Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Capsule, Oral:
Florical: 364 mg (elemental calcium 145 mg) and fluoride 3.75 mg
Powder, Oral:
Generic: Elemental calcium 800 mg/2 g (480 g)
Suspension, Oral:
Generic: 1250 mg (elemental calcium 500 mg) per 5 mL (5 mL, 473 mL, 500 mL)
Tablet, Oral:
Cal-Carb Forte: 1250 mg (elemental calcium 500 mg) [DSC]
Calcium 600: 1500 mg (elemental calcium 600 mg) [scored]
Calcium 600: 1500 mg (elemental calcium 600 mg) [contains fd&c yellow #6 aluminum lake, soy polysaccarides]
Calcium High Potency: 1500 mg (elemental calcium 600 mg) [contains fd&c yellow #6 (sunset yellow)]
Caltrate 600: 1500 mg (elemental calcium 600 mg) [scored]
Florical: 364 mg (elemental calcium 145 mg) and fluoride 3.75 mg
Oysco 500: 1250 mg (elemental calcium 500 mg) [contains brilliant blue fcf (fd&c blue #1), tartrazine (fd&c yellow #5)]
Generic: 648 mg, 1250 mg (elemental calcium 500 mg), 1500 mg (elemental calcium 600 mg)
Tablet, Oral [preservative free]:
Calcium 600: 1500 mg (elemental calcium 600 mg) [lactose free, salt free, sugar free]
Generic: 1250 mg (elemental calcium 500 mg), 1500 mg (elemental calcium 600 mg)
Tablet Chewable, Oral:
Antacid: 500 mg
Antacid: 500 mg [peppermint flavor]
Antacid: 500 mg [contains brilliant blue fcf (fd&c blue #1), fd&c yellow #10 (quinoline yellow), fd&c yellow #6 (sunset yellow)]
Antacid: 500 mg [contains fd&c blue #1 aluminum lake, fd&c red #40 aluminum lake, fd&c yellow #5 aluminum lake, fd&c yellow #6 aluminum lake]
Antacid Calcium: 500 mg [peppermint flavor]
Antacid Calcium: 500 mg [gluten free; peppermint flavor]
Antacid Calcium Extra Strength: 750 mg [DSC] [contains fd&c blue #1 aluminum lake, fd&c red #40 aluminum lake; assorted flavor]
Antacid Calcium Extra Strength: 750 mg [DSC] [gluten free; contains fd&c blue #1 aluminum lake, fd&c red #40 aluminum lake; assorted fruit flavor]
Antacid Extra Strength: 750 mg [contains brilliant blue fcf (fd&c blue #1), fd&c red #40]
Antacid Extra Strength: 750 mg [contains corn starch, fd&c blue #1 aluminum lake, fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake; assorted flavor]
Antacid Extra Strength: 750 mg [contains fd&c red #40, fd&c yellow #6 (sunset yellow), tartrazine (fd&c yellow #5)]
Cal-Gest Antacid: 500 mg [contains fd&c blue #1 aluminum lake, fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake; assorted fruit flavor]
Cal-Mint: Elemental calcium 260 mg [animal products free, gelatin free, gluten free, lactose free, no artificial color(s), no artificial flavor(s), starch free, sugar free, yeast free]
Calci-Chew: 1250 mg (elemental calcium 500 mg) [cherry flavor]
Calcium Antacid: 500 mg [contains brilliant blue fcf (fd&c blue #1), fd&c red #40, fd&c yellow #10 (quinoline yellow), fd&c yellow #6 (sunset yellow)]
Calcium Antacid: 500 mg [contains brilliant blue fcf (fd&c blue #1), fd&c red #40, fd&c yellow #6 (sunset yellow), soybeans (glycine max), tartrazine (fd&c yellow #5); assorted flavor]
Calcium Antacid: 500 mg [contains fd&c blue #1 aluminum lake]
Calcium Antacid: 500 mg [contains fd&c blue #1 aluminum lake, fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake; assorted fruit flavor]
Calcium Antacid Extra Strength: 750 mg [contains brilliant blue fcf (fd&c blue #1), fd&c red #40]
Calcium Antacid Extra Strength: 750 mg [contains brilliant blue fcf (fd&c blue #1), fd&c red #40, fd&c yellow #6 (sunset yellow), tartrazine (fd&c yellow #5); assorted flavor]
Calcium Antacid Extra Strength: 750 mg [contains corn starch, fd&c blue #1 aluminum lake, fd&c red #40 aluminum lake; assorted flavor]
Calcium Antacid Extra Strength: 750 mg [DSC] [gluten free; contains brilliant blue fcf (fd&c blue #1), fd&c yellow #10 (quinoline yellow), fd&c yellow #6 (sunset yellow)]
Calcium Antacid Ultra Max St: 1000 mg [contains brilliant blue fcf (fd&c blue #1), fd&c red #40, fd&c yellow #6 (sunset yellow), soybeans (glycine max), tartrazine (fd&c yellow #5)]
GoodSense Antacid: 500 mg [contains corn starch, fd&c blue #1 aluminum lake, fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake]
GoodSense Antacid: 750 mg [gluten free; contains corn starch, fd&c blue #1 aluminum lake, fd&c red #40 aluminum lake; assorted flavor]
GoodSense Antacid: 750 mg [gluten free; contains corn starch, fd&c blue #1 aluminum lake, fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake; assorted flavor]
