Boxed Warning
Pregnancy:
Bexarotene capsules are a member of the retinoid class of drugs that is associated with birth defects in humans. Bexarotene capsules also caused birth defects when administered orally to pregnant rats. Bexarotene capsules must not be administered to a pregnant woman.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Capsule, Oral:
Targretin: 75 mg
Generic: 75 mg
Pharmacology
Mechanism of Action
Selectively binds to and activates retinoid X receptors (RXRs). Once activated, RXRs function as transcription factors to regulate the expression of genes which control cellular differentiation and proliferation. Bexarotene inhibits the growth in vitro of some tumor cell lines of hematopoietic and squamous cell origin and induces tumor regression in vivo in some animal models.
Pharmacokinetics/Pharmacodynamics
Absorption
Improved 48% by a fat-containing meal
Metabolism
Hepatic via CYP3A4 isoenzyme to four metabolites; further metabolized by glucuronidation
Excretion
Feces (primarily); urine (minimal, <1%)
Time to Peak
~2 hours
Half-Life Elimination
~7 hours
Protein Binding
>99% to plasma proteins
Use: Labeled Indications
Cutaneous T-cell lymphoma, refractory: Treatment of cutaneous manifestations of cutaneous T-cell lymphoma in patients who are refractory to at least one prior systemic therapy
Contraindications
Known hypersensitivity to bexarotene or any component of the formulation; pregnancy
Documentation of allergenic cross-reactivity for retinoids is limited. However, because of similarities in chemical structure and/or pharmacologic actions, the possibility of cross-sensitivity cannot be ruled out with certainty.
Dosage and Administration
Dosing: Adult
Cutaneous T-cell lymphoma, refractory: Oral: Initial: 300 mg/m2 once daily taken as a single daily dose; if well tolerated, but no tumor response after 8 weeks, may increase to 400 mg/m2 once daily; continue as long as clinical benefit is demonstrated (bexarotene was administered in studies for up to 97 weeks).
Mycosis fungoides/Sezary syndrome, refractory/resistant (off-label dose): Oral: 75 to 150 mg daily in combination with PUVA; maximum dose: 300 mg daily (Rupoli, 2010; Singh, 2004)
Dosing: Geriatric
Refer to adult dosing.
Dosing: Adjustment for Toxicity
If necessitated by toxicity, may decrease dose from 300 mg/m2/day to 200 mg/m2/day, then to 100 mg/m2/day, or temporarily hold. Upon recovery, may titrate dose upward with careful monitoring.
Hepatotoxicity: If AST, ALT, or bilirubin >3 times ULN, consider withholding or discontinuing therapy.
Hypertriglyceridemia: Consider dose reduction, treatment interruption, and or antilipemic therapy.
Leukopenia and neutropenia: Leukopenia and neutropenia resolved after dose reduction or discontinuation.
Dosing: Obesity
ASCO Guidelines for appropriate chemotherapy dosing in obese adults with cancer: Utilize patient’s actual body weight (full weight) for calculation of body surface area- or weight-based dosing, particularly when the intent of therapy is curative; manage regimen-related toxicities in the same manner as for nonobese patients; if a dose reduction is utilized due to toxicity, consider resumption of full weight-based dosing with subsequent cycles, especially if cause of toxicity (eg, hepatic or renal impairment) is resolved (Griggs, 2012).
Extemporaneously Prepared
A 1 mg/mL oral suspension may be prepared with capsules. Cut one 75 mg capsule in half, rinse the interior contents of the capsule, and suspend with 75 mL sterile water. Administer immediately after preparation. To ensure administration of full dose, rinse empty glass with half a glass of water and administer residue.
Targretin data on file, Eisai Inc.
Administration
Administer with a meal.
Storage
Store at 2°C to 25°C (36°F to 77°F). Protect from light. Avoid humidity and high temperatures after opening bottle.
