Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral, as phosphate:
Generic: 250 mg [equivalent to chloroquine base 150 mg], 500 mg [equivalent to chloroquine base 300 mg]
Pharmacology
Mechanism of Action
Binds to and inhibits DNA and RNA polymerase; interferes with metabolism and hemoglobin utilization by parasites; inhibits prostaglandin effects; chloroquine concentrates within parasite acid vesicles and raises internal pH resulting in inhibition of parasite growth; may involve aggregates of ferriprotoporphyrin IX acting as chloroquine receptors causing membrane damage; may also interfere with nucleoprotein synthesis
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid and almost complete
Distribution
Widely in body tissues including eyes, heart, kidneys, liver, leukocytes, and lungs where retention is prolonged
Metabolism
Partially hepatic to main metabolite, desethylchloroquine
Excretion
Urine (~70%; ~35% as unchanged drug); acidification of urine increases elimination; small amounts of drug may be present in urine months following discontinuation of therapy
Time to Peak
Serum: Oral: Within 1-2 hours
Half-Life Elimination
3 to 5 days
Protein Binding
~55%
Use: Labeled Indications
Malaria: Treatment of uncomplicated malaria due to susceptible strains of Plasmodium vivax, Plasmodium malariae, Plasmodium ovale, and Plasmodium falciparum; prophylaxis of malaria (in geographic areas where chloroquine resistance is not present).
Limitations of use: Chloroquine does not prevent relapses in patients with vivax or ovale malaria (not effective against exoerythrocytic forms). Do not use for the treatment of complicated malaria (high-grade parasitemia and/or complications [eg, cerebral malaria, acute renal failure]) or for malaria prophylaxis in areas where chloroquine resistance occurs (resistance to chloroquine is widespread in P. falciparum and reported in P. vivax).
Extraintestinal amebiasis: Treatment of extraintestinal amebiasis.
Use: Off Label
Discoid lupus erythematosusb
Data from a prospective, randomized, controlled, double-blind clinical trial supports the use of chloroquine in the treatment of discoid lupus erythematosus Bezerra 2005. Chloroquine also demonstrated a reduction in epidermal vascular endothelial growth factor (VEGF) expression resulting in a significant reduction in the median number of CD34+ dermal blood vessels Lesiak 2009. Additional data may be necessary to further define the role of chloroquine in the treatment of this condition.
Contraindications
Hypersensitivity to chloroquine, 4-aminoquinoline compounds, or any component of the formulation; the presence of retinal or visual field changes of any etiology (when used for indications other than acute malaria)
Dosage and Administration
Dosing: Adult
Note: Each 250 mg of chloroquine phosphate is equivalent to 150 mg of chloroquine base
Malaria chemoprophylaxis: Oral: 500 mg (300 mg base) weekly on the same day each week; begin 1 to 2 weeks prior to exposure; continue while in endemic area and for 4 weeks after leaving endemic area (CDC 2018)
Malaria treatment, uncomplicated: Oral: 1 g (600 mg base) on day 1, followed by 500 mg (300 mg base) 6-, 24-, and 48 hours after first dose. Note: For treatment of chloroquine-sensitive P. vivax and P. ovale, concomitant therapy with an 8-aminoquinoline (eg, primaquine) is necessary (CDC 2013).
Extraintestinal amebiasis: Oral: 1 g (600 mg base) daily for 2 days followed by 500 mg daily (300 mg base) for at least 2 to 3 weeks; may be combined with an intestinal amebicide.
Lupus erythematosus (off-label use): Not considered first-line agent (Bezerra 2005; Lesiak 2008). Due to the risk of retinal toxicity, do not exceed a daily dose of 2.3 mg/kg/day of chloroquine phosphate using actual body weight; intermediate doses may be obtained by splitting tablets or eliminating a tablet on certain days of the week (AAO [Marmor 2016]).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Dosage expressed as chloroquine phosphate. Chloroquine phosphate 16.6 mg is equivalent to 10 mg chloroquine base.
