Boxed Warning
Suicidality and antidepressants:
Antidepressants increased the risk of suicidal thinking and behavior (suicidality) compared with placebo in short-term studies in children, adolescents, and young adults with major depressive disorder and other psychiatric disorders. Anyone considering the use of citalopram or any other antidepressant in a child, adolescent, or young adult must balance this risk with the clinical need. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared with placebo in adults older than 24 years; there was a reduction in risk with antidepressants compared with placebo in adults 65 years and older. Depression and certain other psychiatric disorders are themselves associated with increases in the risk of suicide. Appropriately monitor and closely observe patients of all ages who are started on antidepressant therapy for clinical worsening, suicidality, or unusual changes in behavior. Advise families and caregivers of the need for close observation and communication with the health care provider. Citalopram is not approved for use in pediatric patients.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Solution, Oral:
Generic: 10 mg/5 mL (10 mL, 240 mL)
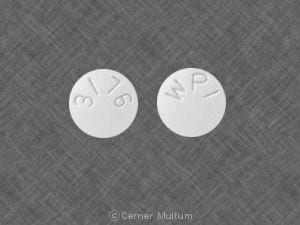
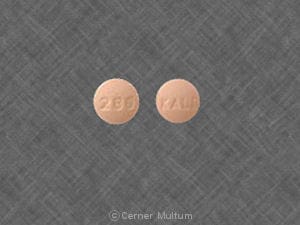
Tablet, Oral:
CeleXA: 10 mg
CeleXA: 20 mg, 40 mg [scored]
Generic: 10 mg, 20 mg, 40 mg
Pharmacology
Mechanism of Action
A racemic bicyclic phthalane derivative, citalopram selectively inhibits serotonin reuptake in the presynaptic neurons and has minimal effects on norepinephrine or dopamine. Uptake inhibition of serotonin is primarily due to the S-enantiomer of citalopram. Displays little to no affinity for serotonin, dopamine, adrenergic, histamine, GABA, or muscarinic receptor subtypes.
Pharmacokinetics/Pharmacodynamics
Distribution
Vd: 12 L/kg
Metabolism
Extensively hepatic, via CYP3A4 and 2C19 (major pathways), and 2D6 (minor pathway); metabolized to demethylcitalopram (DCT), didemethylcitalopram (DDCT), citalopram-N-oxide, and a deaminated propionic acid derivative, which are at least eight times less potent than citalopram
Excretion
Urine (Citalopram 10% and DCT 5%)
Note: Clearance was decreased, while half-life was significantly increased in patients with hepatic impairment. Mild to moderate renal impairment may reduce clearance (17%) and prolong half-life of citalopram. No pharmacokinetic information is available concerning patients with severe renal impairment. AUC and half-life were significantly increased in elderly patients (≥60 years), and in poor CYP2C19 metabolizers, steady state Cmax and AUC was increased by 68% and 107%, respectively.
Onset of Action
Depression: The onset of action is 1 to 4 weeks; however, individual response varies greatly and full response may not be seen until 8 to 12 weeks after initiation of treatment.
Time to Peak
Serum: 1 to 6 hours, average within 4 hours
Duration of Action
1 to 2 days
Half-Life Elimination
24 to 48 hours (average: 35 hours); doubled with hepatic impairment and increased by 30% (following multiple doses) to 50% (following single dose) in elderly patients (≥60 years)
Protein Binding
Plasma: ~80%
Use in Specific Populations
Special Populations: Renal Function Impairment
Oral clearance decreased 17% in mild to moderate renal impairment.
Special Populations: Hepatic Function Impairment
Oral clearance decreased 37% and half-life doubled in reduced hepatic function.
Special Populations: Elderly
Multiple dose: AUC increased 23% and half-life increased 30%. Single dose: AUC increased 30% and half-life increased 50%.
Special Populations: Gender
AUC in women was 1.5 to 2 times that in men in 3 studies; no difference was observed in 5 other studies.
Use: Labeled Indications
Major depressive disorder (unipolar): Treatment of unipolar major depressive disorder
Use: Off Label
Aggressive or agitated behavior associated with dementiaa
Data from a randomized, double-blind, placebo-controlled study support the use of citalopram in the treatment of agitation associated with dementia Porsteinsson 2014.
Binge eating disordercyes
Data from a limited number of patients studied suggest that citalopram may be beneficial for the treatment of binge eating disorder by reducing binge episode frequency, weight, and severity of illness; however, average doses used (>40 mg) are no longer recommended due to an increased risk of cardiovascular effects McElroy 2003.
Based on the
Generalized anxiety disorderc
Data from a limited number of adult and geriatric patients suggest that citalopram may be beneficial for the treatment of generalized anxiety disorder
Obsessive-compulsive disorderbyes
Data from a randomized, double-blind, placebo-controlled study support the use of citalopram in the treatment of OCD Montgomery 2001.
Based on the American Psychiatric Association practice guideline for the treatment of patients with obsessive-compulsive disorder, the use of an SSRI, such as citalopram, is an effective and recommended treatment option for patients with this condition.
Panic disorderbyes
Data from 3 double-blind, randomized, parallel-group, placebo-controlled, multicenter studies and 2 single-blind, flexible-dose studies support the use of citalopram in the treatment of panic disorder Leinonen 2000, Perna 2001, Seedat 2003, Stahl 2003, Wade 1997.
Based on the American Psychiatric Association guidelines for the treatment of patients with panic disorder and the World Federation of Societies of Biological Psychiatry guidelines for the pharmacological treatment of anxiety, obsessive-compulsive, and posttraumatic stress disorders, citalopram is effective and recommended in the management of panic disorder.
Posttraumatic stress disordercyes
Data from a double-blind, randomized, placebo- and active-controlled trial and an open-label study suggest that the use of citalopram may be beneficial in the treatment of posttraumatic stress disorder (PTSD) English 2006, Tucker 2003.
Based on the
Premature ejaculationcyes
Data from a limited number of patients in controlled trials suggest that citalopram may be beneficial for the treatment of premature ejaculation Atmaca 2002a, Safarinejad 2006.
According to the
Premenstrual dysphoric disordercyes
Data from a limited number of patients studied suggest that citalopram may be beneficial for the treatment of premenstrual dysphoric disorder as a continuous daily dose or during the luteal phase Wikander 1998.
Based on the International Society for Premenstrual Disorders auditable standards for diagnosis and management of premenstrual disorder, SSRIs are effective and recommended in the management of premenstrual dysphoric disorder.
Social anxiety disordercyes
Data from a limited number of clinical trials suggest that citalopram may be beneficial for the treatment of social anxiety disorder Atmaca 2002b, Furmark 2005.
Based on the World Federation of Societies of Biological Psychiatry guidelines for the pharmacological treatment of anxiety, obsessive-compulsive, and posttraumatic stress disorders, SSRIs such as citalopram are effective and recommended for the management of social anxiety disorder.
Vasomotor symptoms associated with menopausebyes
Data from 2 randomized, placebo-controlled trials and a meta-analysis support the use of citalopram in the treatment of vasomotor symptoms (eg, hot flashes) in peri- or postmenopausal women Barton 2010, Kalay 2007, Shams 2014.
