Boxed Warning
Epidural use:
The 500 mcg/mL strength product should be diluted prior to use in an appropriate solution.
Note: Epidural clonidine is not recommended for obstetrical, postpartum, or perioperative pain management. The risk of hemodynamic instability, especially hypotension and bradycardia, from epidural clonidine may be unacceptable in these patients. However, in a rare obstetrical, postpartum or perioperative patient, potential benefits may outweigh the possible risks.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Patch Weekly, Transdermal:
Catapres-TTS-1: 0.1 mg/24 hr (4 ea)
Catapres-TTS-2: 0.2 mg/24 hr (4 ea)
Catapres-TTS-3: 0.3 mg/24 hr (4 ea)
Generic: 0.1 mg/24 hr (1 ea, 4 ea); 0.2 mg/24 hr (1 ea, 4 ea); 0.3 mg/24 hr (1 ea, 4 ea)
Solution, Epidural, as hydrochloride:
Duraclon: 100 mcg/mL (10 mL [DSC])
Solution, Epidural, as hydrochloride [preservative free]:
Duraclon: 100 mcg/mL (10 mL)
Duraclon: 500 mcg/mL (10 mL [DSC]) [pyrogen free]
Generic: 100 mcg/mL (10 mL); 500 mcg/mL (10 mL)
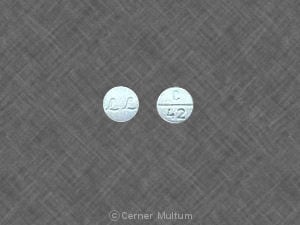
Tablet, Oral, as hydrochloride:
Catapres: 0.1 mg [scored; contains brilliant blue fcf (fd&c blue #1), corn starch, fd&c yellow #6 (sunset yellow)]
Catapres: 0.2 mg, 0.3 mg [scored; contains corn starch, fd&c yellow #6 (sunset yellow)]
Generic: 0.1 mg, 0.2 mg, 0.3 mg
Tablet Extended Release 12 Hour, Oral, as hydrochloride:
Kapvay: 0.1 mg
Generic: 0.1 mg
Pharmacology
Mechanism of Action
Stimulates alpha-2 adrenoceptors in the brain stem, thus activating an inhibitory neuron, resulting in reduced sympathetic outflow from the CNS, producing a decrease in peripheral resistance, renal vascular resistance, heart rate, and blood pressure; epidural clonidine may produce pain relief at spinal presynaptic and postjunctional alpha-2 adrenoceptors by preventing pain signal transmission; pain relief occurs only for the body regions innervated by the spinal segments where analgesic concentrations of clonidine exist. For the treatment of ADHD, the mechanism of action is unknown; it has been proposed that postsynaptic alpha-2 agonist stimulation regulates subcortical activity in the prefrontal cortex, the area of the brain responsible for emotions, attentions, and behaviors and causes reduced hyperactivity, impulsiveness, and distractibility. Epidurally administered clonidine produces dose-dependent analgesia not antagonized by opiate antagonists. The analgesia is limited to the body regions innervated by the spinal segments where analgesic concentrations of clonidine are present. Clonidine is thought to produce analgesia at presynaptic and postjunctional alpha-2 adrenoceptors in the spinal cord by preventing pain signal transmission to the brain.
Pharmacokinetics/Pharmacodynamics
Absorption
Oral: Extended-release tablets (Kapvay) are not bioequivalent with immediate-release formulations; peak plasma concentrations are 50% lower compared to immediate-release formulations
Distribution
Vd: ~2.9 L/kg; highly lipid soluble; distributes readily into extravascular sites; Note: Epidurally administered clonidine readily distributes into plasma via the epidural veins and attains clinically significant systemic concentrations.
Metabolism
Extensively hepatic to inactive metabolites; undergoes enterohepatic recirculation
Excretion
Urine (40% to 60% as unchanged drug)
Clearance: Oral:
Neonates: 0.16 L/kg/hour (Xie 2011)
Infants and Children ≤4 years: ~0.3 L/kg/hour (Xie 2011)
Children 5 to10 years: ~0.26 L/kg/hour (Xie 2011)
Adults: Single dose: ~0.25 L/kg/hour; Multiple dose: ~0.4 L/kg/hour (Frisk-Holmberg 1981)
Onset of Action
Antihypertensive effect: Oral: Immediate release: 0.5 to 1 hour (maximum reduction in blood pressure: 2 to 4 hours); Transdermal: Initial application: 2 to 3 days; Transdermal: Steady state reached in ~3 days
Attention-deficit/hyperactivity disorder: Oral: Extended release (Kapvay): Onset of action: 1 to 2 weeks (AAP [Wolraich 2011])
Time to Peak
Plasma: Oral: Immediate release: 1 to 3 hours; Extended release (Kapvay): 7 to 8 hours
Half-Life Elimination
Children: 6.13 ± 1.33 hours (Lonnqvist 1993)
Adults: Normal renal function: 12 to 16 hours; Renal impairment: ≤41 hours
Epidural administration: CSF half-life elimination: 1.3 ± 0.5 hours; plasma half-life elimination: 22 ± 15 hours
Transdermal: Half-life elimination (after patch removal): ~20 hours (due to skin depot effect; increase in plasma clonidine concentrations may occur after patch removal [MacGregor 1985])
Protein Binding
20% to 40%
Use in Specific Populations
Special Populations: Renal Function Impairment
The half-life increases up to 41 hours in patients with severe renal impairment.
Use: Labeled Indications
Attention-deficit/hyperactivity disorder (extended-release tablet): Treatment of attention-deficit/hyperactivity disorder (monotherapy or as adjunctive therapy)
Hypertension (immediate-release tablet and transdermal patch): Management of hypertension. Note: Not recommended for the initial treatment of hypertension (ACC/AHA [Whelton 2018]). Clonidine should be avoided for the treatment of hypertension in patients with heart failure with reduced ejection fraction of ischemic origin (AHA/ACC/ASH [Rosendorff 2015]).
