Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Solution Reconstituted, Intravenous, as sodium [strength expressed as base]:
Sodium Diuril: 500 mg (1 ea)
Generic: 500 mg (1 ea)
Solution Reconstituted, Intravenous, as sodium [strength expressed as base, preservative free]:
Generic: 500 mg (1 ea)
Suspension, Oral:
Diuril: 250 mg/5 mL (237 mL) [contains alcohol, usp, benzoic acid, fd&c yellow #10 (quinoline yellow), methylparaben, propylparaben, saccharin sodium]
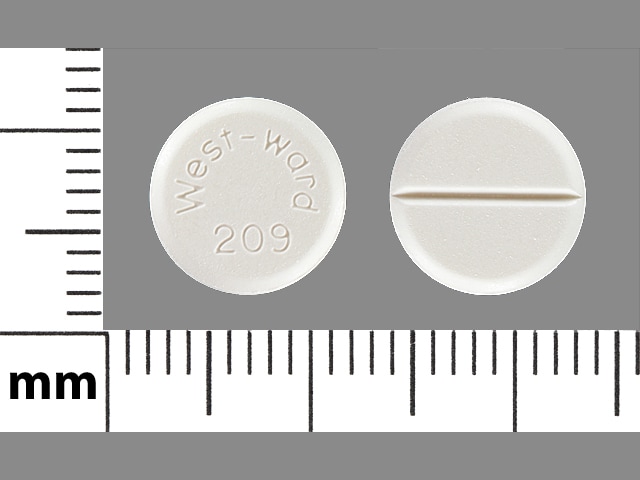
Tablet, Oral:
Generic: 250 mg, 500 mg
Pharmacology
Mechanism of Action
Inhibits sodium and chloride reabsorption in the distal tubules causing increased excretion of sodium, chloride, and water resulting in diuresis. Loss of potassium, hydrogen ions, magnesium, phosphate, and bicarbonate also occurs.
Pharmacokinetics/Pharmacodynamics
Absorption
Oral: Poor
Metabolism
Not metabolized
Excretion
Urine (10% to 15% [oral], 96% [IV] as unchanged drug)
Onset of Action
Diuresis: Oral: Within 2 hours; IV: 15 minutes; Peak effect: Oral: ~4 hours; IV: 30 minutes
Duration of Action
Diuretic action: Oral: ~6 to 12 hours; IV: 2 hours
Half-Life Elimination
45 to 120 minutes
Use: Labeled Indications
Edema: Adjunctive treatment of edema
Hypertension: Management of hypertension
Guideline recommendations: The 2017 Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults recommends if monotherapy is warranted, in the absence of comorbidities (eg, cerebrovascular disease, chronic kidney disease, diabetes, heart failure, ischemic heart disease, etc), that thiazide-like diuretics or dihydropyridine calcium channel blockers may be preferred options due to improved cardiovascular endpoints (eg, prevention of heart failure and stroke). ACE inhibitors and ARBs are also acceptable for monotherapy. Combination therapy may be required to achieve blood pressure goals and is initially preferred in patients at high risk (stage 2 hypertension or atherosclerotic cardiovascular disease [ASCVD] risk ≥10%) (ACC/AHA [Whelton 2017]).
Contraindications
Hypersensitivity to chlorothiazide, any component of the formulation or sulfonamide-derived drugs; anuria
Note: Although the FDA approved product labeling states this medication is contraindicated with other sulfonamide-containing drug classes, the scientific basis of this statement has been challenged. See “Warnings/Precautions” for more detail.
Dosage and Administration
Dosing: Adult
Note: The manufacturer states that IV and oral dosing are equivalent. Some clinicians may use lower IV doses; however, because of chlorothiazide's poor oral absorption.
Hypertension: Oral: 500 to 2,000 mg daily divided in 1 to 2 doses
Edema: Oral, IV:
ACCF/AHA 2013 heart failure guidelines:
Oral: 250 to 500 mg once or twice daily (maximum daily dose: 1,000 mg)
IV: 500 to 1,000 mg once daily in combination with a loop diuretic for sequential nephron blockade
Manufacturer’s labeling: Dosing in the prescribing information may not reflect current clinical practice. 500 to 1,000 mg once or twice daily.
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Although the manufacturer states that IV and oral dosing are equivalent; some clinicians use lower IV doses due to the poor oral absorption.
