Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
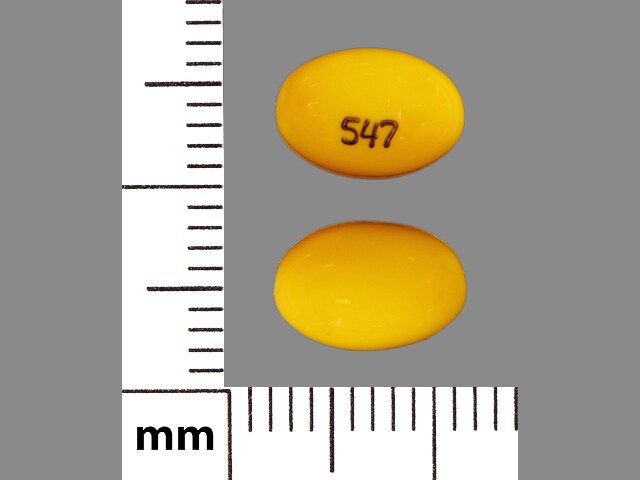
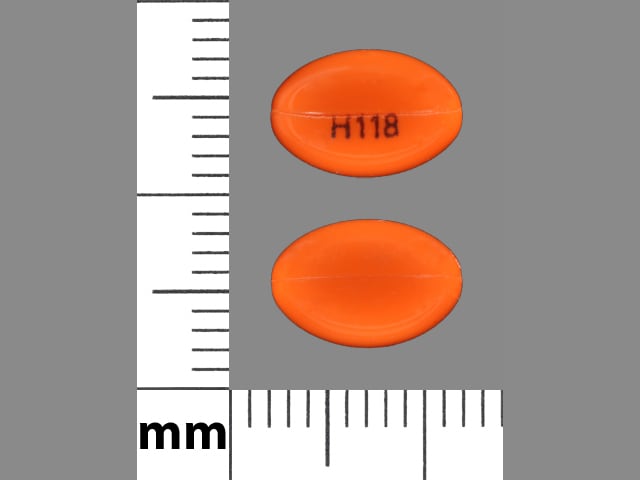
Capsule, Oral:
Rocaltrol: 0.25 mcg, 0.5 mcg [contains fd&c yellow #6 (sunset yellow), methylparaben, propylparaben]
Generic: 0.25 mcg, 0.5 mcg
Solution, Intravenous:
Generic: 1 mcg/mL (1 mL)
Solution, Oral:
Rocaltrol: 1 mcg/mL (15 mL)
Generic: 1 mcg/mL (15 mL)
Pharmacology
Mechanism of Action
Calcitriol, the active form of vitamin D (1,25 hydroxyvitamin D3), binds to and activates the vitamin D receptor in kidney, parathyroid gland, intestine, and bone, stimulating intestinal calcium transport and absorption. It reduces parathyroid hormone (PTH) levels and improves calcium and phosphate homeostasis by stimulating bone resorption of calcium and increasing renal tubular reabsorption of calcium. Decreased renal conversion of vitamin D to its primary active metabolite (1,25 hydroxyvitamin D) in chronic renal failure leads to reduced activation of vitamin D receptor, which subsequently removes inhibitory suppression of parathyroid hormone (PTH) release; increased serum PTH (secondary hyperparathyroidism) reduces calcium excretion and enhances bone resorption.
Pharmacokinetics/Pharmacodynamics
Absorption
Oral: Rapid
Metabolism
Primarily to calcitroic acid and a lactone metabolite
Excretion
Excretion: Feces (27%); urine (7%, unchanged in 24 hours)
Clearance: Children 1.8 to 16 years undergoing peritoneal dialysis: 15.3 mL/hour/kg
Onset of Action
Oral: 2 hours; maximum effect: 10 hours
Time to Peak
Serum: Oral: 3 to 6 hours; Hemodialysis: 8 to 12 hours
Duration of Action
Oral, IV: 3 to 5 days
Half-Life Elimination
Children 1.8 to 16 years undergoing peritoneal dialysis: 27.4 hours; Healthy adults: 5 to 8 hours; Hemodialysis: 16 to 22 hours
Protein Binding
99.9%
Use in Specific Populations
Special Populations: Renal Function Impairment
The half-life is increased by at least 2-fold.