Malaria:
Chemoprophylaxis: Infants, Children, and Adolescents: Oral: 8.3 mg/kg chloroquine phosphate once weekly on the same day each week; maximum dose: 500 mg chloroquine phosphate/dose. Begin 1 to 2 weeks prior to exposure; continue while in endemic area and continue for at least 4 weeks after leaving endemic area (CDC 2014); if suppressive therapy is delayed, double the initial loading dose (16.6 mg/kg, up to 1,000 mg chloroquine phosphate) and administer in 2 divided doses 6 hours apart; continue for 8 weeks after leaving endemic area
Treatment, acute attack, uncomplicated: Infants, Children, and Adolescents: Oral: Initial 16.6 mg/kg chloroquine phosphate (maximum initial dose: 1,000 mg chloroquine phosphate); followed by 8.3 mg/kg chloroquine phosphate (maximum dose: 500 mg chloroquine phosphate/dose) administered at 6, 24, and 48 hours after initial dose for a total of 4 doses (CDC 2013)
Extraintestinal amebiasis, liver abscess: Children and Adolescents: Limited data available: Oral: 16.6 mg/kg chloroquine phosphate/dose once daily in combination with metronidazole or tinidazole for 21 days followed by paromomycin or iodoquinol; maximum dose: 1,000 mg chloroquine phosphate/dose (Bradley 2015; Seidel 1984; Tony 1992)
Extemporaneously Prepared
16.67 mg chloroquine PHOSPHATE/mL (equivalent to 10 mg chloroquine BASE/mL) Oral Suspension (ASHP Standard Concentration) (ASHP 2017)
A 16.67 mg chloroquine PHOSPHATE/mL oral suspension (equivalent to 10 mg chloroquine BASE/mL) may be made from tablets. Crush two 500 mg chloroquine PHOSPHATE tablets (equivalent to 300 mg BASE/tablet) in a mortar and reduce to a fine powder. Add a small amount of sterile water for irrigation, USP and mix to a uniform paste; mix while adding cherry syrup in incremental proportions to almost 60 mL; transfer to a calibrated amber glass bottle, rinse mortar with cherry syrup, and add sufficient quantity of cherry syrup to make 60 mL. Label “shake well.” Stable for 4 weeks when stored at room temperature or refrigerated (Mirochnick 1994).
Mirochnick M, Barnett E, Clark DF, McNamara E, Cabral H. Stability of chloroquine in an extemporaneously prepared suspension stored at three temperatures. Pediatr Infect Dis J. 1994;13(9):827-828.7808855
15 mg chloroquine PHOSPHATE/mL (equivalent to 9 mg chloroquine BASE/mL) Oral Suspension
A 15 mg chloroquine PHOSPHATE/mL oral suspension (equivalent to 9 mg chloroquine BASE/mL) may be made from tablets and a 1:1 mixture of Ora-Sweet and Ora-Plus. Crush three 500 mg chloroquine PHOSPHATE tablets (equivalent to 300 mg BASE/tablet) in a mortar and reduce to a fine powder. Add 15 mL of the vehicle and mix to a uniform paste; mix while adding the vehicle in incremental proportions to almost 100 mL; transfer to a calibrated bottle, rinse mortar with vehicle, and add quantity of vehicle sufficient to make 100 mL. Label “shake well before using” and “protect from light”. Stable for up to 60 days when stored in the dark at room temperature or refrigerated (preferred).
Allen LV Jr, Erickson MA 3rd. Stability of Alprazolam, Chloroquine Phosphate, Cisapride, Enalapril Maleate, and Hydralazine Hydrochloride in Extemporaneously Compounded Oral Liquids. Am J Health Syst Pharm. 1998;55(18):1915-1920.9784772
Storage
Store at 25°C (77°F); excursions are permitted between 15°C and 30°C (59°F and 86°F); protect from light.