Use: Off Label
ICU sedation, transition from dexmedetomidine to clonidinec
Data from 2 single-center studies (one retrospective, one prospective) in ICU patients receiving dexmedetomidine suggest clonidine is safe and effective to transition patients off dexmedetomidine. Clonidine should be discontinued prior to hospital discharge Gagnon 2015, Terry 2015. Additional trials may be necessary to further define the potential cost savings of this therapy.
Opioid withdrawal, medically supervisedbyes
Data from a meta-analysis of alpha2-agonists for the management of opioid withdrawal support the use of alpha2-agonists such as clonidine for decreasing the severity and duration of opioid withdrawal compared to placebo Gowing 2016.
Based on the
Contraindications
Hypersensitivity to clonidine hydrochloride or any component of the formulation.
Epidural administration: Injection site infection; concurrent anticoagulant therapy; bleeding diathesis; administration above the C4 dermatome.
Canadian labeling: Additional contraindications (not in US labeling): Severe bradyarrhythmia from second- or third-degree atrioventricular block or sick sinus syndrome; sinus node dysfunction; hereditary problems of galactose intolerance (eg, galactosemia).
Dosage and Administration
Dosing: Adult
Note: Safety: Do not discontinue therapy abruptly. When discontinuing, taper gradually to decrease risk of withdrawal symptoms (eg, rebound hypertension) (see Discontinuation of therapy below for additional information). Dosage forms: Oral doses are expressed as clonidine hydrochloride, whereas transdermal patch doses are expressed as clonidine base. Accordingly, due to differences in bioavailability, oral doses cannot be converted directly to a transdermal patch. For conversions, see Transitioning between dosage forms below. In addition, immediate-release tablets should not be interchanged with extended-release formulations due to different pharmacokinetic profiles.
Hypertension (alternative agent): Note: Not recommended for initial management but may be considered as additional therapy for resistant hypertension in patients who do not respond adequately to combination therapy with preferred agents (ACC/AHA [Whelton 2018]).
Oral: Immediate release: Initial: 0.1 mg twice daily; increase dose in increments of 0.1 mg/day at weekly intervals based on response and tolerability; usual dose range: 0.2 to 0.6 mg/day in 2 divided doses. The manufacturer's labeling includes a maximum daily dose of 2.4 mg; however, doses >0.6 mg/day are generally not used.
Transdermal: Initial: 0.1 mg/24-hour patch applied once every 7 days; increase by 0.1 mg at 1- to 2-week intervals; usual dose range: 0.1 to 0.3 mg/24-hour patch applied once every 7 days. Onset of effect is delayed for 2 to 3 days following initial application.
Note: In patients undergoing surgery, maintenance dose is generally continued perioperatively to avoid rebound hypertension associated with abrupt withdrawal. It may be appropriate to transition to a transdermal patch ≥3 days before surgery in select patients who are not expected to resume enteral medication ≤12 hours after surgery. See Transitioning between dosage forms below (Muluk 2019).
ICU sedation, transition from dexmedetomidine to clonidine (off-label use): Note: Consider use in patients who are hemodynamically stable and able to receive medications enterally. Monitor blood pressure and heart rate during initiation and transition (Gagnon 2015).
Oral: Immediate release:
Initial: Note: Decrease dexmedetomidine dose by 25% within 6 hours of each clonidine dose. Dexmedetomidine can usually be stopped within 48 hours.
Dexmedetomidine dose <0.7 mcg/kg/hour: 0.1 to 0.2 mg every 6 to 8 hours (Gagnon 2015; Gagnon 2017).
Dexmedetomidine dose ≥0.7 mcg/kg/hour: 0.3 mg every 6 to 8 hours (Gagnon 2015; Gagnon 2017).
Maintenance: Titrate to achieve target sedation levels to a usual dosage range of 0.2 to 0.5 mg every 6 hours (Gagnon 2015). Gradually taper clonidine by extending the dosing interval every 24 to 48 hours (Gagnon 2015; Gagnon 2017; Terry 2015).
Opioid withdrawal, medically supervised (adjunctive or alternative agent) (off-label use): Note: Adjunct to opioid agonist for relief of withdrawal symptoms. May also be used as primary treatment when opioid agonist therapy is not indicated or not available. May be combined with other adjunctive medications as needed. To assess severity of withdrawal symptoms and adjust therapy, the use of a standard instrument for scoring of clinical observations (eg, Clinical Opioid Withdrawal Scale) is suggested (APA [Kleber 2006]; ASAM [Kampman 2015]; Stolbach 2019).
Oral: Immediate release:
Initial: 0.1 to 0.2 mg (patients >90 kg may receive up to 0.3 mg); may repeat every 45 to 60 minutes if needed, up to a total of 4 doses until symptoms resolve, provided blood pressure and heart rate remain stable; maximum dose: typically, 0.8 mg/day or up to 1.2 mg/day for patients >90 kg (APA [Kleber 2006]; Sevarino 2019; Stolbach 2019).
Maintenance: 0.1 to 0.3 mg every 6 to 8 hours determined by symptom severity; maximum dose: 1.2 mg/day in divided doses (ASAM [Kampman 2015]).
Note: After a stable oral dose is established, may transition to an equivalent dose of a transdermal patch (see Transitioning between dosage forms below); according to some institutional protocols, may initiate therapy with a transdermal patch in select patients (APA [Kleber 2006]; ASAM [Kampman 2015]; Gowing 2016; Sevarino 2019).
Transitioning between dosage forms:
Transition from oral to transdermal:Note: If transitioning from oral to transdermal therapy, overlap oral regimen for 1 to 3 days; transdermal route takes 2 to 3 days to achieve therapeutic effect.