Use: Labeled Indications
Hypoparathyroidism/pseudohypoparathyroidism: Management of hypocalcemia in patients with hypoparathyroidism or pseudohypoparathyroidism (oral)
Secondary hyperparathyroidism in patients with chronic kidney disease: Management of secondary hyperparathyroidism in patients with moderate to severe chronic kidney disease (CKD) not on dialysis (oral) or in patients on dialysis (oral or IV). Note: Although the manufacturer’s labeling states that calcitriol may be used specifically to treat hypocalcemia in dialysis patients, due to the risk of hypercalcemia, use should generally be reserved for patients with severe and progressive hyperparathyroidism (KDIGO 2017).
Use: Off Label
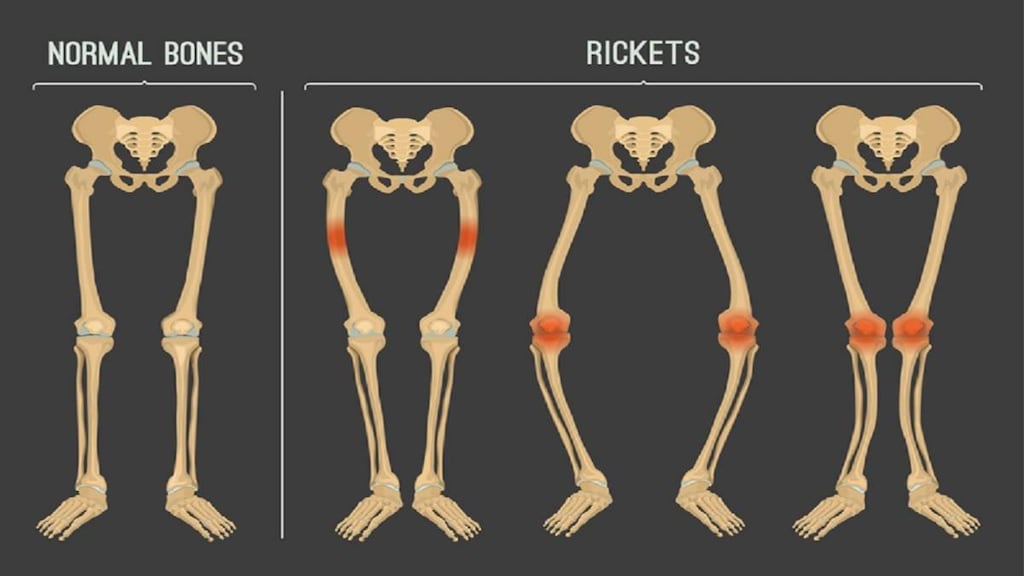
Hypophosphatemia, X-linked (ie, vitamin D-resistant rickets)c
Clinical experience suggests that calcitriol (in conjunction with phosphate replacement therapy) may be beneficial in select adult patients with X-linked hypophosphatemia (eg, those with spontaneous insufficiency fractures or disabling lower extremity skeletal pain, planned/pending orthopedic procedures, biochemical evidence of osteomalacia). Goals of therapy include reduction of pain, improvement of fracture healing, hasten recovery and reduce the risk of prosthetic loosening following joint replacement surgery, and/or reduce the extent of osteomalacia (ie, abundance of unmineralized osteoid present in the skeleton). In patients undergoing orthopedic procedures initiate therapy 3 to 6 months before the procedure. Discontinuation of therapy should be considered if clinical improvement is not observed within 9 to 12 months Carpenter 2011.
Vitamin D-dependent rickets type I/pseudovitamin D deficiency rickets (PDDR)c
Data from a retrospective chart review consisting of children, adolescents, and adults (ages 2 to 33 years) with a diagnosis of pseudovitamin D deficiency rickets (PDDR) treated with calcitriol suggests that calcitriol may be effective for the treatment of this condition Edouard 2011.