GoodSense Antacid: 1000 mg [gluten free; contains corn starch, fd&c blue #1 aluminum lake, fd&c red #40 aluminum lake; assorted flavor]
GoodSense Antacid: 1000 mg [gluten free; contains corn starch, fd&c blue #1 aluminum lake, fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake; assorted flavor]
Maalox: 600 mg [contains aspartame; wild berry flavor]
Maalox Childrens: 400 mg [contains aspartame; wild berry flavor]
Titralac: 420 mg [low sodium, sugar free; contains saccharin]
Tums: 500 mg [peppermint flavor]
Tums: 500 mg [gluten free]
Tums: 500 mg [gluten free; contains fd&c blue #1 aluminum lake, fd&c red #40 aluminum lake, fd&c yellow #6 aluminum lake, tartrazine (fd&c yellow #5)]
Tums Chewy Bites: 750 mg [contains corn starch, fd&c blue #1 aluminum lake, fd&c blue #2 aluminum lake, fd&c red #40 aluminum lake, fd&c yellow #5 aluminum lake, fd&c yellow #6 aluminum lake, methylparaben, propylparaben, sodium benzoate, soybean lecithin, soybean oil]
Tums Chewy Delights: 1177 mg [contains coconut oil (copra/cocos nucifera oil), corn starch, fd&c yellow #6 (sunset yellow), soybean lecithin]
Tums Chewy Delights: 1177 mg [contains fd&c red #40 aluminum lake, soybean lecithin; cherry flavor]
Tums E-X 750: 750 mg
Tums E-X 750: 750 mg [assorted flavor]
Tums E-X 750: 750 mg [gluten free; contains fd&c blue #1 aluminum lake, fd&c red #40 aluminum lake; assorted berries flavor]
Tums E-X 750: 750 mg [sugar free]
Tums Extra Strength 750: 750 mg [gluten free; contains fd&c blue #1 aluminum lake, fd&c red #40 aluminum lake, fd&c yellow #5 aluminum lake, fd&c yellow #6 aluminum lake; assorted fruit flavor]
Tums Extra Strength 750: 750 mg [sugar free; contains fd&c red #40 aluminum lake, fd&c yellow #5 aluminum lake]
Tums Freshers: 500 mg [DSC] [gluten free; contains brilliant blue fcf (fd&c blue #1); mint flavor]
Tums Freshers: 500 mg [DSC] [kosher certified; contains brilliant blue fcf (fd&c blue #1), tartrazine (fd&c yellow #5)]
Tums Freshers: 500 mg [DSC] [kosher certified; contains brilliant blue fcf (fd&c blue #1), tartrazine (fd&c yellow #5); spearmint flavor]
Tums Kids: 750 mg [DSC] [scored; contains fd&c blue #1 aluminum lake, fd&c red #40 aluminum lake; cherry flavor]
Tums Lasting Effects: 500 mg [contains fd&c red #40 aluminum lake, fd&c yellow #6 aluminum lake, tartrazine (fd&c yellow #5)]
Tums Smoothies: 750 mg [peppermint flavor]
Tums Smoothies: 750 mg [contains fd&c blue #1 aluminum lake, fd&c red #40 aluminum lake, fd&c yellow #6 aluminum lake, soybeans (glycine max); assorted tropical fruit flavor]
Tums Smoothies: 750 mg [contains fd&c blue #1 aluminum lake, fd&c red #40 aluminum lake, soybeans (glycine max); berry flavor]
Tums Smoothies: 750 mg [gluten free; contains corn starch, fd&c blue #1 aluminum lake, fd&c red #40 aluminum lake, fd&c yellow #5 aluminum lake, fd&c yellow #6 aluminum lake, soybeans (glycine max)]
Tums Ultra 1000: 1000 mg
Tums Ultra 1000: 1000 mg [peppermint flavor]
Tums Ultra 1000: 1000 mg [contains fd&c blue #1 aluminum lake, fd&c red #40 aluminum lake, fd&c yellow #5 aluminum lake, fd&c yellow #6 aluminum lake; assorted berries flavor]
Tums Ultra 1000: 1000 mg [contains fd&c red #40 aluminum lake, fd&c yellow #6 aluminum lake, tartrazine (fd&c yellow #5); assorted tropical fruit flavor]
Tums Ultra 1000: 1000 mg [gluten free; contains fd&c blue #1 aluminum lake, fd&c red #40 aluminum lake, fd&c yellow #6 aluminum lake, tartrazine (fd&c yellow #5)]
Generic: 500 mg, 750 mg, 1250 mg (elemental calcium 500 mg), Elemental calcium 260 mg
Pharmacology
Mechanism of Action
As dietary supplement, used to prevent or treat negative calcium balance; in osteoporosis, it helps to prevent or decrease the rate of bone loss. Calcium is an integral component of the skeleton and also moderates nerve and muscle performance and allows normal cardiac function. Also used to treat hyperphosphatemia in patients with chronic kidney disease by combining with dietary phosphate to form insoluble calcium phosphate, which is excreted in feces. Calcium salts as antacids neutralize gastric acidity resulting in increased gastric and duodenal bulb pH; they additionally inhibit proteolytic activity of pepsin if the pH is increased >4 and increase lower esophageal sphincter tone (IOM, 2011).