An example transition is below:
Day 1: Place transdermal patch; administer 100% of oral dose.
Day 2: Patch remains; administer 50% of oral dose.
Day 3: Patch remains; administer 25% of oral dose.
Day 4: Patch remains; no further oral dosing.
Transition from transdermal to oral:After transdermal patch removal, therapeutic clonidine levels persist for ~8 hours and then slowly decrease over several days, with a potential for continued effect for 24 to 48 hours after removal. A persistent effect on blood pressure should be considered when restarting oral clonidine. Consider starting oral clonidine no sooner than 8 hours after patch removal (Muluk 2019).
Discontinuation of therapy: Do not stop oral therapy abruptly to decrease risk of rebound hypertension and other withdrawal symptoms (eg, nervousness, agitation, headache, tremor); discontinue slowly over 6 to 10 days by reducing the dose by one-third to one-half every 2 to 3 days. For patients on both a beta-blocker and clonidine, withdraw the beta-blocker several days before clonidine, then slowly taper clonidine. Rebound hypertension and withdrawal symptoms are less likely with a transdermal patch compared to oral therapy (Elliott 2019; Houston 1981). Note: Clonidine administration is generally not interrupted during the perioperative period (Muluk 2019).
Dosing: Geriatric
Hypertension: Oral: Immediate release: Initial: 0.1 mg once daily at bedtime, increase gradually as needed.
Dosing: Pediatric
Note: Dosing is expressed as the salt (clonidine hydrochloride) unless otherwise noted. Formulations of clonidine (immediate release vs extended release) are not interchangeable on a mg per mg basis due to different pharmacokinetic profiles. Compounded oral suspensions may be available in multiple concentrations (eg, up to a 10-times more concentrated); precautions should be taken to verify and avoid confusion between the different concentrations; dose should be clearly presented as mcg or mg as appropriate.
Attention-deficit/hyperactivity disorder (ADHD):
Oral:
Immediate release: Limited data available (Pliszka 2007):
Children ≥6 years and Adolescents:
≤45 kg: Initial: 0.05 mg at bedtime; sequentially increase every 3 to 7 days in 0.05 mg/day increments given as 0.05 mg twice daily, then 3 times daily, then 4 times daily; maximum daily dose weight-dependent: Patient weight: 27 to 40.5 kg: 0.2 mg/day; patient weight: 40.5 to 45 kg; 0.3 mg/day.
>45 kg: Initial: 0.1 mg at bedtime; sequentially increase every 3 to 7 days in 0.1 mg/day increments given as 0.1 mg twice daily, then 3 times daily, then 4 times daily; maximum daily dose: 0.4 mg/day.
Extended release (Kapvay): Children ≥6 years and Adolescents: Initial: 0.1 mg at bedtime; increase in 0.1 mg/day increments every 7 days until desired response; doses should be administered twice daily in the morning and at bedtime (either split equally or with the higher split dosage given at bedtime); maximum daily dose: 0.4 mg/day. Note: When discontinuing therapy, taper daily dose by ≤0.1 mg every 3 to 7 days.
Topical: Transdermal patch: Limited data available: Children ≥6 years and adolescents may be switched to the transdermal delivery system after oral therapy is titrated to an optimal and stable dose; a transdermal dose approximately equivalent to the total oral daily dose may be used; apply transdermal patch and change every 5 to 7 days. Adjustment in dose of transdermal patch may be needed; there is variation in absorption and no exact equivalence or fixed ratio exist between the oral and transdermal routes (Du 2008; Hunt 1987; Hunt 1990).
Clonidine tolerance test (test of growth hormone release from the pituitary): Limited data available: Children and Adolescents: Oral: Immediate release: 0.15 mg/m2 or 5 mcg/kg as a single dose; maximum dose: 0.25 mg (250 mcg) (Lanes 1982; Richmond 2008).
Conduct disorder/oppositional-defiant disorder with or without ADHD: Limited data available; efficacy results variable (Connor 2010; Pringsheim 2015): Children ≥5 years and Adolescents: Oral: Immediate release: Initial: 0.05 mg/day; gradual titration every 3 to 7 days in 0.05 mg increments to a 2 or 3 times daily dose schedule has been used most frequently, some patients may require 4 daily doses; usual final dose range: 0.2 to 0.3 mg/day in 2 to 3 divided doses, reported overall range: 0.15 to 0.4 mg/day in divided doses; most reported experience in patients with ADHD comorbidity (Connor 2000; Hazell 2003; Kemph 1993; Palumbo 2008).
Epidural analgesia, adjunct therapy: Note: Manufacturer suggests reserving use for severe intractable pain, unresponsive to other opioid analgesics (eg, patients with cancer).
Children and Adolescents: Epidural: Continuous infusion: Initial: 0.5 mcg/kg/hour; adjust with caution, based on clinical effect; do not exceed adult doses. Do not discontinue clonidine abruptly; if needed, gradually reduce dose over 2 to 4 days to avoid withdrawal symptoms.
Hypertension:
Chronic: Limited data available:
Oral: Immediate release:
Weight-directed dosing: Children and Adolescents: Initial: 5 to 10 mcg/kg/day in divided doses every 8 to 12 hours; increase gradually as needed; usual range: 5 to 25 mcg/kg/day in divided doses every 8 to 12 hours; maximum daily dose: 0.9 mg/day (Flynn 2006; Kavey 2010; Rocchini 1984).
Fixed dosing: Children ≥12 years and Adolescents: Initial: 0.1 mg twice daily; increase gradually. In adults, titration is done by increasing by 0.1 mg/day at weekly intervals; usual maintenance dose: 0.2 to 0.6 mg/day in divided doses; maximum recommended daily dose: 2.4 mg/day (rarely required) (NHBPEP 2004; NHLBI 2012).
