Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral, as acetate:
Generic: 25 mg
Pharmacology
Mechanism of Action
Decreases inflammation by suppression of migration of polymorphonuclear leukocytes and reversal of increased capillary permeability
Pharmacokinetics/Pharmacodynamics
Absorption
Readily
Distribution
Distributes to muscles, liver, skin, intestines, and kidneys
Metabolism
Hepatic to active metabolite hydrocortisone (cortisol)
Excretion
Urine and feces (Czock 2005)
Time to Peak
~2 hours
Half-Life Elimination
~0.5 hours
Use: Labeled Indications
Allergic states: Control of severe or incapacitating allergic conditions intractable to adequate trials of conventional treatment of atopic dermatitis, bronchial asthma, contact dermatitis, drug hypersensitivity reactions, seasonal or perennial allergic rhinitis, and serum sickness.
Dermatologic diseases: Bullous dermatitis herpetiformis, exfoliative dermatitis, mycosis fungoides, pemphigus, severe erythema multiforme (Stevens-Johnson syndrome), severe psoriasis, severe seborrheic dermatitis.
Endocrine disorders: Congenital adrenal hyperplasia, hypercalcemia associated with cancer, nonsuppurative thyroiditis, primary or secondary adrenocortical insufficiency (hydrocortisone or cortisone is the first choice; synthetic analogs may be used in conjunction with mineralocorticoids when applicable; in infancy, mineralocorticoid supplementation is of particular importance).
Gastrointestinal diseases: To tide the patient over a critical period of the disease in regional enteritis and ulcerative colitis.
Hematologic disorders: Acquired (autoimmune) hemolytic anemia, congenital (erythroid) hypoplastic anemia, erythroblastopenia (red blood cell [RBC] anemia), immune thrombocytopenia (formerly known as idiopathic thrombocytopenic purpura) in adults, secondary thrombocytopenia in adults.
Neoplastic diseases: Palliative management of leukemias and lymphomas in adults; acute leukemia of childhood.
Ophthalmic diseases: Severe acute and chronic allergic and inflammatory processes involving the eye and its adnexa (eg, allergic conjunctivitis, allergic corneal marginal ulcers, anterior segment inflammation, chorioretinitis, diffuse posterior uveitis and choroiditis, keratitis, herpes zoster ophthalmicus, iritis and iridocyclitis, optic neuritis, sympathetic ophthalmia).
Renal diseases: To induce diuresis or remission of proteinuria in nephrotic syndrome, without uremia, of the idiopathic type or that is caused by lupus erythematosus.
Respiratory diseases: Aspiration pneumonitis, berylliosis, fulminating or disseminated pulmonary tuberculosis when used concurrently with appropriate antituberculosis chemotherapy, Loeffler syndrome not manageable by other means, symptomatic sarcoidosis.
Rheumatic disorders: Adjunctive therapy for short-term administration (to tide the patient over an acute episode or exacerbation) in acute and subacute bursitis; acute gouty arthritis; acute nonspecific tenosynovitis; ankylosing spondylitis; epicondylitis; posttraumatic osteoarthritis; psoriatic arthritis; rheumatoid arthritis (RA), including juvenile RA (select cases may require low-dose maintenance therapy); and synovitis of osteoarthritis. During an exacerbation or as maintenance therapy in select cases of acute rheumatic carditis, systemic dermatomyositis (polymyositis), and systemic lupus erythematosus.
Miscellaneous: Tuberculous meningitis with subarachnoid block or impending block when used concurrently with appropriate antituberculous chemotherapy; trichinosis with neurologic or myocardial involvement.
Contraindications
Hypersensitivity to cortisone or any component of the formulation; systemic fungal infection; administration of live virus vaccines (with immunosuppressive doses of cortisone).
Documentation of allergenic cross-reactivity for glucocorticoids is limited. However, because of similarities in chemical structure and/or pharmacologic actions, the possibility of cross-sensitivity cannot be ruled out with certainty.