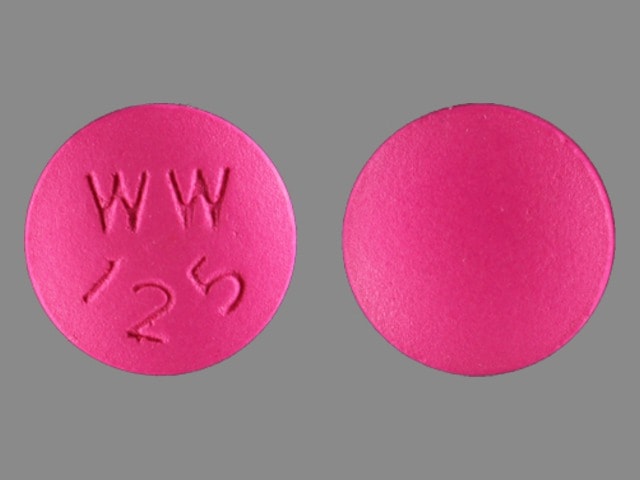
Chloroquine Images
Drug Interactions
Abiraterone Acetate: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Management: Avoid concurrent use of abiraterone with CYP2D6 substrates that have a narrow therapeutic index whenever possible. When concurrent use is not avoidable, monitor patients closely for signs/symptoms of toxicity. Consider therapy modification
Agalsidase Alfa: Chloroquine may diminish the therapeutic effect of Agalsidase Alfa. Avoid combination
Agalsidase Beta: Chloroquine may diminish the therapeutic effect of Agalsidase Beta. Avoid combination
Ampicillin: Chloroquine may decrease the serum concentration of Ampicillin. Management: Chloroquine prescribing information recommends separating administration of ampicillin and chloroquine by at least 2 hours to minimize any potential negative impact of chloroquine on ampicillin bioavailability. Consider therapy modification
Androgens: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Exceptions: Danazol. Monitor therapy
Antacids: May decrease the serum concentration of Chloroquine. Management: Separate administration of antacids and chloroquine by at least 4 hours to minimize any potential negative impact of antacids on chloroquine bioavailability. Consider therapy modification
Antidiabetic Agents: May enhance the hypoglycemic effect of Hypoglycemia-Associated Agents. Monitor therapy
Antipsychotic Agents (Phenothiazines): Antimalarial Agents may increase the serum concentration of Antipsychotic Agents (Phenothiazines). Monitor therapy
Aprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Artemether: May enhance the adverse/toxic effect of Antimalarial Agents. Management: Artemether/Lumefantrine (combination product) should not be used with other antimalarials unless there is no other treatment option. Avoid combination
Asunaprevir: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Consider therapy modification
Bacampicillin: Chloroquine may decrease the serum concentration of Bacampicillin. Management: Chloroquine prescribing information recommends separating administration of ampicillin and chloroquine by at least 2 hours to minimize any potential negative impact of chloroquine on ampicillin bioavailability. Bacampicillin is a prodrug of ampicillin. Consider therapy modification
Beta-Blockers: Aminoquinolines (Antimalarial) may decrease the metabolism of Beta-Blockers. Exceptions: Atenolol; Carteolol (Ophthalmic); Levobunolol; Metipranolol; Nadolol; Sotalol. Monitor therapy
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Cardiac Glycosides: Aminoquinolines (Antimalarial) may increase the serum concentration of Cardiac Glycosides. Monitor therapy
Cholera Vaccine: Chloroquine may diminish the therapeutic effect of Cholera Vaccine. Management: Administer cholera vaccine at least 10 days prior to initiation of chloroquine. Consider therapy modification
Cimetidine: May increase the serum concentration of Chloroquine. Monitor therapy
CloBAZam: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Clofazimine: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
CYP2D6 Inhibitors (Moderate): May decrease the metabolism of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
CYP2D6 Inhibitors (Strong): May decrease the metabolism of CYP2D6 Substrates (High risk with Inhibitors). Consider therapy modification
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May increase the metabolism of CYP3A4 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
CYP3A4 Inhibitors (Moderate): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CYP3A4 Inhibitors (Strong): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Consider therapy modification
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dacomitinib: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Management: Avoid concurrent use of dacomitinib with CYP2D6 subtrates that have a narrow therapeutic index. Consider therapy modification
Dapsone (Systemic): Antimalarial Agents may enhance the adverse/toxic effect of Dapsone (Systemic). Specifically, concomitant use of antimalarial agents with dapsone may increase the risk of hemolytic reactions. Dapsone (Systemic) may enhance the adverse/toxic effect of Antimalarial Agents. Specifically, concomitant use of dapsone with antimalarial agents may increase the risk for hemolytic reactions. Management: Closely monitor patients for signs/symptoms of hemolytic reactions with concomitant use of dapsone and antimalarial agents, particularly in patients deficient in glucose-6-phosphate dehydrogenase (G6PD), methemoglobin reductase, or with hemoglobin M. Consider therapy modification
Dapsone (Topical): Antimalarial Agents may enhance the adverse/toxic effect of Dapsone (Topical). Specifically, the risk of hemolytic reactions may be increased. Management: Closely monitor for signs/symptoms of hemolytic reactions with concomitant use of topical dapsone and antimalarial agents. Patients with glucose-6-phosphate dehydrogenase deficiency may be at particularly high risk for adverse hematologic effects. Consider therapy modification