Edema (diuresis), heart failure, hypertension: Infants, Children, and Adolescents:
Oral: 10 to 40 mg/kg/day in 1 or 2 divided doses (AAP [Flynn 2017]; Hobbins 1981; Stewart 2011)
Maximum daily doses:
Infants and Children <2 years: 375 mg/day
Children ≥2 years: 1,000 mg/day
Adolescents: 2,000 mg/day
IV: Limited data available: 5 to 10 mg/kg/day in divided doses once or twice daily (Costello 2007); in some cases, doses up to 20 mg/kg/day have been used; maximum dose: 500 mg/dose (Moffett 2017)
Diabetes insipidus (central): Limited data available: Infants: Oral: Initial: 10 mg/kg/day in 2 divided doses; may need to titrate dose to target urine osmolality: 100 to 150 mOsm/L; an effective dosing range of 5 to 10 mg/kg/dose twice or three times daily has been suggested (Al Nofal 2015; Rivkees 2007; Sperling 2014)
Reconstitution
Powder for injection: To reconstitute, add SWFI 18 mL to make 28 mg/mL. May be further diluted with dextrose or sodium chloride solutions.
Extemporaneously Prepared
A 50 mg/mL oral suspension may be made with tablets. Crush ten 500 mg chlorothiazide tablets in a mortar and reduce to a fine powder; mix with a small amount of glycerin to form a uniform paste. Add 2 g carboxymethylcellulose gel (mix 2 g carboxymethylcellulose with 5 to 10 mL water to form a paste; add 40 mL water and heat to 60°C with moderate stirring until dissolution occurs; cool and allow to stand for 1 to 2 hours to form a clear gel). Dissolve 500 mg citric acid in 5 mL water and add to chlorothiazide carboxymethylcellulose mixture with 0.1% parabens. Add a quantity of purified water sufficient to make 100 mL (Nahata, 2004). Label "shake well" and "refrigerate". Stable for 30 days.
Nahata MC, Pai VB, and Hipple TF, Pediatric Drug Formulations, 5th ed, Cincinnati, OH: Harvey Whitney Books Co, 2004.
Administration
IV: Do not administer injection via IM or SubQ route. Administer slowly by direct IV injection or infusion; avoid extravasation of parenteral solution since it is extremely irritating to tissues.
Dietary Considerations
May need to decrease sodium and calcium, may need to increase potassium, zinc, magnesium, and riboflavin in diet. Some products may contain sodium.
Storage
Powder for injection: Prior to reconstitution, store between 2°C to 25°C (36°F to 77°F). The manufacturer's labeling recommends any unused reconstituted solution be discarded. Precipitation will occur in <24 hours in pH <7.4.
Suspension, tablets: Store at room temperature 15°C to 30°C (59°F to 86°F). Protect from freezing.
Chlorothiazide Images
Drug Interactions
Ajmaline: Sulfonamides may enhance the adverse/toxic effect of Ajmaline. Specifically, the risk for cholestasis may be increased. Monitor therapy
Alcohol (Ethyl): May enhance the orthostatic hypotensive effect of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Alfuzosin: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Allopurinol: Thiazide and Thiazide-Like Diuretics may enhance the potential for allergic or hypersensitivity reactions to Allopurinol. Thiazide and Thiazide-Like Diuretics may increase the serum concentration of Allopurinol. Specifically, Thiazide Diuretics may increase the concentration of Oxypurinol, an active metabolite of Allopurinol. Monitor therapy
Amifostine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Amifostine. Management: When amifostine is used at chemotherapy doses, blood pressure lowering medications should be withheld for 24 hours prior to amifostine administration. If blood pressure lowering therapy cannot be withheld, amifostine should not be administered. Consider therapy modification
Aminolevulinic Acid (Systemic): Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Systemic). Avoid combination
Aminolevulinic Acid (Topical): Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Topical). Monitor therapy
Amphetamines: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Angiotensin-Converting Enzyme Inhibitors: Thiazide and Thiazide-Like Diuretics may enhance the hypotensive effect of Angiotensin-Converting Enzyme Inhibitors. Thiazide and Thiazide-Like Diuretics may enhance the nephrotoxic effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Anticholinergic Agents: May increase the serum concentration of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Antidiabetic Agents: Thiazide and Thiazide-Like Diuretics may diminish the therapeutic effect of Antidiabetic Agents. Monitor therapy
Antidiabetic Agents: Hyperglycemia-Associated Agents may diminish the therapeutic effect of Antidiabetic Agents. Monitor therapy