Based on the
Contraindications
Hypersensitivity to citalopram or any component of the formulation; use of MAO inhibitors intended to treat psychiatric disorders (concurrently or within 14 days of discontinuing either citalopram or the MAO inhibitor); initiation of citalopram in a patient receiving linezolid or intravenous methylene blue; concomitant use with pimozide
Canadian labeling: Additional contraindications (not in US labeling): Known QT interval prolongation or congenital long QT syndrome
Dosage and Administration
Dosing: Adult
Note: Maximum daily dose: Due to the risk of QT prolongation, the maximum recommended daily dose for all indications is 40 mg. A lower maximum daily dose of 20 mg is recommended in patients >60 years of age, those with significant hepatic impairment, and patients who are concurrently receiving medications that significantly increase citalopram levels (eg, cimetidine, omeprazole) or known poor metabolizers of CYP2C19 substrates. Initial dose and titration: In patients sensitive to side effects, some experts suggest a lower starting dose of 10 mg daily and gradual titration in increments of no more than 10 mg, particularly in patients with anxiety who are generally more sensitive to overstimulation effects (eg, anxiety, insomnia) with antidepressants (Hirsch 2018c; WFSBP [Bandelow 2012]).
Aggressive or agitated behavior associated with dementia (off-label use): Oral: Initial: 10 mg once daily; increase to 20 mg once daily after ≥3 days. In adults ≤60 years, may further increase dose based on response and tolerability up to 30 mg/day (Pollock 2002; Pollock 2007; Porsteinsson 2014); for adults >60 years, do not exceed the maximum dose of 20 mg/day.
Binge eating disorder (off-label use): Oral: Initial: 20 mg once daily. In adults ≤60 years of age, may gradually increase dose based on response and tolerability at intervals ≥1 week to 40 mg once daily. Although doses up to 60 mg/day have been studied, due to safety considerations the recommended maximum dose is 40 mg/day for adults ≤60 years of age and 20 mg/day for adults >60 years (McElroy 2003).
Generalized anxiety disorder (off-label use): Oral: Initial: 10 mg once daily; may gradually increase dose based on response and tolerability in 10 mg increments at intervals ≥1 week to a maximum dose of 40 mg/day for adults ≤60 years and 20 mg/day for adults >60 years of age (Blank 2006; Varia 2002).
Major depressive disorder (unipolar): Oral: Initial: 20 mg once daily. In adults ≤60 years of age, may gradually increase dose based on response and tolerability at intervals ≥1 week to a maximum dose of 40 mg/day; for adults >60 years of age, do not exceed the maximum dose of 20 mg/day. Daily doses that exceeded these limits have been studied but are not recommended due to safety considerations.
Obsessive-compulsive disorder (off-label use): Oral: Initial: 20 mg once daily. In adults ≤60 years of age, may gradually increase dose based on response and tolerability in 10 to 20 mg increments at intervals ≥1 week to a maximum dose of 40 mg/day; for adults >60 years of age, do not exceed the maximum dose of 20 mg/day. Daily doses that exceeded these limits have been studied but are not recommended due to safety considerations (APA [Koran 2007]; Montgomery 2001). Note: An adequate trial for assessment of effect in obsessive-compulsive disorder is considered to be ≥6 weeks at maximum tolerated dose (Issari 2016).
Panic disorder (off-label use): Oral: Initial: 10 mg once daily for 3 to 7 days, then 20 mg once daily. In adults ≤60 years, may gradually increase dose based on response and tolerability in 10 to 20 mg increments at intervals ≥1 week to a maximum of 40 mg/day; for adults >60 years of age, do not exceed the maximum dose of 20 mg/day. Daily doses that exceeded these limits have been studied but are not recommended due to safety considerations (APA 2009b; Leinonen 2000; Perna 2001; Seedat 2003; Stahl 2003; Wade 1997).
Posttraumatic stress disorder (off-label use): Oral: Initial: 20 mg once daily. In adults ≤60 years of age, may gradually increase dose based on response and tolerability in 10 to 20 mg increments at intervals ≥1 week to a maximum dose of 40 mg once daily; for adults >60 years of age, do not exceed the maximum dose of 20 mg/day. Daily doses that exceeded these limits have been studied but are not recommended due to safety considerations (English 2006; Tucker 2003).
Premature ejaculation (off-label use): Oral: Initial: 20 mg once daily. In adults ≤60 years of age, may gradually increase dose based on response and tolerability at intervals of ≥1 week (some experts suggest 3- to 4-week titration intervals [Khera 2018]) up to a maximum of 40 mg/day (Althof 2014; Atmaca 2002a; Safarinejad 2006); for adults >60 years of age, do not exceed the maximum dose of 20 mg/day.
Premenstrual dysphoric disorder (PMDD) (off-label use):
Continuous daily dosing regimen: Oral: Initial: 10 mg once daily; over the first month increase to usual effective dose of 20 mg once daily; in subsequent menstrual cycles, further dose increases (eg, in 10 mg increments per menstrual cycle) up to 40 mg/day may be necessary in some patients for optimal response (Casper 2018; Freeman 2002; Wikander 1998).
Intermittent regimens:
Luteal phase dosing regimen: Oral: Initial: 10 mg once daily during the luteal phase of menstrual cycle only (ie, beginning therapy 14 days before anticipated onset of menstruation and continued to the onset of menses); over the first month increase to usual effective dose of 20 mg once daily during the luteal phase; in a subsequent menstrual cycle, a further increase to 30 mg/day during the luteal phase may be necessary in some patients for optimal response (Casper 2018; Freeman 2002; Wikander 1998).
Symptom-onset dosing regimen: Oral: Initial: 10 mg once daily from the day of symptom onset until a few days after the start of menses; over the first month increase to usual effective dose of 20 mg once daily; in a subsequent menstrual cycle a further increase to 30 mg/day may be necessary in some patients for optimal response (Casper 2018; Ravindran 2007).
Social anxiety disorder (off-label use): Oral: Initial: 10 to 20 mg once daily. In adults ≤60 years of age, after ~6 weeks may gradually increase dose based on response and tolerability in 10 to 20 mg increments at intervals ≥1 week up to maximum of 40 mg/day; for adults >60 years of age, do not exceed the maximum dose of 20 mg/day. Daily doses that exceeded these limits have been studied but are not recommended due to safety considerations (Atmaca 2002b; Furmark 2005; Stein 2019; WFSBP [Bandelow 2012]).
Vasomotor symptoms associated with menopause (alternative agent) (off-label use): Oral: Initial: 10 mg once daily; may increase dose to 20 mg once daily after 1 week. In adults ≤60 years of age, doses as high as 40 mg/day have been studied; however, doses >20 mg/day have demonstrated little additional benefit and greater adverse effects (Barton 2010; Kalay 2007; NAMS 2015). For adults >60 years of age, do not exceed the maximum dose of 20 mg/day.
