Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Capsule, Oral, as hydrochloride:
Allergy Relief: 10 mg
ZyrTEC Allergy: 10 mg
Solution, Oral, as hydrochloride:
All Day Allergy Childrens: 5 mg/5 mL (118 mL [DSC]) [contains methylparaben, propylene glycol, propylparaben]
All Day Allergy Childrens: 5 mg/5 mL (118 mL [DSC]) [dye free, gluten free; contains methylparaben, propylene glycol, propylparaben; grape flavor]
Allergy Relief Childrens: 5 mg/5 mL (118 mL) [dye free, sugar free; contains propylene glycol, sodium benzoate; grape flavor]
Cetirizine HCl Allergy Child: 5 mg/5 mL (120 mL) [alcohol free, dye free, gluten free, sugar free; contains methylparaben, propylene glycol, propylparaben; grape flavor]
Cetirizine HCl Allergy Child: 5 mg/5 mL (120 mL) [alcohol free, sugar free; contains methylparaben, propylene glycol, propylparaben]
Cetirizine HCl Allergy Child: 5 mg/5 mL (118 mL) [dye free, gluten free, sugar free; contains propylene glycol, sodium benzoate; grape flavor]
Cetirizine HCl Childrens: 5 mg/5 mL (118 mL) [contains methylparaben, propylene glycol, propylparaben]
Cetirizine HCl Childrens Alrgy: 5 mg/5 mL (118 mL, 120 mL) [contains methylparaben, propylene glycol, propylparaben; grape flavor]
Cetirizine HCl Hives Relief: 5 mg/5 mL (120 mL) [alcohol free, sugar free; contains methylparaben, propylene glycol, propylparaben; grape flavor]
GoodSense All Day Allergy: 5 mg/5 mL (118 mL) [dye free, gluten free, sugar free; contains propylene glycol, sodium benzoate, sorbitol]
ZyrTEC Childrens Allergy: 5 mg/5 mL (118 mL) [dye free, sugar free; contains propylene glycol, sodium benzoate]
ZyrTEC Childrens Allergy: 5 mg/5 mL (118 mL) [dye free, sugar free; contains propylene glycol, sodium benzoate; grape flavor]
Generic: 5 mg/5 mL (120 mL, 473 mL, 480 mL)
Tablet, Oral, as hydrochloride:
All Day Allergy: 10 mg [contains corn starch]
Allergy Relief Cetirizine: 10 mg
Allergy Relief/Indoor/Outdoor: 10 mg [scored]
GoodSense All Day Allergy: 10 mg [contains corn starch, fd&c blue #1 aluminum lake]
ZyrTEC Allergy: 10 mg
Generic: 5 mg, 10 mg
Tablet Chewable, Oral, as hydrochloride:
All Day Allergy Childrens: 10 mg [DSC] [tutti-frutti flavor]
Cetirizine HCl Childrens: 5 mg, 10 mg [contains aspartame, fd&c yellow #6 aluminum lake]
Generic: 5 mg, 10 mg
Tablet Disintegrating, Oral, as hydrochloride:
ZyrTEC Allergy: 10 mg
ZyrTEC Allergy Childrens: 10 mg
ZyrTEC Allergy Childrens: 10 mg [citrus flavor]
Pharmacology
Mechanism of Action
Competes with histamine for H1-receptor sites on effector cells in the gastrointestinal tract, blood vessels, and respiratory tract
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid
Distribution
Children: 0.7 L/kg ; Adults: 0.56 L/kg (Simons 1999)
Metabolism
Limited hepatic
Excretion
Urine (70%; 50% as unchanged drug); feces (10%)
Onset of Action
Suppression of skin wheal and flare: Oral: 20 to 60 minutes.
Time to Peak
Serum: Oral: 1 hour; IV: 108 seconds.
Duration of Action
Suppression of skin wheal and flare: Oral: ≥24 hours.