Antipsychotic Agents (Second Generation [Atypical]): Blood Pressure Lowering Agents may enhance the hypotensive effect of Antipsychotic Agents (Second Generation [Atypical]). Monitor therapy
Barbiturates: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Benperidol: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Beta2-Agonists: May enhance the hypokalemic effect of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Bile Acid Sequestrants: May decrease the absorption of Thiazide and Thiazide-Like Diuretics. The diuretic response is likewise decreased. Consider therapy modification
Brigatinib: May diminish the antihypertensive effect of Antihypertensive Agents. Brigatinib may enhance the bradycardic effect of Antihypertensive Agents. Monitor therapy
Brimonidine (Topical): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Bromperidol: Blood Pressure Lowering Agents may enhance the hypotensive effect of Bromperidol. Bromperidol may diminish the hypotensive effect of Blood Pressure Lowering Agents. Avoid combination
Calcium Salts: Thiazide and Thiazide-Like Diuretics may decrease the excretion of Calcium Salts. Continued concomitant use can also result in metabolic alkalosis. Monitor therapy
CarBAMazepine: Thiazide and Thiazide-Like Diuretics may enhance the adverse/toxic effect of CarBAMazepine. Specifically, there may be an increased risk for hyponatremia. Monitor therapy
Cardiac Glycosides: Thiazide and Thiazide-Like Diuretics may enhance the adverse/toxic effect of Cardiac Glycosides. Specifically, cardiac glycoside toxicity may be enhanced by the hypokalemic and hypomagnesemic effect of thiazide diuretics. Monitor therapy
Corticosteroids (Orally Inhaled): May enhance the hypokalemic effect of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Corticosteroids (Systemic): May enhance the hypokalemic effect of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Cyclophosphamide: Thiazide and Thiazide-Like Diuretics may enhance the adverse/toxic effect of Cyclophosphamide. Specifically, granulocytopenia may be enhanced. Monitor therapy
Dexketoprofen: May enhance the adverse/toxic effect of Sulfonamides. Monitor therapy
Dexmethylphenidate: May diminish the therapeutic effect of Antihypertensive Agents. Monitor therapy
Diacerein: May enhance the therapeutic effect of Diuretics. Specifically, the risk for dehydration or hypokalemia may be increased. Monitor therapy
Diazoxide: Thiazide and Thiazide-Like Diuretics may enhance the adverse/toxic effect of Diazoxide. Monitor therapy
Diazoxide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Dichlorphenamide: Thiazide and Thiazide-Like Diuretics may enhance the hypokalemic effect of Dichlorphenamide. Monitor therapy
Dofetilide: Thiazide and Thiazide-Like Diuretics may enhance the QTc-prolonging effect of Dofetilide. Thiazide and Thiazide-Like Diuretics may increase the serum concentration of Dofetilide. Management: Although hydrochlorothiazide is specifically cited as a contraindication, the risk likely extends to all thiazide and thiazide-like diuretics and may be even greater with chlorthalidone or bendroflumethiazide. Consider alternatives when possible. Consider therapy modification
DULoxetine: Blood Pressure Lowering Agents may enhance the hypotensive effect of DULoxetine. Monitor therapy
Fexinidazole [INT]: Thiazide and Thiazide-Like Diuretics may enhance the arrhythmogenic effect of Fexinidazole [INT]. Avoid combination
Herbs (Hypertensive Properties): May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Herbs (Hypotensive Properties): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Hypotension-Associated Agents: Blood Pressure Lowering Agents may enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Ipragliflozin: May enhance the adverse/toxic effect of Thiazide and Thiazide-Like Diuretics. Specifically, the risk for intravascular volume depletion may be increased. Monitor therapy
Ivabradine: Thiazide and Thiazide-Like Diuretics may enhance the arrhythmogenic effect of Ivabradine. Monitor therapy
Levodopa-Containing Products: Blood Pressure Lowering Agents may enhance the hypotensive effect of Levodopa-Containing Products. Monitor therapy
Levosulpiride: Thiazide and Thiazide-Like Diuretics may enhance the adverse/toxic effect of Levosulpiride. Avoid combination
Licorice: May enhance the hypokalemic effect of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Lithium: Thiazide and Thiazide-Like Diuretics may decrease the excretion of Lithium. Consider therapy modification
Lormetazepam: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Mecamylamine: Sulfonamides may enhance the adverse/toxic effect of Mecamylamine. Avoid combination