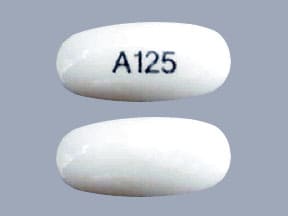
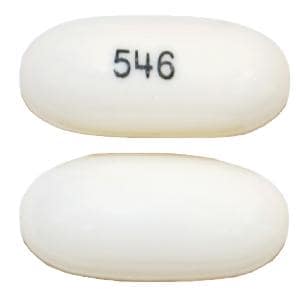
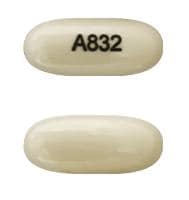
Bexarotene (Systemic) Images
Drug Interactions
Abemaciclib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Abemaciclib. Avoid combination
Aminolevulinic Acid (Systemic): Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Systemic). Avoid combination
Aminolevulinic Acid (Topical): Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Topical). Monitor therapy
Antihepaciviral Combination Products: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Antihepaciviral Combination Products. Avoid combination
Asunaprevir: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Asunaprevir. Avoid combination
AtorvaSTATin: Bexarotene (Systemic) may decrease the serum concentration of AtorvaSTATin. Monitor therapy
Avapritinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Avapritinib. Avoid combination
Axitinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Axitinib. Avoid combination
BCG (Intravesical): Myelosuppressive Agents may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
Bedaquiline: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Bedaquiline. Avoid combination
Benzhydrocodone: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Benzhydrocodone. Specifically, the serum concentrations of hydrocodone may be reduced. Monitor therapy
Bosutinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Bosutinib. Avoid combination
Brigatinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Brigatinib. Management: Avoid concurrent use of brigatinib with moderate CYP3A4 inducers when possible. If combined, increase the daily dose of brigatinib in 30 mg increments after 7 days of treatment with the current brigatinib dose, up to maximum of twice the dose. Consider therapy modification
CARBOplatin: May increase the serum concentration of Bexarotene (Systemic). Monitor therapy
Chloramphenicol (Ophthalmic): May enhance the adverse/toxic effect of Myelosuppressive Agents. Monitor therapy
Cladribine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Avoid combination
Clarithromycin: CYP3A4 Inducers (Moderate) may increase serum concentrations of the active metabolite(s) of Clarithromycin. CYP3A4 Inducers (Moderate) may decrease the serum concentration of Clarithromycin. Management: Consider alternative antimicrobial therapy for patients receiving a CYP3A inducer. Drugs that enhance the metabolism of clarithromycin into 14-hydroxyclarithromycin may alter the clinical activity of clarithromycin and impair its efficacy. Consider therapy modification
CloZAPine: Myelosuppressive Agents may enhance the adverse/toxic effect of CloZAPine. Specifically, the risk for neutropenia may be increased. Monitor therapy
CloZAPine: CYP3A4 Inducers (Moderate) may decrease the serum concentration of CloZAPine. Monitor therapy
Cobimetinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Cobimetinib. Avoid combination
Codeine: CYP3A4 Inducers (Moderate) may decrease serum concentrations of the active metabolite(s) of Codeine. Monitor therapy
CYP3A4 Substrates (High risk with Inducers): CYP3A4 Inducers (Moderate) may decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Exceptions: Apixaban; Rivaroxaban. Monitor therapy
Daclatasvir: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Daclatasvir. Management: Increase the daclatasvir dose to 90 mg once daily if used with a moderate CYP3A4 inducer. Consider therapy modification
Dasabuvir: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Dasabuvir. Avoid combination
Deferiprone: Myelosuppressive Agents may enhance the neutropenic effect of Deferiprone. Management: Avoid the concomitant use of deferiprone and myelosuppressive agents whenever possible. If this combination cannot be avoided, monitor the absolute neutrophil count more closely. Consider therapy modification
Deflazacort: CYP3A4 Inducers (Moderate) may decrease serum concentrations of the active metabolite(s) of Deflazacort. Avoid combination
Dipyrone: May enhance the adverse/toxic effect of Myelosuppressive Agents. Specifically, the risk for agranulocytosis and pancytopenia may be increased Avoid combination
Doravirine: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Doravirine. Monitor therapy
Elbasvir: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Elbasvir. Avoid combination
Elexacaftor, Tezacaftor, and Ivacaftor: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Elexacaftor, Tezacaftor, and Ivacaftor. Monitor therapy
Encorafenib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Encorafenib. Avoid combination
Entrectinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Entrectinib. Avoid combination
Erdafitinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Erdafitinib. Management: Dose modifications of erdafitinib may be required. See full monograph for details. Consider therapy modification
Estriol (Systemic): CYP3A4 Inducers (Moderate) may decrease the serum concentration of Estriol (Systemic). Monitor therapy
Estriol (Topical): CYP3A4 Inducers (Moderate) may decrease the serum concentration of Estriol (Topical). Monitor therapy
Estrogen Derivatives (Contraceptive): Bexarotene (Systemic) may decrease the serum concentration of Estrogen Derivatives (Contraceptive). Management: Women of childbearing potential receiving bexarotene should use two reliable forms of contraception (including at least one nonhormonal form). Consider therapy modification
Fedratinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Fedratinib. Avoid combination
FentaNYL: CYP3A4 Inducers (Moderate) may decrease the serum concentration of FentaNYL. Monitor therapy
Flibanserin: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Flibanserin. Avoid combination
Gemfibrozil: May increase the serum concentration of Bexarotene (Systemic). Avoid combination
Glecaprevir and Pibrentasvir: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Glecaprevir and Pibrentasvir. Monitor therapy
Grazoprevir: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Grazoprevir. Avoid combination
GuanFACINE: CYP3A4 Inducers (Moderate) may decrease the serum concentration of GuanFACINE. Management: Increase the guanfacine dose by up to double when initiating guanfacine in a patient taking a moderate CYP3A4 inducer. Increase guanfacine dose gradually over 1 to 2 weeks if initiating a moderate CYP3A4 inducer in a patient already taking guanfacine. Consider therapy modification
HYDROcodone: CYP3A4 Inducers (Moderate) may decrease the serum concentration of HYDROcodone. Monitor therapy
Ibrutinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Ibrutinib. Monitor therapy
Ifosfamide: CYP3A4 Inducers (Moderate) may decrease serum concentrations of the active metabolite(s) of Ifosfamide. CYP3A4 Inducers (Moderate) may increase serum concentrations of the active metabolite(s) of Ifosfamide. Monitor therapy
Istradefylline: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Istradefylline. Monitor therapy
Ivacaftor: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Ivacaftor. Monitor therapy
Lefamulin: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Lefamulin. Management: Avoid concomitant use of lefamulin with moderate CYP3A4 inducers unless the benefits outweigh the risks. Consider therapy modification
Lefamulin (Intravenous): CYP3A4 Inducers (Moderate) may decrease the serum concentration of Lefamulin (Intravenous). Management: Avoid concomitant use of lefamulin (intravenous) with moderate CYP3A4 inducers unless the benefits outweigh the risks. Consider therapy modification
Lemborexant: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Lemborexant. Avoid combination
Lorlatinib: CYP3A4 Inducers (Moderate) may enhance the hepatotoxic effect of Lorlatinib. CYP3A4 Inducers (Moderate) may decrease the serum concentration of Lorlatinib. Management: Avoid use of lorlatinib with moderate CYP3A4 inducers. If such a combination must be used, monitor AST, ALT, and bilirubin within 48 hours of starting the combination and at least three times within the first week of combined use. Consider therapy modification
Lumacaftor and Ivacaftor: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Lumacaftor and Ivacaftor. Monitor therapy
Lumateperone: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Lumateperone. Avoid combination
Lurasidone: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Lurasidone. Management: Monitor for decreased lurasidone effects if combined with moderate CYP3A4 inducers and consider increasing the lurasidone dose if coadministered with a moderate CYP3A4 inducer for 7 or more days. Consider therapy modification
Meperidine: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Meperidine. Monitor therapy
Mesalamine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Monitor therapy
Mirodenafil: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Mirodenafil. Monitor therapy
Multivitamins/Fluoride (with ADE): May enhance the adverse/toxic effect of Retinoic Acid Derivatives. Avoid combination
Multivitamins/Minerals (with ADEK, Folate, Iron): May enhance the adverse/toxic effect of Retinoic Acid Derivatives. Avoid combination
Multivitamins/Minerals (with AE, No Iron): May enhance the adverse/toxic effect of Retinoic Acid Derivatives. Avoid combination
Naldemedine: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Naldemedine. Monitor therapy
Neratinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Neratinib. Avoid combination
NiMODipine: CYP3A4 Inducers (Moderate) may decrease the serum concentration of NiMODipine. Monitor therapy