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Domperidone: QT-prolonging Agents (Moderate Risk) may enhance the QTc-prolonging effect of Domperidone. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Duvelisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fexinidazole [INT]: May enhance the QTc-prolonging effect of QT-prolonging Agents (Moderate Risk). Avoid combination
Fosaprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosnetupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Haloperidol: QT-prolonging Miscellaneous Agents (Moderate Risk) may enhance the QTc-prolonging effect of Haloperidol. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Herbs (Hypoglycemic Properties): May enhance the hypoglycemic effect of Hypoglycemia-Associated Agents. Monitor therapy
Hypoglycemia-Associated Agents: May enhance the hypoglycemic effect of other Hypoglycemia-Associated Agents. Monitor therapy
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Imatinib: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Kaolin: May decrease the serum concentration of Chloroquine. Management: Separate administration of kaolin and chloroquine by at least 4 hours to minimize any potential negative impact of kaolin on chloroquine bioavailability. Consider therapy modification
Lanthanum: May decrease the serum concentration of Chloroquine. Management: Administer chloroquine at least two hours before or after lanthanum. Consider therapy modification
Larotrectinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Local Anesthetics: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Local Anesthetics. Specifically, the risk for methemoglobinemia may be increased. Monitor therapy
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Lumefantrine: Antimalarial Agents may enhance the adverse/toxic effect of Lumefantrine. Management: Artemether/Lumefantrine (combination product) should not be used with other antimalarials unless there is no other treatment option. Avoid combination
Maitake: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Mefloquine: Aminoquinolines (Antimalarial) may enhance the adverse/toxic effect of Mefloquine. Specifically, the risk for QTc-prolongation and the risk for convulsions may be increased. Mefloquine may increase the serum concentration of Aminoquinolines (Antimalarial). Management: Avoid concurrent use, and delay administration of mefloquine until at least 12 hours after the last dose of an aminoquinoline antimalarial when possible. Avoid combination
MiFEPRIStone: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Minimize doses of CYP3A4 substrates, and monitor for increased concentrations/toxicity, during and 2 weeks following treatment with mifepristone. Avoid cyclosporine, dihydroergotamine, ergotamine, fentanyl, pimozide, quinidine, sirolimus, and tacrolimus. Consider therapy modification
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Monoamine Oxidase Inhibitors: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Netupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Nitric Oxide: May enhance the adverse/toxic effect of Methemoglobinemia Associated Agents. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Monitor therapy
Ondansetron: QT-prolonging Miscellaneous Agents (Moderate Risk) may enhance the QTc-prolonging effect of Ondansetron. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Panobinostat: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Peginterferon Alfa-2b: May decrease the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Peginterferon Alfa-2b may increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Pegvisomant: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Pentamidine (Systemic): QT-prolonging Miscellaneous Agents (Moderate Risk) may enhance the QTc-prolonging effect of Pentamidine (Systemic). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Perhexiline: CYP2D6 Substrates (High risk with Inhibitors) may increase the serum concentration of Perhexiline. Perhexiline may increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Pimozide: May enhance the QTc-prolonging effect of QT-prolonging Agents (Moderate Risk). Avoid combination
Praziquantel: Chloroquine may decrease the serum concentration of Praziquantel. Monitor therapy
Prilocaine: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Prilocaine. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Management: Monitor patients for signs of methemoglobinemia (e.g., hypoxia, cyanosis) when prilocaine is used in combination with other agents associated with development of methemoglobinemia. Avoid lidocaine/prilocaine in infants receiving such agents. Monitor therapy
Primaquine: Chloroquine may increase the serum concentration of Primaquine. Monitor therapy
Prothionamide: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
QT-prolonging Agents (Highest Risk): May enhance the QTc-prolonging effect of Chloroquine. Management: Consider alternatives to this combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
QT-prolonging Antidepressants (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Miscellaneous Agents (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Antipsychotics (Moderate Risk): QT-prolonging Miscellaneous Agents (Moderate Risk) may enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Pimozide. Monitor therapy