Canadian labeling: Additional contraindications (not in US labeling): The Canadian product monograph describes various conditions as relative contraindications, including but not limited to, infections (fungal, mycobacterial, viral), ocular herpes simplex, acute psychoses, diverticulitis, and pregnancy; refer to the product monograph for further details.
Dosage and Administration
Dosing: Adult
Note: Dosing depends on the condition being treated and the response of the patient. Temporary supplemental doses may be warranted during times of stress (ie, trauma, surgery, severe infection). Discontinuation of therapy requires gradual withdrawal by tapering the dose.
Anti-inflammatory/immunosuppressive/endocrine disorders: Oral: Initial: 25 to 300 mg/day; adjust dose to patient response.
Physiologic replacement (off-label dose): Oral: 20 to 35 mg daily in 2 to 3 divided doses. Administer the largest dose in the morning upon awakening, followed by next dose 2 hours after lunch (two-dose regimen) or next dose at lunch, followed by smallest dose in the afternoon no later than 4 to 6 hours before bedtime (three-dose regimen) (ES [Bornstein 2016])
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Dose depends upon condition being treated and response of patient; dosage for children and adolescents should be based on disease severity and patient response rather than by rigid adherence to dosage guidelines by age, weight, or body surface area. Discontinuation of long-term therapy requires gradual withdrawal by tapering the dose.
Anti-inflammatory or immunosuppressive: Children and Adolescents: Oral: General range: 0.7 to 10 mg/kg/day; or 20 to 300 mg/m2/day in divided doses every 6 to 8 hours; usual range: 2.5 to 10 mg/kg/day (Nelson 1996; Rudolph 1996); usual adult daily dose range: 25 to 300 mg/day
Physiologic replacement: Children and Adolescents: Oral: 0.5 to 0.75 mg/kg/day or 20 to 25 mg/m2/day in divided doses every 8 hours (Keenan 1990, Kliegman 2007, Moreira 2011); usual adult daily dose range: 25 to 35 mg/day. Most physiologic replacement protocols divide the daily dose equally into 3 doses every 8 hours; however, some recommend administering a slightly higher dose in the morning to attempt to mimic the normal diurnal variation of endogenous cortisol (Shulman 2007).
Administration
Administer with food to decrease GI upset.
Dietary Considerations
May need diet with increased potassium, pyridoxine, vitamin C, vitamin D, folate, calcium, and phosphorus and decreased sodium; may be taken with food to decrease GI upset.
Storage
Store at 20°C to 25°C (68°F to 77°F). Protect from light and moisture.
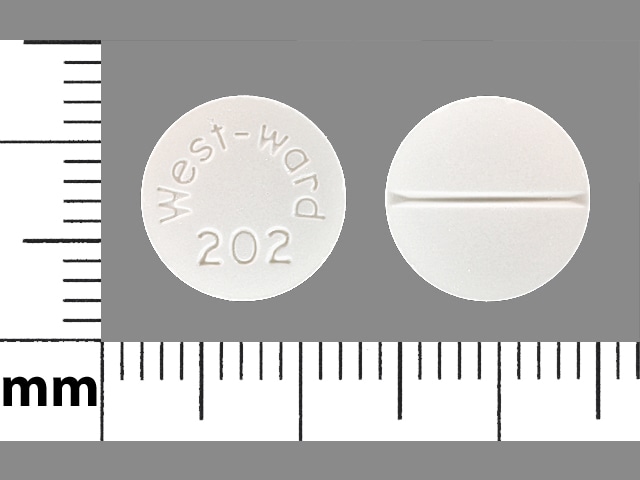
Cortisone Images
Drug Interactions
Acetylcholinesterase Inhibitors: Corticosteroids (Systemic) may enhance the adverse/toxic effect of Acetylcholinesterase Inhibitors. Increased muscular weakness may occur. Monitor therapy
Aldesleukin: Corticosteroids may diminish the antineoplastic effect of Aldesleukin. Avoid combination
Amezinium: Cortisone may enhance the stimulatory effect of Amezinium. Monitor therapy
Amphotericin B: Corticosteroids (Systemic) may enhance the hypokalemic effect of Amphotericin B. Monitor therapy
Androgens: Corticosteroids (Systemic) may enhance the fluid-retaining effect of Androgens. Monitor therapy
Antacids: May decrease the bioavailability of Corticosteroids (Oral). Management: Consider separating doses by 2 or more hours. Budesonide enteric coated tablets could dissolve prematurely if given with drugs that lower gastric acid, with unknown impact on budesonide therapeutic effects. Consider therapy modification
Antidiabetic Agents: Hyperglycemia-Associated Agents may diminish the therapeutic effect of Antidiabetic Agents. Monitor therapy
Aprepitant: May increase the serum concentration of Corticosteroids (Systemic). Management: No dose adjustment is needed for single 40 mg aprepitant doses. For other regimens, reduce oral dexamethasone or methylprednisolone doses by 50%, and IV methylprednisolone doses by 25%. Antiemetic regimens containing dexamethasone reflect this adjustment. Consider therapy modification