Methenamine: Thiazide and Thiazide-Like Diuretics may diminish the therapeutic effect of Methenamine. Monitor therapy
Methylphenidate: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Molsidomine: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Multivitamins/Fluoride (with ADE): May enhance the hypercalcemic effect of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Multivitamins/Minerals (with ADEK, Folate, Iron): Thiazide and Thiazide-Like Diuretics may enhance the hypercalcemic effect of Multivitamins/Minerals (with ADEK, Folate, Iron). Monitor therapy
Multivitamins/Minerals (with AE, No Iron): Thiazide and Thiazide-Like Diuretics may increase the serum concentration of Multivitamins/Minerals (with AE, No Iron). Specifically, thiazide diuretics may decrease the excretion of calcium, and continued concomitant use can also result in metabolic alkalosis. Monitor therapy
Naftopidil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Neuromuscular-Blocking Agents (Nondepolarizing): Thiazide and Thiazide-Like Diuretics may enhance the neuromuscular-blocking effect of Neuromuscular-Blocking Agents (Nondepolarizing). Monitor therapy
Nicergoline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicorandil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nitroprusside: Blood Pressure Lowering Agents may enhance the hypotensive effect of Nitroprusside. Monitor therapy
Nonsteroidal Anti-Inflammatory Agents: Thiazide and Thiazide-Like Diuretics may enhance the nephrotoxic effect of Nonsteroidal Anti-Inflammatory Agents. Nonsteroidal Anti-Inflammatory Agents may diminish the therapeutic effect of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Obinutuzumab: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Management: Consider temporarily withholding blood pressure lowering medications beginning 12 hours prior to obinutuzumab infusion and continuing until 1 hour after the end of the infusion. Consider therapy modification
Opioid Agonists: May enhance the adverse/toxic effect of Diuretics. Opioid Agonists may diminish the therapeutic effect of Diuretics. Monitor therapy
OXcarbazepine: Thiazide and Thiazide-Like Diuretics may enhance the adverse/toxic effect of OXcarbazepine. Specifically, there may be an increased risk for hyponatremia. Monitor therapy
Pentoxifylline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Pholcodine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Pholcodine. Monitor therapy
Phosphodiesterase 5 Inhibitors: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Porfimer: Photosensitizing Agents may enhance the photosensitizing effect of Porfimer. Monitor therapy
Promazine: Thiazide and Thiazide-Like Diuretics may enhance the QTc-prolonging effect of Promazine. Avoid combination
Prostacyclin Analogues: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Quinagolide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Reboxetine: May enhance the hypokalemic effect of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Selective Serotonin Reuptake Inhibitors: May enhance the hyponatremic effect of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Sodium Phosphates: Diuretics may enhance the nephrotoxic effect of Sodium Phosphates. Specifically, the risk of acute phosphate nephropathy may be enhanced. Management: Consider avoiding this combination by temporarily suspending treatment with diuretics, or seeking alternatives to oral sodium phosphate bowel preparation. If the combination cannot be avoided, hydrate adequately and monitor fluid and renal status. Consider therapy modification
Topiramate: Thiazide and Thiazide-Like Diuretics may enhance the hypokalemic effect of Topiramate. Thiazide and Thiazide-Like Diuretics may increase the serum concentration of Topiramate. Management: Monitor for increased topiramate levels/adverse effects (e.g., hypokalemia) with initiation/dose increase of a thiazide diuretic. Closely monitor serum potassium concentrations with concomitant therapy. Topiramate dose reductions may be necessary. Consider therapy modification
Toremifene: Thiazide and Thiazide-Like Diuretics may enhance the hypercalcemic effect of Toremifene. Monitor therapy
Verteporfin: Photosensitizing Agents may enhance the photosensitizing effect of Verteporfin. Monitor therapy
Vitamin D Analogs: Thiazide and Thiazide-Like Diuretics may enhance the hypercalcemic effect of Vitamin D Analogs. Monitor therapy
Yohimbine: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Test Interactions
May interfere with tests for parathyroid function; may lead to false-negative aldosterone/renin ratio (ARR) (Funder 2016)
Adverse Reactions
Frequency not defined.