Half-Life Elimination
Children: 6.2 hours; Adults: 8 hours
Protein Binding
Plasma: Mean: 93%
Use: Labeled Indications
Oral:
Allergic rhinitis: Relief of symptoms associated with allergic rhinitis.
Urticaria, chronic spontaneous: Treatment of uncomplicated skin manifestations of chronic spontaneous urticaria.
Injection:
Urticaria, acute: Treatment of acute urticaria.
Use: Off Label
Anaphylaxis (adjunct to epinephrine for relief of cutaneous symptoms)yes
Based on joint guidelines from the American Academy of Allergy, Asthma & Immunology, American College of Allergy, Asthma & Immunology, and Joint Council of Allergy, Asthma and Immunology on the diagnosis and management of anaphylaxis and guidelines from the World Allergy Organization on anaphylaxis, cetirizine may be used as adjunctive treatment, although should not be used as monotherapy or as first-line therapy of anaphylaxis.
Angioedema, acute allergic or recurrent idiopathicc
Clinical experience suggests the utility of second-generation H1 receptor antagonists (eg, cetirizine) for the treatment of acute allergic or recurrent idiopathic angioedema Cicardi 2014, James 2017.
Infusion reaction, premedicationc
Clinical experience suggests the utility of second-generation H1 receptor antagonists (eg, cetirizine) as an adjunct to premedication prior to the infusion of certain chemotherapy agents (eg, certain taxanes) or biologics to prevent infusion reactions Castells 2019, Durham 2018, Kirkham 2019.
Contraindications
Hypersensitivity to cetirizine, hydroxyzine, levocetirizine, or any component of the formulation.
Canadian labeling: Additional contraindications (not in US labeling): Hypersensitivity to piperazine derivatives; severe renal impairment (CrCl <10 mL/minute).
Dosage and Administration
Dosing: Adult
Allergic rhinitis or conjunctivitis: Oral: 10 mg once daily; alternatively, may be given as needed 2 to 5 hours before exposure to allergen, although this may be less effective than daily administration (deShazo 2019).
OTC labeling (patient-guided therapy for symptoms of hay fever or other upper respiratory allergies): 5 to 10 mg once daily (maximum: 10 mg/day).
Anaphylaxis (adjunct to epinephrine for relief of cutaneous symptoms) (off-label use): Note: Do not use for initial or sole treatment of anaphylaxis because H1 antihistamines do not relieve upper or lower airway obstruction or shock (AAAAI/ACAAI/JCAAI [Lieberman 2015]; Sheikh 2007; WAO [Simons 2011]; WAO [Simons 2015]).
Oral: 10 mg as a single dose (AAAAI/ACAAI/JCAAI [Lieberman 2015]; WAO [Simons 2011]).
Angioedema, acute allergic or recurrent idiopathic (off-label use): Note: Not indicated for angioedema with anaphylaxis; use epinephrine if anaphylaxis symptoms are present (ie, risk of airway or cardiovascular compromise is present) (James 2017; Zuraw 2019).
Oral: 10 mg once or twice daily; may increase up to 20 mg twice daily (Cicardi 2014; James 2017; Zuraw 2019).
Infusion reaction, premedication (adjunct) (alternative agent) (off-label use): Note: Used in some protocols as an alternative to a sedating antihistamine (eg, diphenhydramine). An optimal premedication regimen has not been identified; refer to institutional protocols as variations exist (Castells 2019; Durham 2018; Kirkham 2019).
Oral: 10 mg typically administered 30 to 60 minutes prior to infusion of certain chemotherapy agents or biologics; may be given with an H2 antihistamine (eg, ranitidine) and/or a glucocorticoid (Castells 2019; Durham 2018).
Urticaria (acute and chronic spontaneous):
Acute:
Oral (off-label use): Initial: 10 mg once daily. If symptom control is inadequate, may increase to 10 mg twice daily (Asero 2020; Zuberbier 2018).
IV: 10 mg once daily as needed; switch to scheduled oral dosing when feasible.