Nisoldipine: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Nisoldipine. Avoid combination
Olaparib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Olaparib. Avoid combination
PACLitaxel (Conventional): May increase the serum concentration of Bexarotene (Systemic). Bexarotene (Systemic) may decrease the serum concentration of PACLitaxel (Conventional). Monitor therapy
Palbociclib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Palbociclib. Management: The US label does not provide specific recommendations concerning use with moderate CYP3A4 inducers, but the Canadian label recommends avoiding use of moderate CYP3A4 inducers. Consider therapy modification
Perampanel: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Perampanel. Management: Increase the perampanel starting dose to 4 mg/day when perampanel is used concurrently with moderate and strong CYP3A4 inducers. Consider therapy modification
Pexidartinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Pexidartinib. Monitor therapy
Pimavanserin: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Pimavanserin. Avoid combination
Pitolisant: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Pitolisant. Monitor therapy
Porfimer: Photosensitizing Agents may enhance the photosensitizing effect of Porfimer. Monitor therapy
Pretomanid: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Pretomanid. Avoid combination
Progestins (Contraceptive): Bexarotene (Systemic) may decrease the serum concentration of Progestins (Contraceptive). Management: Women of childbearing potential receiving bexarotene should use two reliable forms of contraception (including at least one nonhormonal form). Consider therapy modification
Promazine: May enhance the myelosuppressive effect of Myelosuppressive Agents. Monitor therapy
Ranolazine: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Ranolazine. Avoid combination
Rolapitant: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Rolapitant. Monitor therapy
Simeprevir: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Simeprevir. Avoid combination
Sonidegib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Sonidegib. Avoid combination
Tamoxifen: Bexarotene (Systemic) may decrease the serum concentration of Tamoxifen. Monitor therapy
Tazemetostat: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Tazemetostat. Avoid combination
Tetracyclines: May enhance the adverse/toxic effect of Retinoic Acid Derivatives. The development of pseudotumor cerebri is of particular concern. Avoid combination
Tezacaftor and Ivacaftor: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Tezacaftor and Ivacaftor. Monitor therapy
Ubrogepant: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Ubrogepant. Management: Use an initial ubrogepant dose of 100 mg and second dose (if needed) of 100 mg when used with a moderate CYP3A4 inducer. Consider therapy modification
Upadacitinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Upadacitinib. Monitor therapy
Velpatasvir: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Velpatasvir. Avoid combination
Venetoclax: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Venetoclax. Avoid combination
Verteporfin: Photosensitizing Agents may enhance the photosensitizing effect of Verteporfin. Monitor therapy
Vitamin A: May enhance the adverse/toxic effect of Retinoic Acid Derivatives. Avoid combination
Voxelotor: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Voxelotor. Management: Avoid concomitant use of voxelotor and moderate CYP3A4 inducers. If concomitant use is unavoidable, increase the voxelotor dose to 2,500 mg once daily. Consider therapy modification
Zanubrutinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Zanubrutinib. Avoid combination
Zolpidem: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Zolpidem. Monitor therapy
Test Interactions
Treatment with bexarotene may interfere with CA125 assay values in patients with ovarian cancer (per manufacturer's labeling).
Adverse Reactions
Frequency not always defined.
>10%:
Cardiovascular: Peripheral edema (11% to 13%)
Central nervous system: Headache (30% to 42%), chills (10% to 13%), insomnia (5% to 11%)
Dermatologic: Exfoliative dermatitis (10% to 28%), skin rash (17% to 23%), xeroderma (9% to 11%), alopecia (4% to 11%)
Endocrine & metabolic: Hyperlipidemia (79%), hypercholesterolemia (32% to 62%), hypothyroidism (29% to 53%), increased lactate dehydrogenase (7% to 13%)
Gastrointestinal: Diarrhea (7% to 42%), anorexia (2% to 23%), nausea (8% to 16%), vomiting (4% to 13%), abdominal pain (4% to 11%)
Hematologic & oncologic: Leukopenia (17% to 47%), anemia (6% to 25%), hypochromic anemia (4% to 13%)
Infection: Infection (13% to 23%; bacterial infection: 1% to 13%)
Neuromuscular & skeletal: Weakness (20% to 45%), back pain (2% to 11%)
