Boxed Warning
Hepatotoxicity:
Acetaminophen has been associated with cases of acute liver failure, at times resulting in liver transplant and death. Most of the cases of liver injury are associated with the use of acetaminophen at doses that exceed 4,000 mg per day, and often involve more than one acetaminophen-containing product.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Capsule, Oral:
Generic: Butalbital 50 mg and acetaminophen 300 mg
Tablet, Oral:
Allzital: Butalbital 25 mg and acetaminophen 325 mg
Bupap: Butalbital 50 mg and acetaminophen 300 mg [contains fd&c red #40 aluminum lake, fd&c yellow #10 aluminum lake]
Marten-Tab: Butalbital 50 mg and acetaminophen 325 mg [DSC] [scored]
Generic: Butalbital 25 mg and acetaminophen 325 mg, Butalbital 50 mg and acetaminophen 300 mg, Butalbital 50 mg and acetaminophen 325 mg
Pharmacology
Mechanism of Action
Butalbital: Short- to intermediate-acting barbiturate; depresses the sensory cortex, decreases motor activity, alters cerebellar function, and produces drowsiness, sedation, hypnosis, and dose-dependent respiratory depression.
Acetaminophen: Although not fully elucidated, the analgesic effects are believed to be due to activation of descending serotonergic inhibitory pathways in the CNS. Interactions with other nociceptive systems may be involved as well (Smith 2009). Antipyresis is produced from inhibition of the hypothalamic heat-regulating center.
Pharmacokinetics/Pharmacodynamics
Absorption
Butalbital: Well absorbed
Excretion
Butalbital: Urine (59% to 88% as unchanged drug or metabolites)
Half-Life Elimination
Butalbital: ~35 hours
Protein Binding
Butalbital: 45%
Use: Labeled Indications
Tension or muscle contraction headache: Relief of the symptomatic complex of tension or muscle contraction headache
Contraindications
Hypersensitivity to butalbital, acetaminophen, or any component of the formulation; porphyria
Dosage and Administration
Dosing: Adult
Note: Limit butalbital use to ≤3 days per month to avoid medication overuse headache (Garza 2006); studies have found increased risk with use of ≥5 days per month (Da Silva 2014).
Tension or muscle contraction headache: Oral:
Butalbital 25 mg/acetaminophen 325 mg: 2 tablets every 4 hours as needed (maximum: 12 tablets [butalbital 300 mg/acetaminophen 3,900 mg] per 24 hours).
Butalbital 50 mg/acetaminophen 300 to 325 mg: 1 or 2 tablets every 4 hours as needed (maximum: 6 tablets [butalbital 300 mg/acetaminophen 1,950 mg] per 24 hours).
Discontinuation of therapy: For low butalbital doses or less frequent use, consider abrupt discontinuation of therapy or a gradual taper over 2 to 4 weeks. If use is frequent or at high doses or if a patient has developed chronic migraine, discontinuing the butalbital-containing product and replacing with a gradual (eg, over 2 to 4 weeks) phenobarbital taper is advised to avoid withdrawal symptoms (ie, worsened headache, nausea/vomiting, restlessness, anxiety, diaphoresis, disturbed sleep, seizures). Consider providing bridge therapy with a medication to treat acute headaches and optimizing a preventative regimen to avoid rebound headache (Boes 2006; Garza 2019).
Dosing: Geriatric
Avoid use (Beers Criteria [AGS 2019]).
Dosing: Pediatric
Note: Based on experience in adult patients, limit use to ≤3 days per month to avoid medication overuse headache (Garza 2006). Multiple product formulations available; use precaution with product selection. All sources of acetaminophen (eg, prescription, OTC, combination products) should be considered when evaluating a patient's maximum daily dose. To lower the risk for hepatotoxicity, limit daily dose to ≤75 mg/kg/day (maximum of 5 daily doses), not to exceed 4,000 mg/day; while recommended doses are generally considered safe, hepatotoxicity has been reported (rarely) even with doses below recommendations (AAP [Sullivan 2011]; Heard 2014; Lavonas 2010).