Topical: Transdermal patch: Limited data available: Children and Adolescents: Based on information from other indications, may be switched to the transdermal delivery system after oral therapy is titrated to an optimal and stable dose; a transdermal dose approximately equivalent to the total oral daily dose may be used; apply transdermal patch and change every 5 to 7 days. Adjustment in dose of transdermal patch may be needed; there is variation in absorption and no exact equivalence or fixed ratio exist between the oral and transdermal routes (Galloway 2000; Hunt 1990).
Hypertensive urgency: Limited data available:
Weight-directed dosing: Children and Adolescents: Oral: Immediate release: 2 to 5 mcg/kg/dose every 6 to 8 hours. Some patients may require doses up to 10 mcg/kg/dose (AAP [Flynn 2017].
Fixed dosing: Children and Adolescents: Oral: Immediate release: 0.05 to 0.1 mg/dose; may repeat dose(s) up to a maximum total dose of 0.8 mg (NHBPEP 2004).
Neuropathic pain: Limited data available:
Oral: Immediate release: Some centers use the following doses (Galloway 2000): Children and Adolescents: Initial: 2 mcg/kg/dose every 4 to 6 hours; increase incrementally over several days; range: 2 to 4 mcg/kg/dose every 4 to 6 hours.
Topical: Transdermal patch: Children and Adolescents: May be switched to the transdermal delivery system after oral therapy is titrated to an optimal and stable dose; a transdermal dose approximately equivalent to the total oral daily dose may be used; apply transdermal patch and change every 5 to 7 days. Adjustment in dose of transdermal patch may be needed; there is variation in absorption and no exact equivalence or fixed ratio exist between the oral and transdermal routes (Galloway 2000).
Sedation, critically ill patients: Limited data available: Infants, Children, and Adolescents: Oral: Immediate release: Usual reported dose: 1 to 5 mcg/kg/dose every 6 to 8 hours; maximum dose: 200 mcg/dose; reported daily dose range: 2 to 20 mcg/kg/day; Avoid abrupt discontinuation to prevent withdrawal symptoms (Arenas-López 2004; Capino 2016; Duffett 2014; Playfor 2006).
Tic disorders and Tourette syndrome: Limited data available; greater efficacy shown in patients with ADHD comorbidity (Weisman 2013): Children ≥7 years and Adolescents: Oral: Immediate release: Initial: 0.025 to 0.05 mg/day; gradual titration to a 3 to 4 times daily schedule using small increments (0.025 mg); usual daily dose: 0.1 to 0.4 mg/day in 3 to 4 divided doses (AACAP [Murphy 2013]; Pringsheim 2012; The Tourette Syndrome Study Group 2002).
Reconstitution
Epidural formulation: Prior to administration, the 500 mcg/mL concentration must be diluted in 0.9% sodium chloride for injection (preservative-free) to a final concentration of 100 mcg/mL.
Extemporaneously Prepared
Note: Compounded oral suspension may be available in multiple concentrations (eg, up to 10 times more concentrated); use caution to avoid confusion; verify concentration.
0.02 mg/mL (20 mcg/mL) Oral Liquid (ASHP Standard Concentration) (ASHP 2017)
A 0.02 mg/mL (20 mcg/mL) oral liquid may be made from tablets. Crush six 0.1 mg tablets in a glass mortar and levigate with 1 to 2 mL Simple Syrup, NF. Add additional Simple Syrup, NF and transfer to a calibrated amber bottle. Rinse the mortar and pestle with the vehicle and add quantity of vehicle sufficient to make 30 mL. Label “refrigerate.” Stable for 35 days when stored in an ambler plastic bottle and refrigerated.
Sauberan JB, Phuong P, Ilog ND, Rossi SS. Stability and osmolality of extemporaneously prepared clonidine oral liquid for neonates. Ann Pharmacother. 2016;50(3):243-244. doi: 10.1177/1060028015620625.26728366
0.01 mg/mL (10 mcg/mL) Oral Suspension
A 0.01 mg/mL (10 mcg/mL) oral suspension may be made from tablets. Crush twenty 0.1 mg tablets in a glass mortar and reduce to a fine powder. Slowly add Ora-Blend in ~15 mL increments while mixing to form a uniform paste until approximately half of the total volume (~100 mL) is added. Transfer the suspension to a graduated cylinder. Rinse the mortar and pestle with the remaining vehicle and add quantity to fill the volume within the graduated cylinder to 200 mL. Transfer this amount to a calibrated bottle. Label “shake well.” When stored in clear plastic syringes, the suspension is stable for at least 91 days at room temperature (25°C) or refrigerated (4°C).
Ma C, Decarie D, Ensom MHH. Stability of clonidine oral suspension in oral plastic syringes. Am J Health-Syst Pharm. 2014;71:657-661.24688040
0.1 mg/mL (100 mcg/mL) Oral Suspension
A 0.1 mg/mL (100 mcg/mL) oral suspension may be made from tablets. Crush thirty 0.2 mg tablets in a glass mortar and reduce to a fine powder. Slowly add 2 mL Purified Water USP and mix to a uniform paste. Slowly add Simple Syrup, NF in 15 mL increments; transfer to a calibrated bottle, rinse mortar with vehicle, and add quantity of vehicle sufficient to make 60 mL. Label "shake well" and "refrigerate". Stable for 28 days when stored in amber glass bottles and refrigerated.
Levinson ML and Johnson CE. Stability of an extemporaneously compounded clonidine hydrochloride oral liquid. Am J Hosp Pharm. 1992;49(1):122-125.1570852
Administration
Epidural: Specialized techniques are required for continuous epidural administration; administration via this route should only be performed by qualified individuals familiar with the techniques of epidural administration and patient management problems associated with this route. Familiarization of the epidural infusion device is essential. Do not discontinue clonidine abruptly; if needed, gradually reduce dose over 2 to 3 days to avoid withdrawal symptoms.
Oral: May be taken with or without food.