Dosage adjustments: For concomitant therapy with moderate to strong CYP2C19 inhibitors or other drugs that significantly increase citalopram levels (eg, cimetidine, omeprazole, voriconazole) and in persons who are known to be poor metabolizers of CYP2C19: Maximum dose: 20 mg/day.
Discontinuation of therapy:When discontinuing antidepressant treatment that has lasted for >3 weeks, gradually taper the dose (eg, over 2 to 4 weeks) to minimize withdrawal symptoms and detect reemerging symptoms (APA 2010; WFSBP [Bauer 2015]). Reasons for a slower titration (eg, over 4 weeks) include use of a drug with a half-life <24 hours (eg, paroxetine, venlafaxine), prior history of antidepressant withdrawal symptoms, or high doses of antidepressants (APA 2010; Hirsch 2019). If intolerable withdrawal symptoms occur, resume the previously prescribed dose and/or decrease dose at a more gradual rate (Shelton 2001). Select patients (eg, those with a history of discontinuation syndrome) on long-term treatment (>6 months) may benefit from tapering over >3 months (WFSBP [Bauer 2015]). Evidence supporting ideal taper rates is limited (Shelton 2001; WFSBP [Bauer 2015]).
Switching antidepressants: Evidence for ideal antidepressant switching strategies is limited; strategies include cross-titration (gradually discontinuing the first antidepressant while at the same time gradually increasing the new antidepressant) and direct switch (abruptly discontinuing the first antidepressant and then starting the new antidepressant at an equivalent dose or lower dose and increasing it gradually). Cross-titration (eg, over 1 to 4 weeks depending upon sensitivity to discontinuation symptoms and adverse effects) is standard for most switches, but is contraindicated when switching to or from an MAOI. A direct switch may be an appropriate approach when switching to another agent in the same or similar class (eg, when switching between two SSRIs), when the antidepressant to be discontinued has been used for <1 week, or when the discontinuation is for adverse effects. When choosing the switch strategy, consider the risk of discontinuation symptoms, potential for drug interactions, other antidepressant properties (eg, half-life, adverse effects, pharmacodynamics), and the degree of symptom control desired (Hirsch 2018b; Ogle 2013; WFSBP [Bauer 2013]).
Switching to or from an MAOI:
Allow 14 days to elapse between discontinuing an MAOI and initiation of citalopram.
Allow 14 days to elapse between discontinuing citalopram and initiation of an MAOI.
Dosing: Geriatric
Note: For patients >60 years of age, the maximum recommended dose is 20 mg/day due to the risk of QT prolongation.
Generalized anxiety disorder (off-label use): Oral: Initial: 10 mg once daily; may increase dose based on response and tolerability in 10 mg increments at intervals ≥1 week up to 20 mg/day. Doses up to 40 mg/day have been studied; however, according to the manufacturer, dosing should not exceed 20 mg/day. (Blank 2006; Lenze 2005)
Major depressive disorder (unipolar): Adults >60 years: Oral: Initial: 10 to 20 mg once daily (Marano 2015; VA/DoD 2016); maximum dose: 20 mg/day due to increased exposure and the risk of QT prolongation.
Discontinuation of therapy: Refer to adult dosing.
Switching antidepressants: Refer to adult dosing.
Dosing: Pediatric
Note: Slower titration of dose every 2 to 4 weeks may minimize risk of SSRI associated behavioral activation, which has been shown to increase risk of suicidal behavior. Doses >40 mg are not recommended due to risk of QTc prolongation.
Depression: Limited data available; efficacy results variable: One randomized, placebo-controlled trial has shown citalopram to be effective for the treatment of depression in pediatric patients (Wagner 2004); other controlled pediatric trials have not shown benefit (Sharp 2006; von Knorring 2006; Wagner 2005). Some experts recommend the following doses (Dopheide 2006): Oral:
Children 7 to ≤11 years: Initial: 10 mg/day given once daily; increase dose slowly by 5 mg/day every 2 weeks as clinically needed; dosage range: 20 to 40 mg/day
Children and Adolescents ≥12 years: Initial: 20 mg/day given once daily; increase dose slowly by 10 mg/day every 2 weeks as clinically needed; dosage range: 20 to 40 mg/day
Obsessive-compulsive disorder: Limited data available: Several open label trials have been published (Mukaddes 2003; Thomsen 1997; Thomsen 2001). Some experts recommend the following doses: Oral:
Children 7 to ≤11 years: Initial: 5 to 10 mg/day given once daily; increase dose slowly by 5 mg/day every 2 weeks as clinically needed; dosage range: 10 to 40 mg/day
Children and Adolescents ≥12 years: Initial: 10 to 20 mg/day given once daily; increase dose slowly by 10 mg/day every 2 weeks as clinically needed; dosage range: 10 to 40 mg/day
Note: Higher mg/kg doses are needed in children compared to adolescents.
Discontinuation of therapy: Consider planning antidepressant discontinuation for lower-stress times, recognizing non-illness-related factors could cause stress or anxiety and be misattributed to antidepressant discontinuation (Hathaway 2018). Upon discontinuation of antidepressant therapy, gradually taper the dose to minimize the incidence of discontinuation syndromes (withdrawal) and allow for the detection of reemerging disease state symptoms (eg, relapse). Evidence supporting ideal taper rates after illness remission is limited. APA and NICE guidelines suggest tapering therapy over at least several weeks with consideration to the half-life of the antidepressant; antidepressants with a shorter half-life may need to be tapered more conservatively. After long-term (years) antidepressant treatment, WFSBP guidelines recommend tapering over 4 to 6 months, with close monitoring during and for 6 months after discontinuation. If intolerable discontinuation symptoms occur following a dose reduction, consider resuming the previously prescribed dose and/or decrease dose at a more gradual rate (APA 2010; Bauer 2002; Fenske 2009; Haddad 2001; NCCMH 2010; Schatzberg 2006; Shelton 2001; Warner 2006).
MAO inhibitor recommendations:
Switching to or from an MAO inhibitor intended to treat psychiatric disorders:
Allow 14 days to elapse between discontinuing an MAO inhibitor intended to treat psychiatric disorders and initiation of citalopram.
Allow 14 days to elapse between discontinuing citalopram and initiation of an MAO inhibitor intended to treat psychiatric disorders.
Administration
Oral: May be administered without regard to food.
Dietary Considerations
May be taken without regard to food.
Storage
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Protect from moisture.