Chronic spontaneous:
Oral: Initial: 10 mg once daily. If symptom control is inadequate, may increase in increments of 10 mg/day every 1 to 4 weeks up to 20 mg twice daily. Reevaluate necessity for continued treatment periodically (Khan 2020; Zuberbier 2018).
Dosing: Geriatric
Upper respiratory allergies, urticaria: Oral: 5 mg once daily (maximum dose: 5 mg daily). The previously available prescription product recommended a maximum dose of 10 mg once daily in patients <77 years of age or 5 mg once daily in patients ≥77 years of age (Zyrtec Prescribing Information, 2006).
Dosing: Pediatric
Allergic symptoms, hay fever:
Children 2 to 5 years: Oral: Initial: 2.5 mg once daily; dosage may be increased to 2.5 mg twice daily or 5 mg once daily; maximum daily dose: 5 mg/day.
Children ≥6 years and Adolescents: Oral: 5 to 10 mg once daily.
Anaphylaxis; adjunctive for cutaneous symptoms: Limited data available (Canadian Paediatric Society [Cheng 2011]): Note: Do not use for initial or sole treatment of anaphylaxis; H1 antihistamines are not effective for upper or lower airway obstruction or shock (AAAAI/ACAAI/JCAAI [Lieberman 2015]; WAO [Simons 2011]; WAO [Simons 2015]). If cutaneous symptoms persist, dose may be repeated in 24 hours (see Urticaria, acute dosing).
Infants ≥6 months and Children <2 years: Oral: 2.5 mg once.
Children 2 to 5 years: Oral 2.5 to 5 mg once.
Children >5 years and Adolescents: Oral: 5 to 10 mg once.
Rhinitis, allergic(perennial):
Infants 6 to <12 months: Oral: 2.5 mg once daily.
Children 12 to 23 months: Oral: Initial: 2.5 mg once daily; dosage may be increased to 2.5 mg twice daily.
Urticaria, acute:
IV:
Infants ≥6 months to Children ≤5 years: 2.5 mg every 24 hours.
Children 6 to 11 years: 5 mg or 10 mg every 24 hours; reserve higher dose for more severe symptoms.
Children ≥12 years and Adolescents: 10 mg every 24 hours.
Oral: Limited data available (Canadian Paediatric Society [Cheng 2011]):
Infants ≥6 months and Children <2 years: Oral: 2.5 mg once daily.
Children 2 to 5 years: Oral: 2.5 to 5 mg once daily.
Children >5 years and Adolescents: Oral: 5 to 10 mg once daily.
Urticaria, chronic: Limited data available in Children >5 years and Adolescents. Note: Considered first-line therapy for management of chronic urticaria; if response inadequate after 2 to 4 weeks of therapy or symptoms intolerable, consider increasing the dose of cetirizine (as age and weight permits) as second-line treatment rather than changing therapy (Zuberbier 2018).
Infants 6 to <12 months: Oral: 2.5 mg once daily.
Infants ≥12 months and Children <2 years: Oral: Initial: 2.5 mg once daily; dosage may be increased to 2.5 mg twice daily.
Children 2 to 5 years: Oral: Initial: 2.5 mg once daily; dosage may be increased to 2.5 mg twice daily or 5 mg once daily; maximum daily dose: 5 mg/day.
Children 6 to 11 years: Oral: 5 mg once daily or twice daily (Caffarelli 2019; Del Pozzo-Magaña 2017)
Children ≥12 years and Adolescents: Oral: 10 mg once daily (Caffarelli 2019; Del Pozzo-Magaña 2017)
Administration
Oral: May be administered with or without food.
Chewable tablet: Chew tablet before swallowing; may be taken with or without water.
IV: Injection: For IV use only; do not administer IM or SubQ; administer as an IV push over 1 to 2 minutes.