Contraindications
Hypersensitivity to calcitriol, other vitamin D analogues, or any component of the formulation; hypercalcemia, vitamin D toxicity
Dosage and Administration
Dosing: Adult
Hypocalcemia in hypoparathyroidism/pseudohypoparathyroidism: Oral: Initial: 0.25 mcg once daily (may adjust dose at 2- to 4-week intervals to achieve target calcium levels while avoiding hypercalcemia); range: 0.5 to 2 mcg/day.
Hypophosphatemia, X-linked (ie, vitamin D-resistant rickets) (off-label use): Oral: Initial: 0.5 to 0.75 mcg/day in 2 divided doses; after 4 to 6 weeks, assess biochemical response; dose may be adjusted upward or downward in increments of 0.25 mcg/day every 3 to 4 weeks to maintain normal serum parathyroid hormone (PTH) and calcium while avoiding hypercalciuria. Consider discontinuing therapy if clinical improvement is not observed within 9 to 12 months. Note: Calcitriol may be initiated ~1 week prior to initiating phosphate therapy to reduce the risk of exacerbating preexisting secondary hyperparathyroidism or causing it to develop (Carpenter 2011).
Secondary hyperparathyroidism in CKD: Note: KDIGO guidelines do not recommend routine use of calcitriol or other vitamin D analogs in patients with chronic kidney disease (CKD) stages G3 to G5; it may be reasonable to reserve use for patients with CKD stages G4 or G5 and with severe and progressive hyperparathyroidism. Caution is advised to avoid hypercalcemia or elevated phosphate levels (KDIGO 2017).
Patients on chronic renal dialysis:
Oral: Initial: 0.25 mcg once daily; may increase dose by 0.25 mcg/day at 4- to 8-week intervals, up to 0.5 to 1 mcg/day patients with normal or mildly decreased serum calcium levels may respond to 0.25 mcg every other day.
IV: Initiate carefully; may consider 0.5 mcg 3 times weekly approximately every other day or if necessary higher doses (eg, 1 to 2 mcg 3 times weekly approximately every other day). Adjust dose by 0.5 to 1 mcg at 2- to 4-week intervals; dosing range: 0.5 to 4 mcg 3 times weekly. Gradual dose reduction and discontinuation of therapy may be necessary as PTH levels decrease in response to therapy.
Patients with moderate to severe CKD not yet on dialysis: Oral: Initial: The magnitude of PTH response is highly variable (Shoben 2012). KDIGO guidelines recommend initiating with low doses independent of initial PTH concentration and then titrating based on PTH response while avoiding hypercalcemia (KDIGO 2017); the manufacturer recommends an initial dose of 0.25 mcg/day, although lower doses (eg, 0.25 mcg 3 to 4 times weekly) have also been used (Shoben 2012); may increase to 0.5 mcg/day if needed.
Vitamin D-dependent rickets type 1/pseudovitamin D deficiency rickets (PDDR) (off-label use): Oral: Initial: 0.5 mcg twice daily; subsequent dosing adjusted to maintain normal serum calcium and PTH levels; median dose after 2 years: 0.25 mcg daily (range: 0.1 to 0.5 mcg daily) (Edouard 2011)
Discontinuation of therapy for hypercalcemia: Discontinue therapy if hypercalcemia occurs; monitor calcium and phosphorous daily until levels normalize. Upon normalization, treatment with calcitriol can be resumed, at a reduced dose than that previously used. Assess dietary calcium intake and adjust if indicated.
Dosing: Geriatric
Refer to adult dosing. Start at the lower end of the dosage range.