Axicabtagene Ciloleucel: Corticosteroids (Systemic) may diminish the therapeutic effect of Axicabtagene Ciloleucel. Management: Avoid use of corticosteroids as premedication before axicabtagene ciloleucel. Corticosteroids may, however, be required for treatment of cytokine release syndrome or neurologic toxicity. Consider therapy modification
Baricitinib: Immunosuppressants may enhance the immunosuppressive effect of Baricitinib. Management: Use of baricitinib in combination with potent immunosuppressants such as azathioprine or cyclosporine is not recommended. Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted. Consider therapy modification
BCG (Intravesical): Immunosuppressants may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
Bile Acid Sequestrants: May decrease the absorption of Corticosteroids (Oral). Monitor therapy
Calcitriol (Systemic): Corticosteroids (Systemic) may diminish the therapeutic effect of Calcitriol (Systemic). Monitor therapy
Cladribine: May enhance the immunosuppressive effect of Immunosuppressants. Avoid combination
Coccidioides immitis Skin Test: Immunosuppressants may diminish the diagnostic effect of Coccidioides immitis Skin Test. Monitor therapy
Corticorelin: Corticosteroids may diminish the therapeutic effect of Corticorelin. Specifically, the plasma ACTH response to corticorelin may be blunted by recent or current corticosteroid therapy. Monitor therapy
Cosyntropin: Cortisone may diminish the diagnostic effect of Cosyntropin. Management: Patients receiving cortisone should omit their pre-test dose on the day selected for cosyntropin testing. Consider therapy modification
CYP3A4 Inducers (Strong): May decrease the serum concentration of Corticosteroids (Systemic). Monitor therapy
CYP3A4 Inhibitors (Strong): May increase the serum concentration of Corticosteroids (Systemic). Monitor therapy
Deferasirox: Corticosteroids (Systemic) may enhance the adverse/toxic effect of Deferasirox. Specifically, the risk for GI ulceration/irritation or GI bleeding may be increased. Monitor therapy
Deferasirox: Corticosteroids may enhance the adverse/toxic effect of Deferasirox. Specifically, the risk for GI ulceration/irritation or GI bleeding may be increased. Monitor therapy
Denosumab: May enhance the adverse/toxic effect of Immunosuppressants. Specifically, the risk for serious infections may be increased. Monitor therapy
Desirudin: Corticosteroids (Systemic) may enhance the anticoagulant effect of Desirudin. More specifically, corticosteroids may increase hemorrhagic risk during desirudin treatment. Management: Discontinue treatment with systemic corticosteroids prior to desirudin initiation. If concomitant use cannot be avoided, monitor patients receiving these combinations closely for clinical and laboratory evidence of excessive anticoagulation. Consider therapy modification
Desmopressin: Corticosteroids (Systemic) may enhance the hyponatremic effect of Desmopressin. Avoid combination
DilTIAZem: May increase the serum concentration of Corticosteroids (Systemic). Monitor therapy
Echinacea: May diminish the therapeutic effect of Immunosuppressants. Consider therapy modification
Estrogen Derivatives: May increase the serum concentration of Corticosteroids (Systemic). Monitor therapy
Fexinidazole [INT]: Corticosteroids (Systemic) may enhance the arrhythmogenic effect of Fexinidazole [INT]. Avoid combination
Fingolimod: Immunosuppressants may enhance the immunosuppressive effect of Fingolimod. Management: Avoid the concomitant use of fingolimod and other immunosuppressants when possible. If combined, monitor patients closely for additive immunosuppressant effects (eg, infections). Consider therapy modification