Transdermal patch: Patches should be applied weekly at a consistent time to a clean, hairless area of the upper outer arm or chest. Rotate patch sites weekly. Redness under patch may be reduced if a topical corticosteroid spray is applied to the area before placement of the patch (Tom 1994). Dispose of any used or unused patches by folding adhesive ends together, replace in pouch or sealed container, and discard properly in trash away from children and pets.
Storage
Epidural formulation: Store at 20°C to 25°C (68°F to 77°F). Preservative free; discard unused portion.
Tablets: Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Protect from light.
Extended release tablets: Store at 20°C to 25°C (68°F to 77°F). Protect from light.
Transdermal patches: Store at 25°C (77°F); excursions permitted between 15°C to 30°C (59°F and 86°F).
CloNIDine Images
Drug Interactions
Alcohol (Ethyl): CNS Depressants may enhance the CNS depressant effect of Alcohol (Ethyl). Monitor therapy
Alfuzosin: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Alizapride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Amifostine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Amifostine. Management: When amifostine is used at chemotherapy doses, blood pressure lowering medications should be withheld for 24 hours prior to amifostine administration. If blood pressure lowering therapy cannot be withheld, amifostine should not be administered. Consider therapy modification
Amphetamines: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Antipsychotic Agents (Second Generation [Atypical]): Blood Pressure Lowering Agents may enhance the hypotensive effect of Antipsychotic Agents (Second Generation [Atypical]). Monitor therapy
Azelastine (Nasal): CNS Depressants may enhance the CNS depressant effect of Azelastine (Nasal). Avoid combination
Barbiturates: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Benperidol: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Beta-Blockers: Alpha2-Agonists may enhance the AV-blocking effect of Beta-Blockers. Sinus node dysfunction may also be enhanced. Beta-Blockers may enhance the rebound hypertensive effect of Alpha2-Agonists. This effect can occur when the Alpha2-Agonist is abruptly withdrawn. Management: Closely monitor heart rate during treatment with a beta blocker and clonidine. Withdraw beta blockers several days before clonidine withdrawal when possible, and monitor blood pressure closely. Recommendations for other alpha2-agonists are unavailable. Exceptions: Levobunolol; Metipranolol. Consider therapy modification
Blonanserin: CNS Depressants may enhance the CNS depressant effect of Blonanserin. Consider therapy modification
Bradycardia-Causing Agents: May enhance the bradycardic effect of other Bradycardia-Causing Agents. Monitor therapy
Brexanolone: CNS Depressants may enhance the CNS depressant effect of Brexanolone. Monitor therapy
Brigatinib: May diminish the antihypertensive effect of Antihypertensive Agents. Brigatinib may enhance the bradycardic effect of Antihypertensive Agents. Monitor therapy
Brimonidine (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Brimonidine (Topical): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Bromopride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromperidol: Blood Pressure Lowering Agents may enhance the hypotensive effect of Bromperidol. Bromperidol may diminish the hypotensive effect of Blood Pressure Lowering Agents. Avoid combination
Bromperidol: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Buprenorphine: CNS Depressants may enhance the CNS depressant effect of Buprenorphine. Management: Consider reduced doses of other CNS depressants, and avoiding such drugs in patients at high risk of buprenorphine overuse/self-injection. Initiate buprenorphine at lower doses in patients already receiving CNS depressants. Consider therapy modification
Calcium Channel Blockers (Nondihydropyridine): CloNIDine may enhance the AV-blocking effect of Calcium Channel Blockers (Nondihydropyridine). Sinus node dysfunction may also be enhanced. Monitor therapy
Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Cannabis: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Cardiac Glycosides: CloNIDine may enhance the AV-blocking effect of Cardiac Glycosides. Sinus node dysfunction may also be enhanced. Monitor therapy
Ceritinib: Bradycardia-Causing Agents may enhance the bradycardic effect of Ceritinib. Management: If this combination cannot be avoided, monitor patients for evidence of symptomatic bradycardia, and closely monitor blood pressure and heart rate during therapy. Exceptions are discussed in separate monographs. Consider therapy modification
Chlormethiazole: May enhance the CNS depressant effect of CNS Depressants. Management: Monitor closely for evidence of excessive CNS depression. The chlormethiazole labeling states that an appropriately reduced dose should be used if such a combination must be used. Consider therapy modification
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
CNS Depressants: May enhance the adverse/toxic effect of other CNS Depressants. Monitor therapy
Dexmethylphenidate: May diminish the therapeutic effect of Antihypertensive Agents. Monitor therapy
Diazoxide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Dimethindene (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Doxylamine: May enhance the CNS depressant effect of CNS Depressants. Management: The manufacturer of Diclegis (doxylamine/pyridoxine), intended for use in pregnancy, specifically states that use with other CNS depressants is not recommended. Monitor therapy
Dronabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Droperidol: May enhance the CNS depressant effect of CNS Depressants. Management: Consider dose reductions of droperidol or of other CNS agents (eg, opioids, barbiturates) with concomitant use. Exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Consider therapy modification
DULoxetine: Blood Pressure Lowering Agents may enhance the hypotensive effect of DULoxetine. Monitor therapy
EPHEDrine (Systemic): CloNIDine may enhance the therapeutic effect of EPHEDrine (Systemic). Monitor therapy
Esketamine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Fexinidazole [INT]: Bradycardia-Causing Agents may enhance the arrhythmogenic effect of Fexinidazole [INT]. Avoid combination
Flunitrazepam: CNS Depressants may enhance the CNS depressant effect of Flunitrazepam. Consider therapy modification
Herbs (Hypertensive Properties): May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Herbs (Hypotensive Properties): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
HYDROcodone: CNS Depressants may enhance the CNS depressant effect of HYDROcodone. Management: Avoid concomitant use of hydrocodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
HydrOXYzine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Hypotension-Associated Agents: Blood Pressure Lowering Agents may enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Ivabradine: Bradycardia-Causing Agents may enhance the bradycardic effect of Ivabradine. Monitor therapy
Kava Kava: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Lacosamide: Bradycardia-Causing Agents may enhance the AV-blocking effect of Lacosamide. Monitor therapy
