Boxed Warning
Severe neutropenia:
Clozapine treatment has caused severe neutropenia, defined as an absolute neutrophil count (ANC) less than 500/mm3. Severe neutropenia can lead to serious infection and death. Prior to initiating treatment, a baseline ANC must be at least 1,500/mm3 for the general population and must be at least 1,000/mm3 for patients with documented Benign Ethnic Neutropenia. During treatment, patients must have regular ANC monitoring. Advise patients to immediately report symptoms consistent with severe neutropenia or infection (eg, fever, weakness, lethargy, sore throat).
Because of the risk of severe neutropenia, clozapine is available only through a restricted program under a Risk Evaluation Mitigation Strategy (REMS) called the Clozapine REMS Program.
Orthostatic hypotension, bradycardia, syncope:
Orthostatic hypotension, bradycardia, syncope, and cardiac arrest have occurred with treatment. The risk is highest during the initial titration period, particularly with rapid dose escalation. These reactions can occur with the first dose, with dosages as low as 12.5 mg/day. Initiate treatment at 12.5 mg once or twice daily, titrate slowly, and use divided dosages. Use cautiously in patients with cardiovascular or cerebrovascular disease or conditions predisposing to hypotension (eg, dehydration, use of antihypertensive medications).
Seizures:
Seizures have occurred with treatment. The risk is dose-related. Initiate treatment at 12.5 mg, titrate gradually, and use divided dosing. Use caution when administering to patients with a history of seizures or other predisposing risk factors for seizure (CNS pathology, medications that lower the seizure threshold, alcohol abuse). Caution patients about engaging in any activity where sudden loss of consciousness could cause serious risk to themselves or others.
Myocarditis, cardiomyopathy and mitral valve incompetence:
Fatal myocarditis and cardiomyopathy have occurred with treatment. Discontinue clozapine and obtain a cardiac evaluation upon suspicion of these reactions. Generally, patients with clozapine-related myocarditis or cardiomyopathy should not be rechallenged with clozapine. Consider the possibility of myocarditis or cardiomyopathy if chest pain, tachycardia, palpitations, dyspnea, fever, flu-like symptoms, hypotension, or electrocardiogram (ECG) changes occur.
Increased mortality in elderly patients with dementia-related psychosis:
Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Clozapine is not approved for use in patients with dementia-related psychosis.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Suspension, Oral:
Versacloz: 50 mg/mL (100 mL) [contains methylparaben sodium, propylparaben sodium]
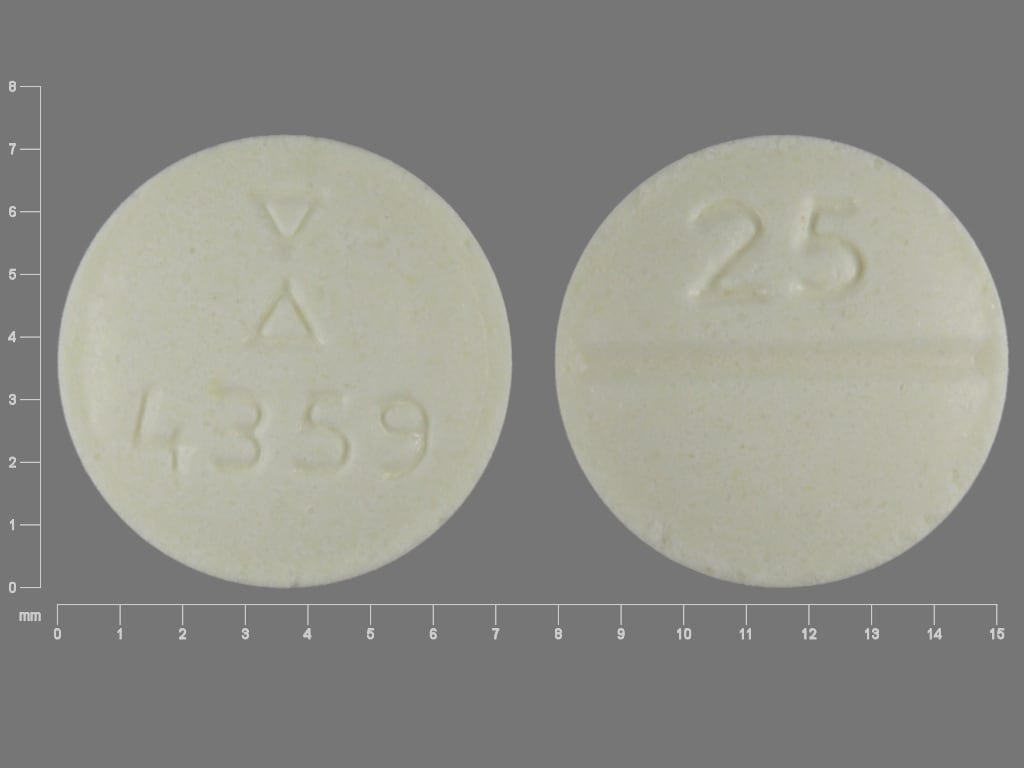
Tablet, Oral:
Clozaril: 25 mg [contains corn starch]
Clozaril: 25 mg [DSC], 50 mg [scored; contains corn starch]
Clozaril: 100 mg [contains corn starch]
Clozaril: 100 mg [DSC] [scored; contains corn starch]
Clozaril: 200 mg [contains corn starch]
Generic: 25 mg, 50 mg, 100 mg, 200 mg
Tablet Disintegrating, Oral:
FazaClo: 12.5 mg [DSC], 25 mg [DSC], 100 mg [DSC], 150 mg [DSC], 200 mg [DSC] [contains aspartame]
Generic: 12.5 mg, 25 mg, 100 mg, 150 mg, 200 mg
Pharmacology
Mechanism of Action
The therapeutic efficacy of clozapine (dibenzodiazepine antipsychotic) is proposed to be mediated through antagonism of the dopamine type 2 (D2) and serotonin type 2A (5-HT2A) receptors. In addition, it acts as an antagonist at alpha-adrenergic, histamine H1, cholinergic, and other dopaminergic and serotonergic receptors.
Pharmacokinetics/Pharmacodynamics
Metabolism
Extensively hepatic via CYP1A2 (primary), 2C19, 3A4 and 2D6; forms metabolites with limited (desmethyl metabolite) or no activity (hydroxylated and N-oxide derivative derivatives). Note: A pediatric pharmacokinetic study (n=6; age: 9 to 16 years) found higher concentrations of the desmethyl metabolite in comparison to clozapine (especially in females) when compared with data from adult studies; the authors suggest that both the parent drug and desmethyl metabolite contribute to the efficacy and adverse effect profile in children and adolescents (Frazier 2003; Sheehan 2010).
Excretion
Urine (~50%) and feces (30%) with trace amounts of unchanged drug
Onset of Action
Within 1 week for sedation, improvement in sleep; 6 to 12 weeks for antipsychotic effects; Adequate trial: 6 to 12 weeks at a therapeutic dose and blood level; Maximum effect: 6 to 12 months; improvement may continue 6 to 12 months after clozapine initiation (Meltzer 2003).
Time to Peak
Suspension: 2.2 hours (range: 1 to 3.5 hours); Tablets: 2.5 hours (range: 1 to 6 hours); Dispersible tablets: 2.3 hours (range: 1 to 6 hours)
Duration of Action
Variable
Half-Life Elimination
Steady state: 12 hours (range: 4 to 66 hours)
Protein Binding
97% to serum proteins
Use in Specific Populations
Special Populations: Renal Function Impairment
Clozapine concentrations may be increased.
Special Populations: Hepatic Function Impairment
Clozapine concentrations may be increased.
Use: Labeled Indications
Schizophrenia, treatment resistant: Treatment of severely ill patients with schizophrenia who fail to respond adequately to antipsychotic treatment.
Suicidal behavior in schizophrenia or schizoaffective disorder: To reduce the risk of suicidal behavior in patients with schizophrenia or schizoaffective disorder who are judged to be at chronic risk for reexperiencing suicidal behavior, based on history and recent clinical state.
Use: Off Label
Bipolar disorder (treatment resistant)cyes
Data from a meta-analysis of 15 trials support the use of clozapine in treatment-resistant bipolar disorder with mania or psychosis Li 2015.
Based on bipolar disorder guidelines from the American Psychiatric Association, the World Federation of Societies of Biological Psychiatry, and the Canadian Network for Mood and Anxiety Treatments and International Society for Bipolar Disorders, clozapine is an effective and recommended treatment as monotherapy or adjunct therapy for acute manic episodes and maintenance management of bipolar disorder, especially when refractory APA [Hirschfeld 2002], CANMAT/ISBD [Yatham 2018], WFSBP [Grunze 2009].
Psychosis/agitation (treatment resistant) associated with dementiacyes
Data from a retrospective chart review of patients admitted with a DSM-IV diagnosis of treatment-resistant dementia and symptoms of agitation suggest that clozapine may be beneficial for the treatment of this condition Lee 2007. Additional data may be necessary to further define the role of clozapine in the treatment of this condition.
Based on the American Psychiatric Association (APA) practice guideline on the use of antipsychotics to treat agitation or psychosis in patients with dementia, antipsychotics, such as clozapine, may be considered for the treatment of agitation and psychosis in certain patients; however, evidence for efficacy is modest and use should be limited to patients whose symptoms are dangerous, severe, or cause significant patient distress due to safety risks associated with antipsychotic use.