Fosaprepitant: May increase the serum concentration of Corticosteroids (Systemic). The active metabolite aprepitant is likely responsible for this effect. Consider therapy modification
Hyaluronidase: Corticosteroids may diminish the therapeutic effect of Hyaluronidase. Management: Patients receiving corticosteroids (particularly at larger doses) may not experience the desired clinical response to standard doses of hyaluronidase. Larger doses of hyaluronidase may be required. Consider therapy modification
Indacaterol: May enhance the hypokalemic effect of Corticosteroids (Systemic). Monitor therapy
Indium 111 Capromab Pendetide: Corticosteroids (Systemic) may diminish the diagnostic effect of Indium 111 Capromab Pendetide. Avoid combination
Isoniazid: Corticosteroids (Systemic) may decrease the serum concentration of Isoniazid. Monitor therapy
Leflunomide: Immunosuppressants may enhance the adverse/toxic effect of Leflunomide. Specifically, the risk for hematologic toxicity such as pancytopenia, agranulocytosis, and/or thrombocytopenia may be increased. Management: Consider not using a leflunomide loading dose in patients receiving other immunosuppressants. Patients receiving both leflunomide and another immunosuppressant should be monitored for bone marrow suppression at least monthly. Consider therapy modification
Loop Diuretics: Corticosteroids (Systemic) may enhance the hypokalemic effect of Loop Diuretics. Monitor therapy
Macimorelin: Corticosteroids (Systemic) may diminish the diagnostic effect of Macimorelin. Avoid combination
Mifamurtide: Corticosteroids (Systemic) may diminish the therapeutic effect of Mifamurtide. Avoid combination
MiFEPRIStone: May diminish the therapeutic effect of Corticosteroids (Systemic). MiFEPRIStone may increase the serum concentration of Corticosteroids (Systemic). Management: Avoid mifepristone in patients who require long-term corticosteroid treatment of serious illnesses or conditions (e.g., for immunosuppression following transplantation). Corticosteroid effects may be reduced by mifepristone treatment. Avoid combination
Mitotane: May decrease the serum concentration of Corticosteroids (Systemic). Consider therapy modification
Natalizumab: Immunosuppressants may enhance the adverse/toxic effect of Natalizumab. Specifically, the risk of concurrent infection may be increased. Avoid combination
Neuromuscular-Blocking Agents (Nondepolarizing): May enhance the adverse neuromuscular effect of Corticosteroids (Systemic). Increased muscle weakness, possibly progressing to polyneuropathies and myopathies, may occur. Consider therapy modification
Nicorandil: Corticosteroids (Systemic) may enhance the adverse/toxic effect of Nicorandil. Gastrointestinal perforation has been reported in association with this combination. Monitor therapy
Nivolumab: Immunosuppressants may diminish the therapeutic effect of Nivolumab. Consider therapy modification
Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective): Corticosteroids (Systemic) may enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective). Monitor therapy
Nonsteroidal Anti-Inflammatory Agents (Nonselective): Corticosteroids (Systemic) may enhance the adverse/toxic effect of Nonsteroidal Anti-Inflammatory Agents (Nonselective). Monitor therapy
Ocrelizumab: May enhance the immunosuppressive effect of Immunosuppressants. Monitor therapy
Pidotimod: Immunosuppressants may diminish the therapeutic effect of Pidotimod. Monitor therapy
Pimecrolimus: May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Quinolones: Corticosteroids (Systemic) may enhance the adverse/toxic effect of Quinolones. Specifically, the risk of tendonitis and tendon rupture may be increased. Monitor therapy
Ritodrine: Corticosteroids may enhance the adverse/toxic effect of Ritodrine. Monitor therapy
Roflumilast: May enhance the immunosuppressive effect of Immunosuppressants. Consider therapy modification
