Monitor therapy
Carbonic Anhydrase Inhibitors: May decrease the excretion of Amphetamines. Exceptions: Brinzolamide; Dorzolamide. Monitor therapy
Cocaine (Topical): May enhance the hypertensive effect of Sympathomimetics. Management: Consider alternatives to use of this combination when possible. Monitor closely for substantially increased blood pressure or heart rate and for any evidence of myocardial ischemia with concurrent use. Consider therapy modification
CYP2D6 Inhibitors (Moderate): May increase the serum concentration of Amphetamines. Monitor therapy
CYP2D6 Inhibitors (Strong): May increase the serum concentration of Amphetamines. Exceptions: FLUoxetine; PARoxetine. Monitor therapy
Doxofylline: Sympathomimetics may enhance the adverse/toxic effect of Doxofylline. Monitor therapy
Esketamine: May enhance the hypertensive effect of CNS Stimulants. Monitor therapy
Ethosuximide: Amphetamines may diminish the therapeutic effect of Ethosuximide. Amphetamines may decrease the serum concentration of Ethosuximide. Monitor therapy
Gastrointestinal Acidifying Agents: May decrease the serum concentration of Amphetamines. Monitor therapy
Guanethidine: May enhance the arrhythmogenic effect of Sympathomimetics. Guanethidine may enhance the hypertensive effect of Sympathomimetics. Monitor therapy
Iobenguane Radiopharmaceutical Products: Amphetamines may diminish the therapeutic effect of Iobenguane Radiopharmaceutical Products. Management: Discontinue all drugs that may inhibit or interfere with catecholamine transport or uptake for at least 5 biological half-lives before iobenguane administration. Do not administer these drugs until at least 7 days after each iobenguane dose. Avoid combination
Iobenguane Radiopharmaceutical Products: CNS Stimulants may diminish the therapeutic effect of Iobenguane Radiopharmaceutical Products. Management: Discontinue all drugs that may inhibit or interfere with catecholamine transport or uptake for at least 5 biological half-lives before iobenguane administration. Do not administer these drugs until at least 7 days after each iobenguane dose. Avoid combination
Ioflupane I 123: Amphetamines may diminish the diagnostic effect of Ioflupane I 123. Monitor therapy
Iohexol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iohexol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iohexol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Iomeprol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iomeprol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iomeprol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Iopamidol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iopamidol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iopamidol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Methenamine: May decrease the serum concentration of Amphetamines. This effect is likely due to an enhanced excretion of amphetamines in the urine. Monitor therapy
Monoamine Oxidase Inhibitors: May enhance the hypertensive effect of Amphetamines. While linezolid and tedizolid may interact via this mechanism, management recommendations differ from other monoamine oxidase inhibitors. Refer to monographs specific to those agents for details. Avoid combination
Multivitamins/Fluoride (with ADE): May decrease the serum concentration of Amphetamines. More specifically, the ascorbic acid (vitamin C) in many multivitamins may decrease amphetamine concentrations. Monitor therapy
Multivitamins/Minerals (with ADEK, Folate, Iron): May decrease the serum concentration of Amphetamines. Monitor therapy
Multivitamins/Minerals (with AE, No Iron): May decrease the serum concentration of Amphetamines. Specifically, vitamin C may impair absorption of amphetamines. Monitor therapy
Opioid Agonists: Amphetamines may enhance the analgesic effect of Opioid Agonists. Monitor therapy
PHENobarbital: Amphetamines may decrease the serum concentration of PHENobarbital. Monitor therapy
Phenytoin: Amphetamines may decrease the serum concentration of Phenytoin. Monitor therapy
Quinolones: Amphetamines may enhance the cardiotoxic effect of Quinolones. Monitor therapy
Selective Serotonin Reuptake Inhibitors (Strong CYP2D6 Inhibitors): Amphetamines may enhance the serotonergic effect of Selective Serotonin Reuptake Inhibitors (Strong CYP2D6 Inhibitors). This could result in serotonin syndrome. Selective Serotonin Reuptake Inhibitors (Strong CYP2D6 Inhibitors) may increase the serum concentration of Amphetamines. Management: Monitor for increased amphetamine toxicities, including signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability) when these agents are combined. Monitor therapy
Serotonergic Agents (High Risk): Amphetamines may enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Exceptions: Amitriptyline; Amoxapine; ClomiPRAMINE; Desipramine; Dothiepin; Doxepin (Systemic); Doxepin (Topical); FLUoxetine; Imipramine; Isocarboxazid; Linezolid; Lofepramine; Melitracen [INT]; Methylene Blue; Moclobemide; Nortriptyline; PARoxetine; Phenelzine; Protriptyline; Tranylcypromine; Trimipramine. Monitor therapy
Sibutramine: May enhance the adverse/toxic effect of Centrally Acting Weight Loss Agents. Avoid combination
Solriamfetol: Sympathomimetics may enhance the hypertensive effect of Solriamfetol. Monitor therapy
Solriamfetol: CNS Stimulants may enhance the hypertensive effect of Solriamfetol. Monitor therapy
Sympathomimetics: May enhance the adverse/toxic effect of other Sympathomimetics. Monitor therapy
Tedizolid: May enhance the hypertensive effect of Sympathomimetics. Tedizolid may enhance the tachycardic effect of Sympathomimetics. Monitor therapy
Tricyclic Antidepressants: May enhance the adverse/toxic effect of Amphetamines. Tricyclic Antidepressants may potentiate the cardiovascular effects of Amphetamines. Amphetamines may enhance the serotonergic effect of Tricyclic Antidepressants. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) and increased cardiovascular effects when these agents are combined. Monitor therapy
Urinary Acidifying Agents: May decrease the serum concentration of Amphetamines. Monitor therapy
Adverse Reactions
Frequency not defined.