Storage
Capsule, tablet, oral solution, injection: Store at 20°C to 25°C (68°F to 77°F); excursions are permitted between 15°C and 30°C (59°F and 86°F).
Injection: Discard unused portion.
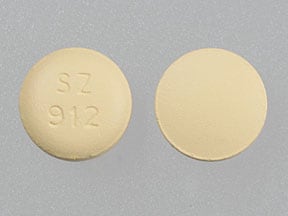
Cetirizine (Systemic) Images
Drug Interactions
Acetylcholinesterase Inhibitors: May diminish the therapeutic effect of Anticholinergic Agents. Anticholinergic Agents may diminish the therapeutic effect of Acetylcholinesterase Inhibitors. Monitor therapy
Aclidinium: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Alcohol (Ethyl): CNS Depressants may enhance the CNS depressant effect of Alcohol (Ethyl). Monitor therapy
Alizapride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Amantadine: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Amezinium: Antihistamines may enhance the stimulatory effect of Amezinium. Monitor therapy
Amphetamines: May diminish the sedative effect of Antihistamines. Monitor therapy
Anticholinergic Agents: May enhance the adverse/toxic effect of other Anticholinergic Agents. Monitor therapy
Azelastine (Nasal): CNS Depressants may enhance the CNS depressant effect of Azelastine (Nasal). Avoid combination
Benzylpenicilloyl Polylysine: Antihistamines may diminish the diagnostic effect of Benzylpenicilloyl Polylysine. Management: Suspend systemic H1 antagonists for benzylpenicilloyl-polylysine skin testing and delay testing until systemic antihistaminic effects have dissipated. A histamine skin test may be used to assess persistent antihistaminic effects. Consider therapy modification
Betahistine: Antihistamines may diminish the therapeutic effect of Betahistine. Monitor therapy
Blonanserin: CNS Depressants may enhance the CNS depressant effect of Blonanserin. Consider therapy modification
Botulinum Toxin-Containing Products: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Brexanolone: CNS Depressants may enhance the CNS depressant effect of Brexanolone. Monitor therapy
Brimonidine (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromopride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromperidol: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Buprenorphine: CNS Depressants may enhance the CNS depressant effect of Buprenorphine. Management: Consider reduced doses of other CNS depressants, and avoiding such drugs in patients at high risk of buprenorphine overuse/self-injection. Initiate buprenorphine at lower doses in patients already receiving CNS depressants. Consider therapy modification
Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Cannabis: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Chloral Betaine: May enhance the adverse/toxic effect of Anticholinergic Agents. Monitor therapy
Chlormethiazole: May enhance the CNS depressant effect of CNS Depressants. Management: Monitor closely for evidence of excessive CNS depression. The chlormethiazole labeling states that an appropriately reduced dose should be used if such a combination must be used. Consider therapy modification
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Cimetropium: Anticholinergic Agents may enhance the anticholinergic effect of Cimetropium. Avoid combination
CNS Depressants: May enhance the adverse/toxic effect of other CNS Depressants. Monitor therapy
Dimethindene (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Doxylamine: May enhance the CNS depressant effect of CNS Depressants. Management: The manufacturer of Diclegis (doxylamine/pyridoxine), intended for use in pregnancy, specifically states that use with other CNS depressants is not recommended. Monitor therapy
Dronabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Droperidol: May enhance the CNS depressant effect of CNS Depressants. Management: Consider dose reductions of droperidol or of other CNS agents (eg, opioids, barbiturates) with concomitant use. Exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Consider therapy modification
Eluxadoline: Anticholinergic Agents may enhance the constipating effect of Eluxadoline. Avoid combination
Erdafitinib: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Esketamine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Flunitrazepam: CNS Depressants may enhance the CNS depressant effect of Flunitrazepam. Consider therapy modification
Gastrointestinal Agents (Prokinetic): Anticholinergic Agents may diminish the therapeutic effect of Gastrointestinal Agents (Prokinetic). Monitor therapy