QT-prolonging Class IC Antiarrhythmics (Moderate Risk): QT-prolonging Miscellaneous Agents (Moderate Risk) may enhance the QTc-prolonging effect of QT-prolonging Class IC Antiarrhythmics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Kinase Inhibitors (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Miscellaneous Agents (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Miscellaneous Agents (Moderate Risk): May enhance the QTc-prolonging effect of Chloroquine. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Domperidone. Monitor therapy
QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Miscellaneous Agents (Moderate Risk). QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of QT-prolonging Miscellaneous Agents (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Quinolone Antibiotics (Moderate Risk): QT-prolonging Miscellaneous Agents (Moderate Risk) may enhance the QTc-prolonging effect of QT-prolonging Quinolone Antibiotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Strong CYP3A4 Inhibitors (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Miscellaneous Agents (Moderate Risk). QT-prolonging Strong CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of QT-prolonging Miscellaneous Agents (Moderate Risk). Avoid combination
Quinolones: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Quinolones may diminish the therapeutic effect of Blood Glucose Lowering Agents. Specifically, if an agent is being used to treat diabetes, loss of blood sugar control may occur with quinolone use. Monitor therapy
Rabies Vaccine: Chloroquine may diminish the therapeutic effect of Rabies Vaccine. Monitor therapy
Salicylates: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Selective Serotonin Reuptake Inhibitors: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Sodium Nitrite: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Sodium Nitrite. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Monitor therapy
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
Tamoxifen: May enhance the adverse/toxic effect of Chloroquine. Specifically, concomitant use of tamoxifen and chloroquine may increase the risk of retinal toxicity. Monitor therapy
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Adverse Reactions
Frequency not defined.
Cardiovascular: Atrioventricular block, bundle branch block, cardiac arrhythmia, cardiomyopathy, ECG changes (including prolonged QRS and QTc intervals, T-wave inversion, or depression), hypotension, torsades de pointes, ventricular fibrillation, ventricular tachycardia
Central nervous system: Agitation, anxiety, confusion, decreased deep tendon reflex, delirium, depression, extrapyramidal reaction (dystonia, dyskinesia, protrusion of the tongue, torticollis), hallucination, headache, insomnia, motor dysfunction (sensorimotor disorder), personality changes, polyneuropathy, psychosis, seizure, suicidal tendencies
Dermatologic: Alopecia, bleaching of hair, blue gray skin pigmentation, erythema multiforme, exacerbation of psoriasis, exfoliative dermatitis, lichen planus, pleomorphic rash, pruritus, skin photosensitivity, Stevens-Johnson syndrome, toxic epidermal necrolysis, urticaria
Endocrine & metabolic: Hypoglycemia
Gastrointestinal: Abdominal cramps, anorexia, diarrhea, nausea, vomiting
Hematologic & oncologic: Agranulocytosis (reversible), aplastic anemia, hemolytic anemia (in G6PD-deficient patients), neutropenia, pancytopenia, thrombocytopenia
Hepatic: Hepatitis, increased liver enzymes
Hypersensitivity: Anaphylactoid reaction, anaphylaxis, angioedema
Immunologic: DRESS syndrome
Neuromuscular & skeletal: Myopathy, neuromuscular disease, proximal myopathy
Ophthalmic: Accommodation disturbances, blurred vision, corneal opacity (reversible), macular degeneration (may be irreversible), maculopathy (may be irreversible), nocturnal amblyopia, retinopathy (including irreversible changes in some patients' long-term or high-dose therapy), transient scotomata, visual field defects
Otic: Deafness (nerve), hearing loss (risk increased in patients with preexisting auditory damage), tinnitus
Warnings/Precautions
Concerns related to adverse effects:
- Cardiovascular effects: Cases of cardiomyopathy resulting in cardiac failure (sometimes fatal) have been reported during long term therapy at high doses. Monitor for signs and symptoms of cardiomyopathy; discontinue if cardiomyopathy develops. Consider chronic toxicity and discontinue chloroquine if conduction disorders (bundle branch block/AV block) are diagnosed. QT prolongation, torsade de pointes, and ventricular arrhythmias (some fatal) have been reported; risk is increased with high doses. Use with caution in patients with cardiac disease, history of ventricular arrhythmias, uncorrected hypokalemia and/or hypomagnesemia, or bradycardia, and during concomitant administration with QT interval prolonging agents due to potential for QT prolongation. In a scientific statement from the American Heart Association, chloroquine has been determined to be an agent that may either cause direct myocardial toxicity or exacerbate underlying myocardial dysfunction (magnitude: major) (AHA [Page 2016]).