Headache, tension or muscle contraction: Children ≥12 years and Adolescents:
Butalbital 25 mg/acetaminophen 325 mg: Oral: 2 tablets every 4 hours as needed; maximum daily dose: 12 tablets/24 hours (total: butalbital 300 mg/acetaminophen 3,900 mg per 24 hours)
Butalbital 50 mg/acetaminophen 300 or 325 mg: Oral: 1 or 2 tablets every 4 hours as needed; maximum daily dose: 6 tablets/24 hours (butalbital 300 mg/acetaminophen ≤1,950 mg per 24 hours)
Storage
Store at 20ºC to 25ºC (68ºF to 77ºF). Protect from light and moisture.
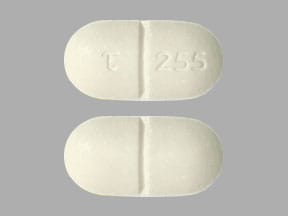
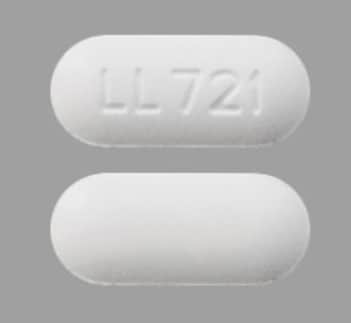
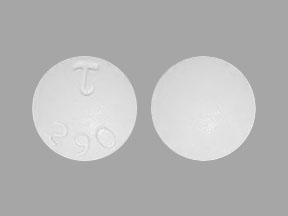
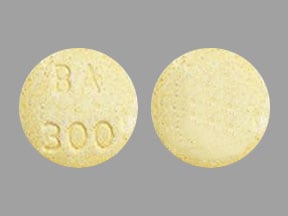
Butalbital and Acetaminophen Images
Drug Interactions
Alcohol (Ethyl): May enhance the hepatotoxic effect of Acetaminophen. Monitor therapy
Alizapride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Azelastine (Nasal): CNS Depressants may enhance the CNS depressant effect of Azelastine (Nasal). Avoid combination
Barbiturates: May increase the metabolism of Acetaminophen. This may 1) diminish the effect of acetaminophen; and 2) increase the risk of liver damage. Exceptions: Amobarbital; Butabarbital; Butalbital; Methohexital; PENTobarbital; Secobarbital; Thiopental. Monitor therapy
Beta-Blockers: Barbiturates may decrease the serum concentration of Beta-Blockers. Exceptions: Atenolol; Levobunolol; Metipranolol; Nadolol. Monitor therapy
Blonanserin: CNS Depressants may enhance the CNS depressant effect of Blonanserin. Consider therapy modification
Blood Pressure Lowering Agents: Barbiturates may enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Brexanolone: CNS Depressants may enhance the CNS depressant effect of Brexanolone. Monitor therapy
Brimonidine (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromopride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromperidol: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Buprenorphine: CNS Depressants may enhance the CNS depressant effect of Buprenorphine. Management: Consider reduced doses of other CNS depressants, and avoiding such drugs in patients at high risk of buprenorphine overuse/self-injection. Initiate buprenorphine at lower doses in patients already receiving CNS depressants. Consider therapy modification
Busulfan: Acetaminophen may increase the serum concentration of Busulfan. Monitor therapy
Calcium Channel Blockers: Barbiturates may increase the metabolism of Calcium Channel Blockers. Management: Monitor for decreased therapeutic effects of calcium channel blockers with concomitant barbiturate therapy. Calcium channel blocker dose adjustments may be necessary. Nimodipine Canadian labeling contraindicates concomitant use with phenobarbital. Exceptions: Clevidipine. Monitor therapy
Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Cannabis: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
CarBAMazepine: May increase the metabolism of Acetaminophen. This may 1) diminish the effect of acetaminophen; and 2) increase the risk of liver damage. Monitor therapy
Chloramphenicol (Systemic): May decrease the metabolism of Barbiturates. Barbiturates may increase the metabolism of Chloramphenicol (Systemic). Consider therapy modification
Chlormethiazole: May enhance the CNS depressant effect of CNS Depressants. Management: Monitor closely for evidence of excessive CNS depression. The chlormethiazole labeling states that an appropriately reduced dose should be used if such a combination must be used. Consider therapy modification
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
CNS Depressants: May enhance the adverse/toxic effect of other CNS Depressants. Monitor therapy
CycloSPORINE (Systemic): Barbiturates may increase the metabolism of CycloSPORINE (Systemic). Consider therapy modification
Dapsone (Topical): May enhance the adverse/toxic effect of Methemoglobinemia Associated Agents. Monitor therapy
Dasatinib: Acetaminophen may enhance the hepatotoxic effect of Dasatinib. Dasatinib may increase the serum concentration of Acetaminophen. Consider therapy modification
Dimethindene (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Doxycycline: Barbiturates may decrease the serum concentration of Doxycycline. Consider therapy modification