Pharmacokinetics/Pharmacodynamics
Absorption
Minimal unless chronic, high doses; absorption predominantly in the duodenum and dependent on calcitriol and vitamin D; mean absorption of calcium intake varies with age (infants 60%, prepubertal children 28%, pubertal children 34%, adults 25%); during pregnancy, calcium absorption doubles; calcium is absorbed in soluble, ionized form; solubility of calcium is increased in an acid environment (IOM 2011); decreased absorption occurs in patients with achlorhydria, renal osteodystrophy, steatorrhea, or uremia
Distribution
Primarily in bones, teeth (IOM, 2011)
Excretion
Primarily feces (75%; as unabsorbed calcium); urine (22%) (IOM, 2011)
Protein Binding
~40%, primarily to albumin (Wills 1971)
Use: Labeled Indications
Antacid: For the relief of acid indigestion, heartburn, sour stomach, and GI upset associated with these symptoms
Calcium supplementation: For use as a dietary supplement when calcium intake may be inadequate (eg, osteoporosis, osteomalacia, hypocalcemic rickets) (IOM 2011)
Use: Off Label
Hyperphosphatemia in chronic kidney diseasebyes
In a meta-analysis of trials evaluating the use of phosphate binders in patients with chronic kidney disease (CKD), the use of calcium carbonate was shown to be safe and effective Navaneethan 2009.
Based on the National Kidney Foundation K/DOQI clinical practice guidelines for bone metabolism and disease in CKD, calcium-containing phosphate lowering agents given for hyperphosphatemia in CKD (stages 3 to 5) are effective and recommended in the management of this condition. Based on the Kidney Disease: Improving Global Outcomes (KDIGO) Clinical Practice Guideline Update for the Diagnosis, Evaluation, Prevention, and Treatment of Chronic Kidney Disease–Mineral and Bone Disorder (CKD-MBD), preventative treatment with phosphate-lowering agents is not recommended; when used in cases of overt hyperphosphatemia, restricting the dose of calcium-based phosphate binders is recommended.
Hypoparathyroidism (management of chronic hypocalcemia)yes
Based on guidelines from the Endocrine Society and the European Society of Endocrinology for the management of hypoparathyroidism, supplemental calcium (in conjunction with vitamin D) is effective and recommended in the management of chronic hypocalcemia associated with hypoparathyroidism Endocrine Society [Brandi 2016], European Society of Endocrinology [Bollerslev 2015]. Other oral calcium preparations (calcium citrate) are preferred for patients with achlorhydria or who are on chronic proton pump inhibitor therapy European Society of Endocrinology [Bollerslev 2015].
Contraindications
Hypersensitivity to any component of the formulation
Dosage and Administration
Dosing: Adult
Note: One gram of calcium carbonate is equal to 400 mg of elemental calcium.
Antacid: Oral: Generally, 1 to 4 tablets as symptoms occur; maximum: 8 g/day as calcium carbonate for up to 2 weeks; OTC dosing recommendations may vary by product and/or manufacturer; specific product labeling should be consulted
Calcium supplementation (OTC labeling): Oral: 500 mg to 4 g/day as calcium carbonate (equivalent to 200 mg to 1.6 g of elemental calcium) in 1 to 3 divided doses.
Note: The recommended daily intake of elemental calcium (from dietary sources and supplemental sources if needed) for optimal bone health is 1.2 g/day (postmenopausal women) or 1 to 1.2 g/day in other adults. It is preferred to obtain these daily amounts primarily through dietary sources. There is no evidence that intakes higher than these improve bone strength (AACE [Camacho 2016]; Endocrine Society [Watts 2012]; IOM 2011; NOF [Cosman 2014]).
Hyperphosphatemia in chronic kidney disease (off-label use): Oral: Total dose of elemental calcium (including dietary sources and calcium-based phosphate binders) should not exceed 2 g/day (Eknoyan 2003).
Hypoparathyroidism (management of chronic hypocalcemia) (off-label use): Oral: 500 mg to 1 g of elemental calcium administered 2 to 3 times daily; required dose can vary greatly and more frequent dosing may be necessary. Note: Use of IV calcium may be required in acute hypocalcemia with corrected calcium <7 mg/dL [≤1.75 mmol/L] or in severely symptomatic patients (eg, arrhythmias, broncho- or laryngospasm, tetany, seizures) (Bilezikian 2016)
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Antacid: Note: Chronic antacid therapy not recommended for management of GERD in pediatric patients (AAP [Lightdale 2013]; Vandenplas 2009). OTC products may vary in approved ages and uses; consult product specific labeling for details. Dose expressed as calcium carbonate.