- Extrapyramidal effects: Acute extrapyramidal disorders may occur, usually resolving after discontinuation of therapy and/or symptomatic treatment.
- Hematologic effects: Rare hematologic reactions including reversible agranulocytosis, aplastic anemia, neutropenia, pancytopenia, and thrombocytopenia have been reported; monitor CBC during prolonged therapy. Consider discontinuation if severe blood disorders occur that are unrelated to disease.
- Hypoglycemia: Severe hypoglycemia, including loss of consciousness, has been reported in patients treated with or without antidiabetic agents. Counsel patients about risk of hypoglycemia and associated signs and symptoms.
- Neuromuscular effects: Skeletal muscle myopathy or neuromyopathy, leading to progressive weakness and atrophy of proximal muscle groups have been reported; muscle strength (especially proximal muscles) should be assessed periodically during prolonged therapy; discontinue therapy if weakness occurs.
- Retinal toxicity: Retinal toxicity, potentially causing irreversible retinopathy, is predominantly associated with high daily doses and a duration of >5 years of use of chloroquine or hydroxychloroquine in the treatment of rheumatic diseases. Other major risk factors include concurrent tamoxifen use, renal impairment, lower body weight, and potentially the presence of macular disease. Risk is most accurately assessed on the basis of duration of use relative to daily dose/body weight (Marmor [AAO 2016]; Melles 2014). Based on these risks, the American Academy of Ophthalmology (AAO) recommends not exceeding a daily chloroquine phosphate dosage of 2.3 mg/kg using actual body weight. Previous recommendations to use ideal body weight are no longer advised; very thin patients in particular were at increased risk for retinal toxicity using this practice. Current AAO guidelines do not specifically address dosing in obese patients. AAO also recommends baseline screening for retinal toxicity and annual screening beginning after 5 years of use (or sooner if major risk factors are present) (Marmor [AAO 2016]).
Disease-related concerns:
- Auditory damage: Use with caution in patients with preexisting auditory damage; discontinue immediately if hearing defects are noted.
- G6PD deficiency: Although the manufacturer’s labeling recommends chloroquine be used with caution in patients with G6PD deficiency due to a potential for hemolytic anemia, there is limited data to support this risk. Many experts consider chloroquine, when given in usual therapeutic doses to WHO Class II and III G6PD deficient patients, to probably be safe (Cappellini 2008; Glader 2017; Luzzatto 2016; Youngster 2010). Safety in Class I G6PD deficiency (ie, severe form of the deficiency associated with chronic hemolytic anemia) is generally unknown (Glader 2017). In a trial conducted in West Africa involving 74 G6PD deficient patients (predominantly Class III deficiency), there were no cases of hemolysis reported following exposure to usual doses of chloroquine (Mandi 2005). In addition, the ACR Rheumatology guidelines do not mention the need to evaluate G6PD levels prior to initiation of therapy (Singh 2015).
- Hepatic impairment: Use with caution in patients with hepatic impairment, alcoholism, or concurrent therapy with hepatotoxic agents.
- Porphyria: Use with caution in patients with porphyria; may exacerbate disease symptoms.
- Psoriasis: Use with caution in patients with psoriasis; may exacerbate disease symptoms.
- Seizure disorder: Use with caution in patients with a history of seizure disorder; may cause seizures.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Other warnings/precautions:
- Appropriate use: Chloroquine does not prevent relapses in patients with vivax or ovale malaria (not effective against exoerythrocytic forms); additional treatment with an antimalarial effective against these forms (eg, an 8-aminoquinoline) is required for the treatment of infections with P. vivax and P. ovale. Do not use for the treatment of complicated malaria (high-grade parasitemia and/or complications [eg, cerebral malaria, acute renal failure]).