Psychosis in Parkinson diseasecyes
Data from a meta-analysis evaluating several small randomized, controlled trials suggest that clozapine may be beneficial for the treatment of psychosis in patients in Parkinson disease Frieling 2007. Additional data may be necessary to further define the role of clozapine in this condition.
Based on the American Academy of Neurology guidelines for the management of depression, psychosis and dementia in Parkinson disease, clozapine given for psychosis and motor function is probably effective and should be considered in patients with Parkinson disease and psychosis
Contraindications
Serious hypersensitivity to clozapine or any component of the formulation (eg, photosensitivity, vasculitis, erythema multiforme, or Stevens-Johnson syndrome [SJS])
Canadian labeling: Additional contraindications (not in US labeling): Myeloproliferative disorders; history of toxic or idiosyncratic agranulocytosis or severe granulocytopenia (unless due to previous chemotherapy); concomitant use with other agents that suppress bone marrow function; active hepatic disease associated with nausea, anorexia, or jaundice; progressive hepatic disease or hepatic failure; paralytic ileus; uncontrolled epilepsy; severe CNS depression or comatose states; severe renal impairment; severe cardiac disease (eg, myocarditis); patients unable to undergo blood testing
Dosage and Administration
Dosing: Adult
Note: Prior to initiating treatment, obtain a baseline CBC, including the ANC; the ANC must be ≥1,500/mm3 for the general population and ≥1,000/mm3 for patients with documented Benign Ethnic Neutropenia (BEN) in order to initiate treatment. To continue treatment, the ANC must be monitored regularly. Laboratory hematology results may be presented in different units; 1 mcL equals 1 mm3.
Bipolar disorder, treatment resistant (acute manic episodes or maintenance treatment; monotherapy or adjunctive therapy) (off-label use): Oral: Initial: 25 mg daily; increase based on response and tolerability in 25 mg increments to a maximum dose of 550 mg/day. Usual daily dose ~100 to 300 mg/day (CANMAT/ISBD [Yatham 2018]; Green 2000; Li 2015; WFSBP [Grunze 2009]).
Psychosis in Parkinson disease (off-label use): Oral: Initial: 6.25 mg/day, in 1 or 2 divided doses; increase based on response and tolerability by 6.25 or 12.5 mg increments in 3- to 7-day intervals to a maximum dose of 50 mg/day (Morgante 2004; Parkinson Study Group 1999; Pollack 2004).
Schizophrenia: Oral: Initial: 12.5 mg once or twice daily; increase, as tolerated, in increments of 25 to 50 mg daily to a target dose of 300 to 450 mg daily (administered in divided doses) by the end of 2 weeks; may further titrate in increments not exceeding 100 mg and no more frequently than once or twice weekly. Maximum total daily dose: 900 mg. Note: In some efficacy studies, total daily dosage was administered in 3 divided doses.
Suicidal behavior in schizophrenia or schizoaffective disorder: Oral: Initial: 12.5 mg once or twice daily; increased, as tolerated, in increments of 25 to 50 mg daily to a target dose of 300 to 450 mg daily (administered in divided doses) by the end of 2 weeks; may further titrate in increments not exceeding 100 mg and no more frequently than once or twice weekly. Mean dose is ~300 mg daily; maximum total daily dose: 900 mg.
Dosage adjustment with concomitant therapy:
Strong CYP1A2 inhibitors (eg, fluvoxamine, ciprofloxacin):
Initiating clozapine with concomitant medication or adding a concomitant medication while taking clozapine: Use one-third of the clozapine dose.
Discontinuing concomitant medication while continuing clozapine: Increase clozapine dose based on clinical response.
Moderate or weak CYP1A2 inhibitors (eg, oral contraceptives, caffeine), CYP2D6 or CYP3A4 inhibitors (eg, cimetidine, escitalopram, erythromycin, paroxetine, bupropion, fluoxetine, quinidine, duloxetine, terbinafine, sertraline):
Initiating clozapine with concomitant medication or adding a concomitant medication while taking clozapine: Monitor for adverse reactions and if necessary, consider reducing the clozapine dose.
Discontinuing concomitant medication while continuing clozapine: Monitor for lack of effectiveness and if necessary, consider increasing the clozapine dose.
Strong CYP3A4 inducers (eg, phenytoin, carbamazepine, St John’s wort, rifampin):
Initiating clozapine with concomitant medication or adding a concomitant medication while taking clozapine: Concomitant use is not recommended. However, if the CYP3A4 inducer is necessary, monitor for decreased effectiveness and if necessary, consider increasing the clozapine dose.
Discontinuing concomitant medication while continuing clozapine: Reduce clozapine dose based on clinical response.
Moderate or weak CYP1A2 (eg, tobacco smoke) or CYP3A4 inducers:
Initiating clozapine with concomitant medication or adding a concomitant medication while taking clozapine: Monitor for decreased effectiveness and if necessary, consider increasing the clozapine dose.
Discontinuing concomitant medication while continuing clozapine: Monitor for adverse reactions and if necessary, consider reducing the clozapine dose.
Reinitiation of therapy: If dosing is interrupted for ≥48 hours, therapy must be reinitiated at 12.5 mg once or twice daily to minimize the risk of hypotension, bradycardia, and syncope; if dose is well tolerated, may be increased more rapidly than with initial titration, unless cardiopulmonary arrest occurred during initial titration, then retitrate with extreme caution.
Discontinuation of therapy: The manufacturer recommends reducing the dose gradually over a period of 1 to 2 weeks if termination of therapy is not related to neutropenia. American Psychiatric Association (APA), Canadian Psychiatric Association (CPA), and World Federation of Societies of Biological Psychiatry (WFSBP) guidelines recommend gradually tapering antipsychotics to avoid withdrawal symptoms and minimize the risk of relapse (APA [Lehman 2004]; Cerovecki 2013; CPA [Addington 2005]; WFSBP [Hasan 2012]); risk for withdrawal symptoms may be highest with highly anticholinergic or dopaminergic antipsychotics (Cerovecki 2013). When stopping antipsychotic therapy in patients with schizophrenia, the CPA guidelines recommend a gradual taper over 6 to 24 months, and the APA guidelines recommend reducing the dose by 10% each month (APA [Lehman 2004]; CPA [Addington 2005]). Continuing anti-parkinsonism agents for a brief period after discontinuation may prevent withdrawal symptoms (Cerovecki 2013). When switching antipsychotics, three strategies have been suggested: Cross-titration (gradually discontinuing the first antipsychotic while gradually increasing the new antipsychotic), overlap and taper (maintaining the dose of the first antipsychotic while gradually increasing the new antipsychotic, then tapering the first antipsychotic), and abrupt change (abruptly discontinuing the first antipsychotic and either increasing the new antipsychotic gradually or starting it at a treatment dose). Evidence supporting ideal switch strategies and taper rates is limited, and results are conflicting (Cerovecki 2013; Remington 2005).
Dosing: Geriatric
Note: Prior to initiating treatment, obtain a baseline CBC, including the ANC; the ANC must be ≥1,500/mm3 for the general population and ≥1,000/mm3 for patients with documented Benign Ethnic Neutropenia (BEN) in order to initiate treatment. To continue treatment, the ANC must be monitored regularly. Laboratory hematology results may be presented in different units; 1 mcL equals 1 mm3.
Schizophrenia: Oral: Experience in the elderly is limited; may initiate with 12.5 mg once daily for 3 days, then increase to 25 mg once daily for 3 days as tolerated; may further increase, as tolerated, in increments of 12.5 to 25 mg daily every 3 days to desired response, up to 700 mg/day (mean dose: 300 mg/day) (Howanitz 1999; Pridan 2015).
Psychosis/agitation (treatment-resistant) associated with dementia (off-label use): Oral: Initial: 12.5 mg at bedtime; titrate by 12.5 mg every 3 to 5 days as needed (given as divided doses in morning and at bedtime); doses as high as 50 mg have been studied (Lee 2007). In patients without a clinically significant response after 4 weeks, taper and withdraw therapy. In patients with an adequate response, attempt to taper and withdraw therapy within 4 months, unless symptoms recurred with a previous taper attempt. Assess symptoms at least monthly during taper and for at least 4 months after withdrawal of therapy (APA [Reus 2016]).
Dosing: Pediatric
Note: Laboratory hematology results may be presented in different units; 1 mcL equals 1 mm3. Obtain a baseline CBC, including the ANC. In order to initiate treatment, minimum baseline ANC values must be met; for the general population, the ANC must be ≥1,500/mm3 and for patients with documented Benign Ethnic Neutropenia (BEN), the ANC must be ≥1,000/mm3. The ANC must be monitored regularly with continued treatment.
Schizophrenia; treatment resistant: Limited data available: Note: Dose should be individualized based on tolerability, concomitant antipsychotic therapy, and clinical response
Initial dose:
Children ≥6 years: Oral: 6.25 or 12.5 mg once daily
Adolescents: Oral: 12.5 mg once or twice daily
Titration and maintenance dosing: Increase daily dose by ≤25 mg increments (lower initial doses should use smaller increments [1 to 2 times the starting dose]), as tolerated, every 3 to 5 days, to a target dose of 200 to 400 mg/day in divided doses. Dose may be divided, with a higher dose at bedtime; if excessive daytime sedation, entire dose may be at bedtime (Findling 2007; Kumar 2013; Kumra 1996; Kumra 2008; Schneider 2014). Mean effective dose range in most pediatric studies: 220 to 431 mg/day (Schneider 2014).