Children 2 to 5 years, weighing >10.9 kg: Oral: 375 to 400 mg of calcium carbonate as symptoms occur for up to 2 weeks; maximum daily dose: 1,500 mg/day of calcium carbonate
Children 6 to 11 years: Oral: 750 to 800 mg of calcium carbonate as symptoms occur for up to 2 weeks; maximum daily dose: 3,000 mg/day of calcium carbonate
Children ≥12 years and Adolescents: Oral: 500 to 3,000 mg of calcium carbonate as symptoms occur for up to 2 weeks; maximum daily dose: 7,500 mg/day of calcium carbonate
Calcium dietary supplementation: Oral:
Children 2 to 4 years: 750 mg of calcium carbonate twice daily
Children ≥4 years and Adolescents: 750 mg of calcium carbonate 3 times daily
Hypocalcemia: Dose depends on clinical condition and serum calcium concentration: Dose expressed as elemental calcium: Limited data available: Oral: Infants and Children: 45 to 65 mg/kg/day in 4 divided doses (Nelson 1996)
Hyperphosphatemia in chronic kidney disease: Infants, Children, and Adolescents: Limited data available: Oral: Calcium provided from phosphate binders should be limited to 1,500 mg/day of elemental calcium and total calcium intake (including dietary sources and calcium-based phosphate binders) should not exceed 2,000 mg/day of elemental calcium (KDOQI [Uhlig 2010])
Rickets (due to vitamin D deficiency); treatment: Limited data available: Infants and Children: Dose expressed as elemental calcium: Oral: 30 to 75 mg/kg/day in 3 divided doses; begin at higher end of range and titrate downward over 2 to 4 weeks (Misra 2008)
Administration
Oral: Administer with food. Doses >600 mg (elemental calcium) per day should be divided for optimal absorption (AACE [Camacho 2016]).
Capsules may be swallowed whole or opened and the contents mixed with food or drink.
Dietary Considerations
Take with food. Limit intake of bran, foods high in oxalates, or whole grain cereals which may decrease calcium absorption.
Some products may contain phenylalanine and/or sodium.
Dietary Reference Intake for Calcium (IOM 2011):
0 to <6 months: Adequate intake: 200 mg elemental calcium daily
6 to 12 months: Adequate intake: 260 mg elemental calcium daily
1 to 3 years: RDA: 700 mg elemental calcium daily
4 to 8 years: RDA: 1,000 mg elemental calcium daily
9 to 18 years: RDA: 1,300 mg elemental calcium daily
19 to 50 years: RDA: 1,000 mg elemental calcium daily
Females ≥51 years: RDA: 1,200 mg elemental calcium daily
Males: 51 to 70 years: RDA: 1,000 mg elemental calcium daily; >70 years: RDA: 1,200 mg elemental calcium daily
Pregnancy/Lactating: RDA: Requirements are the same as in nonpregnant or nonlactating females
Storage
Store between 15°C to 30°C (59°F to 86°F). Protect oral suspension from freezing.
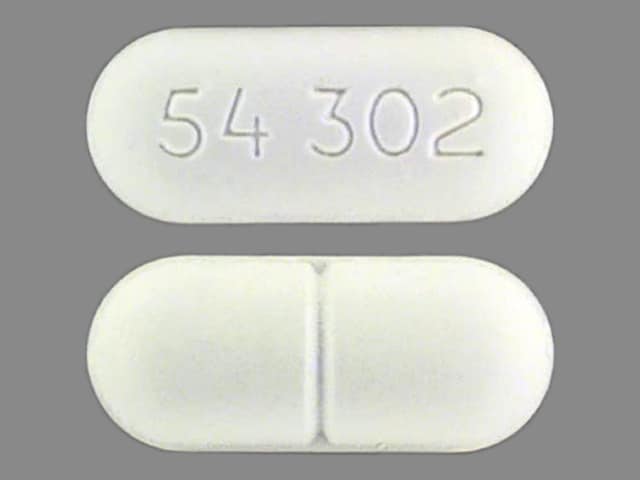
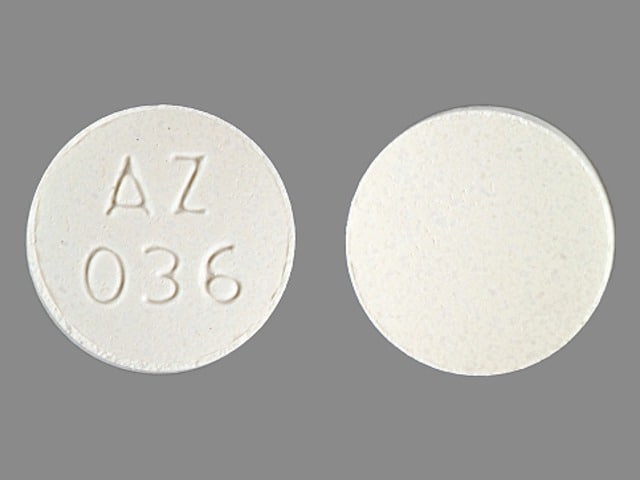
Calcium Carbonate Images
Drug Interactions
Acalabrutinib: Antacids may decrease the serum concentration of Acalabrutinib. Management: Separate administration of acalabrutinib from the administration of any antacids by at least 2 hours in order to minimize the potential for a significant interaction. Consider therapy modification
Allopurinol: Antacids may decrease the absorption of Allopurinol. Consider therapy modification
Alpha-Lipoic Acid: Calcium Salts may decrease the absorption of Alpha-Lipoic Acid. Alpha-Lipoic Acid may decrease the absorption of Calcium Salts. Consider therapy modification
Amphetamines: Antacids may decrease the excretion of Amphetamines. Monitor therapy
Antipsychotic Agents (Phenothiazines): Antacids may decrease the absorption of Antipsychotic Agents (Phenothiazines). Monitor therapy
Atazanavir: Antacids may decrease the absorption of Atazanavir. Consider therapy modification
Baloxavir Marboxil: Polyvalent Cation Containing Products may decrease the serum concentration of Baloxavir Marboxil. Avoid combination
Bictegravir: Calcium Salts may decrease the serum concentration of Bictegravir. Management: Bictegravir, emtricitabine, and tenofovir alafenamide can be administered with calcium salts under fed conditions, but coadministration with or 2 hours after a calcium salt is not recommended under fasting conditions. Consider therapy modification
Bisacodyl: Antacids may diminish the therapeutic effect of Bisacodyl. Antacids may cause the delayed-release bisacodyl tablets to release drug prior to reaching the large intestine. Gastric irritation and/or cramps may occur. Consider therapy modification
Bismuth Subcitrate: Antacids may diminish the therapeutic effect of Bismuth Subcitrate. Management: Avoid administration of antacids within 30 minutes of bismuth subcitrate (tripotassium bismuth dicitrate) administration. Consider therapy modification
Bisphosphonate Derivatives: Polyvalent Cation Containing Products may decrease the serum concentration of Bisphosphonate Derivatives. Management: Avoid administration of oral medications containing polyvalent cations within: 2 hours before or after tiludronate/clodronate/etidronate; 60 minutes after oral ibandronate; or 30 minutes after alendronate/risedronate. Exceptions: Pamidronate; Zoledronic Acid. Consider therapy modification
Bosutinib: Antacids may decrease the serum concentration of Bosutinib. Management: Administer antacids more than 2 hours before or after bosutinib. Consider therapy modification
Bromperidol: Antacids may decrease the absorption of Bromperidol. Monitor therapy
Calcium Acetate: Calcium Salts may enhance the adverse/toxic effect of Calcium Acetate. Avoid combination
Calcium Channel Blockers: Calcium Salts may diminish the therapeutic effect of Calcium Channel Blockers. Monitor therapy
