Boxed Warning
Risks from concomitant use of benzodiazepines and opioids:
Concomitant use of benzodiazepines and opioids may result in profound sedation, respiratory depression, coma, and death. Reserve concomitant prescribing of these drugs for use in patients for whom alternative treatment options are inadequate. Limit dosages and durations to the minimum required. Follow patients for signs and symptoms of respiratory depression and sedation.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Film, Oral:
Sympazan: 5 mg (1 ea, 60 ea); 10 mg (1 ea, 60 ea); 20 mg (1 ea, 60 ea)
Suspension, Oral:
Onfi: 2.5 mg/mL (120 mL) [contains methylparaben, polysorbate 80, propylene glycol, propylparaben; berry flavor]
Generic: 2.5 mg/mL (120 mL)
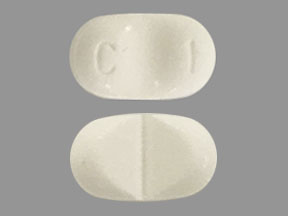
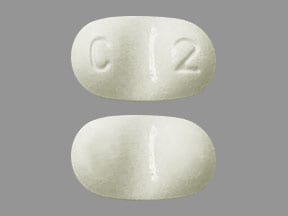
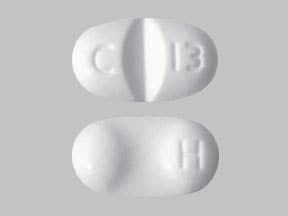
Tablet, Oral:
Onfi: 10 mg, 20 mg [scored; contains corn starch]
Generic: 10 mg, 20 mg
Pharmacology
Mechanism of Action
Clobazam is a 1,5 benzodiazepine which binds to stereospecific benzodiazepine receptors on the postsynaptic GABA neuron at several sites within the central nervous system, including the limbic system, reticular formation. Enhancement of the inhibitory effect of GABA on neuronal excitability results by increased neuronal membrane permeability to chloride ions. This shift in chloride ions results in hyperpolarization (a less excitable state) and stabilization. Benzodiazepine receptors and effects appear to be linked to the GABA-A receptors. Benzodiazepines do not bind to GABA-B receptors (Vinkers 2012).
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid and extensive; not affected by food or crushing tablet
Distribution
100 L
Metabolism
Hepatic via CYP3A4 and to a lesser extent via CYP2C19 and 2B6 (N-demethylation to active metabolite [N-desmethyl] with ~20% activity of clobazam). CYP2C19 primarily mediates subsequent hydroxylation of the N-desmethyl metabolite; metabolic rate increased in children (53% to 69%) (Ng 2007). Plasma concentrations of NCLB are 5 times higher in CYP2C19 poor metabolizers versus extensive metabolizers.
Excretion
Urine (~82%; unchanged drug: 2%, NCLB and other metabolites: ~94%); feces (~11%; 1% unchanged drug)
Onset of Action
Maximum effect: 5 to 9 days
Time to Peak
Oral film: 0.33 to 4 hours; Tablet: 0.5 to 4 hours; Oral suspension: 0.5 to 2 hours
Half-Life Elimination
Children: Clobazam: 16 hours (Ng 2007); Adults: Clobazam: 36 to 42 hours; N-desmethyl (active): 71 to 82 hours
Protein Binding
Clobazam: 80% to 90%; N-desmethylclobazam (NCLB): 70%
Use in Specific Populations
Special Populations: Elderly
Clearance is lower in elderly patients.
Special Populations Note
CYP2C19 poor metabolizers: AUC and Cmax of active metabolite are ~3 to 5 times higher in poor metabolizers compared with extensive metabolizers and ~2 times higher in intermediate metabolizers.
Use: Labeled Indications
Lennox-Gastaut syndrome: Adjunctive treatment of seizures associated with Lennox-Gastaut syndrome in patients ≥2 years
Use: Off Label
Catamenial epilepsyc
Data from a limited number of patients studied suggest that clobazam may be beneficial for the treatment of catamenial epilepsy Feely 1984. Additional data may be necessary to further define the role of clobazam in this condition.
Seizures, treatment refractory (adjunctive)byes
Data from a limited number of patients studied in 4 randomized, double-blind, placebo-controlled cross-over trials support the use of clobazam as an adjunctive therapy in treatment refractory epilepsy. More data exist to support use in patients with focal (partial)-onset seizures than for patients with generalized onset seizures Michael 2008.