Cardiovascular: Hypotension, necrotizing angiitis, orthostatic hypotension
Central nervous system: Dizziness, headache, paresthesia, restlessness, vertigo
Dermatologic: Alopecia, erythema multiforme, exfoliative dermatitis, skin photosensitivity, skin rash, Stevens-Johnson syndrome, toxic epidermal necrolysis, urticaria
Endocrine & metabolic: Glycosuria, hypercalcemia, hyperglycemia, hyperuricemia, hypochloremic alkalosis, hypokalemia, hypomagnesemia, hyponatremia, increased serum cholesterol, increased serum triglycerides
Gastrointestinal: Abdominal cramps, anorexia, constipation, diarrhea, gastric irritation, nausea, pancreatitis, sialadenitis, vomiting
Genitourinary: Hematuria (IV), impotence
Hematologic & oncologic: Agranulocytosis, aplastic anemia, hemolytic anemia, leukopenia, purpura, thrombocytopenia
Hepatic: Jaundice
Hypersensitivity: Anaphylaxis
Neuromuscular & skeletal: Muscle spasm, systemic lupus erythematosus, weakness
Ophthalmic: Blurred vision, xanthopsia
Renal: Interstitial nephritis, renal failure, renal insufficiency
Respiratory: Pneumonitis, pulmonary edema, respiratory distress
Miscellaneous: Fever
Warnings/Precautions
Concerns related to adverse effects:
- Electrolyte disturbances: Hypercalcemia, hypokalemia, hypochloremic alkalosis, hyponatremia, and hypomagnesemia can occur.
- Hypersensitivity reactions: Hypersensitivity reactions may occur.
- Orthostatic hypotension: Concomitant ethanol use may increase the risk of orthostatic hypotension.
- Photosensitivity: Photosensitization may occur.
- Sulfonamide (“sulfa”) allergy: The FDA-approved product labeling for many medications containing a sulfonamide chemical group includes a broad contraindication in patients with a prior allergic reaction to sulfonamides. There is a potential for cross-reactivity between members of a specific class (eg, two antibiotic sulfonamides). However, concerns for cross-reactivity have previously extended to all compounds containing the sulfonamide structure (SO2NH2). An expanded understanding of allergic mechanisms indicates cross-reactivity between antibiotic sulfonamides and nonantibiotic sulfonamides may not occur or at the very least this potential is extremely low (Brackett 2004; Johnson 2005; Slatore 2004; Tornero 2004). In particular, mechanisms of cross-reaction due to antibody production (anaphylaxis) are unlikely to occur with nonantibiotic sulfonamides. T-cell-mediated (type IV) reactions (eg, maculopapular rash) are less well understood and it is not possible to completely exclude this potential based on current insights. In cases where prior reactions were severe (Stevens-Johnson syndrome/TEN), some clinicians choose to avoid exposure to these classes.
Disease-related concerns:
- Adrenal insufficiency: Avoid use of diuretics for treatment of elevated blood pressure in patients with primary adrenal insufficiency (Addison disease). Adjustment of glucocorticoid/mineralocorticoid therapy and/or use of other antihypertensive agents is preferred to treat hypertension (Bornstein 2016; Inder 2015).
- Diabetes: Use with caution in patients with prediabetes or diabetes mellitus; may see a change in glucose control.
- Gout: In certain patients with a history of gout, a familial predisposition to gout, or chronic renal failure, gout can be precipitated.
- Hepatic impairment: Use with caution in patients with hepatic impairment; avoid electrolyte and acid/base imbalances that might lead to hepatic encephalopathy.
- Hypercalcemia: Thiazide diuretics may decrease renal calcium excretion; consider avoiding use in patients with hypercalcemia.
- Hypercholesterolemia: Use with caution in patients with moderate or high cholesterol concentrations; increased cholesterol and triglyceride levels have been reported with thiazides.
- Hypokalemia: Use with caution in patients with hypokalemia; correct before initiating therapy.
- Renal impairment: Avoid in severe renal disease (ineffective). May precipitate azotemia; discontinue or consider withholding if renal impairment occurs.
- Systemic lupus erythematosus (SLE): Can cause SLE exacerbation or activation.