Reinitiation of therapy: Based on experience in adult patients, if dosing is interrupted for ≥48 hours, therapy must be reinitiated at initial doses to minimize the risk of hypotension, bradycardia, and syncope; if dose is well tolerated, may be increased more rapidly than with initial titration, unless cardiopulmonary arrest occurred during initial titration, then retitrate with extreme caution.
Dosing adjustment with concomitant therapy: Children ≥10 years and Adolescents: The presented dosing adjustments are based on experience in adult patients; specific recommendations for pediatric patients are limited.
Strong CYP1A2 inhibitors (eg, fluvoxamine, ciprofloxacin):
Initiating clozapine with concomitant inhibitor or adding a concomitant inhibitor while taking clozapine: Use one-third of the clozapine dose.
Discontinuing concomitant inhibitor while continuing clozapine: Increase clozapine dose based on clinical response.
Moderate or weak CYP1A2 inhibitors (eg, oral contraceptives, caffeine), CYP2D6 or CYP3A4 inhibitors (eg, cimetidine, escitalopram, erythromycin, paroxetine, bupropion, fluoxetine, quinidine, duloxetine, terbinafine, sertraline):
Initiating clozapine with concomitant inhibitor or adding a concomitant inhibitor while taking clozapine: Monitor for adverse reactions and if necessary, consider reducing the clozapine dose.
Discontinuing concomitant inhibitor while continuing clozapine: Monitor for lack of clozapine effectiveness and if necessary, consider increasing the clozapine dose.
Strong CYP3A4 inducers (eg, phenytoin, carbamazepine, St John's wort, rifampin):
Initiating clozapine with concomitant inducer or adding a concomitant inducer while taking clozapine: Concomitant use is not recommended. If the CYP3A4 inducer is necessary, monitor for decreased clozapine effectiveness and if necessary, consider increasing the clozapine dose.
Discontinuing concomitant inducer while continuing clozapine: Reduce clozapine dose based on clinical response.
Moderate or weak CYP1A2 (eg, tobacco smoking) or CYP3A4 inducers:
Initiating clozapine with concomitant inducer or adding a concomitant inducer while taking clozapine: Monitor for decreased clozapine effectiveness and if necessary, consider increasing the clozapine dose.
Discontinuing concomitant inducer while continuing clozapine: Monitor for adverse reactions and if necessary, consider reducing the clozapine dose.
Administration
Administer without regard to food. Total daily dose may be divided into uneven doses with larger dose administered at bedtime.
Orally disintegrating tablet: Remove from foil blister by peeling apart (do not push tablet through the foil). Remove immediately prior to use. Place tablet in mouth and chew or allow to dissolve; swallow with saliva. If dosing requires splitting tablet, throw unused portion away.
Suspension: Shake bottle prior to use. Using syringe adaptor and oral syringe provided withdrawal dose from bottle. Administer immediately after preparation using the oral syringe provided.
Dietary Considerations
Some products may contain phenylalanine.
Storage
Suspension: Store at ≤25°C (77°F). Protect from light. Do not refrigerate or freeze. Stable for 100 days after initial bottle opening.
Tablet: Store at ≤30°C (86°F).
Tablet, dispersible: Store at 20°C to 25°C (68°F to 77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Protect from moisture; do not remove from package until ready to use.
CloZAPine Images
Drug Interactions
Acetylcholinesterase Inhibitors: May diminish the therapeutic effect of Anticholinergic Agents. Anticholinergic Agents may diminish the therapeutic effect of Acetylcholinesterase Inhibitors. Monitor therapy
Acetylcholinesterase Inhibitors (Central): May enhance the neurotoxic (central) effect of Antipsychotic Agents. Severe extrapyramidal symptoms have occurred in some patients. Monitor therapy
Aclidinium: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Alcohol (Ethyl): CNS Depressants may enhance the CNS depressant effect of Alcohol (Ethyl). Monitor therapy
Alfuzosin: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Alizapride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Alpha-/Beta-Agonists: CloZAPine may diminish the therapeutic effect of Alpha-/Beta-Agonists. Exceptions: EPINEPHrine (Nasal); EPINEPHrine (Oral Inhalation); Isometheptene; Levonordefrin; Pseudoephedrine. Monitor therapy
Amifampridine: Agents With Seizure Threshold Lowering Potential may enhance the neuroexcitatory and/or seizure-potentiating effect of Amifampridine. Monitor therapy
Amifostine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Amifostine. Management: When amifostine is used at chemotherapy doses, blood pressure lowering medications should be withheld for 24 hours prior to amifostine administration. If blood pressure lowering therapy cannot be withheld, amifostine should not be administered. Consider therapy modification
Amisulpride: Antipsychotic Agents may enhance the adverse/toxic effect of Amisulpride. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Avoid combination
Amisulpride: May enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Avoid combination
Amphetamines: Antipsychotic Agents may diminish the stimulatory effect of Amphetamines. Monitor therapy
Anticholinergic Agents: May enhance the adverse/toxic effect of other Anticholinergic Agents. Monitor therapy
Antidiabetic Agents: Hyperglycemia-Associated Agents may diminish the therapeutic effect of Antidiabetic Agents. Monitor therapy
Anti-Parkinson Agents (Dopamine Agonist): Antipsychotic Agents (Second Generation [Atypical]) may diminish the therapeutic effect of Anti-Parkinson Agents (Dopamine Agonist). Management: Consider using an alternative antipsychotic agent when possible in patients with Parkinson disease. If an atypical antipsychotic is necessary, consider using clozapine or quetiapine, which may convey the lowest interaction risk. Consider therapy modification
Antipsychotic Agents (Second Generation [Atypical]): Blood Pressure Lowering Agents may enhance the hypotensive effect of Antipsychotic Agents (Second Generation [Atypical]). Monitor therapy
Azelastine (Nasal): CNS Depressants may enhance the CNS depressant effect of Azelastine (Nasal). Avoid combination
Barbiturates: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Benperidol: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Benzodiazepines: May enhance the adverse/toxic effect of CloZAPine. Management: Consider decreasing the dose of (or possibly discontinuing) benzodiazepines prior to initiating clozapine. Consider therapy modification
Blonanserin: CNS Depressants may enhance the CNS depressant effect of Blonanserin. Consider therapy modification
Blood Pressure Lowering Agents: May enhance the hypotensive effect of Antipsychotic Agents (Second Generation [Atypical]). Monitor therapy
Blood Pressure Lowering Agents: May enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Botulinum Toxin-Containing Products: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Brexanolone: CNS Depressants may enhance the CNS depressant effect of Brexanolone. Monitor therapy
Brimonidine (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Brimonidine (Topical): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Bromopride: May enhance the adverse/toxic effect of Antipsychotic Agents. Avoid combination
Bromperidol: Blood Pressure Lowering Agents may enhance the hypotensive effect of Bromperidol. Bromperidol may diminish the hypotensive effect of Blood Pressure Lowering Agents. Avoid combination
Bromperidol: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Buprenorphine: CNS Depressants may enhance the CNS depressant effect of Buprenorphine. Management: Consider reduced doses of other CNS depressants, and avoiding such drugs in patients at high risk of buprenorphine overuse/self-injection. Initiate buprenorphine at lower doses in patients already receiving CNS depressants. Consider therapy modification
BuPROPion: May enhance the neuroexcitatory and/or seizure-potentiating effect of Agents With Seizure Threshold Lowering Potential. Monitor therapy
Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Cannabis: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
CarBAMazepine: May enhance the myelosuppressive effect of CloZAPine. More specifically, the risk of bone marrow suppression with this combination may be increased due to the independent myelosuppressive effects of the drugs. CarBAMazepine may decrease the serum concentration of CloZAPine. Avoid combination
Ceritinib: May enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Chloral Betaine: May enhance the adverse/toxic effect of Anticholinergic Agents. Monitor therapy
Chlormethiazole: May enhance the CNS depressant effect of CNS Depressants. Management: Monitor closely for evidence of excessive CNS depression. The chlormethiazole labeling states that an appropriately reduced dose should be used if such a combination must be used. Consider therapy modification
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Cimetidine: May increase the serum concentration of CloZAPine. Management: Consider use of an alternative H2 antagonist. Monitor for increased toxic effects of clozapine if cimetidine is initiated/dose increased, or decreased effects if cimetidine is discontinued/dose decreased. Consider therapy modification
Cimetropium: Anticholinergic Agents may enhance the anticholinergic effect of Cimetropium. Avoid combination
Ciprofloxacin (Systemic): May enhance the QTc-prolonging effect of CloZAPine. Ciprofloxacin (Systemic) may increase the serum concentration of CloZAPine. Management: Reduce the clozapine dose to one-third of the original dose when adding ciprofloxacin and monitor closely for evidence of excessive QTc prolongation and clozapine toxicity. Resume the previous clozapine dose following ciprofloxacin discontinuation. Consider therapy modification
Clarithromycin: QT-prolonging Antipsychotics (Moderate Risk) may enhance the QTc-prolonging effect of Clarithromycin. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
CNS Depressants: May enhance the adverse/toxic effect of other CNS Depressants. Monitor therapy
CYP1A2 Inducers (Moderate): May decrease the serum concentration of CloZAPine. Monitor therapy
CYP1A2 Inducers (Weak): May decrease the serum concentration of CloZAPine. Monitor therapy