Dosing: Pediatric
Hypocalcemia in patients with chronic kidney disease (CKD)/Metabolic bone disease: Limited data available: Indicated when serum levels of 25(OH)D are >30 ng/mL (75 nmol/L) and serum levels of intact parathyroid hormone (iPTH) are above the target range for the stage of CKD; serum levels of corrected total calcium are <9.5 to 10 mg/dL (2.37 mmol/L) and serum levels of phosphorus in children are less than age-appropriate upper limits of normal (K/DOQI Guidelines 2005):
Children and Adolescents:
CKD Stages 2 to 4: Oral:
<10 kg: 0.05 mcg every other day
10 to 20 kg: 0.1 to 0.15 mcg daily
>20 kg: 0.25 mcg daily
Dosage adjustment:
If iPTH decrease is <30% after 3 months of therapy and serum levels of calcium and phosphorus are within the target ranges based upon the CKD Stage, increase dosage by 50%.
If iPTH decrease < target range for CKD stage hold calcitriol therapy until iPTH increases to above target range; resume therapy at half the previous dosage (if dosage <0.25 mcg capsule or 0.05 mcg liquid, use every other day therapy).
If serum levels of total corrected calcium exceed 10.2 mg/dL (2.37 mmol/L) hold calcitriol therapy until serum calcium decreased to <9.8 mg/dL (2.37 mmol/L); resume therapy at half the previous dosage (if dosage <0.25 mcg capsule or 0.05 mcg liquid, use every other day therapy).
If serum levels of phosphorus increase to > age-appropriate upper limits, hold calcitriol therapy (initiate or increase phosphate binders until the levels of serum phosphorus decrease to age-appropriate limits); resume therapy at half the previous dosage.
CKD Stage 5 on dialysis: Oral, IV: Serum calcium times phosphorus product (Ca x P) should not exceed 65 mg2/dL2 for infants and children <12 years of age and 55 mg2/dL2 for adolescents, serum phosphorus should be within target, serum calcium <10 mg/dL (2.37 mmol/L) or <10.5 mg/dL (2.5 mmol/L) if iPTH >1,000 pg/mL: Note: If undergoing hemodialysis, doses should be given on dialysis days.
iPTH 300 to 500 pg/mL: 0.0075 mcg/kg 3 times weekly; maximum dose: 0.25 mcg/dose
iPTH >500 to 1,000 pg/mL: 0.015 mcg/kg 3 times weekly; maximum dose: 0.5 mcg/dose
iPTH >1,000 pg/mL: 0.025 mcg/kg 3 times weekly; maximum dose: 1 mcg/dose
Dosage adjustment: If iPTH decrease is <30% after 3 months of therapy and serum levels of calcium and phosphorus are within the target ranges based upon the CKD Stage 5, increase dosage by 50%
Note: Intermittent administration of calcitriol by IV or oral routes is more effective than daily oral calcitriol in lowering iPTH levels (KDIGO 2005).
Hypoparathyroidism/pseudohypoparathyroidism: Oral (evaluate dosage at 2- to 4-week intervals):
Infants: Limited data available: 0.02 to 0.06 mcg/kg once daily (Sperling 2014)
Children 1 to 5 years: Oral: 0.25 to 0.75 mcg once daily
Children ≥6 years and Adolescents: Oral: 0.5 to 2 mcg once daily
Secondary hyperparathyroidism associated with moderate to severe CKD in patients not yet on dialysis (predialysis): Note: KDIGO recommends against routine vitamin D supplement or analog use to suppress PTH concentrations in the absence of suspected or documented deficiency (KDIGO 2012).
Children <3 years: Oral: 0.01 to 0.015 mcg/kg/dose once daily
Children ≥3 years and Adolescents: Oral: 0.25 mcg once daily; may increase if necessary to 0.5 mcg/day
Vitamin D-dependent rickets: Infants, Children, and Adolescents: Oral: Initial: 0.25 to 2 mcg once daily; adjust dose base on clinical response, use lower dose once rickets has healed (Kliegman 2016)
Administration
IV: May be administered as a bolus dose IV through the catheter at the end of hemodialysis.
Oral: May be administered without regard to food. Administer with meals to reduce GI problems.
Dietary Considerations
May be taken without regard to food. Give with meals to reduce GI problems. Adequate calcium intake should be maintained during therapy; dietary phosphorous may need to be restricted.
Storage
Oral capsule, injection, solution: Store at room temperature of 15°C to 30°C (59°F to 86°F). Protect from light.