Citalopram Images
Drug Interactions
Acalabrutinib: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Agents with Antiplatelet Properties (e.g., P2Y12 inhibitors, NSAIDs, SSRIs, etc.): May enhance the antiplatelet effect of other Agents with Antiplatelet Properties. Monitor therapy
Alcohol (Ethyl): May enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk of psychomotor impairment may be enhanced. Management: Patients receiving selective serotonin reuptake inhibitors should be advised to avoid alcohol. Monitor for increased psychomotor impairment in patients who consume alcohol during treatment with selective serotonin reuptake inhibitors. Consider therapy modification
Almotriptan: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Alosetron: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Amphetamines: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Anticoagulants: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Anticoagulants. Exceptions: Bemiparin; Enoxaparin; Heparin. Monitor therapy
Antiemetics (5HT3 Antagonists): May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Exceptions: Alosetron; Ondansetron; Ramosetron. Monitor therapy
Antipsychotic Agents: Serotonergic Agents (High Risk) may enhance the adverse/toxic effect of Antipsychotic Agents. Specifically, serotonergic agents may enhance dopamine blockade, possibly increasing the risk for neuroleptic malignant syndrome. Antipsychotic Agents may enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Monitor therapy
Apixaban: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Apixaban. Specifically, the risk for bleeding may be increased. Management: Carefully consider risks and benefits of this combination and monitor closely. Monitor therapy
ARIPiprazole: CYP2D6 Inhibitors (Weak) may increase the serum concentration of ARIPiprazole. Management: Monitor for increased aripiprazole pharmacologic effects. Aripiprazole dose adjustments may or may not be required based on concomitant therapy and/or indication. Consult full interaction monograph for specific recommendations. Monitor therapy
Aspirin: Selective Serotonin Reuptake Inhibitors may enhance the antiplatelet effect of Aspirin. Monitor therapy
Bemiparin: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Bemiparin. Management: Avoid concomitant use of bemiparin with antiplatelet agents. If concomitant use is unavoidable, monitor closely for signs and symptoms of bleeding. Consider therapy modification
Blood Glucose Lowering Agents: Selective Serotonin Reuptake Inhibitors may enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Brexanolone: Selective Serotonin Reuptake Inhibitors may enhance the CNS depressant effect of Brexanolone. Monitor therapy
Bromopride: May enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Avoid combination
BuPROPion: May enhance the adverse/toxic effect of Citalopram. Specifically, the risk for seizures and serotonin syndrome may be increased with this combination. BuPROPion may increase the serum concentration of Citalopram. Management: Initiate citalopram at the lower end of the normal dose range in patients receiving bupropion and consider limiting the maximum citalopram adult dose to 20 mg/day during concomitant bupropion treatment. Consider therapy modification
BusPIRone: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
CarBAMazepine: May decrease the serum concentration of Citalopram. Monitor therapy
Cephalothin: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Cephalothin. Specifically, the risk for bleeding may be increased. Monitor therapy
Cimetidine: May increase the serum concentration of Citalopram. Monitor therapy
CNS Depressants: May enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk of psychomotor impairment may be enhanced. Monitor therapy
Collagenase (Systemic): Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Collagenase (Systemic). Specifically, the risk of injection site bruising and/or bleeding may be increased. Monitor therapy
Cyclobenzaprine: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
CYP2C19 Inducers (Moderate): May decrease the serum concentration of CYP2C19 Substrates (High risk with Inducers). Monitor therapy
CYP2C19 Inducers (Strong): May increase the metabolism of CYP2C19 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
CYP2C19 Inhibitors (Moderate): May increase the serum concentration of Citalopram. Management: Limit citalopram dose to a maximum of 20 mg/day if used with a moderate CYP2C19 inhibitor. Patients using this combination should be monitored closely for evidence of citalopram toxicity (eg, serotonin syndrome, QT prolongation). Exceptions: FLUoxetine; FluvoxaMINE; Moclobemide. Consider therapy modification
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May increase the metabolism of CYP3A4 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
Cyproheptadine: May diminish the therapeutic effect of Selective Serotonin Reuptake Inhibitors. Monitor therapy
Dabigatran Etexilate: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Dabigatran Etexilate. Agents with Antiplatelet Properties may increase the serum concentration of Dabigatran Etexilate. This mechanism applies specifically to clopidogrel. Management: Carefully consider risks and benefits of this combination and monitor closely; Canadian labeling recommends avoiding prasugrel or ticagrelor. Monitor therapy
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dabrafenib: May decrease the serum concentration of CYP2C19 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP2C19 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dapoxetine: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Do not use serotonergic agents (high risk) with dapoxetine or within 7 days of serotonergic agent discontinuation. Do not use dapoxetine within 14 days of monoamine oxidase inhibitor use. Dapoxetine labeling lists this combination as contraindicated. Avoid combination
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Deoxycholic Acid: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Deoxycholic Acid. Specifically, the risk for bleeding or bruising in the treatment area may be increased. Monitor therapy
Desmopressin: Selective Serotonin Reuptake Inhibitors may enhance the adverse/toxic effect of Desmopressin. Monitor therapy
Dexmethylphenidate-Methylphenidate: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Dextromethorphan: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Domperidone: QT-prolonging Agents (Moderate Risk) may enhance the QTc-prolonging effect of Domperidone. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Doxepin-Containing Products: Citalopram may enhance the QTc-prolonging effect of Doxepin-Containing Products. Citalopram may enhance the serotonergic effect of Doxepin-Containing Products. This could result in serotonin syndrome. Management: Monitor for QTc interval prolongation, ventricular arrhythmias, and serotonin syndrome when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
DULoxetine: Selective Serotonin Reuptake Inhibitors may enhance the antiplatelet effect of DULoxetine. Selective Serotonin Reuptake Inhibitors may enhance the serotonergic effect of DULoxetine. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, mental status changes) when these agents are combined. In addition, monitor for signs and symptoms of bleeding. Monitor therapy
Edoxaban: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Edoxaban. Specifically, the risk of bleeding may be increased. Monitor therapy
Eletriptan: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Enoxaparin: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Enoxaparin. Management: Discontinue antiplatelet agents prior to initiating enoxaparin whenever possible. If concomitant administration is unavoidable, monitor closely for signs and symptoms of bleeding. Consider therapy modification
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Enzalutamide: May decrease the serum concentration of CYP2C19 Substrates (High risk with Inducers). Conversely, concentrations of active metabolites may be increased for those drugs activated by CYP2C19. Management: Concurrent use of enzalutamide with CYP2C19 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP2C19 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Ergot Derivatives: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Exceptions: Nicergoline. Monitor therapy