Lemborexant: May enhance the CNS depressant effect of CNS Depressants. Management: Dosage adjustments of lemborexant and of concomitant CNS depressants may be necessary when administered together because of potentially additive CNS depressant effects. Close monitoring for CNS depressant effects is necessary. Consider therapy modification
Levodopa-Containing Products: Blood Pressure Lowering Agents may enhance the hypotensive effect of Levodopa-Containing Products. Monitor therapy
Lofexidine: May enhance the CNS depressant effect of CNS Depressants. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Lormetazepam: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Macimorelin: CloNIDine may diminish the diagnostic effect of Macimorelin. Avoid combination
Magnesium Sulfate: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Methotrimeprazine: CNS Depressants may enhance the CNS depressant effect of Methotrimeprazine. Methotrimeprazine may enhance the CNS depressant effect of CNS Depressants. Management: Reduce adult dose of CNS depressant agents by 50% with initiation of concomitant methotrimeprazine therapy. Further CNS depressant dosage adjustments should be initiated only after clinically effective methotrimeprazine dose is established. Consider therapy modification
Methylphenidate: May enhance the adverse/toxic effect of CloNIDine. Monitor therapy
MetyroSINE: CNS Depressants may enhance the sedative effect of MetyroSINE. Monitor therapy
Midodrine: May enhance the bradycardic effect of Bradycardia-Causing Agents. Monitor therapy
Minocycline (Systemic): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Mirtazapine: May diminish the antihypertensive effect of Alpha2-Agonists. Management: Consider avoiding concurrent use. If the combination cannot be avoided, monitor for decreased effects of alpha2-agonists if mirtazapine is initiated/dose increased, or increased effects if mirtazapine is discontinued/dose decreased. Consider therapy modification
Molsidomine: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nabilone: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Naftopidil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicergoline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicorandil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nitroprusside: Blood Pressure Lowering Agents may enhance the hypotensive effect of Nitroprusside. Monitor therapy
Obinutuzumab: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Management: Consider temporarily withholding blood pressure lowering medications beginning 12 hours prior to obinutuzumab infusion and continuing until 1 hour after the end of the infusion. Consider therapy modification
Opioid Agonists: CNS Depressants may enhance the CNS depressant effect of Opioid Agonists. Management: Avoid concomitant use of opioid agonists and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Orphenadrine: CNS Depressants may enhance the CNS depressant effect of Orphenadrine. Avoid combination
Oxomemazine: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
OxyCODONE: CNS Depressants may enhance the CNS depressant effect of OxyCODONE. Management: Avoid concomitant use of oxycodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Paraldehyde: CNS Depressants may enhance the CNS depressant effect of Paraldehyde. Avoid combination
Pentoxifylline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Perampanel: May enhance the CNS depressant effect of CNS Depressants. Management: Patients taking perampanel with any other drug that has CNS depressant activities should avoid complex and high-risk activities, particularly those such as driving that require alertness and coordination, until they have experience using the combination. Consider therapy modification
Pholcodine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Pholcodine. Monitor therapy
Phosphodiesterase 5 Inhibitors: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Piribedil: CNS Depressants may enhance the CNS depressant effect of Piribedil. Monitor therapy
Pramipexole: CNS Depressants may enhance the sedative effect of Pramipexole. Monitor therapy
Prostacyclin Analogues: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Quinagolide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
ROPINIRole: CNS Depressants may enhance the sedative effect of ROPINIRole. Monitor therapy
Rotigotine: CNS Depressants may enhance the sedative effect of Rotigotine. Monitor therapy
Rufinamide: May enhance the adverse/toxic effect of CNS Depressants. Specifically, sleepiness and dizziness may be enhanced. Monitor therapy
Ruxolitinib: May enhance the bradycardic effect of Bradycardia-Causing Agents. Management: Ruxolitinib Canadian product labeling recommends avoiding use with bradycardia-causing agents to the extent possible. Monitor therapy
Selective Serotonin Reuptake Inhibitors: CNS Depressants may enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk of psychomotor impairment may be enhanced. Monitor therapy
Serotonin/Norepinephrine Reuptake Inhibitors: May diminish the antihypertensive effect of Alpha2-Agonists. Monitor therapy
Siponimod: Bradycardia-Causing Agents may enhance the bradycardic effect of Siponimod. Management: Avoid coadministration of siponimod with drugs that may cause bradycardia. Consider therapy modification
Sodium Oxybate: May enhance the CNS depressant effect of CNS Depressants. Management: Consider alternatives to combined use. When combined use is needed, consider minimizing doses of one or more drugs. Use of sodium oxybate with alcohol or sedative hypnotics is contraindicated. Consider therapy modification
Suvorexant: CNS Depressants may enhance the CNS depressant effect of Suvorexant. Management: Dose reduction of suvorexant and/or any other CNS depressant may be necessary. Use of suvorexant with alcohol is not recommended, and the use of suvorexant with any other drug to treat insomnia is not recommended. Consider therapy modification
Tapentadol: May enhance the CNS depressant effect of CNS Depressants. Management: Avoid concomitant use of tapentadol and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Terlipressin: May enhance the bradycardic effect of Bradycardia-Causing Agents. Monitor therapy
Tetrahydrocannabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Thalidomide: CNS Depressants may enhance the CNS depressant effect of Thalidomide. Avoid combination
Tofacitinib: May enhance the bradycardic effect of Bradycardia-Causing Agents. Monitor therapy
Tricyclic Antidepressants: May diminish the antihypertensive effect of Alpha2-Agonists. Management: Consider avoiding this combination. If used, monitor for decreased effects of the alpha2-agonist. Exercise great caution if discontinuing an alpha2-agonist in a patient receiving a TCA. Consider therapy modification
Trimeprazine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Yohimbine: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Zolpidem: CNS Depressants may enhance the CNS depressant effect of Zolpidem. Management: Reduce the Intermezzo brand sublingual zolpidem adult dose to 1.75 mg for men who are also receiving other CNS depressants. No such dose change is recommended for women. Avoid use with other CNS depressants at bedtime; avoid use with alcohol. Consider therapy modification
Test Interactions
Positive Coombs' test; may lead to false-positive aldosterone/renin ratio (Funder 2016)
Adverse Reactions
Frequency not always defined.