Doxylamine: May enhance the CNS depressant effect of CNS Depressants. Management: The manufacturer of Diclegis (doxylamine/pyridoxine), intended for use in pregnancy, specifically states that use with other CNS depressants is not recommended. Monitor therapy
Dronabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Droperidol: May enhance the CNS depressant effect of CNS Depressants. Management: Consider dose reductions of droperidol or of other CNS agents (eg, opioids, barbiturates) with concomitant use. Exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Consider therapy modification
Esketamine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Estrogen Derivatives (Contraceptive): Barbiturates may diminish the therapeutic effect of Estrogen Derivatives (Contraceptive). Contraceptive failure is possible. Management: Use of a non-hormonal contraceptive is recommended. Consider therapy modification
Felbamate: May increase the serum concentration of Barbiturates. Barbiturates may decrease the serum concentration of Felbamate. Management: Monitor for elevated barbiturate concentrations/toxicity if felbamate is initiated/dose increased, or reduced concentrations/effects if felbamate is discontinued/dose decreased. Refer to phenobarbital dosing guidelines for patients receiving that agent. Monitor therapy
Flucloxacillin: May enhance the adverse/toxic effect of Acetaminophen. Specifically, the risk for high anion gap metabolic acidosis may be increased. Monitor therapy
Flunitrazepam: CNS Depressants may enhance the CNS depressant effect of Flunitrazepam. Consider therapy modification
Fosphenytoin-Phenytoin: May decrease the serum concentration of Acetaminophen. Specifically, serum concentrations of acetaminophen may be decreased (leading to decreased efficacy), but the formation of the toxic N-acetyl-p-benzoquinone imine (NAPQI) metabolite may be increased (leading to increased hepatotoxicity). Monitor therapy
Griseofulvin: Barbiturates may decrease the serum concentration of Griseofulvin. Monitor therapy
Hemin: Barbiturates may diminish the therapeutic effect of Hemin. Avoid combination
HYDROcodone: CNS Depressants may enhance the CNS depressant effect of HYDROcodone. Management: Avoid concomitant use of hydrocodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
HydrOXYzine: May enhance the CNS depressant effect of Barbiturates. Management: Consider a decrease in the barbiturate dose, as appropriate, when used together with hydroxyzine. With concurrent use, monitor patients closely for excessive response to the combination. Consider therapy modification
Imatinib: Acetaminophen may enhance the hepatotoxic effect of Imatinib. Monitor therapy
Isoniazid: May enhance the adverse/toxic effect of Acetaminophen. Monitor therapy
Kava Kava: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
LamoTRIgine: Barbiturates may decrease the serum concentration of LamoTRIgine. Management: See lamotrigine prescribing information for specific age-dependent dosing guidelines regarding concurrent use with a barbiturate, as well as for adjusting lamotrigine dosing if concurrent barbiturate therapy is discontinued. Consider therapy modification
Lemborexant: May enhance the CNS depressant effect of CNS Depressants. Management: Dosage adjustments of lemborexant and of concomitant CNS depressants may be necessary when administered together because of potentially additive CNS depressant effects. Close monitoring for CNS depressant effects is necessary. Consider therapy modification
Local Anesthetics: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Local Anesthetics. Specifically, the risk for methemoglobinemia may be increased. Monitor therapy
Lofexidine: May enhance the CNS depressant effect of CNS Depressants. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Magnesium Sulfate: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Methotrimeprazine: CNS Depressants may enhance the CNS depressant effect of Methotrimeprazine. Methotrimeprazine may enhance the CNS depressant effect of CNS Depressants. Management: Reduce adult dose of CNS depressant agents by 50% with initiation of concomitant methotrimeprazine therapy. Further CNS depressant dosage adjustments should be initiated only after clinically effective methotrimeprazine dose is established. Consider therapy modification
Methoxyflurane: Barbiturates may enhance the nephrotoxic effect of Methoxyflurane. Barbiturates may increase the metabolism of Methoxyflurane. Avoid combination