Calcitriol (Systemic) Images
Drug Interactions
Aluminum Hydroxide: Vitamin D Analogs may increase the serum concentration of Aluminum Hydroxide. Specifically, the absorption of aluminum may be increased, leading to increased serum aluminum concentrations. Avoid combination
Aprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Bile Acid Sequestrants: May decrease the serum concentration of Vitamin D Analogs. More specifically, bile acid sequestrants may impair absorption of Vitamin D Analogs. Management: Avoid concomitant administration of vitamin D analogs and bile acid sequestrants (eg, cholestyramine). Separate administration of these agents by several hours to minimize the potential risk of interaction. Monitor plasma calcium concentrations. Consider therapy modification
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Burosumab: Vitamin D Analogs may enhance the adverse/toxic effect of Burosumab. Avoid combination
Calcium Salts: May enhance the adverse/toxic effect of Vitamin D Analogs. Monitor therapy
Cardiac Glycosides: Vitamin D Analogs may enhance the arrhythmogenic effect of Cardiac Glycosides. Monitor therapy
Clofazimine: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Corticosteroids (Systemic): May diminish the therapeutic effect of Calcitriol (Systemic). Monitor therapy
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May increase the metabolism of CYP3A4 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
CYP3A4 Inhibitors (Moderate): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CYP3A4 Inhibitors (Strong): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Consider therapy modification
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Danazol: May enhance the hypercalcemic effect of Vitamin D Analogs. Monitor therapy
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Duvelisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: Serum Phosphate Level-Altering Agents may diminish the therapeutic effect of Erdafitinib. Management: Avoid coadministration of serum phosphate level-altering agents with erdafitinib before initial dose increase period based on serum phosphate levels (Days 14 to 21). Consider therapy modification
Fosaprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosnetupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Larotrectinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Magnesium Salts: Calcitriol (Systemic) may increase the serum concentration of Magnesium Salts. Management: Consider using a non-magnesium-containing antacid or phosphate-binding product in patients also receiving calcitriol. If magnesium-containing products must be used with calcitriol, serum magnesium concentrations should be monitored closely. Consider therapy modification
MiFEPRIStone: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Minimize doses of CYP3A4 substrates, and monitor for increased concentrations/toxicity, during and 2 weeks following treatment with mifepristone. Avoid cyclosporine, dihydroergotamine, ergotamine, fentanyl, pimozide, quinidine, sirolimus, and tacrolimus. Consider therapy modification
Mineral Oil: May decrease the serum concentration of Vitamin D Analogs. More specifically, mineral oil may interfere with the absorption of Vitamin D Analogs. Management: Avoid concomitant, oral administration of mineral oil and vitamin D analogs. Consider separating the administration of these agents by several hours to minimize the risk of interaction. Monitor plasma calcium concentrations. Consider therapy modification
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Multivitamins/Fluoride (with ADE): May enhance the adverse/toxic effect of Vitamin D Analogs. Avoid combination
Multivitamins/Minerals (with ADEK, Folate, Iron): May enhance the adverse/toxic effect of Vitamin D Analogs. Avoid combination
Netupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Orlistat: May decrease the serum concentration of Vitamin D Analogs. More specifically, orlistat may impair absorption of Vitamin D Analogs. Management: Monitor clinical response (including serum calcium) to oral vitamin D analogs closely if used with orlistat. If this combination must be used, consider giving the vitamin D analog at least 2 hrs before or after orlistat. Consider therapy modification
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Sevelamer: May decrease the serum concentration of Calcitriol (Systemic). Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