Oral, Transdermal: Incidence of adverse events may be less with transdermal compared to oral due to the lower peak/trough ratio.
>10%:
Central nervous system: Drowsiness (2% to 38%), headache (1% to 29%), fatigue (4% to 16%), dizziness (2% to 16%)
Dermatologic: Transient skin rash (localized; characterized by pruritus and erythema; transdermal 15% to 50%), contact dermatitis (transdermal 8% to 34%)
Gastrointestinal: Xerostomia (≤40%), upper abdominal pain (15%)
1% to 10%:
Cardiovascular: Bradycardia (≤4%), edema (3%), localized blanching (transdermal 1%), palpitations (1%), tachycardia (≤3%), atrioventricular block, cardiac arrhythmia, cardiac failure, cerebrovascular accident, chest pain, ECG abnormality, flushing, orthostatic hypotension, prolonged Q-T Interval on ECG, Raynaud's phenomenon, syncope
Central nervous system: Sedation (3% to 10%), irritability (5% to 9%), nightmares (4% to 9%), insomnia (≤6%), emotional disturbance (4%), lethargy (3%), nervousness (1% to 3%), depression (1%), throbbing (transdermal 1%), withdrawal syndrome (1%), aggressive behavior, agitation, anxiety, behavioral changes, delirium, delusions, hallucination (visual and auditory), malaise, numbness (localized; transdermal), paresthesia, parotid pain (oral), restlessness, vivid dream
Dermatologic: Localized vesiculation (transdermal 7%), allergic contact sensitivity (transdermal 5%), hyperpigmentation (transdermal 5%), burning sensation of skin (transdermal 3%), excoriation (transdermal 3%), macular eruption (1%), papule (transdermal 1%), alopecia, hypopigmentation (localized; transdermal), pallor, skin rash, urticaria
Endocrine & metabolic: Gynecomastia (1%), weight gain (<1%), decreased libido, hyperglycemia (transient; oral), increased thirst
Gastrointestinal: Constipation (1% to 10%), viral gastrointestinal infection (5%), anorexia (1%), abdominal pain (oral), diarrhea, gastrointestinal pseudo-obstruction (oral), nausea, parotitis (oral), sore throat, vomiting
Genitourinary: Urinary incontinence (4%), sexual disorder (3%), erectile dysfunction (2% to 3%), nocturia (1%), pollakiuria, urinary retention
Hematologic & oncologic: Thrombocytopenia (oral)
Hepatic: Abnormal hepatic function tests (mild transient abnormalities; <1%), hepatitis
Hypersensitivity: Angioedema
Neuromuscular & skeletal: Weakness (10%), tremor (1% to 4%), arthralgia (1%), myalgia (1%), leg cramps (<1%), increased creatine phosphokinase (transient; oral), limb pain
Ophthalmic: Accommodation disturbance, blurred vision, burning sensation of eyes, decreased lacrimation, dry eye syndrome, increased lacrimation
Otic: Otitis media (≤3%), otalgia
Respiratory: Asthma, dry nose, epistaxis, flu-like symptoms, nasal congestion, nasopharyngitis, respiratory tract infection, rhinorrhea
Miscellaneous: Crying (1% to 3%), fever
Epidural: Note: The following adverse events occurred more often than placebo in cancer patients with intractable pain being treated with concurrent epidural morphine.
>10%:
Cardiovascular: Hypotension (45%), orthostatic hypotension (32%)
Central nervous system: Confusion (13%), dizziness (13%)
Gastrointestinal: Xerostomia (13%)
1% to 10%:
Cardiovascular: Chest pain (5%)
Central nervous system: Hallucination (5%)
Dermatologic: Diaphoresis (5%)
Gastrointestinal: Nausea and vomiting (8%)
Otic: Tinnitus (5%)
Warnings/Precautions
Concerns related to adverse effects:
- Bradycardia: May cause dose-dependent reductions in heart rate; use with caution in patients with preexisting bradycardia or those predisposed to developing bradycardia.
- CNS depression: May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks which require mental alertness (eg, operating machinery or driving).
- Hypotension: Symptomatic hypotension may occur with use. In all patients, use epidural clonidine with caution due to the potential for severe hypotension, especially in women and those of low body weight. Most hypotensive episodes occur within the first 4 days of initiation; however, episodes may occur throughout the duration of therapy.
- Respiratory depression: Epidural administration may result in mild respiratory depression (usually associated with higher than recommended doses).
- Xerostomia: May cause significant xerostomia.
Disease-related concerns:
- Cardiovascular disease: Use with caution in patients with severe coronary insufficiency, including recent MI and conduction disturbances, including sinus node dysfunction. The use of epidural clonidine frequently reduces heart rate; AV block greater than first-degree has been reported rarely. Epidural clonidine is not recommended for use in patients with severe cardiovascular disease or hemodynamic instability. May lead to cardiovascular instability (hypotension, bradycardia).
- Cerebrovascular disease: Use with caution in patients with cerebrovascular disease.