Based on the American Academy of Neurology and the American Epilepsy Society practice guideline update summary on the efficacy and tolerability of the new antiepileptic drugs II: treatment-resistant epilepsy, clobazam is possibly effective as add-on therapy for treatment-resistant adult focal epilepsy.
Contraindications
Hypersensitivity to clobazam or any component of the formulation.
Canadian labeling: Additional contraindications (not in US labeling): Myasthenia gravis; narrow-angle glaucoma; severe hepatic or respiratory disease; sleep apnea; history of substance abuse; use in the first trimester of pregnancy; breast-feeding
Dosage and Administration
Dosing: Adult
Catamenial epilepsy (off-label use): Oral: 20 to 30 mg daily for 10 days during the perimenstrual period (Feely 1984).
Lennox-Gastaut (adjunctive): Oral: Initial: 5 mg twice daily for ≥1 week, then increase based on response and tolerability to 10 mg twice daily for ≥1 week, then increase to 20 mg twice daily thereafter.
CYP2C19 poor metabolizers: Initial: 5 mg once daily for ≥1 week, then increase based on response and tolerability to 5 mg twice daily for ≥1 week, then increase to 10 mg twice daily; after ≥1 week may increase to 20 mg twice daily.
Seizures, treatment refractory (adjunctive; off-label): Oral: Initial: 5 to 15 mg/day; may gradually increase based on response and tolerability to 40 mg/day (Koeppen 1987; Schmidt 1986). Alternatively, a maximum dose of 80 mg/day has also been recommended (Canadian manufacturer's labeling). Daily doses of up to 30 mg may be taken as a single dose at bedtime; higher doses should be divided (Allen 1983; Canadian manufacturer's labeling).
CYP2C19 poor metabolizers: Initiate at lowest recommended doses; titrate slowly as tolerated to half of usual recommended maximum dose. If needed, dose may be further increased as tolerated to usual recommended maximum dose beginning day 21 (Canadian manufacturer's labeling).
Discontinuation of therapy: Withdraw gradually by decreasing the total daily dosage by 5 to 10 mg/day on a weekly basis until discontinued.
Dosing: Geriatric
Lennox-Gastaut (adjunctive): Oral: Initial: 5 mg once daily for ≥1 week, then increase to 5 mg twice daily for ≥1 week, then increase to 10 mg twice daily; after ≥1 week may increase to 20 mg twice daily based on patient tolerability and response; maximum 40 mg/day.
Discontinuation of therapy: See adult dosing.
Dosing: Pediatric
Note: Dosage should be titrated according to patient tolerability and response.
Lennox-Gastaut syndrome: Children ≥2 years and Adolescents: Oral:
≤30 kg: Initial: 5 mg once daily for ≥1 week, may then increase to 5 mg twice daily for ≥1 week, then increase to 10 mg twice daily thereafter (maximum daily dose: 20 mg/day)
>30 kg: Initial: 5 mg twice daily for ≥1 week, may then increase to 10 mg twice daily for ≥1 week, then increase to 20 mg twice daily thereafter (maximum daily dose: 40 mg/day)
Seizures, generalized or partial, monotherapy or adjunctive therapy: Limited data available (Frisium prescribing information [U.K.; Canada] 2011; Canadian Study Group 1998; Ng 2007):
Infants and Children <2 years: Oral: Initial: 0.5 to 1 mg/kg/day usually in divided doses twice daily; maximum initial daily dose: 5 mg/day; may increase dosage slowly (not more often than every 5 to 7 days); maximum daily dose: 10 mg/day
Children 2 to 16 years: Oral: Initial: 5 mg once daily; may increase dosage slowly (not more often than every 5 days), usual range: 10 to 20 mg/day or 0.3 to 1 mg/kg/day in divided doses twice daily; maximum daily dose: 40 mg/day
Discontinuation of therapy: Children ≥2 years and Adolescents: Withdraw gradually by decreasing the total daily dosage by 5 to 10 mg/day on a weekly basis until discontinued.
Dosage adjustment for CYP2C19 poor metabolizers: Children ≥2 years and Adolescents:
≤30 kg: Initial: 5 mg once daily for ≥1 week, then increase to 5 mg twice daily for ≥1 week, may then increase to 10 mg twice daily based on patient tolerability and response
>30 kg: Initial: 5 mg once daily for ≥1 week, then increase to 5 mg twice daily for ≥1 week, then increase to 10 mg twice daily for ≥1 week, may then increase to 20 mg twice daily based on patient tolerability and response
Administration
Administer with or without food. Daily doses >5 mg should be divided and administered twice daily.