Respiratory: Flu-like symptoms (4% to 13%)
Miscellaneous: Fever (5% to 17%)
1% to 10%:
Cardiovascular: Angina pectoris, cardiac failure (right), cerebrovascular accident, chest pain, hypertension, subdural hematoma, syncope, tachycardia
Central nervous system: Agitation, ataxia, confusion, depression, dizziness, hyperesthesia, myasthenia, neuropathy
Dermatologic: Acne vulgaris, allergic skin reaction, cellulitis, cheilitis, cutaneous nodule, maculopapular rash, skin photosensitivity, pustular rash, skin rash, sunburn, vesiculobullous dermatitis
Endocrine & metabolic: Albuminuria, hyperglycemia, weight gain, weight loss
Gastrointestinal: Colitis, constipation, dyspepsia, flatulence, gastroenteritis, gingivitis, increased serum amylase, melena, pancreatitis, xerostomia
Genitourinary: Dysuria, hematuria, mastalgia, urinary incontinence, urinary tract infection, urinary urgency
Hematologic & oncologic: Acquired blood coagulation disorder, eosinophilia, hemorrhage, hypoproteinemia, lymphocytosis, thrombocythemia, thrombocytopenia
Hepatic: Hepatic failure, increased serum ALT, increased serum AST, increased serum bilirubin
Infection: Candidiasis, sepsis
Neuromuscular & skeletal: Arthralgia, arthrosis, myalgia, ostealgia
Ophthalmic: Blepharitis, cataract (new and worsening), conjunctivitis, corneal lesion, keratitis, visual field defect, xerophthalmia
Otic: Otalgia, otitis externa
Renal: Increased serum creatinine, renal function abnormality
Respiratory: Bronchitis, cough, dyspnea, hemoptysis, hypoxia, pharyngitis, pleural effusion, pneumonia, pulmonary edema, rhinitis
Miscellaneous: Serous drainage
Warnings/Precautions
Concerns related to adverse effects:
- Hepatotoxicity: Dose-related elevations in ALT, AST, and bilirubin have been reported; cases of cholestasis and liver failure (fatal) have occurred. Monitor for liver function test abnormalities and temporarily withhold or discontinue if ALT, AST, or bilirubin are >3 times the upper limit of normal (ULN). Liver function test elevations resolved within 1 month in most patients following dose reduction or discontinuation.
- Hypothyroidism: Bexarotene rapidly suppresses thyroid-stimulating hormone (TSH) levels by directly inhibiting TSH secretion, and also affects thyroid hormone metabolism (Hamnvik, 2011). Reductions in total thyroxine (T4) and thyroid-stimulating hormone (TSH) are reversible. Hypothyroidism commonly occurs. Monitor thyroid functions tests, including free T4 levels at baseline and during treatment. Thyroid supplementation is usually required; patients already receiving thyroid hormone therapy may require increased thyroid hormone doses to achieve therapeutic levels (Hamnvik, 2011).
- Leukopenia: Grade 1 to 3 leukopenia has occurred (predominantly as neutropenia); the incidence is higher with doses >300 mg/m2/day. The onset of leukopenia was generally 4 to 8 weeks. Grade 3 and 4 neutropenia have occurred. Leukopenia and neutropenia typically resolved within 30 days after discontinuation or dose reduction. Monitor complete blood cell count (CBC) with differential at baseline and periodically during treatment. Leukopenia and neutropenia were rarely associated with severe conditions or serious adverse events.
- Lipid abnormalities: Bexarotene induces significant lipid abnormalities in a majority of patients (increased triglycerides and total cholesterol, and decreased high-density lipoprotein [HDL]) and usually occur within 2 to 4 weeks; effects are reversible on discontinuation or generally mitigated by dose reduction and/or antilipemic therapy. Monitor fasting lipid panel; may require dose reduction, treatment interruption, and/or concomitant antilipemic therapy. Fasting triglycerides should be normal (or normalized with appropriate therapy) prior to initiation; triglycerides should be maintained <400 mg/dL. In studies, HMG-CoA reductase inhibitors were used to manage lipids; gemfibrozil is not recommended due to potential for drug interactions.
- Pancreatitis: Pancreatitis associated with hypertriglyceridemia has been reported. Interrupt treatment and evaluate if pancreatitis is suspected. Cutaneous T-cell lymphoma patients with risk factors for pancreatitis (eg, prior pancreatitis, uncontrolled hyperlipidemia, excessive ethanol consumption, uncontrolled diabetes, biliary tract disease, concomitant medications causing hyperlipidemia or concomitant medications associated with pancreatic toxicity) may be at increased risk for bexarotene-associated pancreatitis.
- Photosensitivity: Retinoids are associated with photosensitivity; phototoxicity (sunburn, sunlight sensitivity) has occurred with bexarotene when patients were exposed to direct sunlight. Advise patients to minimize exposure to sunlight and artificial ultraviolet light during treatment.