- Renal impairment: Use with caution in patients with chronic renal impairment. The hemodynamic effects may be prolonged in those with renal impairment; elimination half-life significantly prolonged (up to 41 hours) in patients with severe renal impairment.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Pediatric: Since children commonly have gastrointestinal illnesses with vomiting, they are susceptible to hypertensive episodes due to abrupt inability to take oral medication. Epidural clonidine should be reserved for pediatric cancer patients with severe intractable pain, unresponsive to other analgesics or epidural or spinal opioids.
- Surgical patients: Discontinue oral immediate-release formulations within 4 hours of surgery, then restart as soon as possible afterward.
Dosage form specific issues:
- Epidural use: [US Boxed Warning]: Must dilute concentrated epidural injectable (500 mcg/mL) solution prior to use. Epidural clonidine is not recommended for perioperative, obstetrical, or postpartum pain due to risk of hemodynamic instability. Should be administered via continuous epidural infusion device. Monitor closely for catheter-related infection such as meningitis or epidural abscess.
- Product interchangeability: Oral formulations of clonidine (immediate release versus extended release) are not interchangeable on a mg:mg basis due to different pharmacokinetic profiles.
- Transdermal patch: May contain conducting metal (eg, aluminum); remove patch prior to MRI. Due to the potential for altered electrical conductivity, remove transdermal patch before cardioversion or defibrillation. Localized contact sensitization to the transdermal system has been reported; in these patients, allergic reactions (eg, generalized rash, urticaria, angioedema) have also occurred following subsequent substitution of oral therapy.
Other warnings/precautions:
- Contact lens wearers: Clonidine may cause eye dryness in patients who wear contact lenses.
- Discontinuation of therapy: Gradual withdrawal is needed (discontinue oral immediate release or epidural dose gradually over 6 to 10 days to avoid rebound hypertension) if drug needs to be stopped. Patients should be instructed about abrupt discontinuation (causes rapid increase in BP and symptoms of sympathetic overactivity). In patients on both a beta-blocker and clonidine where withdrawal of clonidine is necessary, withdraw the beta-blocker first and several days before clonidine withdrawal, then slowly decrease clonidine. In children and adolescents, extended release formulation (Kapvay) should be tapered in decrements of no more than 0.1 mg every 3 to 7 days. The clonidine withdrawal syndrome is more pronounced after abrupt cessation of long-term therapy than after short-term therapy (1 to 2 months). It has usually been associated with previous administration of high oral doses (>1.2 mg daily in adults) and/or continuation of beta-blocker therapy. The danger of abrupt discontinuation may be increased in patients with hypertension and/or other cardiovascular considerations. Blood pressure may increase 8 to 24 hours after last dose, but has occurred 60 hours after the last clonidine dose. Rebound hypertension has occurred with discontinuation of transdermal and epidural clonidine.
Monitoring Parameters
Blood pressure, standing and sitting/supine, mental status, heart rate
Epidural: Carefully monitor infusion pump; inspect catheter tubing for obstruction or dislodgement to reduce risk of inadvertent abrupt withdrawal of infusion. Monitor closely for catheter-related infection (eg, meningitis or epidural abscess).
Hypertension: The 2017 Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults (ACC/AHA [Whelton 2018]):
Confirmed hypertension and known CVD or 10-year ASCVD risk ≥10%: Target blood pressure <130/80 mm Hg is recommended.
Confirmed hypertension without markers of increased CVD risk: Target blood pressure <130/80 mm Hg may be reasonable.
Pregnancy
Pregnancy Considerations
Clonidine crosses the placenta; concentrations in the umbilical cord plasma are similar to those in the maternal serum and concentrations in the amniotic fluid may be 4 times those in the maternal serum.
The pharmacokinetics of clonidine may be altered during pregnancy due to an increase in nonrenal clearance, possibly regulated by maternal CYP2D6 genotype (Buchanan 2009; Claessens 2010).
Chronic maternal hypertension may increase the risk of birth defects, low birth weight, preterm delivery, stillbirth, and neonatal death. Actual fetal/neonatal risks may be related to duration and severity of maternal hypertension. Untreated hypertension may also increase the risks of adverse maternal outcomes, including gestational diabetes, myocardial infarction, preeclampsia, stroke, and delivery complications (ACOG 203 2019). Agents other than clonidine are more commonly used to treat hypertension in pregnancy (ACOG 203 2019; ESC [Regitz-Zagrosek 2018]); use of clonidine should be considered in consult with subspecialists (ACOG 203 2019). Females with preexisting hypertension may continue their medication during pregnancy unless contraindications exist (ESC [Regitz-Zagrosek 2018]).
If treatment for attention-deficit/hyperactivity disorder in pregnancy is needed, other agents are preferred (Ornoy 2018).
[US Boxed Warning]: Epidural clonidine is not recommended for obstetrical or postpartum pain due to risk of hemodynamic instability. However, in a rare obstetrical, or postpartum patient, potential benefits may outweigh the possible risks. Severe maternal hypotension may occur following epidural use which may result in decreased placental perfusion. Clonidine has been evaluated for use as an adjunctive agent for epidural labor analgesia (Allen 2018; Kumari 2018; Landau 2002; Roelants 2015; Zhang 2015) including patients who are opioid dependent (Hoyt 2018).
Patient Education
What is this drug used for?
- It is used to treat high blood pressure.
- It is used to treat attention deficit problems with hyperactivity.
- It is used to control pain when infused into the spine.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Dry mouth
- Constipation
- Fatigue
- Headache
- Nausea
- Loss of strength and energy
- Trouble sleeping
- Nightmares
- Lack of appetite
- Abdominal pain
- Irritability
- Sweating a lot
- Vomiting
- Noise or ringing in the ears
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Severe dizziness
- Passing out
- Slow heartbeat
- Fast heartbeat
- Abnormal heartbeat
- Contact lens discomfort
- Severe skin irritation
- Skin discoloration
- Skin redness
- Burning of skin
- Difficulty breathing
- Slow breathing
- Shallow breathing
- Confusion
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.