Escitalopram: Citalopram may enhance the antiplatelet effect of Escitalopram. Escitalopram may enhance the QTc-prolonging effect of Citalopram. Escitalopram may enhance the serotonergic effect of Citalopram. This could result in serotonin syndrome. Avoid combination
Esomeprazole: May increase the serum concentration of Citalopram. Monitor therapy
Fat Emulsion (Fish Oil Based): May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Monitor therapy
Fexinidazole [INT]: May enhance the QTc-prolonging effect of QT-prolonging Agents (Moderate Risk). Avoid combination
Fluconazole: May enhance the QTc-prolonging effect of Citalopram. Fluconazole may increase the serum concentration of Citalopram. Management: Limit citalopram dose to a maximum of 20 mg/day if used with fluconazole, which is a strong CYP2C19 inhibitor. Consider therapy modification
FLUoxetine: Citalopram may enhance the antiplatelet effect of FLUoxetine. Citalopram may enhance the serotonergic effect of FLUoxetine. This could result in serotonin syndrome. FLUoxetine may increase the serum concentration of Citalopram. Management: Limit citalopram dose to a maximum of 20 mg/day. Monitor for signs and symptoms of bleeding, QTc interval prolongation, or serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor) if combined. Consider therapy modification
FluvoxaMINE: Citalopram may enhance the antiplatelet effect of FluvoxaMINE. Citalopram may enhance the serotonergic effect of FluvoxaMINE. This could result in serotonin syndrome. FluvoxaMINE may increase the serum concentration of Citalopram. Management: Limit citalopram dose to a maximum of 20 mg/day. Monitor for signs and symptoms of bleeding, QTc prolongation, or serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor) if combined. Consider therapy modification
Gilteritinib: Citalopram may enhance the QTc-prolonging effect of Gilteritinib. Gilteritinib may diminish the therapeutic effect of Citalopram. Management: Avoid use of this combination if possible. If use is necessary, monitor for reduced response to citalopram and for QTc prolongation and arrhythmias. Patients with other risk factors may be at greater risk for these serious toxicities. Consider therapy modification
Glucosamine: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Haloperidol: QT-prolonging Antidepressants (Moderate Risk) may enhance the QTc-prolonging effect of Haloperidol. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Heparin: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Heparin. Management: Decrease the dose of heparin or agents with antiplatelet properties if coadministration is required. Consider therapy modification
Herbs (Anticoagulant/Antiplatelet Properties) (eg, Alfalfa, Anise, Bilberry): May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Bleeding may occur. Management: Avoid combination when possible. If used, monitor more closely for evidence of bleeding. Discontinue herbal products with anticoagulant or antiplatelet actions 2 weeks prior to surgical, dental, or invasive procedures. Consider therapy modification
Hydroxychloroquine: Citalopram may enhance the hypoglycemic effect of Hydroxychloroquine. Hydroxychloroquine may enhance the QTc-prolonging effect of Citalopram. Monitor therapy
Ibritumomab Tiuxetan: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Ibritumomab Tiuxetan. Both agents may contribute to impaired platelet function and an increased risk of bleeding. Monitor therapy
Ibrutinib: May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Monitor therapy
Inotersen: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Ioflupane I 123: Selective Serotonin Reuptake Inhibitors may diminish the diagnostic effect of Ioflupane I 123. Monitor therapy
Lasmiditan: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Limaprost: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Linezolid: May enhance the serotonergic effect of Selective Serotonin Reuptake Inhibitors. This could result in serotonin syndrome. Avoid combination
Lofexidine: QT-prolonging Antidepressants (Moderate Risk) may enhance the QTc-prolonging effect of Lofexidine. Lofexidine may enhance the QTc-prolonging effect of QT-prolonging Antidepressants (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Lorcaserin: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Lumacaftor and Ivacaftor: May decrease the serum concentration of Citalopram. Monitor therapy
Metaxalone: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Methylene Blue: Selective Serotonin Reuptake Inhibitors may enhance the serotonergic effect of Methylene Blue. This could result in serotonin syndrome. Avoid combination
Metoclopramide: May enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Management: Seek alternatives to this combination when possible. Monitor patients receiving metoclopramide with selective serotonin reuptake inhibitors for signs of extrapyramidal symptoms, neuroleptic malignant syndrome, and serotonin syndrome. Consider therapy modification
MetyroSINE: May enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Monitor therapy
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Monoamine Oxidase Inhibitors (Antidepressant): Selective Serotonin Reuptake Inhibitors may enhance the serotonergic effect of Monoamine Oxidase Inhibitors (Antidepressant). This could result in serotonin syndrome. Avoid combination
Multivitamins/Fluoride (with ADE): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Multivitamins/Minerals (with ADEK, Folate, Iron): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Multivitamins/Minerals (with AE, No Iron): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Nefazodone: May enhance the serotonergic effect of Selective Serotonin Reuptake Inhibitors. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective): Selective Serotonin Reuptake Inhibitors may enhance the antiplatelet effect of Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective). Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective) may diminish the therapeutic effect of Selective Serotonin Reuptake Inhibitors. Monitor therapy
Nonsteroidal Anti-Inflammatory Agents (Nonselective): Selective Serotonin Reuptake Inhibitors may enhance the antiplatelet effect of Nonsteroidal Anti-Inflammatory Agents (Nonselective). Nonsteroidal Anti-Inflammatory Agents (Nonselective) may diminish the therapeutic effect of Selective Serotonin Reuptake Inhibitors. Management: Consider alternatives to NSAIDs. Monitor for evidence of bleeding and diminished antidepressant effects. It is unclear whether COX-2-selective NSAIDs reduce risk. Exceptions: Diclofenac (Topical); Ibuprofen (Topical); Piroxicam (Topical). Consider therapy modification
Nonsteroidal Anti-Inflammatory Agents (Topical): May enhance the antiplatelet effect of Selective Serotonin Reuptake Inhibitors. Monitor therapy
Obinutuzumab: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Obinutuzumab. Specifically, the risk of serious bleeding-related events may be increased. Monitor therapy
Omega-3 Fatty Acids: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Omeprazole: May increase the serum concentration of Citalopram. Management: Limit citalopram dose to a maximum of 20 mg/day if used with omeprazole. Consider therapy modification
Ondansetron: May enhance the QTc-prolonging effect of QT-prolonging Antidepressants (Moderate Risk). Ondansetron may enhance the serotonergic effect of QT-prolonging Antidepressants (Moderate Risk). This could result in serotonin syndrome. Management: Monitor for QTc interval prolongation, ventricular arrhythmias, and serotonin syndrome when these agents are combined. Patients with additional risk factors for QTc prolongation or serotonin syndrome may be at even higher risk. Monitor therapy
Opioid Agonists: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Exceptions: FentaNYL; Meperidine; TraMADol. Monitor therapy
Oxitriptan: Serotonergic Agents (High Risk) may enhance the serotonergic effect of Oxitriptan. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Pentamidine (Systemic): May enhance the QTc-prolonging effect of QT-prolonging Antidepressants (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Pentosan Polysulfate Sodium: May enhance the adverse/toxic effect of Agents with Antiplatelet Properties. Specifically, the risk of bleeding may be increased by concurrent use of these agents. Monitor therapy