MetyraPONE: May increase the serum concentration of Acetaminophen. More importantly, by inhibiting the conjugative metabolism of acetaminophen, metyrapone may shift the metabolism towards the oxidative route that produces a hepatotoxic metabolite. Monitor therapy
MetyroSINE: CNS Depressants may enhance the sedative effect of MetyroSINE. Monitor therapy
Mianserin: May enhance the CNS depressant effect of Barbiturates. Mianserin may diminish the therapeutic effect of Barbiturates. Barbiturates may decrease the serum concentration of Mianserin. Avoid combination
Minocycline (Systemic): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Mipomersen: Acetaminophen may enhance the hepatotoxic effect of Mipomersen. Monitor therapy
Multivitamins/Minerals (with ADEK, Folate, Iron): May decrease the serum concentration of Barbiturates. Monitor therapy
Nabilone: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Nitric Oxide: May enhance the adverse/toxic effect of Methemoglobinemia Associated Agents. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Monitor therapy
Opioid Agonists: CNS Depressants may enhance the CNS depressant effect of Opioid Agonists. Management: Avoid concomitant use of opioid agonists and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Orphenadrine: CNS Depressants may enhance the CNS depressant effect of Orphenadrine. Avoid combination
Oxomemazine: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
OxyCODONE: CNS Depressants may enhance the CNS depressant effect of OxyCODONE. Management: Avoid concomitant use of oxycodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Paraldehyde: CNS Depressants may enhance the CNS depressant effect of Paraldehyde. Avoid combination
Perampanel: May enhance the CNS depressant effect of CNS Depressants. Management: Patients taking perampanel with any other drug that has CNS depressant activities should avoid complex and high-risk activities, particularly those such as driving that require alertness and coordination, until they have experience using the combination. Consider therapy modification
Phenylephrine (Systemic): Acetaminophen may increase the serum concentration of Phenylephrine (Systemic). Monitor therapy
Piribedil: CNS Depressants may enhance the CNS depressant effect of Piribedil. Monitor therapy
Pramipexole: CNS Depressants may enhance the sedative effect of Pramipexole. Monitor therapy
Prilocaine: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Prilocaine. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Management: Monitor patients for signs of methemoglobinemia (e.g., hypoxia, cyanosis) when prilocaine is used in combination with other agents associated with development of methemoglobinemia. Avoid lidocaine/prilocaine in infants receiving such agents. Monitor therapy
Primidone: May enhance the adverse/toxic effect of Barbiturates. Primidone is converted to phenobarbital, and thus becomes additive with existing barbiturate therapy. Monitor therapy
Probenecid: May increase the serum concentration of Acetaminophen. Probenecid may also limit the formation of at least one major non-toxic metabolite, possibly increasing the potential for formation of the toxic NAPQI metabolite. Consider therapy modification
Progestins (Contraceptive): Barbiturates may diminish the therapeutic effect of Progestins (Contraceptive). Contraceptive failure is possible. Management: Use of alternative, nonhormonal contraceptives is recommended. Consider therapy modification
Propacetamol: Barbiturates may increase the metabolism of Propacetamol. This may 1) diminish the desired effects of propacetamol; and 2) increase the risk of liver damage. Monitor therapy
Pyridoxine: May increase the metabolism of Barbiturates. Apparent in high pyridoxine doses (eg, 200 mg/day) Monitor therapy
Rifamycin Derivatives: May increase the metabolism of Barbiturates. Monitor therapy
ROPINIRole: CNS Depressants may enhance the sedative effect of ROPINIRole. Monitor therapy
Rotigotine: CNS Depressants may enhance the sedative effect of Rotigotine. Monitor therapy
Rufinamide: May enhance the adverse/toxic effect of CNS Depressants. Specifically, sleepiness and dizziness may be enhanced. Monitor therapy
Selective Serotonin Reuptake Inhibitors: CNS Depressants may enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk of psychomotor impairment may be enhanced. Monitor therapy