Oral film: Apply one oral film on top of tongue where it dissolves. Do not take more than one film at a time. If a second film is needed, apply on top of tongue after the first film completely dissolves. Do not administer with liquids; swallow in a normal manner as the film dissolves; do not chew, spit, or talk as the film dissolves.
Suspension: Shake suspension well before using; only use the oral dosing syringe supplied with the suspension.
Tablets: Tablets can be broken in half or crushed and mixed in applesauce.
Storage
Oral film: Store at 20°C to 25°C (68°F to 77°F); excursions permitted to 15°C to 30°C (59°F to 86°F).
Suspension, tablet: Store at 20°C to 25°C (68°F to 77°F). Dispose of unused suspension 90 days after opening bottle.
Clobazam Images
Drug Interactions
Alcohol (Ethyl): May enhance the CNS depressant effect of CloBAZam. Alcohol (Ethyl) may increase the serum concentration of CloBAZam. Monitor therapy
Alizapride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
ARIPiprazole: CYP2D6 Inhibitors (Weak) may increase the serum concentration of ARIPiprazole. Management: Monitor for increased aripiprazole pharmacologic effects. Aripiprazole dose adjustments may or may not be required based on concomitant therapy and/or indication. Consult full interaction monograph for specific recommendations. Monitor therapy
Azelastine (Nasal): CNS Depressants may enhance the CNS depressant effect of Azelastine (Nasal). Avoid combination
Blonanserin: CNS Depressants may enhance the CNS depressant effect of Blonanserin. Consider therapy modification
Brexanolone: CNS Depressants may enhance the CNS depressant effect of Brexanolone. Monitor therapy
Brimonidine (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromopride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromperidol: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Buprenorphine: CNS Depressants may enhance the CNS depressant effect of Buprenorphine. Management: Consider reduced doses of other CNS depressants, and avoiding such drugs in patients at high risk of buprenorphine overuse/self-injection. Initiate buprenorphine at lower doses in patients already receiving CNS depressants. Consider therapy modification
Cannabidiol: May increase serum concentrations of the active metabolite(s) of CloBAZam. Cannabidiol may increase the serum concentration of CloBAZam. Monitor therapy
Cannabis: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Chlormethiazole: May enhance the CNS depressant effect of CNS Depressants. Management: Monitor closely for evidence of excessive CNS depression. The chlormethiazole labeling states that an appropriately reduced dose should be used if such a combination must be used. Consider therapy modification
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
CloZAPine: Benzodiazepines may enhance the adverse/toxic effect of CloZAPine. Management: Consider decreasing the dose of (or possibly discontinuing) benzodiazepines prior to initiating clozapine. Consider therapy modification
CNS Depressants: May enhance the adverse/toxic effect of other CNS Depressants. Monitor therapy
CYP2C19 Inducers (Moderate): May decrease the serum concentration of CYP2C19 Substrates (High risk with Inducers). Monitor therapy
CYP2C19 Inducers (Strong): May increase the metabolism of CYP2C19 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
CYP2C19 Inhibitors (Moderate): May decrease the metabolism of CYP2C19 Substrates (High risk with Inhibitors). Monitor therapy
CYP2C19 Inhibitors (Strong): May decrease the metabolism of CYP2C19 Substrates (High risk with Inhibitors). Consider therapy modification
CYP2D6 Substrates (High risk with Inhibitors): CloBAZam may increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Dabrafenib: May decrease the serum concentration of CYP2C19 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP2C19 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dimethindene (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Doxylamine: May enhance the CNS depressant effect of CNS Depressants. Management: The manufacturer of Diclegis (doxylamine/pyridoxine), intended for use in pregnancy, specifically states that use with other CNS depressants is not recommended. Monitor therapy
Dronabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Droperidol: May enhance the CNS depressant effect of CNS Depressants. Management: Consider dose reductions of droperidol or of other CNS agents (eg, opioids, barbiturates) with concomitant use. Exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Consider therapy modification
Enzalutamide: May decrease the serum concentration of CYP2C19 Substrates (High risk with Inducers). Conversely, concentrations of active metabolites may be increased for those drugs activated by CYP2C19. Management: Concurrent use of enzalutamide with CYP2C19 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP2C19 substrate should be performed with caution and close monitoring. Consider therapy modification