Calcium Polystyrene Sulfonate: Antacids may enhance the adverse/toxic effect of Calcium Polystyrene Sulfonate. The combined use of these two agents may result in metabolic alkalosis and/or loss of efficacy of the cation exchange resin. Management: To minimize this interaction, consider: a)separating doses by 2 or more hours; b)rectal administration of the exchange resin; or c)alternatives to antacids. Monitor for metabolic alkalosis and attenuation of CPS effects. Avoid magnesium hydroxide. Consider therapy modification
Captopril: Antacids may decrease the serum concentration of Captopril. Monitor therapy
Cardiac Glycosides: Calcium Salts may enhance the arrhythmogenic effect of Cardiac Glycosides. Monitor therapy
Cefditoren: Antacids may decrease the serum concentration of Cefditoren. Management: Concomitant use of cefditoren with antacids is not recommended. Consider alternative methods to control acid reflux (eg, diet modification) or alternative antimicrobial therapy. If antacid therapy can not be avoided, separate dosing by several hours. Consider therapy modification
Cefpodoxime: Antacids may decrease the serum concentration of Cefpodoxime. Monitor therapy
Cefuroxime: Antacids may decrease the serum concentration of Cefuroxime. Management: Administer cefuroxime axetil at least 1 hour before or 2 hours after the administration of short-acting antacids. Consider therapy modification
Chloroquine: Antacids may decrease the serum concentration of Chloroquine. Management: Separate administration of antacids and chloroquine by at least 4 hours to minimize any potential negative impact of antacids on chloroquine bioavailability. Consider therapy modification
Corticosteroids (Oral): Antacids may decrease the bioavailability of Corticosteroids (Oral). Management: Consider separating doses by 2 or more hours. Budesonide enteric coated tablets could dissolve prematurely if given with drugs that lower gastric acid, with unknown impact on budesonide therapeutic effects. Consider therapy modification
Cysteamine (Systemic): Antacids may diminish the therapeutic effect of Cysteamine (Systemic). Monitor therapy
Dabigatran Etexilate: Antacids may decrease the serum concentration of Dabigatran Etexilate. Management: Dabigatran etexilate Canadian product labeling recommends avoiding concomitant use with antacids for 24 hours after surgery. In other situations, administer dabigatran etexilate 2 hours prior to antacids. Monitor clinical response to dabigatran therapy. Consider therapy modification
Dasatinib: Antacids may decrease the serum concentration of Dasatinib. Management: Simultaneous administration of dasatinib and antacids should be avoided. Administer antacids 2 hours before or 2 hours after dasatinib. Consider therapy modification
Deferiprone: Polyvalent Cation Containing Products may decrease the serum concentration of Deferiprone. Management: Separate administration of deferiprone and oral medications or supplements that contain polyvalent cations by at least 4 hours. Consider therapy modification
Delavirdine: Antacids may decrease the serum concentration of Delavirdine. Management: Separate doses of delavirdine and antacids by at least 1 hour. Monitor for decreased delavirdine therapeutic effects with this combination. Consider therapy modification
Dexmethylphenidate: Antacids may increase the absorption of Dexmethylphenidate. Specifically, antacids may interfere with the normal release of drug from the extended-release capsules (Focalin XR brand), which could result in both increased absorption (early) and decreased delayed absorption. Monitor therapy
Diacerein: Antacids may decrease the absorption of Diacerein. Monitor therapy
DOBUTamine: Calcium Salts may diminish the therapeutic effect of DOBUTamine. Monitor therapy
Dolutegravir: Calcium Salts may decrease the serum concentration of Dolutegravir. Management: Administer dolutegravir at least 2 hours before or 6 hours after oral calcium. Administer dolutegravir/rilpivirine at least 4 hours before or 6 hours after oral calcium salts. Alternatively, dolutegravir and oral calcium can be taken together with food. Consider therapy modification
Eltrombopag: Polyvalent Cation Containing Products may decrease the serum concentration of Eltrombopag. Management: Administer eltrombopag at least 2 hours before or 4 hours after oral administration of any polyvalent cation containing product. Consider therapy modification
Elvitegravir: Antacids may decrease the serum concentration of Elvitegravir. Management: Separate administration of antacids and elvitegravir-containing products by at least 2 hours in order to minimize the risk for an interaction. Consider therapy modification
Erdafitinib: Serum Phosphate Level-Altering Agents may diminish the therapeutic effect of Erdafitinib. Management: Avoid coadministration of serum phosphate level-altering agents with erdafitinib before initial dose increase period based on serum phosphate levels (Days 14 to 21). Consider therapy modification
Erlotinib: Antacids may decrease the serum concentration of Erlotinib. Management: Separate the administration of erlotinib and any antacid by several hours in order to minimize the risk of a significant interaction. Consider therapy modification
Estramustine: Calcium Salts may decrease the absorption of Estramustine. Consider therapy modification
Fosinopril: Antacids may decrease the serum concentration of Fosinopril. Management: The US and Canadian fosinopril manufacturer labels recommend separating the doses of antacids and fosinopril by 2 hours. Consider therapy modification
Gefitinib: Antacids may decrease the serum concentration of Gefitinib. Management: Administer gefitinib at least 6 hours before or after administration of an antacid, and closely monitor clinical response to gefitinib. Consider therapy modification