CYP1A2 Inhibitors (Moderate): May increase the serum concentration of CloZAPine. Exceptions: Ciprofloxacin (Systemic). Monitor therapy
CYP1A2 Inhibitors (Strong): May increase the serum concentration of CloZAPine. Management: Reduce the dose of clozapine to one-third of the original dose when adding a strong CYP1A2 inhibitor and monitor patient response closely. Return to the original clozapine dose when the strong CYP1A2 inhibitor is discontinued. Consider therapy modification
CYP1A2 Inhibitors (Weak): May increase the serum concentration of CloZAPine. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Exceptions: Propafenone. Monitor therapy
CYP2D6 Inhibitors (Moderate): May increase the serum concentration of CloZAPine. Monitor therapy
CYP2D6 Inhibitors (Strong): May increase the serum concentration of CloZAPine. Monitor therapy
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CloZAPine. Monitor therapy
CYP3A4 Inducers (Strong): May decrease the serum concentration of CloZAPine. Avoid combination
CYP3A4 Inducers (Weak): May decrease the serum concentration of CloZAPine. Monitor therapy
CYP3A4 Inhibitors (Strong): May increase the serum concentration of CloZAPine. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Exceptions: Ceritinib; Clarithromycin; Saquinavir; Voriconazole. Monitor therapy
Deutetrabenazine: May enhance the adverse/toxic effect of Antipsychotic Agents. Specifically, the risk for akathisia, parkinsonism, or neuroleptic malignant syndrome may be increased. Monitor therapy
Diazoxide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Dimethindene (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Domperidone: QT-prolonging Agents (Moderate Risk) may enhance the QTc-prolonging effect of Domperidone. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Doxylamine: May enhance the CNS depressant effect of CNS Depressants. Management: The manufacturer of Diclegis (doxylamine/pyridoxine), intended for use in pregnancy, specifically states that use with other CNS depressants is not recommended. Monitor therapy
Dronabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
DULoxetine: Blood Pressure Lowering Agents may enhance the hypotensive effect of DULoxetine. Monitor therapy
Eluxadoline: Anticholinergic Agents may enhance the constipating effect of Eluxadoline. Avoid combination
Esketamine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Fexinidazole [INT]: May enhance the QTc-prolonging effect of QT-prolonging Agents (Moderate Risk). Avoid combination
Flunitrazepam: CNS Depressants may enhance the CNS depressant effect of Flunitrazepam. Consider therapy modification
Gastrointestinal Agents (Prokinetic): Anticholinergic Agents may diminish the therapeutic effect of Gastrointestinal Agents (Prokinetic). Monitor therapy
Glucagon: Anticholinergic Agents may enhance the adverse/toxic effect of Glucagon. Specifically, the risk of gastrointestinal adverse effects may be increased. Monitor therapy
Glycopyrrolate (Oral Inhalation): Anticholinergic Agents may enhance the anticholinergic effect of Glycopyrrolate (Oral Inhalation). Avoid combination
Glycopyrronium (Topical): May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Guanethidine: Antipsychotic Agents may diminish the therapeutic effect of Guanethidine. Monitor therapy
Haloperidol: QT-prolonging Antipsychotics (Moderate Risk) may enhance the QTc-prolonging effect of Haloperidol. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Herbs (Hypotensive Properties): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
HYDROcodone: CNS Depressants may enhance the CNS depressant effect of HYDROcodone. Management: Avoid concomitant use of hydrocodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
HydrOXYzine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Hypotension-Associated Agents: Blood Pressure Lowering Agents may enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Iohexol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iohexol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iohexol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Iomeprol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iomeprol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iomeprol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Iopamidol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iopamidol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iopamidol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Ipratropium (Oral Inhalation): May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Itopride: Anticholinergic Agents may diminish the therapeutic effect of Itopride. Monitor therapy
Kava Kava: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Lemborexant: May enhance the CNS depressant effect of CNS Depressants. Management: Dosage adjustments of lemborexant and of concomitant CNS depressants may be necessary when administered together because of potentially additive CNS depressant effects. Close monitoring for CNS depressant effects is necessary. Consider therapy modification
Levosulpiride: Anticholinergic Agents may diminish the therapeutic effect of Levosulpiride. Avoid combination
Lithium: May enhance the neurotoxic effect of Antipsychotic Agents. Lithium may decrease the serum concentration of Antipsychotic Agents. Specifically noted with chlorpromazine. Monitor therapy
Magnesium Sulfate: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Mequitazine: Antipsychotic Agents may enhance the arrhythmogenic effect of Mequitazine. Management: Consider alternatives to one of these agents when possible. While this combination is not specifically contraindicated, mequitazine labeling describes this combination as discouraged. Consider therapy modification
Methotrimeprazine: CNS Depressants may enhance the CNS depressant effect of Methotrimeprazine. Methotrimeprazine may enhance the CNS depressant effect of CNS Depressants. Management: Reduce adult dose of CNS depressant agents by 50% with initiation of concomitant methotrimeprazine therapy. Further CNS depressant dosage adjustments should be initiated only after clinically effective methotrimeprazine dose is established. Consider therapy modification
Methylphenidate: Antipsychotic Agents may enhance the adverse/toxic effect of Methylphenidate. Methylphenidate may enhance the adverse/toxic effect of Antipsychotic Agents. Monitor therapy
Metoclopramide: May enhance the adverse/toxic effect of Antipsychotic Agents. Avoid combination
MetyroSINE: CNS Depressants may enhance the sedative effect of MetyroSINE. Monitor therapy
MetyroSINE: May enhance the adverse/toxic effect of Antipsychotic Agents. Monitor therapy
Mianserin: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Minocycline (Systemic): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Mirabegron: Anticholinergic Agents may enhance the adverse/toxic effect of Mirabegron. Monitor therapy
Molsidomine: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Myelosuppressive Agents: May enhance the adverse/toxic effect of CloZAPine. Specifically, the risk for neutropenia may be increased. Exceptions: Dasatinib; Inotuzumab Ozogamicin; Midostaurin; Nilotinib; Osimertinib; Ribociclib. Monitor therapy
Nabilone: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Naftopidil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nefazodone: May decrease the metabolism of CloZAPine. Monitor therapy
Nicergoline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicorandil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nitroglycerin: Anticholinergic Agents may decrease the absorption of Nitroglycerin. Specifically, anticholinergic agents may decrease the dissolution of sublingual nitroglycerin tablets, possibly impairing or slowing nitroglycerin absorption. Monitor therapy
Nitroprusside: Blood Pressure Lowering Agents may enhance the hypotensive effect of Nitroprusside. Monitor therapy
Obinutuzumab: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Management: Consider temporarily withholding blood pressure lowering medications beginning 12 hours prior to obinutuzumab infusion and continuing until 1 hour after the end of the infusion. Consider therapy modification
Omeprazole: May decrease the serum concentration of CloZAPine. Omeprazole may increase the serum concentration of CloZAPine. Monitor therapy
Ondansetron: May enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Opioid Agonists: CNS Depressants may enhance the CNS depressant effect of Opioid Agonists. Management: Avoid concomitant use of opioid agonists and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Orphenadrine: CNS Depressants may enhance the CNS depressant effect of Orphenadrine. Avoid combination
Oxatomide: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Oxomemazine: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
OxyCODONE: CNS Depressants may enhance the CNS depressant effect of OxyCODONE. Management: Avoid concomitant use of oxycodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Paraldehyde: CNS Depressants may enhance the CNS depressant effect of Paraldehyde. Avoid combination
Pentamidine (Systemic): May enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Pentoxifylline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Perampanel: May enhance the CNS depressant effect of CNS Depressants. Management: Patients taking perampanel with any other drug that has CNS depressant activities should avoid complex and high-risk activities, particularly those such as driving that require alertness and coordination, until they have experience using the combination. Consider therapy modification
Phenylephrine (Systemic): CloZAPine may diminish the therapeutic effect of Phenylephrine (Systemic). Monitor therapy
Pholcodine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Pholcodine. Monitor therapy
Phosphodiesterase 5 Inhibitors: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Pimozide: May enhance the QTc-prolonging effect of QT-prolonging Agents (Moderate Risk). Avoid combination
Potassium Chloride: Anticholinergic Agents may enhance the ulcerogenic effect of Potassium Chloride. Management: Patients on drugs with substantial anticholinergic effects should avoid using any solid oral dosage form of potassium chloride. Avoid combination