Esketamine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Estrogen Derivatives (Contraceptive): CloBAZam may decrease the serum concentration of Estrogen Derivatives (Contraceptive). Consider therapy modification
Flunitrazepam: CNS Depressants may enhance the CNS depressant effect of Flunitrazepam. Consider therapy modification
Fosphenytoin: Benzodiazepines may increase the serum concentration of Fosphenytoin. Short-term exposure to benzodiazepines may not present as much risk as chronic therapy. Monitor therapy
HYDROcodone: CNS Depressants may enhance the CNS depressant effect of HYDROcodone. Management: Avoid concomitant use of hydrocodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
HydrOXYzine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Kava Kava: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Lemborexant: May enhance the CNS depressant effect of CNS Depressants. Management: Dosage adjustments of lemborexant and of concomitant CNS depressants may be necessary when administered together because of potentially additive CNS depressant effects. Close monitoring for CNS depressant effects is necessary. Consider therapy modification
Lofexidine: May enhance the CNS depressant effect of CNS Depressants. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Lumacaftor and Ivacaftor: May decrease the serum concentration of CYP2C19 Substrates (High risk with Inducers). Monitor therapy
Magnesium Sulfate: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Melatonin: May enhance the sedative effect of Benzodiazepines. Monitor therapy
Methadone: Benzodiazepines may enhance the CNS depressant effect of Methadone. Management: Clinicians should generally avoid concurrent use of methadone and benzodiazepines when possible; any combined use should be undertaken with extra caution. Consider therapy modification
Methotrimeprazine: CNS Depressants may enhance the CNS depressant effect of Methotrimeprazine. Methotrimeprazine may enhance the CNS depressant effect of CNS Depressants. Management: Reduce adult dose of CNS depressant agents by 50% with initiation of concomitant methotrimeprazine therapy. Further CNS depressant dosage adjustments should be initiated only after clinically effective methotrimeprazine dose is established. Consider therapy modification
MetyroSINE: CNS Depressants may enhance the sedative effect of MetyroSINE. Monitor therapy
Minocycline (Systemic): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Nabilone: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
NiMODipine: CYP3A4 Inducers (Weak) may decrease the serum concentration of NiMODipine. Monitor therapy
OLANZapine: May enhance the adverse/toxic effect of Benzodiazepines. Management: Avoid concomitant use of parenteral benzodiazepines and IM olanzapine due to risks of additive adverse events (e.g., cardiorespiratory depression). Olanzapine prescribing information provides no specific recommendations regarding oral administration. Avoid combination
Omeprazole: May increase serum concentrations of the active metabolite(s) of CloBAZam. Monitor therapy
Opioid Agonists: CNS Depressants may enhance the CNS depressant effect of Opioid Agonists. Management: Avoid concomitant use of opioid agonists and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Orphenadrine: CNS Depressants may enhance the CNS depressant effect of Orphenadrine. Avoid combination
Oxomemazine: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
OxyCODONE: CNS Depressants may enhance the CNS depressant effect of OxyCODONE. Management: Avoid concomitant use of oxycodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Paraldehyde: CNS Depressants may enhance the CNS depressant effect of Paraldehyde. Avoid combination
Perampanel: May enhance the CNS depressant effect of CNS Depressants. Management: Patients taking perampanel with any other drug that has CNS depressant activities should avoid complex and high-risk activities, particularly those such as driving that require alertness and coordination, until they have experience using the combination. Consider therapy modification
Perhexiline: CYP2D6 Inhibitors (Weak) may increase the serum concentration of Perhexiline. Monitor therapy
Phenytoin: Benzodiazepines may increase the serum concentration of Phenytoin. Short-term exposure to benzodiazepines may not present as much risk as chronic therapy. Monitor therapy
Piribedil: CNS Depressants may enhance the CNS depressant effect of Piribedil. Monitor therapy
Pramipexole: CNS Depressants may enhance the sedative effect of Pramipexole. Monitor therapy
Progestins (Contraceptive): CloBAZam may decrease the serum concentration of Progestins (Contraceptive). Consider therapy modification
ROPINIRole: CNS Depressants may enhance the sedative effect of ROPINIRole. Monitor therapy
Rotigotine: CNS Depressants may enhance the sedative effect of Rotigotine. Monitor therapy
Rufinamide: May enhance the adverse/toxic effect of CNS Depressants. Specifically, sleepiness and dizziness may be enhanced. Monitor therapy