Hyoscyamine: Antacids may decrease the serum concentration of Hyoscyamine. Management: Administer immediate release hyoscyamine before meals and antacids after meals when these agents are given in combination. Consider therapy modification
Iron Preparations: Antacids may decrease the absorption of Iron Preparations. Management: Separate dosing of oral iron preparations and antacids as much as possible to avoid decreased efficacy of iron preparation. If coadministered with antacids, monitor for decreased therapeutic effects of iron preparations. Exceptions: Ferric Carboxymaltose; Ferric Citrate; Ferric Derisomaltose; Ferric Gluconate; Ferric Hydroxide Polymaltose Complex; Ferric Pyrophosphate Citrate; Ferumoxytol; Iron Dextran Complex; Iron Sucrose. Consider therapy modification
Itraconazole: Antacids may decrease the serum concentration of Itraconazole. Antacids may increase the serum concentration of Itraconazole. Management: Administer Sporanox brand itraconazole at least 2 hours before or 2 hours after administration of any antacids. Exposure to Tolsura brand itraconazole may be increased by antacids; consider itraconazole dose reduction. Consider therapy modification
Ketoconazole (Systemic): Antacids may decrease the serum concentration of Ketoconazole (Systemic). Management: Administer oral ketoconazole at least 2 hours prior to use of any antacid product. Monitor patients closely for signs of inadequate clinical response to ketoconazole. Consider therapy modification
Lanthanum: Antacids may diminish the therapeutic effect of Lanthanum. Consider therapy modification
Ledipasvir: Antacids may decrease the serum concentration of Ledipasvir. Management: Separate the administration of ledipasvir and antacids by 4 hours. Consider therapy modification
Mesalamine: Antacids may diminish the therapeutic effect of Mesalamine. Antacid-mediated increases in gastrointestinal pH may cause the premature release of mesalamine from specific sustained-release mesalamine products. Management: Avoid concurrent administration of antacids with sustained-release mesalamine products. Separating antacid and mesalamine administration, and/or using lower antacid doses may be adequate means of avoiding this interaction. Consider therapy modification
Methenamine: Antacids may diminish the therapeutic effect of Methenamine. Consider therapy modification
Methylphenidate: Antacids may increase the absorption of Methylphenidate. Specifically, antacids may interfere with the normal release of drug from the extended-release capsules (Ritalin LA brand), which could result in both increased absorption (early) and decreased delayed absorption. Monitor therapy
Multivitamins/Fluoride (with ADE): May increase the serum concentration of Calcium Salts. Calcium Salts may decrease the serum concentration of Multivitamins/Fluoride (with ADE). More specifically, calcium salts may impair the absorption of fluoride. Management: Avoid eating or drinking dairy products or consuming vitamins or supplements with calcium salts one hour before or after of the administration of fluoride. Consider therapy modification
Multivitamins/Minerals (with ADEK, Folate, Iron): Antacids may decrease the serum concentration of Multivitamins/Minerals (with ADEK, Folate, Iron). Specifically, antacids may decrease the absorption of orally administered iron. Management: Separate dosing of oral iron-containing multivitamin preparations and antacids by as much time as possible in order to minimize impact on therapeutic efficacy of the iron preparation. Consider therapy modification
Mycophenolate: Antacids may decrease the absorption of Mycophenolate. Management: Separate doses of mycophenolate and antacids by at least 2 hours. Monitor for reduced effects of mycophenolate if taken concomitant with antacids. Consider therapy modification
Neratinib: Antacids may decrease the serum concentration of Neratinib. Specifically, antacids may reduce neratinib absorption. Management: Separate the administration of neratinib and antacids by giving neratinib at least 3 hours after the antacid. Consider therapy modification
Nilotinib: Antacids may decrease the serum concentration of Nilotinib. Management: Separate the administration of nilotinib and any antacid by at least 2 hours whenever possible in order to minimize the risk of a significant interaction. Consider therapy modification
PAZOPanib: Antacids may decrease the serum concentration of PAZOPanib. Management: Avoid the use of antacids in combination with pazopanib whenever possible. Separate doses by several hours if antacid treatment is considered necessary. The impact of dose separation has not been investigated. Consider therapy modification
PenicillAMINE: Polyvalent Cation Containing Products may decrease the serum concentration of PenicillAMINE. Management: Separate the administration of penicillamine and oral polyvalent cation containing products by at least 1 hour. Consider therapy modification
Pexidartinib: Antacids may decrease the serum concentration of Pexidartinib. Management: Administer pexidartinib 2 hours before or after antacids. Consider therapy modification
Phosphate Supplements: Antacids may decrease the absorption of Phosphate Supplements. Management: This applies only to oral phosphate administration. Separating administer of oral phosphate supplements from antacid administration by as long as possible may minimize the interaction. Exceptions: Sodium Glycerophosphate Pentahydrate. Consider therapy modification