- Visual disturbances: Any new visual abnormalities experienced by the patient should be evaluated by an ophthalmologist (cataracts may develop or worsen, especially in the geriatric population).
Disease-related concerns:
- Diabetes: Use with caution in patients with diabetes mellitus; may enhance the actions of insulin, sulfonylureas, or thiazolidinediones, resulting in hypoglycemia in patients receiving these agents (hypoglycemia has not been observed with bexarotene monotherapy). Monitor blood glucose as necessary.
- Hepatic impairment: Use with extreme caution in patients with hepatic impairment; bexarotene undergoes extensive hepatic elimination.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
- Vitamin A: Due to the potential for additive toxicities, patients should be advised to limit additional vitamin A intake (in studies, additional vitamin A was limited to ≤15,000 units/day).
Special populations:
- Pregnancy: [U.S. Boxed Warning]: Bexarotene is a retinoid, a drug class associated with birth defects in humans; do not administer during pregnancy. Bexarotene caused birth defects when administered orally to pregnant rats. Pregnancy test needed within 1 week before initiation and every month thereafter. Effective contraception must be in place 1 month before initiation, during therapy, and for at least 1 month after discontinuation. Male patients with sexual partners who are pregnant, possibly pregnant, or who could become pregnant, must use condoms during sexual intercourse during treatment and for at least 1 month after last dose.
Monitoring Parameters
If female, pregnancy test within 1 week before initiation then monthly while on bexarotene; fasting lipid panel (before initiation, then weekly until lipid response established [usually 2 to 4 weeks] and then at 8-week intervals thereafter); liver function tests (baseline, then at 1, 2, and 4 weeks after initiation, then at 8-week intervals thereafter if stable); monitor thyroid function tests (including free T4) at baseline and weekly for the first 5 to 7 weeks, then every 1 to 2 months (Hamnvik, 2011); CBC with differential (baseline and periodic); blood glucose (in diabetic patients); ophthalmic exam (if visual abnormalities occur)
Pregnancy
Pregnancy Considerations
Bexarotene use is contraindicated in pregnancy. [US Boxed Warning]: Bexarotene is a member of the retinoid class of drugs that is associated with birth defects in humans. Bexarotene also caused birth defects when administered orally to pregnant rats. Bexarotene must not be administered to a pregnant woman. If a woman becomes pregnant while taking the drug, it must be stopped immediately and appropriate counseling be given.
Evaluate pregnancy status prior to use in females of reproductive potential. Effective contraception should be used for 1 month prior to initiating treatment, during therapy, and for at least 1 month after bexarotene is discontinued. Either abstinence or two forms of reliable contraception (one should be nonhormonal) are recommended. A negative pregnancy test (sensitivity of at least 50 mIU/mL) within 1 week prior to beginning therapy, and monthly, thereafter, is required for women of childbearing potential. A maximum 1-month supply is recommended so that pregnancy tests may be evaluated.
Male patients must use a condom during sexual intercourse with females who are pregnant, possibly pregnant, or who may become pregnant during therapy and for at least 1 month following discontinuation of bexarotene.
Patient Education
- Discuss specific use of drug and side effects with patient as it relates to treatment. (HCAHPS: During this hospital stay, were you given any medicine that you had not taken before? Before giving you any new medicine, how often did hospital staff tell you what the medicine was for? How often did hospital staff describe possible side effects in a way you could understand?)
- Patient may experience headache, trouble sleeping, lack of appetite, abdominal pain, nausea, vomiting, diarrhea, hair loss, dry skin, flu-like symptoms, or back pain. Have patient report immediately to prescriber signs of infection, signs of a low thyroid level (constipation; difficulty handling heat or cold; trouble with memory; mood changes; or burning, numbness, or tingling feeling), signs of pancreatitis (severe abdominal pain, severe back pain, severe nausea, or vomiting), signs of liver problems (dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin), vision changes, swelling of arms or legs, or severe loss of strength and energy (HCAHPS).
- Educate patient about signs of a significant reaction (eg, wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat). Note: This is not a comprehensive list of all side effects. Patient should consult prescriber for additional questions.
Intended Use and Disclaimer: Should not be printed and given to patients. This information is intended to serve as a concise initial reference for health care professionals to use when discussing medications with a patient. You must ultimately rely on your own discretion, experience and judgment in diagnosing, treating, and advising patients.