Selective Serotonin Reuptake Inhibitors: CNS Depressants may enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk of psychomotor impairment may be enhanced. Monitor therapy
Sodium Oxybate: Benzodiazepines may enhance the CNS depressant effect of Sodium Oxybate. Avoid combination
Stiripentol: CloBAZam may increase the serum concentration of Stiripentol. Stiripentol may increase the serum concentration of CloBAZam. Monitor therapy
Suvorexant: CNS Depressants may enhance the CNS depressant effect of Suvorexant. Management: Dose reduction of suvorexant and/or any other CNS depressant may be necessary. Use of suvorexant with alcohol is not recommended, and the use of suvorexant with any other drug to treat insomnia is not recommended. Consider therapy modification
Tapentadol: May enhance the CNS depressant effect of CNS Depressants. Management: Avoid concomitant use of tapentadol and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Teduglutide: May increase the serum concentration of Benzodiazepines. Monitor therapy
Tetrahydrocannabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Thalidomide: CNS Depressants may enhance the CNS depressant effect of Thalidomide. Avoid combination
Theophylline Derivatives: May diminish the therapeutic effect of Benzodiazepines. Consider therapy modification
Trimeprazine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Ubrogepant: CYP3A4 Inducers (Weak) may decrease the serum concentration of Ubrogepant. Management: Use an initial ubrogepant dose of 100 mg and second dose (if needed) of 100 mg when used with a weak CYP3A4 inducer. Consider therapy modification
Yohimbine: May diminish the therapeutic effect of Antianxiety Agents. Monitor therapy
Zolpidem: CNS Depressants may enhance the CNS depressant effect of Zolpidem. Management: Reduce the Intermezzo brand sublingual zolpidem adult dose to 1.75 mg for men who are also receiving other CNS depressants. No such dose change is recommended for women. Avoid use with other CNS depressants at bedtime; avoid use with alcohol. Consider therapy modification
Adverse Reactions
>10%:
Central nervous system: Drowsiness (16% to 25%), lethargy (10% to 15%), drooling (13% to 14%), aggressive behavior (8% to 14%), irritability (11%)
Respiratory: Upper respiratory tract infection (13% to 14%)
Miscellaneous: Fever (10% to 17%)
1% to 10%:
Central nervous system: Ataxia (10%), sedation (9%), insomnia (5% to 7%), psychomotor agitation (5%), fatigue (3% to 5%), dysarthria (2% to 5%)
Gastrointestinal: Constipation (2% to 10%), vomiting (7% to 9%), decreased appetite (7%), increased appetite (2% to 5%), dysphagia (5%)
Genitourinary: Urinary tract infection (2% to 5%)
Respiratory: Cough (3% to 7%), pneumonia (3% to 7%), bronchitis (2% to 5%)
Postmarketing and/or case reports: Abdominal distention, agitation, anemia, angioedema, anxiety, apathy, behavioral changes, blurred vision, confusion, delirium, delusions, depression, diplopia, eosinophilia, facial edema, hallucination, hypothermia, increased liver enzymes, leukopenia, lip edema, mood changes, muscle spasm, pulmonary aspiration, respiratory depression, skin rash, Stevens-Johnson syndrome, suicidal ideation, suicidal tendencies, thrombocytopenia, toxic epidermal necrolysis, urinary retention, urticaria, withdrawal syndrome
Warnings/Precautions
Concerns related to adverse effects:
- Anterograde amnesia: Benzodiazepines have been associated with anterograde amnesia (Nelson 1999).
- CNS depression: May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks which require mental alertness (eg, operating machinery or driving).
- Paradoxical reactions: Paradoxical reactions, including hyperactive or aggressive behavior, have been reported with benzodiazepines; risk may be increased in adolescent/pediatric patients, geriatric patients, or patients with a history of alcohol use disorder or psychiatric/personality disorders (Mancusco 2004).
- Skin reactions: Serious reactions, including Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN), have been reported. Monitor patients closely for signs and symptoms (eg, burning sensation, pleomorphic rash, petechiae, vesicles, bullae) especially during the first 8 weeks or when reintroducing therapy. Permanently discontinue immediately if rash is suggestive of SJS/TEN.
- Sleep-related activities: Hazardous sleep-related activities such as sleep-driving, cooking and eating food, and making phone calls while asleep have been noted with benzodiazepines (Dolder 2008).
- Suicidal ideation: Pooled analysis of trials involving various antiepileptics (regardless of indication) showed an increased risk of suicidal thoughts/behavior (incidence rate: 0.43% treated patients compared to 0.24% of patients receiving placebo); risk observed as early as 1 week after initiation and continued through duration of trials (most trials ≤24 weeks). Monitor all patients for notable changes in behavior that might indicate suicidal thoughts or depression; notify health care provider immediately if symptoms occur.