Phosphate Supplements: Calcium Salts may decrease the absorption of Phosphate Supplements. Management: This applies only to oral phosphate and calcium administration. Administering oral phosphate supplements as far apart from the administration of an oral calcium salt as possible may be able to minimize the significance of the interaction. Exceptions: Sodium Glycerophosphate Pentahydrate. Consider therapy modification
Potassium Phosphate: Antacids may decrease the serum concentration of Potassium Phosphate. Management: Consider separating administration of antacids and oral potassium phosphate by at least 2 hours to decrease risk of a significant interaction. Consider therapy modification
QuiNIDine: Antacids may decrease the excretion of QuiNIDine. Monitor therapy
Quinolones: Antacids may decrease the absorption of Quinolones. Of concern only with oral administration of quinolones. Management: Avoid concurrent administration of quinolones and antacids to minimize the impact of this interaction. Recommendations for optimal dose separation vary by specific quinolone. Exceptions: LevoFLOXacin (Oral Inhalation). Consider therapy modification
Quinolones: Calcium Salts may decrease the absorption of Quinolones. Of concern only with oral administration of both agents. Exceptions: LevoFLOXacin (Oral Inhalation); Moxifloxacin (Systemic). Consider therapy modification
Raltegravir: Calcium Carbonate may decrease the serum concentration of Raltegravir. Management: Use of once-daily raltegravir with calcium carbonate is not recommended; dose separation does not appear to be adequate to minimize the significance of this interaction. Use of other raltegravir products do not require any dose change. Consider therapy modification
Rilpivirine: Antacids may decrease the serum concentration of Rilpivirine. Management: Administer antacids at least 2 hours before or 4 hours after rilpivirine. Administer antacids at least 6 hours before or 4 hours after the rilpivirine/dolutegravir combination product. Consider therapy modification
Riociguat: Antacids may decrease the serum concentration of Riociguat. Management: Separate the administration of antacids and riociguat by at least 1 hour in order to minimize any potential interaction. Consider therapy modification
Rosuvastatin: Antacids may decrease the serum concentration of Rosuvastatin. Monitor therapy
Sodium Polystyrene Sulfonate: Antacids may enhance the adverse/toxic effect of Sodium Polystyrene Sulfonate. The combined use of these two agents may result in metabolic alkalosis and/or loss of efficacy of the exchange resin. Management: To minimize this interaction, consider: a)separating doses by 2 or more hours; b)rectal administration of the exchange resin; or c)alternatives to antacids. Monitor for metabolic alkalosis and attenuation of SPS effects. Avoid magnesium hydroxide. Consider therapy modification
Sotalol: Antacids may decrease the serum concentration of Sotalol. Management: Avoid simultaneous administration of sotalol and antacids. Administer antacids 2 hours after sotalol. Consider therapy modification
Strontium Ranelate: Calcium Salts may decrease the serum concentration of Strontium Ranelate. Management: Separate administration of strontium ranelate and oral calcium salts by at least 2 hours in order to minimize this interaction. Consider therapy modification
Sulpiride: Antacids may decrease the serum concentration of Sulpiride. Management: Separate administration of antacids and sulpiride by at least 2 hours in order to minimize the impact of antacids on sulpiride absorption. Consider therapy modification
Tetracyclines: Antacids may decrease the absorption of Tetracyclines. Management: Separate administration of antacids and oral tetracycline derivatives by several hours when possible to minimize the extent of this potential interaction. Exceptions: Eravacycline. Consider therapy modification
Tetracyclines: Calcium Salts may decrease the serum concentration of Tetracyclines. Management: If coadministration of oral calcium with oral tetracyclines can not be avoided, consider separating administration of each agent by several hours. Exceptions: Eravacycline. Consider therapy modification
Thiazide and Thiazide-Like Diuretics: May decrease the excretion of Calcium Salts. Continued concomitant use can also result in metabolic alkalosis. Monitor therapy
Thyroid Products: Calcium Salts may diminish the therapeutic effect of Thyroid Products. Management: Separate the doses of the thyroid product and the oral calcium supplement by at least 4 hours. Consider therapy modification
Trientine: Polyvalent Cation Containing Products may decrease the serum concentration of Trientine. Management: Avoid concomitant administration of trientine and oral products that contain polyvalent cations. If oral iron supplements are required, separate the administration by 2 hours. If other oral polyvalent cations are needed, separate administration by 1 hour. Consider therapy modification
Velpatasvir: Antacids may decrease the serum concentration of Velpatasvir. Management: Separate administration of velpatasvir and antacids by at least 4 hours. Consider therapy modification
Vitamin D Analogs: Calcium Salts may enhance the adverse/toxic effect of Vitamin D Analogs. Monitor therapy
Adverse Reactions
Well tolerated
1% to 10%:
Central nervous system: Headache, laxative effect
Endocrine & metabolic: Hypercalcemia, hypophosphatemia, milk-alkali syndrome (with very high, chronic dosing and/or renal failure [headache, nausea, irritability, and weakness or alkalosis, hypercalcemia, renal impairment])
Gastrointestinal: Abdominal pain, anorexia, constipation, flatulence, hyperacidity (acid rebound), nausea, vomiting, xerostomia
Warnings/Precautions
Concerns related to adverse effects:
- Gastrointestinal effects: Constipation, bloating, and gas are common with calcium supplements (especially carbonate salt) (IOM 2011).