Salicylates: May enhance the adverse/toxic effect of Corticosteroids (Systemic). These specifically include gastrointestinal ulceration and bleeding. Corticosteroids (Systemic) may decrease the serum concentration of Salicylates. Withdrawal of corticosteroids may result in salicylate toxicity. Monitor therapy
Sargramostim: Corticosteroids (Systemic) may enhance the therapeutic effect of Sargramostim. Specifically, corticosteroids may enhance the myeloproliferative effects of sargramostim. Monitor therapy
Siponimod: Immunosuppressants may enhance the immunosuppressive effect of Siponimod. Monitor therapy
Sipuleucel-T: Immunosuppressants may diminish the therapeutic effect of Sipuleucel-T. Management: Evaluate patients to see if it is medically appropriate to reduce or discontinue therapy with immunosuppressants prior to initiating sipuleucel-T therapy. Consider therapy modification
Somatropin: Cortisone may diminish the therapeutic effect of Somatropin. Somatropin may diminish the therapeutic effect of Cortisone. Growth hormone may reduce the conversion of cortisone to the active cortisol metabolite. Monitor therapy
Tacrolimus (Systemic): Corticosteroids (Systemic) may decrease the serum concentration of Tacrolimus (Systemic). Conversely, when discontinuing corticosteroid therapy, tacrolimus concentrations may increase. Monitor therapy
Tacrolimus (Topical): May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Tertomotide: Immunosuppressants may diminish the therapeutic effect of Tertomotide. Monitor therapy
Tesamorelin: May decrease serum concentrations of the active metabolite(s) of Cortisone. Consider therapy modification
Thiazide and Thiazide-Like Diuretics: Corticosteroids (Systemic) may enhance the hypokalemic effect of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Tisagenlecleucel: Corticosteroids (Systemic) may diminish the therapeutic effect of Tisagenlecleucel. Management: Avoid use of corticosteroids as premedication or at any time during treatment with tisagenlecleucel, except in the case of life-threatening emergency (such as resistant cytokine release syndrome). Consider therapy modification
Tofacitinib: Immunosuppressants may enhance the immunosuppressive effect of Tofacitinib. Management: Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted, and this warning seems particularly focused on more potent immunosuppressants. Consider therapy modification
Trastuzumab: May enhance the neutropenic effect of Immunosuppressants. Monitor therapy
Upadacitinib: Immunosuppressants may enhance the immunosuppressive effect of Upadacitinib. Avoid combination
Urea Cycle Disorder Agents: Corticosteroids (Systemic) may diminish the therapeutic effect of Urea Cycle Disorder Agents. More specifically, Corticosteroids (Systemic) may increase protein catabolism and plasma ammonia concentrations, thereby increasing the doses of Urea Cycle Disorder Agents needed to maintain these concentrations in the target range. Monitor therapy
Vaccines (Inactivated): Immunosuppressants may diminish the therapeutic effect of Vaccines (Inactivated). Management: Vaccine efficacy may be reduced. Complete all age-appropriate vaccinations at least 2 weeks prior to starting an immunosuppressant. If vaccinated during immunosuppressant therapy, revaccinate at least 3 months after immunosuppressant discontinuation. Consider therapy modification
Vaccines (Live): Corticosteroids (Systemic) may enhance the adverse/toxic effect of Vaccines (Live). Corticosteroids (Systemic) may diminish the therapeutic effect of Vaccines (Live). Management: Doses equivalent to less than 2 mg/kg or 20 mg per day of prednisone administered for less than 2 weeks are not considered sufficiently immunosuppressive to create vaccine safety concerns. Higher doses and longer durations should be avoided. Consider therapy modification
Warfarin: Corticosteroids (Systemic) may enhance the anticoagulant effect of Warfarin. Monitor therapy
Test Interactions
May suppress the wheal and flare reactions to skin test antigens
Adverse Reactions
Frequency not defined.