- Chloroquine resistance: Chloroquine is not effective against chloroquine- or hydroxychloroquine-resistant strains of Plasmodium species. Chloroquine resistance is widespread in P. falciparum and is reported in P. vivax. Prior to initiation of chloroquine for prophylaxis, it should be determined if chloroquine is appropriate for use in the region to be visited; do not use for malaria prophylaxis in areas where chloroquine resistance occurs. Patients should be treated with another antimalarial if patient is infected with a resistant strain of plasmodia.
Monitoring Parameters
Evaluate neuromuscular function periodically during prolonged therapy. Periodic CBC in patients receiving prolonged therapy
Ophthalmologic exam at baseline (fundus examination within the first year plus visual fields and spectral-domain optical coherence tomography [SD OCT] if maculopathy is present) to screen for retinal toxicity, followed by annual screening beginning after 5 years of use (or sooner if major risk factors are present) (Marmor [AAO 2016]).
Pregnancy
Pregnancy Considerations
Chloroquine and its metabolites cross the placenta and can be detected in the cord blood and urine of the newborn infant (Akintonwa 1988; Essien 1982; Law 2008).
In one study, chloroquine and its metabolites were measurable in the cord blood 89 days (mean) after the last maternal dose (Law 2008). Chloroquine has not been found to increase the risk of adverse fetal events when used in recommended doses for malaria prophylaxis. However, malaria infection increases the risk of prematurity, spontaneous abortion, and stillbirth (CDC 2018).
Malaria infection in pregnant women may be more severe than in nonpregnant women and has a high risk of maternal and perinatal morbidity and mortality. Therefore, pregnant women and women who are likely to become pregnant are advised to avoid travel to malaria-risk areas. If travel cannot be avoided, chloroquine may be used as prophylaxis. Chloroquine is recommended for the treatment of pregnant women with uncomplicated malaria in chloroquine-sensitive regions; when caused by chloroquine-sensitive P. vivax or P. ovale, infected pregnant women should be maintained on chloroquine prophylaxis for the duration of their pregnancy (refer to current guidelines). Chloroquine may be used in all trimesters of pregnancy (CDC 2013; CDC 2018; Lalloo 2016). Due to pregnancy-induced physiologic changes, some pharmacokinetic properties of chloroquine may be altered (Chukwuani 2004; Fakeye 2002; Karunajeewa 2010; Lee 2008; Massele 1997; Salman 2017; Wilby 2011).
Patient Education
- Discuss specific use of drug and side effects with patient as it relates to treatment. (HCAHPS: During this hospital stay, were you given any medicine that you had not taken before? Before giving you any new medicine, how often did hospital staff tell you what the medicine was for? How often did hospital staff describe possible side effects in a way you could understand?)
- Patient may experience abdominal pain, abdominal cramps, lack of appetite, nausea, vomiting, headache, diarrhea, skin discoloration, hair discoloration, or hair loss. Have patient report immediately to prescriber signs of liver problems (dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin), signs of low blood sugar (dizziness, headache, fatigue, feeling weak, shaking, fast heartbeat, confusion, increased hunger, or sweating), blurred vision, vision changes, vision loss, eye pain, severe eye irritation, abnormal movements, agitation, seizures, trouble sleeping, confusion, behavioral changes, mood changes, sensing things that seem real but are not, trouble hearing, noise or ringing in the ears, muscle pain, muscle weakness, burning or numbness feeling, chills, sore throat, bruising, bleeding, signs of heart problems (cough or shortness of breath that is new or worse, swelling of the ankles or legs, abnormal heartbeat, weight gain of more than five pounds in 24 hours, dizziness, or passing out), severe loss of strength and energy, or signs of Stevens-Johnson syndrome/toxic epidermal necrolysis (red, swollen, blistered, or peeling skin [with or without fever]; red or irritated eyes; or sores in mouth, throat, nose, or eyes) (HCAHPS).
- Educate patient about signs of a significant reaction (eg, wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat). Note: This is not a comprehensive list of all side effects. Patient should consult prescriber for additional questions.
Intended Use and Disclaimer:Should not be printed and given to patients. This information is intended to serve as a concise initial reference for health care professionals to use when discussing medications with a patient. You must ultimately rely on your own discretion, experience, and judgment in diagnosing, treating, and advising patients.