Sodium Nitrite: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Sodium Nitrite. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Monitor therapy
Sodium Oxybate: May enhance the CNS depressant effect of CNS Depressants. Management: Consider alternatives to combined use. When combined use is needed, consider minimizing doses of one or more drugs. Use of sodium oxybate with alcohol or sedative hypnotics is contraindicated. Consider therapy modification
Somatostatin Acetate: May enhance the adverse/toxic effect of Barbiturates. Specifically, Somatostatin Acetate may enhance or prolong Barbiturate effects, including sedative effects. Avoid combination
SORAfenib: Acetaminophen may enhance the hepatotoxic effect of SORAfenib. SORAfenib may increase the serum concentration of Acetaminophen. Consider therapy modification
Suvorexant: CNS Depressants may enhance the CNS depressant effect of Suvorexant. Management: Dose reduction of suvorexant and/or any other CNS depressant may be necessary. Use of suvorexant with alcohol is not recommended, and the use of suvorexant with any other drug to treat insomnia is not recommended. Consider therapy modification
Tapentadol: May enhance the CNS depressant effect of CNS Depressants. Management: Avoid concomitant use of tapentadol and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Teniposide: Barbiturates may decrease the serum concentration of Teniposide. Management: Consider alternatives to combined treatment with barbiturates and teniposide due to the potential for decreased teniposide concentrations. If the combination cannot be avoided, monitor teniposide response closely. Consider therapy modification
Tetrahydrocannabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Thalidomide: CNS Depressants may enhance the CNS depressant effect of Thalidomide. Avoid combination
Theophylline Derivatives: Barbiturates may decrease the serum concentration of Theophylline Derivatives. Exceptions: Dyphylline. Monitor therapy
Tricyclic Antidepressants: Barbiturates may increase the metabolism of Tricyclic Antidepressants. Consider therapy modification
Trimeprazine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Ulipristal: Barbiturates may decrease the serum concentration of Ulipristal. Avoid combination
Valproate Products: May increase the serum concentration of Barbiturates. Barbiturates may decrease the serum concentration of Valproate Products. Monitor therapy
Vitamin K Antagonists (eg, warfarin): Barbiturates may increase the metabolism of Vitamin K Antagonists. Management: Monitor INR more closely. An anticoagulant dose increase may be needed after a barbiturate is initiated or given at an increased dose. Anticoagulant dose decreases may be needed following barbiturate discontinuation or dose reduction. Consider therapy modification
Voriconazole: Barbiturates may decrease the serum concentration of Voriconazole. Avoid combination
Zolpidem: CNS Depressants may enhance the CNS depressant effect of Zolpidem. Management: Reduce the Intermezzo brand sublingual zolpidem adult dose to 1.75 mg for men who are also receiving other CNS depressants. No such dose change is recommended for women. Avoid use with other CNS depressants at bedtime; avoid use with alcohol. Consider therapy modification
Test Interactions
Acetaminophen may produce false-positive tests for urinary 5-hydroxyindoleacetic acid.
Adverse Reactions
Frequency not defined.
Cardiovascular: Tachycardia
Central nervous system: Agitation, confusion, depression, dizziness, drowsiness, euphoria, excitement, headache, increased energy, intoxicated feeling, lethargy, numbness, paresthesia, sedation, seizure, shakiness
Dermatologic: Hyperhidrosis, pruritus
Endocrine & metabolic: Hot flash
Gastrointestinal: Abdominal pain, constipation, dysphagia, flatulence, heartburn, nausea, vomiting, xerostomia
Genitourinary: Diuresis
Hypersensitivity: Hypersensitivity reaction
Neuromuscular & skeletal: Leg pain, muscle fatigue
Otic: Otalgia, tinnitus
Respiratory: Dyspnea, nasal congestion
Miscellaneous: Fever, heavy eyelids
<1%, postmarketing, and/or case reports: Erythema multiforme, toxic epidermal necrolysis
Warnings/Precautions
Concerns related to adverse effects:
- CNS depression: May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks that require mental alertness (eg, operating machinery, driving).