>10%:
Central nervous system: Insomnia, nervousness
Gastrointestinal: Dyspepsia, increased appetite
1% to 10%:
Endocrine & metabolic: Diabetes mellitus, hirsutism
Neuromuscular & skeletal: Arthralgia
Ophthalmic: Cataract, glaucoma
Respiratory: Epistaxis
<1%, postmarketing, and/or case reports: Abdominal distention, acne vulgaris, alkalosis, amenorrhea, amyotrophy, bone fracture, bruise, Cushing's syndrome, decreased glucose tolerance, delirium, edema, emotional lability, euphoria, fluid retention, growth suppression, hallucination, headache, HPA-axis suppression, hyperglycemia, hyperpigmentation, hypersensitivity reaction, hypertension, hypokalemia, myalgia, nausea, osteoporosis, pancreatitis, peptic ulcer, pseudotumor cerebri, psychosis, seizure, skin atrophy, sodium retention, ulcerative esophagitis, vertigo, vomiting
Warnings/Precautions
Concerns related to adverse effects:
- Adrenal suppression: May cause hypercortisolism or suppression of hypothalamic-pituitary-adrenal (HPA) axis, particularly in younger children or in patients receiving high doses for prolonged periods. HPA axis suppression may lead to adrenal crisis. Withdrawal and discontinuation of a corticosteroid should be done slowly and carefully. Particular care is required when patients are transferred from systemic corticosteroids to inhaled products due to possible adrenal insufficiency or withdrawal from steroids, including an increase in allergic symptoms. Adult patients receiving >20 mg per day of prednisone (or equivalent) may be most susceptible. Fatalities have occurred due to adrenal insufficiency in asthmatic patients during and after transfer from systemic corticosteroids to aerosol steroids; aerosol steroids do not provide the systemic steroid needed to treat patients having trauma, surgery, or infections.
- Anaphylactoid reactions: Rare cases of anaphylactoid reactions have been observed in patients receiving corticosteroids.
- Immunosuppression: Prolonged use of corticosteroids may also increase the incidence of secondary infection, mask acute infection (including fungal infections), prolong or exacerbate viral infections, or limit response to inactivated vaccines. Exposure to chickenpox or measles should be avoided. Corticosteroids should not be used for cerebral malaria or viral hepatitis. Close observation is required in patients with latent tuberculosis (TB) and/or TB reactivity; restrict use in active TB (only fulminating or disseminated TB in conjunction with antituberculosis treatment). Amebiasis should be ruled out in any patient with recent travel to tropical climates or unexplained diarrhea prior to initiation of corticosteroids.
- Kaposi sarcoma: Prolonged treatment with corticosteroids has been associated with the development of Kaposi sarcoma (case reports); if noted, discontinuation of therapy should be considered (Goedert 2002).
- Myopathy: Acute myopathy has been reported with high-dose corticosteroids, usually in patients with neuromuscular transmission disorders; may involve ocular and/or respiratory muscles; monitor creatine kinase; recovery may be delayed.
- Psychiatric disturbances: Corticosteroid use may cause psychiatric disturbances, including severe depression, euphoria, insomnia, mood swings, personality changes, to frank psychotic manifestations. Preexisting psychiatric conditions may be exacerbated by corticosteroid use.
Disease-related concerns:
- Cardiovascular disease: Use with caution in patients with heart failure and/or hypertension; use has been associated with electrolyte disturbances, fluid retention, and hypertension. Use with caution in patients with a recent history of myocardial infarction (MI); left ventricular free wall rupture has been reported after the use of corticosteroids.
- Diabetes: Use with caution in patients with diabetes mellitus; may alter glucose production/regulation leading to hyperglycemia.
- Gastrointestinal disease: Use with caution in patients with GI diseases (diverticulitis, fresh intestinal anastomoses, active or latent peptic ulcer, ulcerative colitis [nonspecific) due to perforation risk.