Sucralfate: Vitamin D Analogs may increase the serum concentration of Sucralfate. Specifically, the absorption of aluminum from sucralfate may be increased, leading to an increase in the serum aluminum concentration. Avoid combination
Thiazide and Thiazide-Like Diuretics: May enhance the hypercalcemic effect of Vitamin D Analogs. Monitor therapy
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Vitamin D Analogs: May enhance the adverse/toxic effect of other Vitamin D Analogs. Avoid combination
Adverse Reactions
>10%: Endocrine & metabolic: Hypercalcemia
1% to 10%:
Central nervous system: Headache
Dermatologic: Skin rash
Endocrine & metabolic: Polydipsia
Gastrointestinal: Abdominal pain, nausea
Genitourinary: Urinary tract infection
Frequency not defined:
Cardiovascular: Cardiac arrhythmia, hypertension
Central nervous system: Apathy, drowsiness, hyperthermia, metallic taste, psychosis, sensory disturbance
Dermatologic: Erythema, erythema multiforme, pruritus, urticaria
Endocrine & metabolic: Albuminuria, calcinosis, decreased libido, dehydration, growth suppression, hypercholesterolemia, weight loss
Gastrointestinal: Anorexia, constipation, pancreatitis, stomach pain, vomiting, xerostomia
Genitourinary: Hypercalciuria, nocturia
Hepatic: Increased serum ALT, increased serum AST
Hypersensitivity: Hypersensitivity reaction
Local: Pain at injection site (mild)
Neuromuscular & skeletal: Dystrophy, myalgia, ostealgia, weakness
Ophthalmic: Conjunctivitis, photophobia
Renal: Calcium nephrolithiasis, increased blood urea nitrogen, increased serum creatinine, polyuria
Respiratory: Rhinorrhea
<1%, postmarketing and/or case reports: Agitation, anaphylaxis, apprehension, hypermagnesemia, hyperphosphatemia, hypervitaminosis D, increased hematocrit, increased hemoglobin, increased neutrophils, increased serum alkaline phosphatase, insomnia, limb pain, lymphocytosis
Warnings/Precautions
Concerns related to adverse effects:
- Excessive vitamin D: Excessive vitamin D administration may lead to over suppression of parathyroid hormone (PTH), progressive or acute hypercalcemia, hypercalciuria, hyperphosphatemia and adynamic bone disease. Withhold pharmacologic doses of vitamin D and its derivatives during therapy to avoid the potential for hypercalcemia to develop. In addition, several months may be required for ergocalciferol levels to return to baseline in patients switching from ergocalciferol therapy to calcitriol.
- Hypercalcemia: Monitor calcium levels closely with initiation of therapy and with dose adjustments; discontinue use promptly in patients who develop hypercalcemia. Avoid abrupt dietary modifications (eg, increased intake of dairy products) which may lead to hypercalcemia; adjust calcium intake if indicated and maintain adequate hydration. Chronic hypercalcemia can result in generalized vascular and soft tissue calcification, exacerbate nephrolithiasis, and has been associated with increased mortality in adults with chronic kidney disease (CKD) (KDIGO 2017). Immobilized patients may be at a higher risk for hypercalcemia.
Disease-related concerns:
- Malabsorption syndrome: Use oral calcitriol with caution in patients with malabsorption syndromes; efficacy may be limited and/or response may be unpredictable.
- Renal impairment: Use of calcitriol for the treatment of secondary hyperparathyroidism associated with CKD is not recommended in patients with rapidly worsening kidney function or in noncompliant patients. Increased serum phosphate levels in patients with renal failure may lead to ectopic calcification; the use of a non-aluminum-containing phosphate-lowering agent is recommended along with a low phosphate diet in patients undergoing dialysis.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Dosage form specific issues:
- Aluminum: The parenteral product may contain aluminum; toxic aluminum concentrations may be seen with high doses, prolonged use, or renal dysfunction. Premature neonates are at higher risk due to immature renal function and aluminum intake from other parenteral sources. Parenteral aluminum exposure of >4 to 5 mcg/kg/day is associated with CNS and bone toxicity; tissue loading may occur at lower doses (Federal Register 2002). See manufacturer’s labeling.
- Coconut oil: Products may contain coconut oil (capsule).
- Palm seed oil: Products may contain palm seed oil (oral solution).
- Tartrazine: Some products may contain tartrazine.
Other warnings/precautions:
- Calcium: Adequate dietary (supplemental) calcium is necessary for clinical response to vitamin D. Patients with a tendency to develop hypercalcemia may require low doses of calcium or no supplementation at all.