- Hepatotoxicity: [US Boxed Warning]: Acetaminophen may cause severe hepatotoxicity, potentially requiring liver transplant or resulting in death; hepatotoxicity is usually associated with excessive acetaminophen intake (>4 g/day). Risk is increased with alcohol use, preexisting liver disease, and intake of more than one source of acetaminophen-containing medications. Chronic daily dosing in adults has also resulted in liver damage in some patients.
- Hypersensitivity/anaphylactic reactions: Hypersensitivity and anaphylactic reactions have been reported with acetaminophen use; discontinue immediately if symptoms of allergic or hypersensitivity reactions occur.
- Skin reactions: Rarely, acetaminophen may cause serious and potentially fatal skin reactions such as acute generalized exanthematous pustulosis, Stevens-Johnson syndrome, and toxic epidermal necrolysis. Discontinue treatment if severe skin reactions develop.
Disease-related concerns:
- Abdominal conditions: Use with caution in patients with acute abdominal conditions.
- Drug abuse: Use with caution in patients with a history of drug abuse or acute alcoholism; potential for drug dependency exists. Tolerance, psychological, and physical dependence may occur with prolonged use.
- Ethanol use: Use with caution in patients with alcoholic liver disease; consuming ≥3 alcoholic drinks per day may increase the risk of liver damage.
- G6PD deficiency: Use with caution in patients with known G6PD deficiency.
- Hepatic impairment: Use with caution in patients with severe hepatic impairment.
- Renal impairment: Use with caution in patients with severe renal impairment.
- Respiratory disease: Use with caution in patients with preexisting respiratory compromise (hypoxia and/or hypercapnia), chronic obstructive pulmonary disease, or other obstructive pulmonary disease, and kyphoscoliosis or other skeletal disorder which may alter respiratory function; critical respiratory depression may occur, even at therapeutic dosages.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Debilitated patients: Use with caution in debilitated patients; there is a greater potential for critical respiratory depression, even at therapeutic dosages.
- Elderly: Use with caution in the elderly.
Other warnings/precautions:
- Appropriate use: Limit butalbital use to ≤3 days per month to avoid medication overuse headache (Garza 2006); studies have found increased risk with use of ≥5 days per month (Da Silva 2014).
- Discontinuation of therapy: When discontinuing chronic or high-dose treatment with butalbital, or if a patient has developed chronic migraine on butalbital, discontinuing butalbital and replacing with a gradual phenobarbital taper is advised to avoid barbiturate withdrawal symptoms (ie, anxiety, diaphoresis, disturbed sleep, nausea/vomiting, restlessness, seizures, worsened headache). These patients will likely require bridge therapy with a medication to treat acute headaches and may benefit from an optimized preventative regimen (Boes 2006; Garza 2019).
- Dosage limit: Limit acetaminophen dose from all sources (prescription and OTC) to <4 g/day.
Pregnancy
Pregnancy Considerations
Butalbital crosses the placenta.
Withdrawal seizures were reported in an infant 2 days after birth following maternal use of a butalbital product during the last 2 months of pregnancy; butalbital was detected in the newborns serum (Ostrea 1982). Products containing butalbital are not recommended in pregnant females (Tepper 2014; Wells 2016). Also refer to acetaminophen monograph for information specific to acetaminophen.
Patient Education
- Discuss specific use of drug and side effects with patient as it relates to treatment. (HCAHPS: During this hospital stay, were you given any medicine that you had not taken before? Before giving you any new medicine, how often did hospital staff tell you what the medicine was for? How often did hospital staff describe possible side effects in a way you could understand?)
- Patient may experience intoxicated feeling, fatigue, dizziness, abdominal pain, vomiting, or nausea. Have patient report immediately to prescriber signs of liver problems (dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin), change in amount of urine passed, unable to pass urine, shortness of breath, or signs of Stevens-Johnson syndrome/toxic epidermal necrolysis (red, swollen, blistered, or peeling skin [with or without fever]; red or irritated eyes; or sores in mouth, throat, nose, or eyes) (HCAHPS).
- Educate patient about signs of a significant reaction (eg, wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat). Note: This is not a comprehensive list of all side effects. Patient should consult prescriber for additional questions.
Intended Use and Disclaimer: Should not be printed and given to patients. This information is intended to serve as a concise initial reference for health care professionals to use when discussing medications with a patient. You must ultimately rely on your own discretion, experience, and judgment in diagnosing, treating, and advising patients.