Special populations:
- Surgical patients: If given the morning of surgery, chlorothiazide may render the patient volume depleted and blood pressure may be labile during general anesthesia.
Dosage form specific issues:
- Benzyl alcohol and derivatives: Some dosage forms may contain sodium benzoate/benzoic acid; benzoic acid (benzoate) is a metabolite of benzyl alcohol; large amounts of benzyl alcohol (≥99 mg/kg/day) have been associated with a potentially fatal toxicity (“gasping syndrome”) in neonates; the “gasping syndrome” consists of metabolic acidosis, respiratory distress, gasping respirations, CNS dysfunction (including convulsions, intracranial hemorrhage), hypotension, and cardiovascular collapse (AAP ["Inactive" 1997]; CDC, 1982); some data suggests that benzoate displaces bilirubin from protein binding sites (Ahlfors, 2001); avoid or use dosage forms containing benzyl alcohol derivative with caution in neonates. See manufacturer’s labeling.
Monitoring Parameters
Serum electrolytes, renal function, blood pressure; assess weight, intake and output (I and O) reports daily to determine fluid loss
Hypertension: The 2017 Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults (ACC/AHA [Whelton 2017]):
Confirmed hypertension and known cardiovascular disease or 10-year atherosclerotic cardiovascular disease (ASCVD) risk ≥10%: Target blood pressure <130/80 mm Hg is recommended.
Confirmed hypertension without markers of increased ASCVD risk: Target blood pressure <130/80 mm Hg may be reasonable.
Diabetes and hypertension: The American Diabetes Association (ADA) guidelines (ADA 2019):
Patients 18 to 65 years of age, without ASCVD, and 10-year ASCVD risk <15%: Target blood pressure <140/90 mm Hg is recommended.
Patients 18 to 65 years of age and known ASCVD or 10-year ASCVD risk >15%: Target blood pressure <130/80 mm Hg may be appropriate if it can be safely attained.
Patients >65 years of age (healthy or complex/intermediate health): Target blood pressure <140/90 mm Hg is recommended.
Patients >65 years of age (very complex/poor health): Target blood pressure <150/90 mm Hg is recommended.
Pregnancy
Pregnancy Considerations
Chlorothiazide crosses the placenta and is found in cord blood. Maternal use may cause may cause fetal or neonatal jaundice, thrombocytopenia, or other adverse events observed in adults.
Use of thiazide diuretics to treat edema during normal pregnancies is not appropriate; use may be considered when edema is due to pathologic causes (as in the nonpregnant patient); monitor.
Chronic maternal hypertension is associated with adverse events in the fetus/infant. The risk of birth defects, low birth weight, premature delivery, stillbirth, and neonatal death may be increased with chronic hypertension in pregnancy. Actual risks may be related to duration and severity of maternal hypertension. Diuretics are considered second-line therapy for treating chronic hypertension in pregnancy (ACOG 203 2019).
The treatment of edema associated with chronic heart failure during pregnancy is similar to that of nonpregnant patients. Use of thiazide diuretics may be considered but use with caution due to the potential reduction in placental blood flow. Patients diagnosed after delivery can be treated according to heart failure guidelines (ESC [Bauersachs 2016]; ESC [Regitz-Zagrosek 2018]).
Patient Education
What is this drug used for?
- It is used to treat high blood pressure.
- It is used to get rid of extra fluid.
Frequently reported side effects of this drug
- Constipation
- Diarrhea
- Nausea
- Vomiting
- Abdominal cramps
- Lack of appetite
- Headache
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- High blood sugar like confusion, fatigue, increased thirst, increased hunger, passing a lot of urine, flushing, fast breathing, or breath that smells like fruit.
- Fluid and electrolyte problems like mood changes, confusion, muscle pain or weakness, abnormal heartbeat, severe dizziness, passing out, fast heartbeat, increased thirst, seizures, loss of strength and energy, lack of appetite, unable to pass urine or change in amount of urine passed, dry mouth, dry eyes, or nausea or vomiting.
- Kidney problems like unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain.
- Pancreatitis like severe abdominal pain, severe back pain, severe nausea, or vomiting.
- Severe dizziness
- Passing out
- Burning or numbness feeling
- Vision changes
- Sexual dysfunction
- Agitation
- Shortness of breath
- Severe loss of strength and energy
- Bruising
- Bleeding
- Chills
- Yellow skin
- Sore throat
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.