Glucagon: Anticholinergic Agents may enhance the adverse/toxic effect of Glucagon. Specifically, the risk of gastrointestinal adverse effects may be increased. Monitor therapy
Glycopyrrolate (Oral Inhalation): Anticholinergic Agents may enhance the anticholinergic effect of Glycopyrrolate (Oral Inhalation). Avoid combination
Glycopyrronium (Topical): May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Hyaluronidase: Antihistamines may diminish the therapeutic effect of Hyaluronidase. Management: Patients receiving antihistamines (particularly at larger doses) may not experience the desired clinical response to standard doses of hyaluronidase. Larger doses of hyaluronidase may be required. Consider therapy modification
HYDROcodone: CNS Depressants may enhance the CNS depressant effect of HYDROcodone. Management: Avoid concomitant use of hydrocodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
HydrOXYzine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Ipratropium (Oral Inhalation): May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Itopride: Anticholinergic Agents may diminish the therapeutic effect of Itopride. Monitor therapy
Kava Kava: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Lasmiditan: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Avoid combination
Lemborexant: May enhance the CNS depressant effect of CNS Depressants. Management: Dosage adjustments of lemborexant and of concomitant CNS depressants may be necessary when administered together because of potentially additive CNS depressant effects. Close monitoring for CNS depressant effects is necessary. Consider therapy modification
Levosulpiride: Anticholinergic Agents may diminish the therapeutic effect of Levosulpiride. Avoid combination
Lofexidine: May enhance the CNS depressant effect of CNS Depressants. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Lumacaftor and Ivacaftor: May decrease the serum concentration of P-glycoprotein/ABCB1 Substrates. Lumacaftor and Ivacaftor may increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Magnesium Sulfate: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Methotrimeprazine: CNS Depressants may enhance the CNS depressant effect of Methotrimeprazine. Methotrimeprazine may enhance the CNS depressant effect of CNS Depressants. Management: Reduce adult dose of CNS depressant agents by 50% with initiation of concomitant methotrimeprazine therapy. Further CNS depressant dosage adjustments should be initiated only after clinically effective methotrimeprazine dose is established. Consider therapy modification
MetyroSINE: CNS Depressants may enhance the sedative effect of MetyroSINE. Monitor therapy
Mianserin: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Minocycline (Systemic): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Mirabegron: Anticholinergic Agents may enhance the adverse/toxic effect of Mirabegron. Monitor therapy
Nabilone: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Nitroglycerin: Anticholinergic Agents may decrease the absorption of Nitroglycerin. Specifically, anticholinergic agents may decrease the dissolution of sublingual nitroglycerin tablets, possibly impairing or slowing nitroglycerin absorption. Monitor therapy
Opioid Agonists: CNS Depressants may enhance the CNS depressant effect of Opioid Agonists. Management: Avoid concomitant use of opioid agonists and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Orphenadrine: CNS Depressants may enhance the CNS depressant effect of Orphenadrine. Avoid combination
Oxatomide: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Oxomemazine: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
OxyCODONE: CNS Depressants may enhance the CNS depressant effect of OxyCODONE. Management: Avoid concomitant use of oxycodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Paraldehyde: CNS Depressants may enhance the CNS depressant effect of Paraldehyde. Avoid combination
Perampanel: May enhance the CNS depressant effect of CNS Depressants. Management: Patients taking perampanel with any other drug that has CNS depressant activities should avoid complex and high-risk activities, particularly those such as driving that require alertness and coordination, until they have experience using the combination. Consider therapy modification