Potassium Citrate: Anticholinergic Agents may enhance the ulcerogenic effect of Potassium Citrate. Avoid combination
Pramlintide: May enhance the anticholinergic effect of Anticholinergic Agents. These effects are specific to the GI tract. Consider therapy modification
Prostacyclin Analogues: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
QT-prolonging Agents (Highest Risk): May enhance the QTc-prolonging effect of CloZAPine. Management: Consider alternatives to this combination. Patients with other risk factors (eg, older age, female sex, bradycardia, hypokalemia, hypomagnesemia, heart disease, and higher drug concentrations) are likely at greater risk for these toxicities. Exceptions: QuiNIDine. Consider therapy modification
QT-prolonging Antidepressants (Moderate Risk): QT-prolonging Antipsychotics (Moderate Risk) may enhance the QTc-prolonging effect of QT-prolonging Antidepressants (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Antipsychotics (Moderate Risk): May enhance the QTc-prolonging effect of CloZAPine. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Amisulpride; CloZAPine; Pimozide. Monitor therapy
QT-prolonging Class IC Antiarrhythmics (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Kinase Inhibitors (Moderate Risk): QT-prolonging Antipsychotics (Moderate Risk) may enhance the QTc-prolonging effect of QT-prolonging Kinase Inhibitors (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Miscellaneous Agents (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Domperidone. Monitor therapy
QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Quinolone Antibiotics (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Quinagolide: Antipsychotic Agents may diminish the therapeutic effect of Quinagolide. Monitor therapy
Quinagolide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
QuiNIDine: CloZAPine may enhance the anticholinergic effect of QuiNIDine. CloZAPine may enhance the QTc-prolonging effect of QuiNIDine. QuiNIDine may increase the serum concentration of CloZAPine. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Ramosetron: Anticholinergic Agents may enhance the constipating effect of Ramosetron. Monitor therapy
Revefenacin: Anticholinergic Agents may enhance the anticholinergic effect of Revefenacin. Avoid combination
Rufinamide: May enhance the adverse/toxic effect of CNS Depressants. Specifically, sleepiness and dizziness may be enhanced. Monitor therapy
Saquinavir: May enhance the QTc-prolonging effect of CloZAPine. Avoid combination
Secretin: Anticholinergic Agents may diminish the therapeutic effect of Secretin. Management: Avoid concomitant use of anticholinergic agents and secretin. Discontinue anticholinergic agents at least 5 half-lives prior to administration of secretin. Consider therapy modification
Selective Serotonin Reuptake Inhibitors: CNS Depressants may enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk of psychomotor impairment may be enhanced. Monitor therapy
Serotonergic Agents (High Risk): May enhance the adverse/toxic effect of Antipsychotic Agents. Specifically, serotonergic agents may enhance dopamine blockade, possibly increasing the risk for neuroleptic malignant syndrome. Antipsychotic Agents may enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Monitor therapy
Sodium Oxybate: May enhance the CNS depressant effect of CNS Depressants. Management: Consider alternatives to combined use. When combined use is needed, consider minimizing doses of one or more drugs. Use of sodium oxybate with alcohol or sedative hypnotics is contraindicated. Consider therapy modification
St John's Wort: May decrease the serum concentration of CloZAPine. Avoid combination
Sulpiride: Antipsychotic Agents may enhance the adverse/toxic effect of Sulpiride. Avoid combination
Suvorexant: CNS Depressants may enhance the CNS depressant effect of Suvorexant. Management: Dose reduction of suvorexant and/or any other CNS depressant may be necessary. Use of suvorexant with alcohol is not recommended, and the use of suvorexant with any other drug to treat insomnia is not recommended. Consider therapy modification
Tapentadol: May enhance the CNS depressant effect of CNS Depressants. Management: Avoid concomitant use of tapentadol and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Tetrabenazine: May enhance the adverse/toxic effect of Antipsychotic Agents. Monitor therapy
Tetrahydrocannabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Thalidomide: CNS Depressants may enhance the CNS depressant effect of Thalidomide. Avoid combination
Thiazide and Thiazide-Like Diuretics: Anticholinergic Agents may increase the serum concentration of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Tiotropium: Anticholinergic Agents may enhance the anticholinergic effect of Tiotropium. Avoid combination
Tobacco (Smoked): May decrease the serum concentration of CloZAPine. Monitor therapy
Topiramate: Anticholinergic Agents may enhance the adverse/toxic effect of Topiramate. Monitor therapy
Trimeprazine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Umeclidinium: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Voriconazole: May enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Zolpidem: CNS Depressants may enhance the CNS depressant effect of Zolpidem. Management: Reduce the Intermezzo brand sublingual zolpidem adult dose to 1.75 mg for men who are also receiving other CNS depressants. No such dose change is recommended for women. Avoid use with other CNS depressants at bedtime; avoid use with alcohol. Consider therapy modification
Adverse Reactions
>10%:
Cardiovascular: Tachycardia (17% to 25%), hypotension (9% to 13%), hypertension (4% to 12%)
Central nervous system: Drowsiness (≤39% to 46%), sedation (≤39%), dizziness (14% to 27%), insomnia (2% to 20%), vertigo (≤19%)
Gastrointestinal: Sialorrhea (13% to 48%), weight gain (4% to 31%), constipation (14% to 25%), nausea (5% to 17%), vomiting (3% to 17%), dyspepsia (14%)
Miscellaneous: Fever (5% to 13%)
1% to 10%:
Cardiovascular: Syncope (6%)
Central nervous system: Headache (7% to 10%), agitation (4%), restlessness (4%), akinesia (≤4%), disturbed sleep (≤4%), nightmares (≤4%), akathisia (3%), confusion (3%), seizure (3%; dose related), fatigue (2%)
Dermatologic: Diaphoresis (6%), skin rash (2%)
Gastrointestinal: Xerostomia (5% to 6%), abdominal distress (≤4%), heartburn (≤4%), diarrhea (2%)
Genitourinary: Urine abnormality (2%)
Hematologic & oncologic: Leukopenia (≤3%), neutropenia (≤3%), eosinophilia (1%)
Neuromuscular & skeletal: Tremor (6%), hypokinesia (≤4%), muscle rigidity (3%)
Ophthalmic: Visual disturbance (5%)
<1%, postmarketing, and/or case reports: Abnormal electrocephalogram, agranulocytosis, angioedema, aspiration, bradycardia, cardiac arrhythmia (atrial or ventricular), cardiac failure, cardiomyopathy (usually dilated), cataplexy, cerebrovascular accident, cholestasis, colitis, deep vein thrombosis, delirium, diabetes mellitus, DRESS syndrome, dyschromia, dysphagia, enlargement of salivary glands, erythema multiforme, esophageal dysmotility, fecal impaction, gastroenteritis, granulocytopenia, hepatic cirrhosis, hepatic fibrosis, hepatic insufficiency, hepatic necrosis, hepatitis, hepatotoxicity, hyperglycemia, hyperosmolar coma, hypersensitivity reaction, hyperuricemia, hyponatremia, increased creatine phosphokinase, increased erythrocyte sedimentation rate, increased hematocrit, increased hemoglobin, increased serum cholesterol, increased serum triglycerides, interstitial nephritis (acute), intestinal obstruction, jaundice, ketoacidosis, leukocytosis, liver injury, liver steatosis, lower respiratory tract infection, mitral valve insufficiency, myasthenia syndrome, myocardial infarction, myocarditis, myoclonus, neuroleptic malignant syndrome, nocturnal enuresis, obsessive compulsive disorder, obstructive sleep apnea syndrome (Shirani 2011), orthostatic hypotension, palpitations, pancreatitis (acute), paralytic ileus, paresthesia, periorbital edema, pheochromocytoma (pseudo), pleural effusion, pneumonia, priapism, prolonged QT interval on ECG, psychosis (exacerbated), pulmonary embolism, renal failure, retrograde ejaculation, rhabdomyolysis, sialadenitis, sepsis, skin photosensitivity, status epilepticus, Stevens-Johnson syndrome, syncope, systemic lupus erythematosus, tardive dyskinesia, thrombocytopenia, thrombocytosis, torsades de pointes, vasculitis, weight loss
Warnings/Precautions
Concerns related to adverse effects:
- Anticholinergic effects: May cause anticholinergic effects (constipation, xerostomia, blurred vision, urinary retention); use with caution in patients with decreased gastrointestinal motility, urinary retention, BPH, xerostomia, or visual problems. Because of its potential to significantly decrease GI motility, use is associated with increased risk of paralytic ileus, bowel obstruction, fecal impaction, bowel perforation, and in rare cases death. Bowel regimens and monitoring are recommended (De Hert 2011; Nielsen 2012; Palmer 2008). If ileus or subileus occur discontinue clozapine and reintroduce after addressing inadequate dietary and bowel habits (Nielsen 2013). Relative to other neuroleptics, clozapine has a high potency of cholinergic blockade (Richelson 1999).
- Cardiovascular events:
- [US Boxed Warning]: Orthostatic hypotension, bradycardia, syncope, and cardiac arrest have been reported with clozapine treatment. Risk is highest during the initial titration period especially with rapid dose increases. Symptoms can develop with the first dose and with doses as low as 12.5 mg per day. Initiate treatment with no more than 12.5 mg once daily or twice daily; titrate slowly, and use divided doses. Use with caution in patients at risk for these effects (eg, cerebrovascular disease, cardiovascular disease) or with predisposing conditions for hypotensive episodes (eg, hypovolemia, concurrent antihypertensive medication); reactions can be fatal. Consider dose reduction if hypotension occurs. If patients have had even a brief interval off clozapine (≥2 days), reinitiate treatment at 12.5 mg once daily or twice daily. If the first several doses are tolerated, clozapine may be re-titrated more quickly when the risk of adverse events is low. May also cause tachycardia; tachycardia is not limited to a reflex response to orthostatic hypotension.