- Hypercalcemia: Chronic hypercalcemia may result in generalized vascular and soft tissue calcification, exacerbate nephrolithiasis, and has been associated with increased mortality in adults with chronic kidney disease (CKD) (KDIGO 2017).
Disease-related concerns:
- Achlorhydria: Calcium absorption is impaired in achlorhydria; administration is followed by increased gastric acid secretion within 2 hours of administration especially with high doses. Common in the elderly, use an alternate salt (eg, citrate) and administer with food (IOM 2011; Recker 1985).
- Chronic kidney disease: In CKD patients receiving phosphate-lowering treatment, consider using non-calcium-based phosphate-lowering agents (eg, sevelamer, lanthanum) as an alternative to calcium-based phosphate-lowering agents (eg, calcium acetate, calcium carbonate) or restricting the dose of the calcium-based phosphate-lowering agents (Allison 2013; KDIGO 2017). A meta-analysis observed a trend towards a decrease in all-cause mortality in CKD patients receiving non-calcium-based phosphate-lowering agents compared with those receiving calcium-based phosphate-lowering agents (Jamal 2013); however, further research is needed to identify causes of mortality and fully assess safety of long-term use based on phosphate-lowering agent type.
- Hypoparathyroid disease: Hypercalcemia and hypercalciuria are most likely to occur in hypoparathyroid patients receiving high doses of vitamin D.
- Kidney stones (calcium-containing): Use caution when administering calcium supplements to patients with a history of kidney stones (IOM 2011).
- Renal insufficiency: Use with caution as these patients are more sensitive or susceptible to the effects of excess calcium (IOM 2011).
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Other warnings/precautions:
- Appropriate product selection: Multiple salt forms of calcium exist; close attention must be paid to the salt form when ordering and administering calcium; incorrect selection or substitution of one salt for another without proper dosage adjustment may result in serious over or under dosing.
Monitoring Parameters
Monitor plasma calcium levels if using calcium salts as electrolyte supplements for deficiency.
Calcium supplementation in hypoparathyroidism (Endocrine Society [Brandi 2016]): Note: Frequency of measurement is dependent upon on how stable a patient is to a given dosage regimen with more frequent measurements (eg, weekly) required initially during dosage titration. Once patient is well controlled, monitoring may be required on a yearly or twice-yearly basis.
Serum calcium, phosphate, and magnesium; renal function (ie, 24-hour urinary calcium and creatinine, blood urea nitrogen [BUN]), measured CrCl or estimated glomerular filtration rate (eGFR); renal imaging (every 5 years in asymptomatic patients with a history of renal lithiasis or calcinosis or more frequently as indicated); CNS imaging (basal ganglia and other sites of calcification), ophthalmologic exam, and/or BMD as clinically indicated
Hyperphosphatemia in Chronic Kidney Disease:
CKD stage G3a to G3b: Serum calcium and phosphate: Every 6 to 12 months; PTH: Frequency based on baseline level and progression of CKD
CKD stage G4: Serum calcium and phosphate: Every 3 to 6 months; PTH: Every 6 to 12 months
CKD stage G5 and G5D: Serum calcium and phosphate: Every 1 to 3 months; PTH: Every 3 to 6 months
Pregnancy
Pregnancy Considerations
Calcium crosses the placenta (IOM 2011).
Calcium is required for fetal growth. Intestinal absorption and urinary excretion of calcium increase during pregnancy. The amount of calcium reaching the fetus is determined by maternal physiological changes which are generally not influenced by maternal diet or supplementation (IOM 2011; Prentice 2000).
Calcium requirements are the same in pregnant and nonpregnant females; the recommended dietary allowance (RDA) is not increased in pregnancy (IOM 2011). When used as an antacid, most calcium-containing products are considered acceptable for use in pregnancy in recommended doses (Richter [ACG 2007]). Chronic use of high doses of calcium carbonate as an antacid throughout pregnancy may lead to hypocalcemia and seizures in the neonate (Borkenhagen 2013; Robertson 2002) or severe hypercalcemia presenting as milk-alkali syndrome in the mother (D’Souza 2013; Gordon 2005; Kolnick 2011; Picolos 2004; Trezevant 2017).
Patient Education
What is this drug used for?
- It is used to treat heartburn and upset stomach.
- It is used to treat or prevent low calcium levels.
- It may be given to you for other reasons. Talk with the doctor.
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Severe constipation
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.