P-glycoprotein/ABCB1 Inducers: May decrease the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inducers may also further limit the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Monitor therapy
P-glycoprotein/ABCB1 Inhibitors: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inhibitors may also enhance the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Monitor therapy
Pilsicainide: May increase the serum concentration of Cetirizine (Systemic). Cetirizine (Systemic) may increase the serum concentration of Pilsicainide. Monitor therapy
Piribedil: CNS Depressants may enhance the CNS depressant effect of Piribedil. Monitor therapy
Pitolisant: Antihistamines may diminish the therapeutic effect of Pitolisant. Avoid combination
Potassium Chloride: Anticholinergic Agents may enhance the ulcerogenic effect of Potassium Chloride. Management: Patients on drugs with substantial anticholinergic effects should avoid using any solid oral dosage form of potassium chloride. Avoid combination
Potassium Citrate: Anticholinergic Agents may enhance the ulcerogenic effect of Potassium Citrate. Avoid combination
Pramipexole: CNS Depressants may enhance the sedative effect of Pramipexole. Monitor therapy
Pramlintide: May enhance the anticholinergic effect of Anticholinergic Agents. These effects are specific to the GI tract. Consider therapy modification
Ramosetron: Anticholinergic Agents may enhance the constipating effect of Ramosetron. Monitor therapy
Ranolazine: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Revefenacin: Anticholinergic Agents may enhance the anticholinergic effect of Revefenacin. Avoid combination
ROPINIRole: CNS Depressants may enhance the sedative effect of ROPINIRole. Monitor therapy
Rotigotine: CNS Depressants may enhance the sedative effect of Rotigotine. Monitor therapy
Rufinamide: May enhance the adverse/toxic effect of CNS Depressants. Specifically, sleepiness and dizziness may be enhanced. Monitor therapy
Secretin: Anticholinergic Agents may diminish the therapeutic effect of Secretin. Management: Avoid concomitant use of anticholinergic agents and secretin. Discontinue anticholinergic agents at least 5 half-lives prior to administration of secretin. Consider therapy modification
Selective Serotonin Reuptake Inhibitors: CNS Depressants may enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk of psychomotor impairment may be enhanced. Monitor therapy
Sodium Oxybate: May enhance the CNS depressant effect of CNS Depressants. Management: Consider alternatives to combined use. When combined use is needed, consider minimizing doses of one or more drugs. Use of sodium oxybate with alcohol or sedative hypnotics is contraindicated. Consider therapy modification
Suvorexant: CNS Depressants may enhance the CNS depressant effect of Suvorexant. Management: Dose reduction of suvorexant and/or any other CNS depressant may be necessary. Use of suvorexant with alcohol is not recommended, and the use of suvorexant with any other drug to treat insomnia is not recommended. Consider therapy modification
Tapentadol: May enhance the CNS depressant effect of CNS Depressants. Management: Avoid concomitant use of tapentadol and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Tetrahydrocannabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Thalidomide: CNS Depressants may enhance the CNS depressant effect of Thalidomide. Avoid combination
Thiazide and Thiazide-Like Diuretics: Anticholinergic Agents may increase the serum concentration of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Tiotropium: Anticholinergic Agents may enhance the anticholinergic effect of Tiotropium. Avoid combination
Topiramate: Anticholinergic Agents may enhance the adverse/toxic effect of Topiramate. Monitor therapy
Trimeprazine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Umeclidinium: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Zolpidem: CNS Depressants may enhance the CNS depressant effect of Zolpidem. Management: Reduce the Intermezzo brand sublingual zolpidem adult dose to 1.75 mg for men who are also receiving other CNS depressants. No such dose change is recommended for women. Avoid use with other CNS depressants at bedtime; avoid use with alcohol. Consider therapy modification
Test Interactions
May cause false-positive serum TCA screen. May suppress the wheal and flare reactions to skin test antigens.