Pentoxifylline: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Perhexiline: CYP2D6 Inhibitors (Weak) may increase the serum concentration of Perhexiline. Monitor therapy
Pimozide: May enhance the QTc-prolonging effect of QT-prolonging Agents (Moderate Risk). Avoid combination
Prostacyclin Analogues: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
QT-prolonging Agents (Highest Risk): May enhance the QTc-prolonging effect of Citalopram. Avoid combination
QT-prolonging Antipsychotics (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Antidepressants (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Pimozide. Monitor therapy
QT-prolonging Class IC Antiarrhythmics (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Antidepressants (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Kinase Inhibitors (Moderate Risk): QT-prolonging Antidepressants (Moderate Risk) may enhance the QTc-prolonging effect of QT-prolonging Kinase Inhibitors (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Gilteritinib. Monitor therapy
QT-prolonging Miscellaneous Agents (Moderate Risk): QT-prolonging Antidepressants (Moderate Risk) may enhance the QTc-prolonging effect of QT-prolonging Miscellaneous Agents (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Domperidone; Lofexidine. Monitor therapy
QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk): Citalopram may enhance the QTc-prolonging effect of QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk). QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of Citalopram. Exceptions: Fluconazole. Monitor therapy
QT-prolonging Quinolone Antibiotics (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Antidepressants (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Strong CYP3A4 Inhibitors (Moderate Risk): Citalopram may enhance the QTc-prolonging effect of QT-prolonging Strong CYP3A4 Inhibitors (Moderate Risk). QT-prolonging Strong CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of Citalopram. Exceptions: Voriconazole. Monitor therapy
Ramosetron: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Rasagiline: Selective Serotonin Reuptake Inhibitors may enhance the serotonergic effect of Rasagiline. This could result in serotonin syndrome. Avoid combination
RifAMPin: May decrease the serum concentration of Citalopram. Monitor therapy
Rivaroxaban: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Rivaroxaban. Management: Carefully consider risks and benefits of this combination and monitor closely; Canadian labeling recommends avoiding prasugrel or ticagrelor. Monitor therapy
Safinamide: May enhance the serotonergic effect of Selective Serotonin Reuptake Inhibitors. This could result in serotonin syndrome. Management: Use the lowest effective dose of SSRIs in patients treated with safinamide and monitor for signs and symptoms of serotonin syndrome/serotonin toxicity. Consider therapy modification
Salicylates: Agents with Antiplatelet Properties may enhance the adverse/toxic effect of Salicylates. Increased risk of bleeding may result. Monitor therapy
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Selective Serotonin Reuptake Inhibitors: Citalopram may enhance the antiplatelet effect of Selective Serotonin Reuptake Inhibitors. Citalopram may enhance the serotonergic effect of Selective Serotonin Reuptake Inhibitors. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, mental status changes) when these agents are combined. In addition, monitor for signs and symptoms of bleeding. Exceptions: Dapoxetine; Escitalopram; FLUoxetine; FluvoxaMINE. Monitor therapy
Selegiline: Selective Serotonin Reuptake Inhibitors may enhance the serotonergic effect of Selegiline. This could result in serotonin syndrome. Avoid combination
Serotonergic Agents (High Risk, Miscellaneous): May enhance the serotonergic effect of Selective Serotonin Reuptake Inhibitors. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Serotonergic Non-Opioid CNS Depressants: Selective Serotonin Reuptake Inhibitors may enhance the serotonergic effect of Serotonergic Non-Opioid CNS Depressants. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Serotonergic Opioids (High Risk): May enhance the serotonergic effect of Selective Serotonin Reuptake Inhibitors. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) if these agents are combined. Exceptions: TraMADol. Monitor therapy
Serotonin 5-HT1D Receptor Agonists (Triptans): May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Exceptions: Almotriptan; Eletriptan. Monitor therapy
Serotonin/Norepinephrine Reuptake Inhibitors: Selective Serotonin Reuptake Inhibitors may enhance the antiplatelet effect of Serotonin/Norepinephrine Reuptake Inhibitors. Selective Serotonin Reuptake Inhibitors may enhance the serotonergic effect of Serotonin/Norepinephrine Reuptake Inhibitors. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, mental status changes) when these agents are combined. In addition, monitor for signs and symptoms of bleeding. Exceptions: DULoxetine. Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
St John's Wort: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. St John's Wort may decrease the serum concentration of Serotonergic Agents (High Risk). Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Syrian Rue: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Thiazide and Thiazide-Like Diuretics: Selective Serotonin Reuptake Inhibitors may enhance the hyponatremic effect of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Thrombolytic Agents: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Thrombolytic Agents. Monitor therapy
Thyroid Products: Selective Serotonin Reuptake Inhibitors may diminish the therapeutic effect of Thyroid Products. Thyroid product dose requirements may be increased. Monitor therapy
Tipranavir: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
TraMADol: May enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk for serotonin syndrome/serotonin toxicity and seizures may be increased. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) and seizures when these agents are combined. Monitor therapy
Tricyclic Antidepressants: May enhance the serotonergic effect of Citalopram. Tricyclic Antidepressants may increase the serum concentration of Citalopram. Citalopram may increase the serum concentration of Tricyclic Antidepressants. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) and increased TCA and citalopram concentrations/effects. Exceptions: Doxepin (Systemic); Doxepin (Topical). Monitor therapy
Urokinase: Agents with Antiplatelet Properties may enhance the anticoagulant effect of Urokinase. Avoid combination
Vitamin E (Systemic): May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Vitamin K Antagonists (eg, warfarin): Selective Serotonin Reuptake Inhibitors may enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Voriconazole: Citalopram may enhance the QTc-prolonging effect of Voriconazole. Voriconazole may increase the serum concentration of Citalopram. Management: Limit citalopram dose to a maximum of 20 mg/day if used with voriconazole, which is a moderate CYP2C19 inhibitor. Consider therapy modification
Zanubrutinib: May enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Adverse Reactions
>10%:
Central nervous system: Drowsiness (18%; dose related), insomnia (15%; dose related)
Dermatologic: Diaphoresis (11%; dose related)
Gastrointestinal: Nausea (21%), xerostomia (20%)
1% to 10%:
Cardiovascular: Prolonged Q-T interval on ECG (2%), hypotension (≥1%), orthostatic hypotension (≥1%), tachycardia (≥1%), bradycardia (1%)
Central nervous system: Fatigue (5%; dose related), anxiety (4%), agitation (3%), yawning (2%; dose related), amnesia (≥1%), apathy (≥1%), confusion (≥1%), depression (≥1%), lack of concentration (≥1%), migraine (≥1%), paresthesia (≥1%)
Dermatologic: Skin rash (≥1%), pruritus (≥1%)
Endocrine & metabolic: Decreased libido (1% to 4%), amenorrhea (≥1%), weight gain (≥1%), weight loss (≥1%)
Gastrointestinal: Diarrhea (8%), dyspepsia (5%), anorexia (4%), vomiting (4%), abdominal pain (3%), dysgeusia (≥1%), flatulence (≥1%), increased appetite (≥1%), sialorrhea (≥1%)