Disease-related concerns:
- Drug abuse: Use with caution in patients with a history of drug abuse or acute alcoholism; potential for drug dependency exists. Psychological and physical dependence, as well as tolerance to sedative and anticonvulsive effects, may occur with prolonged use (Vinkers 2012).
- Hepatic impairment: Use with caution in patients with hepatic impairment; dose adjustment may be necessary.
Concurrent drug therapy issues:
- Benzodiazepines and opioids: [US Boxed Warning]: The concomitant use of benzodiazepines and opioids may result in profound sedation, respiratory depression, coma, and death. Reserve concomitant prescribing of these drugs for use in patients for whom alternative treatment options are inadequate. Limit dosages and durations to the minimum required. Follow patients for signs and symptoms of respiratory depression and sedation.
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Elderly: Lower doses are recommended. Elderly patients may be at an increased risk of death with use; risk has been found highest within the first 4 months of use in elderly dementia patients (Jennum 2015; Saarelainen 2018).
- Fall risk: Use with extreme caution in patients who are at risk of falls; benzodiazepines have been associated with falls and traumatic injury (Nelson 1999).
- Poor CYP2C19 metabolizers: Concentrations of the active metabolite are 3 to 5 times higher in patients who are known CYP2C19 poor metabolizers compared to CYP2C19 extensive metabolizers. Dose adjustment is needed in patients who are poor CYP2C19 metabolizers.
Other warnings/precautions:
- Appropriate use: Does not have analgesic, antidepressant, or antipsychotic properties.
- Chronic use: Tolerance to anticonvulsive effects and loss of seizure control have been reported with chronic administration.
- Withdrawal: Rebound or withdrawal symptoms may occur following abrupt discontinuation or large decreases in dose. Use caution when reducing dose or withdrawing therapy; decrease slowly (eg, decrease weekly by 5 to 10 mg/day) and monitor for withdrawal symptoms. Flumazenil may cause withdrawal in patients receiving long-term benzodiazepine therapy.
Monitoring Parameters
Respiratory and mental status/suicidality (eg, suicidal thoughts, depression, behavioral changes); serious skin reactions (Stevens Johnson Syndrome, toxic epidermal necrolysis) during treatment initiation or reintroduction of therapy.
Pregnancy
Pregnancy Considerations
Clobazam crosses the placenta.
An increased risk of fetal malformations may be associated with first trimester benzodiazepine exposure (data not consistent). Exposure to benzodiazepines immediately prior to or during birth may result in hypothermia, hypotonia, respiratory depression, and difficulty feeding in the neonate; neonates exposed to benzodiazepines late in pregnancy may develop dependence and withdrawal. The incidence of premature birth and low birth weights may be increased following maternal use of benzodiazepines; hypoglycemia and respiratory problems in the neonate may occur following exposure late in pregnancy. Neonatal withdrawal symptoms may occur within days to weeks after birth and “floppy infant syndrome” (which also includes withdrawal symptoms) has been reported with some benzodiazepines (Bergman 1992; Iqbal 2002; Wikner 2007). A combination of factors influences the potential teratogenicity of anticonvulsant therapy. When treating women with epilepsy, monotherapy with the lowest effective dose and avoidance medications known to have a high incidence of teratogenic effects is recommended (Harden 2009; Wlodarczyk 2012).
Patients exposed to clobazam during pregnancy are encouraged to enroll themselves into the North American Antiepileptic Drug (NAAED) Pregnancy Registry by calling 1-888-233-2334. Additional information is available at www.aedpregnancyregistry.org.
Patient Education
What is this drug used for?
- It is used to help control certain kinds of seizures.
Frequently reported side effects of this drug
- Drooling
- Constipation
- Lack of appetite
- Increased appetite
- Common cold symptoms
- Trouble sleeping
- Cough
- Vomiting
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Urinary tract infection like blood in the urine, burning or painful urination, passing a lot of urine, fever, lower abdominal pain, or pelvic pain.
- Shortness of breath
- Change in balance
- Confusion
- Severe loss of strength and energy
- Slurred speech
- Seizures
- Passing out
- Severe dizziness
- Severe fatigue
- Depression like thoughts of suicide, anxiety, emotional instability, or confusion.
- Agitation
- Irritability
- Panic attacks
- Mood changes
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.