Adverse Reactions
>10%: Nervous system: Drowsiness (adults 14%; children 2% to 4%), headache (children 11% to 14%, placebo 12%)
2% to 10%:
Gastrointestinal: Abdominal pain (children 4% to 6%), xerostomia (adults 5%), diarrhea (children 2% to 3%), nausea (children 2% to 3%; placebo 2%), vomiting (children 2% to 3%)
Nervous system: Insomnia (children 9%; adults <2%), fatigue (adults 6%), malaise (4%), dizziness (adults 2%)
Respiratory: Pharyngitis (children 3% to 6%; placebo 3%), epistaxis (children 2% to 4%; placebo 3%), bronchospasm (children 2% to 3%; placebo 2%)
<2% (as reported in adults and/or children): Abnormality in thinking, accommodation disturbance, acne vulgaris, acute myocardial infarction, ageusia, alopecia, altered sense of smell, amnesia, anaphylaxis, angioedema, anorexia, anxiety, aphthous stomatitis, arthralgia, arthritis, asthenia, ataxia, back pain, blepharoptosis, blindness, bronchitis, bullous rash, cardiac failure, chest pain, cholestasis, confusion, conjunctivitis, constipation, cutaneous nodule, cystitis, deafness, decreased libido, dehydration, depersonalization, depression, dermatitis, dermatological disorders, diabetes mellitus, diaphoresis, dysgeusia, dysmenorrhea, dyspepsia, dyspnea, dysuria, eczema, edema, emotional lability, enlargement of abdomen, eructation, erythematous rash, euphoria, eye pain, facial edema, fever, flatulence, flushing, furunculosis, fussiness in an infant or toddler, gastritis, glaucoma, glomerulonephritis, heavy menstrual bleeding, hematuria, hemolytic anemia, hemophthalmos, hemorrhoids, hepatic insufficiency, hepatitis, hot flash, hyperesthesia, hyperkeratosis, hyperkinetic muscle activity, hypertension, hypertonia, hypertrichosis, hyperventilation, hypoesthesia, hypotension, increased appetite, increased bronchial secretions, increased liver enzymes (transient), increased serum bilirubin, increased thirst, intermenstrual bleeding, irritability, lack of concentration, leukorrhea, lower extremity edema, lower limb cramp, lymphadenopathy, maculopapular rash, mastalgia (female), melena, migraine, myalgia, myasthenia, myelitis, nasal polyposis, nervousness, nightmares, orofacial dyskinesia, osteoarthritis, otalgia, ototoxicity, pain, pallor, palpitations, paralysis, paresthesia, periorbital edema, pneumonia, polyuria, pruritus, purpuric disease, rectal hemorrhage, respiratory system disorder, rhinitis, rigors, seborrhea, sialorrhea, sinusitis, skin photosensitivity, skin rash, sleep disorder, stomatitis, syncope, tachycardia, thrombocytopenia, tinnitus, tongue discoloration, tongue edema, tremor, twitching, upper respiratory tract infection, urinary frequency, urinary incontinence, urinary retention, urinary tract infection, urticaria, vaginitis, vertigo, visual field defect, voice disorder, weight gain, xeroderma, xerophthalmia
Postmarketing and/or case reports: Aggressive behavior, convulsions, hallucination, hypotension (severe), suicidal ideation
Warnings/Precautions
Concerns related to adverse effects:
- CNS depression: May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks that require mental alertness (eg, operating machinery or driving).
Disease-related concerns:
- Hepatic impairment: Use with caution.
- Renal impairment: Use with caution; consider dosage adjustment.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
- Sedatives: Effects may be potentiated when used with other sedative drugs or ethanol.
Special populations:
- Elderly: Use with caution in elderly patients; may be more sensitive to adverse effects.
Monitoring Parameters
Relief of symptoms, sedation and anticholinergic effects
Pregnancy
Pregnancy Considerations
Guidelines for the use of antihistamines in the treatment of allergic rhinitis or urticaria in pregnancy are generally the same as in nonpregnant females. Cetirizine may be used when a second generation antihistamine is needed. The lowest effective dose should be used (Powell 2015; Scadding 2017; Wallace 2008; Zuberbier 2018).
Patient Education
What is this drug used for?
- It is used to ease allergy signs.
- It is used to treat hives.
Frequently reported side effects of this drug
- Fatigue
- Dry mouth
- Loss of strength and energy
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.