Genitourinary: Ejaculatory disorder (6%), dysmenorrhea (3%), impotence (3%; dose related)
Neuromuscular & skeletal: Tremor (8%), arthralgia (2%), myalgia (2%)
Ophthalmic: Accommodation disturbance (≥1%)
Renal: Polyuria (≥1%)
Respiratory: Rhinitis (5%), upper respiratory tract infection (5%), sinusitis (3%), cough (≥1%)
Miscellaneous: Fever (2%)
<1%, postmarketing, and/or case reports: Abnormal gait, abnormal lacrimation, abnormal serum prolactin levels, acne vulgaris, acute renal failure, aggressive behavior, akathisia, alopecia, altered serum glucose, anaphylaxis, anemia, angina pectoris, angioedema, angle-closure glaucoma, arthritis, asthma, ataxia, atrial fibrillation, blepharoptosis, blood coagulation disorder, breast hypertrophy, bronchitis, bronchospasm, bruxism, bundle branch block, bursitis, cardiac arrest, cardiac failure, cataract, catatonia, cellulitis, cerebrovascular accident, cholecystitis, cholelithiasis, choreoathetosis, colitis, conjunctivitis, dehydration, delirium, delusions, depersonalization, dermatitis, diplopia, diverticulitis, drug dependence, dry eye syndrome, duodenal ulcer, dyskinesia, dysphagia, dyspnea, dystonia, dysuria, ecchymoses, eczema, emotional lability, epistaxis, eructation, erythema multiforme, esophagitis, euphoria, extrapyramidal reaction, extrasystoles, eye pain, facial edema, flu-like symptoms, flushing, galactorrhea, gastric ulcer, gastritis, gastroenteritis, gastroesophageal reflux disease, gastrointestinal hemorrhage, gingival hemorrhage, gingivitis, glossitis, goiter, granulocytopenia, gynecomastia, hallucination, hematuria, hemolytic anemia, hemorrhoids, hepatic necrosis, hepatitis, hiccups, hot flash, hyperbilirubinemia, hyperesthesia, hyperkinesia, hypersensitivity reaction, hypertension, hypertonia, hypertrichosis, hypochromic anemia, hypoesthesia, hypoglycemia, hypohidrosis, hypokalemia, hypokinesia, hyponatremia, hypoprothrombinemia, hypothyroidism, increased libido, increased liver enzymes, increased serum alkaline phosphatase, increased thirst, involuntary muscle movements, ischemic heart disease, jaundice, keratitis, laryngitis, leg cramps, leukocytosis, leukopenia, lymphadenopathy, lymphocytopenia, lymphocytosis, mastalgia, melanosis, myasthenia, mydriasis, myocardial infarction, myoclonus, nephrolithiasis, neuralgia, neuroleptic malignant syndrome (Stevens 2008), nightmares, nystagmus, obesity, oliguria, osteoporosis, pancreatitis, panic attack, paranoia, peripheral edema, phlebitis, photophobia, pneumonia, pneumonitis, priapism, pruritus ani, psoriasis, psychosis, pulmonary embolism, purpura, pyelonephritis, Raynaud's phenomenon (Khouri 2016; Peiró 2007), renal pain, rhabdomyolysis, rigors, seasonal allergic rhinitis, seizure, serotonin syndrome, skeletal pain, skin discoloration, skin photosensitivity, stomatitis, stupor, syncope, thrombocytopenia, thrombosis, tinnitus, tonic-clonic seizures, torsades de pointes, toxic epidermal necrolysis, transient ischemic attacks, urinary incontinence, urinary retention, urticaria, vaginal hemorrhage, ventricular arrhythmia, vertigo, withdrawal syndrome, xeroderma
Warnings/Precautions
Major psychiatric warnings:
- Suicidal thinking/behavior: [US Boxed Warning]: Antidepressants increase the risk of suicidal thinking and behavior in children, adolescents, and young adults (18 to 24 years of age) with major depressive disorder (MDD) and other psychiatric disorders; consider risk prior to prescribing. Short-term studies did not show an increased risk in patients >24 years of age and showed a decreased risk in patients ≥65 years. Closely monitor patients for clinical worsening, suicidality, or unusual changes in behavior, particularly during the initial 1 to 2 months of therapy or during periods of dosage adjustments (increases or decreases); the patient's family or caregiver should be instructed to closely observe the patient and communicate condition with health care provider. A medication guide concerning the use of antidepressants should be dispensed with each prescription. Citalopram is not FDA approved for use in children.
- The possibility of a suicide attempt is inherent in major depression and may persist until remission occurs. Worsening depression and severe abrupt suicidality that are not part of the presenting symptoms may require discontinuation or modification of drug therapy. Use caution in high-risk patients during initiation of therapy.
- Prescriptions should be written for the smallest quantity consistent with good patient care. The patient's family or caregiver should be alerted to monitor patients for the emergence of suicidality and associated behaviors such as anxiety, agitation, panic attacks, insomnia, irritability, hostility, impulsivity, akathisia, hypomania, and mania; patients should be instructed to notify their healthcare provider if any of these symptoms or worsening depression or psychosis occur.
Concerns related to adverse effects:
- Bleeding risk: May impair platelet aggregation resulting in increased risk of bleeding events, particularly if used concomitantly with aspirin, NSAIDs, warfarin, or other anticoagulants. Bleeding (including GI bleeding) related to SSRI or SNRI use has been reported to range from relatively minor bruising and epistaxis to life-threatening hemorrhage.
- CNS depression: Has a low potential to impair cognitive or motor performance; caution operating hazardous machinery or driving.
- Fractures: Bone fractures have been associated with antidepressant treatment. Consider the possibility of a fragility fracture if an antidepressant-treated patient presents with unexplained bone pain, point tenderness, swelling, or bruising (Rabenda 2013; Rizzoli 2012).
- Ocular effects: May cause mild pupillary dilation which in susceptible individuals can lead to an episode of narrow-angle glaucoma. Consider evaluating patients who have not had an iridectomy for narrow-angle glaucoma risk factors.
- QT prolongation: Causes dose-dependent QTc prolongation; torsade de pointes, ventricular tachycardia, and sudden death have been reported. Due to this risk, doses >40 mg/day are not recommended. Additionally, the maximum daily dose should not exceed 20 mg/day in certain populations (eg, CYP2C19 poor metabolizers, patients with hepatic impairment, elderly patients). Use is not recommended in patients with congenital long QT syndrome, bradycardia, recent MI, uncompensated heart failure, hypokalemia, and/or hypomagnesemia, or patients receiving concomitant medications which prolong the QT interval; if use is essential and cannot be avoided in these patients, ECG monitoring is recommended. Discontinue therapy in any patient with persistent QTc measurements >500 msec. Serum electrolytes, particularly potassium and magnesium, should be monitored prior to initiation and periodically during therapy in any patient at increased risk for significant electrolyte disturbances; hypokalemia and/or hypomagnesemia should be corrected prior to use.
- Serotonin syndrome: Potentially life-threatening serotonin syndrome (SS) has occurred with serotonergic agents (eg, SSRIs, SNRIs), particularly when used in combination with other serotonergic agents (eg, triptans, TCAs, fentanyl, lithium, tramadol, buspirone, St John's wort, tryptophan) or agents that impair metabolism of serotonin (eg, MAO inhibitors intended to treat psychiatric disorders, other MAO inhibitors [ie, linezolid and intravenous methylene blue]). Monitor patients closely for signs of SS such as mental status changes (eg, agitation, hallucinations, delirium, coma); autonomic instability (eg, tachycardia, labile blood pressure, diaphoresis); neuromuscular changes (eg, tremor, rigidity, myoclonus); GI symptoms (eg, nausea, vomiting, diarrhea); and/or seizures. Discontinue treatment (and any concomitant serotonergic agent) immediately if signs/symptoms arise.
- Sexual dysfunction: May cause or exacerbate sexual dysfunction.
- SIADH and hyponatremia: SSRIs and SNRIs have been associated with the development of SIADH; hyponatremia has been reported rarely (including severe cases with serum sodium <110 mmol/L), predominately in the elderly; reversible with discontinuation of treatment. Volume depletion and/or concurrent use of diuretics likely increases risk.