Cardiovascular: Cardiomyopathy (with chronic amphetamine use), hypertension, ischemic heart disease (with chronic amphetamine use), palpitations, tachycardia
Central nervous system: Depression (with withdrawal), dizziness, headache, insomnia, overstimulation, psychosis (rare), restlessness
Dermatologic: Dermatological reaction, diaphoresis, urticaria
Endocrine & metabolic: Change in libido
Gastrointestinal: Diarrhea, dysgeusia, nausea, xerostomia
Neuromuscular & skeletal: Tremor
Warnings/Precautions
Concerns related to adverse effects:
- CNS depression: May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks that require mental alertness (eg, operating machinery or driving).
- Psychological effects: Psychological disturbances have been reported in patients receiving anorectic agents together with a restrictive dietary regimen.
- Pulmonary hypertension: May occur (rarely) and may be fatal. Use of an anorectic agent for >3 months increases the risk of pulmonary hypertension. If onset or aggravation of exertional dyspnea, or unexplained symptoms of angina pectoris, syncope, or lower extremity edema occur, immediately discontinue and evaluate for the possible presence of pulmonary hypertension.
- Heart failure: In a scientific statement from the American Heart Association, benzphetamine has been determined to be an agent that may cause direct myocardial toxicity (magnitude: major) (AHA [Page 2016]).
- Valvular heart disease: The use of some anorectic agents has been associated with the development of valvular heart disease; contributing factors include use for extended periods of time, higher than recommended dose, and/or use in combination with other anorectic drugs. Not recommended in patients with known heart murmur or valvular heart disease.
Disease-related concerns:
- Cardiovascular disease: Use is not recommended in patients with symptomatic cardiovascular disease, including arrhythmias. Use with caution in patients with mild hypertension; use is contraindicated in moderate to severe hypertension.
- Diabetes: Use with caution in patients with diabetes mellitus; antidiabetic agent requirements may be altered with anorexic agents and concomitant dietary restrictions.
- Seizure disorders: Use with caution in patients with a history of seizure disorders.
- Tourette syndrome: Use with caution in patients with Tourette's syndrome; stimulants may unmask tics.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Elderly: Use caution in this age group due to risk for causing dependence, hypertension, angina, and myocardial infarction.
Other warnings/precautions:
- Abuse potential: Benzphetamine is pharmacologically related to the amphetamines, which have a high abuse potential; prolonged use may lead to dependency. Prescriptions should be written for the smallest quantity consistent with good patient care to minimize possibility of overdose.
- Appropriate use: Benzphetamine is not recommended for patients who used any anorectic agents within the prior year.
- Discontinuation of therapy: Abrupt discontinuation following prolonged high doses may be associated with extreme fatigue and depression; discontinue if satisfactory weight loss (≥4 pounds) has not occurred within the first 4 weeks of treatment.
- Tolerance: Tolerance to the anorectic effect usually develops within a few weeks; discontinue use if tolerance develops; do not exceed recommended dosage in an attempt to overcome tolerance.
Monitoring Parameters
Baseline cardiac evaluation (for preexisting valvular heart disease, pulmonary hypertension); echocardiogram during therapy (as needed to detect valvular heart disease); weight, waist circumference; blood pressure
Pregnancy
Pregnancy Risk Factor
X
Pregnancy Considerations
Use is contraindicated in women who are or may become pregnant (lack of potential benefit and possible fetal harm). An increased risk of adverse maternal and fetal outcomes is associated with obesity; however, medications for weight loss therapy are not recommended at conception or during pregnancy (ACOG 156 2015).
Patient Education
- Discuss specific use of drug and side effects with patient as it relates to treatment. (HCAHPS: During this hospital stay, were you given any medicine that you had not taken before? Before giving you any new medicine, how often did hospital staff tell you what the medicine was for? How often did hospital staff describe possible side effects in a way you could understand?)
- Patient may experience dry mouth, trouble sleeping, restlessness, diarrhea, nausea, tremors, sweating a lot, or bad taste. Have patient report immediately to prescriber chest pain, fast heartbeat, abnormal heartbeat, severe dizziness, passing out, vision changes, severe anxiety, severe headache, decreased sex drive, shortness of breath, or swelling of arms or legs (HCAHPS).
- Educate patient about signs of a significant reaction (eg, wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat). Note: This is not a comprehensive list of all side effects. Patient should consult prescriber for additional questions.
Intended Use and Disclaimer: Should not be printed and given to patients. This information is intended to serve as a concise initial reference for health care professionals to use when discussing medications with a patient. You must ultimately rely on your own discretion, experience, and judgment in diagnosing, treating, and advising patients.