- [US Boxed Warning]: Fatalities due to myocarditis and cardiomyopathy have been reported. Upon suspicion of these reactions, discontinue clozapine and obtain a cardiac evaluation. Signs and symptoms may include chest pain, tachycardia, palpitations, dyspnea, fever, flu-like symptoms, hypotension, ECG changes, eosinophilia, and/or elevated C-reactive protein. Patients with clozapine-related myocarditis or cardiomyopathy should generally not be rechallenged with clozapine. If the benefit of treatment is judged to outweigh the potential risks of recurrent myocarditis or cardiomyopathy, rechallenge may be considered in consultation with a cardiologist, after a complete cardiac evaluation, and under close monitoring. Myocarditis and cardiomyopathy may occur at any period during clozapine treatment; however, typically myocarditis presents within the first 2 months and cardiomyopathy after 8 weeks of treatment. Mitral valve incompetence has been reported in patients who are diagnosed with cardiomyopathy while taking clozapine. In a scientific statement from the American Heart Association, clozapine has been determined to be an agent that may cause direct myocardial toxicity (magnitude: major) (AHA [Page 2016]).
- CNS depression: May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks that require mental alertness (eg, operating machinery or driving).
- Dyslipidemia: Undesirable changes in lipids have been observed with antipsychotic therapy; incidence varies with product. Periodically monitor total serum cholesterol, triglycerides, LDL, and HDL concentrations. Compared with other antipsychotics, the risk of dyslipidemia is high (Solmi 2017).
- Eosinophilia: Eosinophilia (ie, an eosinophil count >700/mm3) has been reported to occur (usually within first month) with clozapine treatment. If eosinophilia develops, evaluate for signs or symptoms of systemic reactions (eg, rash or other allergic symptoms), myocarditis, or organ-specific disease. If systemic disease is suspected, discontinue clozapine immediately. If a cause of eosinophilia unrelated to clozapine is identified, treat the underlying cause and continue clozapine. If cause of eosinophilia is related to clozapine, but is in the absence of organ involvement, continue clozapine under careful monitoring. If the total eosinophil count continues to increase over several weeks in the absence of systemic disease, base decision to interrupt treatment and rechallenge (after eosinophil count decreases) on an overall clinical assessment, in consultation with internist or hematologist.
- Esophageal dysmotility/aspiration: Antipsychotic use has been associated with esophageal dysmotility and aspiration; risk increases with age. Use with caution in patients at risk for aspiration pneumonia (eg, Alzheimer disease), particularly in patients >75 years (Herzig 2017; Maddalena 2004). Clozapine-induced sialorrhea may also increase the risk of aspiration pneumonia (Gurrera 2016).
- Extrapyramidal symptoms: May cause extrapyramidal symptoms (EPS), including pseudoparkinsonism, acute dystonic reactions, akathisia, and tardive dyskinesia (risk of these reactions is generally much lower relative to typical/conventional antipsychotics; frequencies reported are similar to placebo). Risk of dystonia (and probably other EPS) may be greater with increased doses, use of conventional antipsychotics, males, and younger patients. Factors associated with greater vulnerability to tardive dyskinesia include older in age, female gender combined with postmenopausal status, Parkinson disease, pseudoparkinsonism symptoms, affective disorders (particularly major depressive disorder), concurrent medical diseases such as diabetes, previous brain damage, alcoholism, poor treatment response, and use of high doses of antipsychotics (APA [Lehman 2004]; Soares-Weiser 2007). Consider therapy discontinuation with signs/symptoms of tardive dyskinesia.
- Falls: May increase the risk for falls due to somnolence, orthostatic hypotension, and motor or sensory instability. Complete fall risk assessments at baseline and periodically during treatment in patients with diseases or on medications that may also increase fall risk.
- Fever: Benign transient temperature elevation (>38°C or 100.4°F) may occur; peaking within the first 3 weeks of treatment. May be associated with an increase or decrease in WBC count. Rule out infection, severe neutropenia, myocarditis, and neuroleptic malignant syndrome (NMS) in patients presenting with fever. While it may be appropriate to withhold clozapine doses temporarily while ruling out serious causes of fever, treatment should not be abruptly discontinued for a benign fever with unknown cause (Nielson 2013).
- Hepatotoxicity: Severe, life-threatening and sometimes fatal hepatotoxicity, including hepatic failure, hepatic necrosis, and hepatitis have been reported. Monitor for signs and symptoms of hepatotoxicity including fatigue, malaise, anorexia, nausea, jaundice, bilirubinemia, coagulopathy, and hepatic encephalopathy. Consider permanently discontinuing therapy if hepatitis or transaminase elevations combined with other systemic symptoms occur during clozapine therapy.
- Hyperglycemia: Atypical antipsychotics have been associated with development of hyperglycemia; in some cases, may be extreme and associated with ketoacidosis, hyperosmolar coma, or death. In some cases, hyperglycemia resolved after discontinuation of the antipsychotic; however, some patients have required continuation of antidiabetic treatment. All patients should be monitored for symptoms of hyperglycemia (eg, polydipsia, polyuria, polyphagia, weakness). Use with caution in patients with diabetes or other disorders of glucose regulation; monitor for worsening of glucose control during therapy. Patients with risk factors for diabetes (eg, obesity or family history) should have a baseline fasting blood sugar (FBS) and periodically during treatment. Discontinue immediately in cases of diabetic ketoacidosis or hyperosmolar coma; cautiously restart with monitoring after sustained control of diabetes and removal of potential diabetogenic medications or treatment of diabetogenic comorbidities (Nielsen 2013). Compared with other antipsychotics, the risk of hyperglycemia is high (Solmi 2017).
- Neuroleptic malignant syndrome: Use may be associated with NMS; monitor for mental status changes, fever, muscle rigidity and/or autonomic instability. NMS can recur. Following recovery from NMS, reintroduction of drug therapy should be carefully considered; if an antipsychotic agent is resumed, monitor closely for NMS.
- Neutropenia: [US Boxed Warning]: Clozapine treatment has caused severe neutropenia, defined as an absolute neutrophil count (ANC) less than 500/mm3. Severe neutropenia can lead to serious infection and death. Prior to initiating treatment, a baseline ANC must be ≥1,500/mm3 for the general population and must be ≥1,000/mm3 for patients with documented Benign Ethnic Neutropenia. During treatment, patients must have regular ANC monitoring. Advise patients to immediately report symptoms consistent with severe neutropenia or infection (eg, fever, weakness, lethargy, sore throat). Risk is greatest within the first 18 weeks of therapy. The mechanism of clozapine-induced neutropenia is unknown and is not dose-dependent. Because of the risk of severe neutropenia, clozapine is available only through a restricted program under a Risk Evaluation Mitigation Strategy (REMS) called the Clozapine REMS Program.
- QT prolongation: Clozapine is associated with QT prolongation and ventricular arrhythmias including torsade de pointes; cardiac arrest and sudden death may occur. Use caution in patients with conditions that may increase the risk of QT prolongation, including history of QT prolongation, long QT syndrome, family history of long QT syndrome or sudden cardiac death, significant cardiac arrhythmia, recent myocardial infarction, uncompensated heart failure, treatment with other medications that cause QT prolongation, treatment with medications that inhibit the metabolism of clozapine, hypokalemia, and hypomagnesemia. Consider obtaining a baseline ECG and serum chemistry panel. Correct electrolyte abnormalities prior to initiating therapy. Discontinue clozapine if QTc interval >500 msec.
- Seizures: [US Boxed Warning]: Seizures have been associated with clozapine use in a dose-dependent manner. Initiate treatment with no more than 12.5 mg, titrate gradually using divided dosing. Use with caution in patients at risk of seizures, including those with a history of seizures, head trauma, brain damage, alcoholism, or concurrent therapy with medications which may lower seizure threshold. Elderly patients may be at increased risk of seizures due to an increased prevalence of predisposing factors (Gareri 2008).
- Sialorrhea: Sialorrhea and drooling may occur with clozapine use; symptoms may be more profound during sleep and may be dose-related. As a result of excessive saliva, patients may initially experience choking sensations that cause nighttime awakening, hoarseness or dysphonia of the voice, and a chronic cough. Skin irritation and infections, aspiration pneumonia, chronic sleep disturbances with daytime fatigue and somnolence, painful swelling of the salivary glands, and symptomatic aerophagia with resultant gas bloating, pain, and flatus may also develop. Titrate clozapine slowly to minimize the chances of inducing sialorrhea; consider dose reduction with or without therapeutic augmentation, or therapeutic substitution, if symptoms develop. Nonpharmacological strategies such as propping head up on several pillows while sleeping, sleeping on the side, placing a towel over pillow to prevent soaking, or chewing sugar free gum may be considered in milder cases (Praharaj 2006). Limited evidence exists for pharmacologic interventions; use extreme caution with drugs that have anticholinergic effects to avoid additive adverse effects with clozapine including constipation or cognitive impairment (APA [Lehman 2004]; Praharaj 2006).
- Suicidal ideation: The possibility of a suicide attempt is inherent in psychotic illness or bipolar disorder; use with caution in high-risk patients during initiation of therapy. Prescriptions should be written for the smallest quantity consistent with good patient care.