Disease-related concerns:
- Heart failure: In a scientific statement from the American Heart Association, citalopram has been determined to be an agent that may exacerbate underlying myocardial dysfunction (magnitude: major) (AHA [Page 2016]).
- Hepatic impairment: Use with caution in patients with hepatic impairment; clearance is decreased and plasma concentrations are increased; a maximum of 20 mg/day is recommended in any patient with hepatic impairment due to the risk of QT prolongation.
- Mania/hypomania: May worsen psychosis in some patients or precipitate a shift to mania or hypomania in patients with bipolar disorder. Monotherapy in patients with bipolar disorder should be avoided. Patients presenting with depressive symptoms should be screened for bipolar disorder. Citalopram is not FDA approved for the treatment of bipolar depression.
- Renal impairment: Use with caution in patients with severe renal impairment (pharmacokinetic information is not available). Clearance is decreased in patients with mild to moderate renal impairment, although no dosage adjustment is necessary.
- Seizure disorders: Use with caution in patients with a previous seizure disorder or condition predisposing to seizures such as brain damage or alcoholism.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- CYP2C19 poor metabolizers: Citalopram exposure and maximum concentrations are increased in CYP2C19 poor metabolizers; a maximum daily dose of 20 mg/day is recommended in these patients.
- Elderly: Pharmacokinetics are altered in patients >60 years of age; a lower maximum dose of 20 mg/day is recommended in this population because of the risk of QT prolongation.
- Pediatric: Citalopram is not FDA-approved for use in children; however, if used, monitor weight and growth regularly during therapy due to the potential for decreased appetite and weight loss with SSRI use.
- Pregnancy: Use caution in pregnant patients; high doses of citalopram have been associated with teratogenicity in animals.
Other warnings/precautions:
- Discontinuation syndrome: Abrupt discontinuation or interruption of antidepressant therapy has been associated with a discontinuation syndrome. Symptoms arising may vary with antidepressant however commonly include nausea, vomiting, diarrhea, headaches, light-headedness, dizziness, diminished appetite, sweating, chills, tremors, paresthesias, fatigue, somnolence, and sleep disturbances (eg, vivid dreams, insomnia). Less common symptoms include electric shock-like sensations, cardiac arrhythmias (more common with tricyclic antidepressants), myalgias, parkinsonism, arthralgias, and balance difficulties. Psychological symptoms may also emerge such as agitation, anxiety, akathisia, panic attacks, irritability, aggressiveness, worsening of mood, dysphoria, mood lability, hyperactivity, mania/hypomania, depersonalization, decreased concentration, slowed thinking, confusion, and memory or concentration difficulties. Greater risks for developing a discontinuation syndrome have been associated with antidepressants with shorter half-lives, longer durations of treatment, and abrupt discontinuation.. For antidepressants of short or intermediate half-lives, symptoms may emerge within 2 to 5 days after treatment discontinuation and last 7 to 14 days (APA 2010; Fava 2006; Haddad 2001; Shelton 2001; Warner 2006).
- Electroconvulsive therapy (ECT): Use with caution; no clinical studies have assessed the combined use of citalopram and ECT; may increase the risks (eg, cognitive adverse effects) associated with ECT; consider discontinuing, when possible, prior to ECT treatment.
Monitoring Parameters
ECG (patients at increased risk for QT-prolonging effects due to certain conditions); electrolytes (potassium, and magnesium concentrations [prior to initiation and periodically during therapy in patients at increased risk for electrolyte abnormalities]); liver and renal function tests (baseline; as clinically indicated); serum sodium in at-risk populations (as clinically indicated); CBC (as clinically indicated); suicidal ideation (baseline and with dose changes)
Pregnancy
Pregnancy Risk Factor
C
Pregnancy Considerations
Adverse events have been observed in animal reproduction studies. Citalopram and its metabolites cross the human placenta (Heikkinen, Ekblad, Kero 2002). An increased risk of teratogenic effects, including cardiovascular defects, may be associated with maternal use of citalopram or other SSRIs; however, available information is conflicting. Nonteratogenic effects in the newborn following SSRI/SNRI exposure late in the third trimester include respiratory distress, cyanosis, apnea, seizures, temperature instability, feeding difficulty, vomiting, hypoglycemia, hypo- or hypertonia, hyper-reflexia, jitteriness, irritability, constant crying, and tremor. Symptoms may be due to the toxicity of the SSRIs/SNRIs or a discontinuation syndrome and may be consistent with serotonin syndrome associated with SSRI treatment. Persistent pulmonary hypertension of the newborn (PPHN) has also been reported with SSRI exposure. The long-term effects of in utero SSRI exposure on infant development and behavior are not known.
Due to pregnancy-induced physiologic changes, women who are pregnant may require adjusted doses of citalopram to achieve euthymia (Heikkinen, Ekblad, Kero 2002). The ACOG recommends that therapy with SSRIs or SNRIs during pregnancy be individualized; treatment of depression during pregnancy should incorporate the clinical expertise of the mental health clinician, obstetrician, primary health care provider, and pediatrician. According to the American Psychiatric Association (APA), the risks of medication treatment should be weighed against other treatment options and untreated depression. For women who discontinue antidepressant medications during pregnancy and who may be at high risk for postpartum depression, the medications can be restarted following delivery. Treatment algorithms have been developed by the ACOG and the APA for the management of depression in women prior to conception and during pregnancy (ACOG 2008; APA 2010; Yonkers 2009).
Pregnant women exposed to antidepressants during pregnancy are encouraged to enroll in the National Pregnancy Registry for Antidepressants (NPRAD). Women 18 to 45 years of age or their health care providers may contact the registry by calling 844-405-6185. Enrollment should be done as early in pregnancy as possible.
Patient Education
What is this drug used for?
- It is used to treat low mood (depression).
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Nausea
- Fatigue
- Dry mouth
- Lack of appetite
- Loss of strength and energy
- Trouble sleeping
- Tremors
- Constipation
- Common cold symptoms
- Diarrhea
- Sweating a lot
- Yawning
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Low sodium like headache, difficulty focusing, trouble with memory, confusion, weakness, seizures, or change in balance.
- Depression like thoughts of suicide, anxiety, emotional instability, or confusion.
- Bleeding like vomiting blood or vomit that looks like coffee grounds; coughing up blood; blood in the urine; black, red, or tarry stools; bleeding from the gums; abnormal vaginal bleeding; bruises without a reason or that get bigger; or any severe or persistent bleeding.
- Agitation
- Panic attacks
- Mood changes
- Chest pain
- Fast heartbeat
- Abnormal heartbeat
- Slow heartbeat
- Shortness of breath
- Dizziness
- Passing out
- Seizures
- Sexual dysfunction
- Weight gain
- Weight loss
- Menstrual changes
- Vision changes
- Eye pain
- Eye irritation
- Serotonin syndrome like dizziness, severe headache, agitation, sensing things that seem real but are not, fast heartbeat, abnormal heartbeat, flushing, tremors, sweating a lot, change in balance, severe nausea, or severe diarrhea.
- Erection that lasts more than 4 hours
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.