Monitoring Parameters
Secondary hyperparathyroidism (CKD patients): Note: The frequency of serum calcium, phosphate, and parathyroid hormone (PTH) measurements may be dependent upon the presence and magnitude of abnormalities, the rate of progression of chronic kidney disease (CKD), and the use of treatments for chronic kidney disease-mineral and bone disorder (KDIGO 2017).
During therapy initiation and dosage adjustments: Frequent monitoring of serum calcium and phosphate levels (eg, at least twice weekly) is recommended (manufacturer’s labeling).
KDIGO guidelines (2017): Note: During treatment or when biochemical abnormalities are identified more frequent monitoring may be reasonable.
CKD stage G3a to G3b: Serum calcium and phosphate: Every 6 to 12 months; PTH: Frequency based on baseline level and progression of CKD; alkaline phosphatase
CKD stage G4: Serum calcium and phosphate: Every 3 to 6 months; PTH: Every 6 to 12 months; alkaline phosphatase every 12 months or more frequently in the presence of elevated PTH
CKD stage G5 and G5D: Serum calcium and phosphate: Every 1 to 3 months; PTH: Every 3 to 6 months; alkaline phosphatase every 12 months or more frequently in the presence of elevated PTH
Hypoparathyroidism: Note: Frequency of measurement is dependent upon on how stable a patient is to a given dosage regimen with more frequent measurements (eg, weekly) required initially during dosage titration. Once patient is well controlled, monitoring may be required on a yearly or twice-yearly basis (Endocrine Society [Brandi 2016])
Serum calcium, phosphate, and magnesium; renal function (ie, 24-hour urinary calcium and creatinine, blood urea nitrogen [BUN], measured CrCl or estimated glomerular filtration rate [eGFR]); renal imaging (every 5 years in asymptomatic patients with a history of renal lithiasis or calcinosis or more frequently as indicated); CNS imaging (basal ganglia and other sites of calcification), ophthalmologic exam, and/or BMD as indicated (Endocrine Society [Brandi 2016])
Hypophosphatemia, X-linked (off-label use):Serum calcium, phosphorous, PTH, alkaline phosphatase (ALP) (elevation in ALP of bone-origin may indicate extensive osteomalacia), and creatinine and 24-hour urinary calcium and creatinine (4 to 6 weeks after initiation of therapy, 6 to 8 weeks after satisfactory biochemical response is achieved and then every 3 to 4 months for the first year and every 6 to 9 months thereafter (Carpenter 2011)
Pregnancy
Pregnancy Risk Factor
C
Pregnancy Considerations
Adverse effects have been observed in some animal reproduction studies. Maternal calcitriol may be detected in the fetal circulation. Mild hypercalcemia has been reported in a newborn following maternal use of calcitriol during pregnancy. Adverse effects on fetal development were not observed with use of calcitriol during pregnancy in women (N=9) with pseudovitamin D-dependent rickets. Doses were adjusted every 4 weeks to keep calcium concentrations within normal limits (Edouard 2011). If calcitriol is used for the management of hypoparathyroidism in pregnancy, dose adjustments may be needed as pregnancy progresses and again following delivery. Vitamin D and calcium levels should be monitored closely and kept in the lower normal range (Callies 1998).
Patient Education
What is this drug used for?
- It is used to control low blood calcium levels in certain patients.
- It is used to treat high parathyroid hormone levels in certain patients.
- It may be given to you for other reasons. Talk with the doctor.
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- High calcium like weakness, confusion, fatigue, headache, nausea and vomiting, constipation, or bone pain.
- Fluid and electrolyte problems like mood changes, confusion, muscle pain or weakness, abnormal heartbeat, severe dizziness, passing out, fast heartbeat, increased thirst, seizures, loss of strength and energy, lack of appetite, unable to pass urine or change in amount of urine passed, dry mouth, dry eyes, or nausea or vomiting.
- Passing a lot of urine
- Metallic taste
- Abdominal pain
- Eye irritation
- Weight loss
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.