- Temperature regulation: Impaired core body temperature regulation may occur; caution with strenuous exercise, heat exposure, dehydration, and concomitant medication possessing anticholinergic effects (Kerwin 2004; Safferman 1991).
- Thromboembolism: Cases of deep vein thrombosis and pulmonary embolism (some fatal) have been associated with clozapine. Avoidance of risk factors such as weight gain and sedentary lifestyle may minimize the risk (Paciullo 2008). Balance the benefits and risks of continuing clozapine if thromboembolism occurs; discontinue if there is a recurrence of thromboembolism despite prophylactic treatment (Nielsen 2013).
- Weight gain: Significant weight gain has been observed with antipsychotic therapy; incidence varies with product. Monitor waist circumference and BMI. Compared with other antipsychotics, the risk of weight gain is high (Solmi 2017).
Disease-related concerns:
- Acute infectious/inflammatory processes: Elevation of serum clozapine levels have been reported in the setting of acute infection or inflammatory process. Reactions ranging from mild sedation to symptoms requiring an ICU level of care have been reported. Significant increases of serum levels do not always correlate with clinical signs and symptoms of clozapine toxicity. Signs and symptoms such as hypotension, sialorrhea, and sedation that cannot be explained by other medications or conditions may necessitate a temporary dose reduction or discontinuation, depending on the severity (Clark 2017; Leung 2014).
- Benign ethnic neutropenia: Patients with benign ethnic neutropenia (BEN), a condition observed in certain ethnic groups whose average ANC values are lower than standard laboratory ranges for neutrophils, have different ANC monitoring parameters due to their lower baseline ANC levels. BEN is most commonly observed in individuals of African descent, some Middle Eastern ethic group, in other non-Caucasian ethnic groups with darker skin, and in men. BEN patients are not at increased risk for developing clozapine-induced neutropenia. Consider hematology consultation prior to initiation.
- Cardiovascular disease: Use with caution in patients with cardiovascular disease; gradually increase dose.
- Dementia: [US Boxed Warning]: Elderly patients with dementia-related psychosis treated with antipsychotics are at an increased risk of death compared to placebo. Most deaths appeared to be either cardiovascular (eg, heart failure, sudden death) or infectious (eg, pneumonia) in nature. Use with caution in patients with Lewy body dementia or Parkinson disease dementia due to greater risk of adverse effects, increased sensitivity to extrapyramidal effects, and association with irreversible cognitive decompensation or death (APA [Reus 2016]). Clozapine is not approved for the treatment of dementia-related psychosis.
- Hepatic impairment: Use with caution in patients with hepatic disease or impairment; monitor hepatic function regularly. Dosage reduction may be necessary in patients with significant hepatic impairment.
- Renal impairment: Use with caution in patients with renal impairment. Dosage reduction may be necessary in patients with significant renal impairment.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- CYP2D6 poor metabolizers: Clozapine concentrations may be increased in CYP2D6 poor metabolizers. Dose reduction may be necessary.
- Elderly: The elderly are more susceptible to adverse effects (including agranulocytosis, cardiovascular, anticholinergic, and tardive dyskinesia).
- Smokers: Clozapine levels may be lower in patients who smoke. Smokers may require twice the daily dose as nonsmokers in order to obtain an equivalent clozapine concentration (Tsuda 2014). Smoking cessation may cause toxicity in a patient stabilized on clozapine. Monitor change in smoking patterns. Consider baseline serum clozapine levels and/or empiric dosage adjustments (30% to 40% reduction) in patients expected to have a prolonged hospital stay with forced smoking cessation. Case reports suggest symptoms from increasing clozapine concentrations may develop 2 to 4 weeks after smoking cessation (Lowe 2010).
Dosage form specific issues:
- Brand/generic: Use caution when converting from brand to generic formulation; poor tolerability, including relapse, has been reported usually soon after product switch (1 to 3 months); monitor closely during this time (Bobo 2010).
- Phenylalanine: FazaClo oral disintegrating tablets contain phenylalanine.
Other warnings/precautions:
- Discontinuation of therapy: The manufacturer recommends reducing the dose gradually over a period of 1 to 2 weeks if termination of therapy is not related to neutropenia. When discontinuing antipsychotic therapy, the APA, CPA, and WFSBP guidelines recommend gradually tapering antipsychotics to avoid physical withdrawal symptoms, including anorexia, anxiety, diaphoresis, diarrhea, dizziness, dyskinesia, headache, myalgia, nausea, paresthesia, restlessness, tremulousness, and vomiting (APA [Lehman 2004]; CPA [Addington 2005]; Lambert 2007; WFSBP [Hasan 2012]). The risk of withdrawal symptoms is highest following abrupt discontinuation of highly anticholinergic or dopaminergic antipsychotics (Cerovecki 2013). Additional factors such as duration of antipsychotic exposure, the indication for use, medication half-life, and risk for relapse should be considered. In schizophrenia, there is no reliable indicator to differentiate the minority who will not from the majority who will relapse with drug discontinuation. However, studies in which the medication of well-stabilized patients were discontinued indicate that 75% of patients relapse within 6 to 24 months. Indefinite maintenance antipsychotic medication is generally recommended, and especially for patients who have had multiple prior episodes or two episodes within 5 years (APA [Lehman 2004]).
Monitoring Parameters
Mental status; CBC (see monitoring recommendations based on ANC); vital signs (as clinically indicated); ECG (as clinically indicated); blood pressure (baseline; repeat 3 months after antipsychotic initiation, then yearly); signs and symptoms of myocarditis and cardiomyopathy; weight, height, body mass index, waist circumference (baseline; repeat at 4, 8, and 12 weeks after initiating or changing therapy, then quarterly; consider switching to a different antipsychotic for a weight gain 5% or more of initial weight); electrolytes and liver function (annually and as clinically indicated); personal and family history of obesity, diabetes, dyslipidemia, hypertension, or cardiovascular disease (baseline; repeat annually); fasting plasma glucose level/HbA1c (baseline; repeat 3 months after starting antipsychotic, then yearly); lipid panel (baseline; repeat 3 months after initiation of antipsychotic; if low-density lipoprotein level is normal, repeat at 2- to 5-year intervals or more frequently if clinical indicated); changes in menstruation, libido, development of galactorrhea, and erectile and ejaculatory function (yearly); abnormal involuntary movements or parkinsonian signs (baseline; repeat weekly until dose stabilized for at least 2 weeks after introduction and for 2 weeks after any significant dose increase); tardive dyskinesia (every 12 months; high-risk patients every 6 months); ocular examination (yearly in patients older than 40 years; every 2 years in younger patients) (ADA 2004; Lehman 2004; Marder 2004); bowel function.
Myocarditis and cardiomyopathy: Troponin, creatinine-kinase MB, eosinophils and C-reactive protein periodically. Chest roentgenogram and cardiac imaging as appropriate. 2D-echo Doppler in patients diagnosed with cardiomyopathy, to rule out mitral valve incompetence.
US labeling:
ANC monitoring: Note: Laboratory hematology results may be presented in different units; 1 mcL equals 1 mm3.
General population: Prior to initiating treatment, obtain a baseline CBC, including the ANC; the ANC must be ≥1,500/mm3 for the general population in order to initiate treatment. During the first 6 months of treatment, monitor the ANC weekly. If the ANC remains ≥1,500/mm3, the monitoring frequency can be reduced to every 2 weeks for the next 6 months. If the ANC remains ≥1,500/mm3 for the second 6 months of continuous therapy, the ANC monitoring frequency can be reduced to once every 4 weeks.
Treatment interruption: If ANC is ≥1,500/mm3 and treatment is interrupted for <30 days, continue monitoring as before, if ≥30 days monitor as if a new patient.
Treatment discontinuation: For abrupt clozapine discontinuation for a reason unrelated to neutropenia in the general population, continuation of ANC monitoring is recommended until the ANC is ≥1,500/mm3. Additional ANC monitoring is required for any patient reporting onset of fever, defined as a temperature of 38.5°C (101.3°F) or greater, during the 2 weeks after discontinuation.
Monitor patients for psychosis and cholinergic rebound (eg, headache, nausea, vomiting, diarrhea, profuse diaphoresis).
Hematologic toxicity monitoring: Confirm all initial reports of ANC <1,500/mm3 with a repeat ANC within 24 hours.
Fever: Interrupt clozapine as a precautionary measure in any patient who develops a fever, defined as a temperature of 38.5°C (101.3°F) or greater, and obtain an ANC level. Fever is often the first sign of neutropenic infection.
Mild neutropenia (1,000 to 1,499/mm3): Continue treatment; monitor ANC 3 times weekly until ≥1,500/mm3 and then return to previous monitoring schedule.
Moderate neutropenia (500 to 999/mm3): Interrupt therapy, recommend hematology consultation, and begin daily ANC monitoring until ANC ≥1,000/mm3 and then may consider restarting therapy. Follow with 3 times weekly monitoring until ANC ≥1,500/mm3. Once ANC ≥1,500/mm3, check ANC weekly for 4 weeks and then return to previous monitoring schedule.
If fever occurs in any patient with an ANC <1,000/mm3, initiate appropriate workup and treatment for infection.
Severe neutropenia (<500/mm3): Interrupt therapy, recommend hematology consultation, and begin daily ANC monitoring until ANC ≥1,000/mm3. Follow with 3 times weekly monitoring until ANC ≥1,500/mm3. Do not rechallenge unless prescriber determines benefits outweigh risks. If rechallenged, resume treatment as a new patient once ANC ≥1,500/mm3.
Benign Ethnic Neutropenia (BEN): Prior to initiating treatment, obtain at least 2 baseline CBC levels, including the ANC; the ANC must be ≥1,000/mm3 for patients with documented Benign Ethnic Neutropenia (BEN) in order to initiate treatment. During the first 6 months of treatment, monitor the ANC weekly. If the ANC remains ≥1,000/mm3, the monitoring frequency can be reduced to every 2 weeks for the next 6 months. If the ANC remains ≥1,000/mm3 for the second 6 months of continuous therapy, the ANC monitoring frequency can be reduced to once every 4 weeks.
Treatment interruption: If ANC is ≥1,000/mm3 and treatment is interrupted for <30 days, continue monitoring as before, if ≥30 days monitor as if a new patient.
Treatment discontinuation: For abrupt clozapine discontinuation for a reason unrelated to neutropenia in BEN patients, continuation of ANC monitoring is recommended until the ANC is ≥1,000/mm3 or above their baseline. Additional ANC monitoring is required for any patient reporting onset of fever, defined as a temperature of 38.5°C (101.3°F) or greater, during the 2 weeks after discontinuation.
Monitor patients for psychosis and cholinergic rebound (eg, headache, nausea, vomiting, diarrhea, profuse diaphoresis).
Hematologic toxicity monitoring: Confirm all initial reports of ANC <1,500/mm3 with a repeat ANC within 24 hours.
Fever: Interrupt clozapine as a precautionary measure in any patient who develops a fever, defined as a temperature of 38.5°C (101.3°F) or greater, and obtain an ANC level. Fever is often the first sign of neutropenic infection.
BEN neutropenia (500 to 999/mm3): Continue therapy, recommend hematology consultation, and begin 3 times weekly ANC monitoring until ANC ≥1,000/mm3 or greater than or equal to patients known baseline. Once ANC ≥1,000/mm3 or patient’s known baseline, check ANC weekly for 4 weeks and then return to previous monitoring schedule.
If fever occurs in any patient with an ANC <1,000/mm3, initiate appropriate workup and treatment for infection.
BEN severe neutropenia (<500/mm3): Interrupt therapy, recommend hematology consultation, and begin daily ANC monitoring until ANC ≥500/mm3. Follow with 3 times weekly monitoring until ANC greater than or equal to patients baseline. Do not rechallenge unless prescriber determines benefits outweigh risks. If rechallenged, resume treatment as a new patient once ANC ≥1,000/mm3.
Hospice patients: For hospice patients (ie, terminally ill patients with an estimated life expectancy of ≤6 months), ANC monitoring may be reduced to a frequency of once every 6 months after a discussion with the patient and caregiver. Base ANC monitoring on individual treatment needs to control psychiatric symptoms and terminal illness.
Concurrent use of other drugs associated with neutropenia: If clozapine is used concurrently with an agent known to cause neutropenia (eg, some chemotherapeutic agents), consider monitoring patients more closely. Consult with treating oncologist in patients receiving concomitant chemotherapy.
Canadian labeling:
Prior to initiating treatment, obtain a baseline WBC and ANC; the WBC must be ≥3,500/mm3 and the ANC must be ≥2,000/mm3 in order to initiate treatment. Initiate treatment in an inpatient setting or an outpatient setting with medical supervision and monitor of vital signs for at least 6 to 8 hours after the first few doses. During the first 6 months (26 weeks) of treatment WBC and ANC should be obtained at baseline and at least weekly. If counts remain acceptable (WBC ≥3,500/mm3, ANC ≥2,000/mm3) during this time period, then they may be monitored every other week for the next 6 months (26 weeks). If WBC/ANC continue to remain within these acceptable limits after the second 6 months (26 weeks) of therapy, monitoring can be decreased to every 4 weeks. If clozapine is discontinued, a weekly WBC should be conducted for an additional 4 weeks or until WBC is ≥3,500/mm3 and ANC is ≥2,000/mm3.
Special populations: Patients with low WBC counts because of benign ethnic neutropenia should be given special consideration and may be started on clozapine after consultation with a hematologist. Patients with a history of bone marrow disorders should be evaluated by a hematologist prior to starting clozapine; therapy may be initiated if the benefit outweighs the risk.
Treatment interruption: Note: Only applies to patients with WBC ≥3,500/mm3 and the ANC ≥2,000/mm3. If treatment is interrupted for <3 days, continue monitoring as before. If ≥3 days of therapy interruption, resume weekly hematologic monitoring for an additional 6 weeks, then resume previous monitoring schedule. If treatment is interrupted for >4 weeks, monitor as if a new patient.
Hematologic toxicity monitoring:
Flu-like complaints or other symptoms which might suggest infection: Continue treatment; monitor WBC and ANC twice weekly.
Substantial drop in WBC or ANC (single drop or cumulative drop within 4 weeks of WBC ≥3,000/mm3, reaching a value <4,000/mm3, or ANC ≥1,500/mm3, reaching a value <2,500/mm3): Repeat WBC and ANC; if repeat values are WBC 3,000 to 3,500/mm3 and ANC <2,000/mm3, then monitor twice weekly. Continue treatment; monitor WBC and ANC twice weekly until WBC >3,500/mm3 and ANC >2,000/mm3 then return to previous monitoring schedule.
WBC 2,000 to 3,500/mm3 and/or ANC 1,500 to 2,000/mm3: Continue treatment; monitor WBC and ANC twice weekly until WBC >3,500/mm3 and ANC >2,000/mm3, then return to previous monitoring schedule.
WBC <2,000/mm3 and/or ANC <1,500/mm3: Discontinue treatment and do not rechallenge patient; continue to monitor WBC/ANC closely and monitor for signs of infection. If WBC falls <1,000/mm3 or ANC falls <500/mm3, place patient in protective isolation with close observation.
Eosinophilia (eosinophil count >3,000/mm3): Discontinue treatment and restart only after the eosinophil count is <1,000/mm3. Patients with both eosinophilia and clozapine-induced myocarditis should not be re-exposed to clozapine.
Thrombocytopenia (platelet count <50,000/mm3): Discontinue treatment.
Pregnancy
Pregnancy Risk Factor
B
Pregnancy Considerations
Clozapine crosses the placenta and can be detected in the fetal blood and amniotic fluid (Barnas 1994). Antipsychotic use during the third trimester of pregnancy has a risk for abnormal muscle movements (extrapyramidal symptoms [EPS]) and/or withdrawal symptoms in newborns following delivery. Symptoms in the newborn may include agitation, feeding disorder, hypertonia, hypotonia, respiratory distress, somnolence, and tremor; these effects may be self-limiting or require hospitalization.
The American College of Obstetricians and Gynecologists (ACOG) recommends that therapy during pregnancy be individualized; treatment with psychiatric medications during pregnancy should incorporate the clinical expertise of the mental health clinician, obstetrician, primary healthcare provider, and pediatrician. Safety data related to atypical antipsychotics during pregnancy is limited and routine use is not recommended. However, if a woman is inadvertently exposed to an atypical antipsychotic while pregnant, continuing therapy may be preferable to switching to a typical antipsychotic that the fetus has not yet been exposed to; consider risk:benefit (ACOG 2008). An increased risk of exacerbation of psychosis should be considered when discontinuing or changing treatment during pregnancy and postpartum. In general, other agents are preferred for use in pregnancy; however, clozapine may be used in women who cannot be switched to recommended antipsychotics (Larsen 2015).
Healthcare providers are encouraged to enroll women 18 to 45 years of age exposed to clozapine during pregnancy in the Atypical Antipsychotics Pregnancy Registry (1-866-961-2388 or http://www.womensmentalhealth.org/pregnancyregistry).
Patient Education
What is this drug used for?
- It is used to treat schizophrenia.
- It is used to treat problems with how one acts.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Fatigue
- Dry mouth
- Nausea
- Vomiting
- Weight gain
- Trouble sleeping
- Sweating a lot
- Drooling
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Seizures
- Infection
- High blood sugar like confusion, fatigue, increased thirst, increased hunger, passing a lot of urine, flushing, fast breathing, or breath that smells like fruit.
- Myocarditis like excessive weight gain, abnormal heartbeat, chest pain, fast heartbeat, fever, flu-like signs, shortness of breath, swelling of arms or legs, severe dizziness, or passing out.
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Severe cerebrovascular disease like change in strength on one side is greater than the other, difficulty speaking or thinking, change in balance, or vision changes.
- DVT like edema, warmth, numbness, change in color, or pain in the extremities.
- Tremors
- Difficulty moving
- Stiff muscles
- Pale skin
- Blue/gray discoloration of extremities
- Coughing up blood
- Severe loss of strength and energy
- Vision changes
- Slow heartbeat
- Dizziness
- Passing out
- Severe headache
- Severe constipation
- Neuroleptic malignant syndrome like fever, muscle cramps or stiffness, dizziness, severe headache, confusion, change in thinking, fast heartbeat, abnormal heartbeat, or sweating a lot.
- Tardive dyskinesia like unable to control body movements; tongue, face, mouth, or jaw sticking out; mouth puckering; or puffing cheeks.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.