- Head injury: Increased mortality was observed in patients receiving high-dose IV methylprednisolone; high-dose corticosteroids should not be used for the management of head injury.
- Hepatic impairment: Use with caution in patients with hepatic impairment, including cirrhosis; long-term use has been associated with fluid retention.
- Myasthenia gravis: Use with caution in patients with myasthenia gravis; exacerbation of symptoms has occurred especially during initial treatment with corticosteroids.
- Ocular disease: Use with caution in patients with cataracts and/or glaucoma; increased intraocular pressure, open-angle glaucoma, and cataracts have occurred with prolonged use. Use with caution in patients with a history of ocular herpes simplex; corneal perforation has occurred; do not use in active ocular herpes simplex. Consider routine eye exams in chronic users.
- Osteoporosis: Use with caution in patients with osteoporosis; high doses and/or long-term use of corticosteroids have been associated with increased bone loss and osteoporotic fractures.
- Renal impairment: Use with caution in patients with renal impairment; fluid retention may occur.
- Seizure disorders: Use with caution in patients with a history of seizure disorder; seizures have been reported with adrenal crisis.
- Thyroid disease: Changes in thyroid status may necessitate dosage adjustments; metabolic clearance of corticosteroids increases in hyperthyroid patients and decreases in hypothyroid ones.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Elderly: Because of the risk of adverse effects, systemic corticosteroids should be used cautiously in the elderly in the smallest possible effective dose for the shortest duration.
- Pediatric: May affect growth velocity; growth and development should be routinely monitored in pediatric patients.
Other warnings/precautions:
- Discontinuation of therapy: Withdraw therapy with gradual tapering of dose.
Monitoring Parameters
Blood pressure; glucose (in diabetics); bone mineral density; growth in children; eye exams (with prolonged use); signs and symptoms of infection; signs and symptoms of hypercortisolism or adrenal suppression.
Pregnancy
Pregnancy Considerations
Cortisone crosses the placenta (Migeon 1957). Some studies have shown an association between first trimester systemic corticosteroid use and oral clefts (Park-Wyllie 2000; Pradat 2003). Systemic corticosteroids may also influence fetal growth (decreased birth weight); however, information is conflicting (Lunghi 2010). Hypoadrenalism may occur in newborns following maternal use of corticosteroids in pregnancy (monitor). When systemic corticosteroids are needed in pregnancy, it is generally recommended to use the lowest effective dose for the shortest duration of time, avoiding high doses during the first trimester (Leachman 2006; Lunghi 2010; Makol 2011; Østensen 2009). Cortisone may be used (alternative agent) to treat primary adrenal insufficiency (PAI) in pregnant women. Pregnant women with PAI should be monitored at least once each trimester (Bornstein 2016).
Patient Education
- Discuss specific use of drug and side effects with patient as it relates to treatment. (HCAHPS: During this hospital stay, were you given any medicine that you had not taken before? Before giving you any new medicine, how often did hospital staff tell you what the medicine was for? How often did hospital staff describe possible side effects in a way you could understand?)
- Patient may experience nausea, vomiting, trouble sleeping, or agitation. Have patient report immediately to prescriber signs of infection, signs of low potassium (muscle pain or weakness, muscle cramps, or an abnormal heartbeat); signs of high blood sugar (confusion, fatigue, increased thirst, increased hunger, passing a lot of urine, flushing, fast breathing, or breath that smells like fruit); signs of pancreatitis (severe abdominal pain, severe back pain, severe nausea, or vomiting); signs of adrenal gland problems (severe nausea, vomiting, severe dizziness, passing out, muscle weakness, severe fatigue, mood changes, lack of appetite, or weight loss); signs of Cushings disease (weight gain in upper back or abdomen; moon face; severe headache; or slow healing); signs of skin changes (acne, stretch marks, slow healing, or hair growth); signs of DVT (edema, warmth, numbness, change in color, or pain in the extremities); severe loss of strength and energy; irritability; tremors; fast heartbeat; confusion; sweating a lot; dizziness; passing out; shortness of breath; excessive weight gain; swelling of arms or legs; severe headache; chest pain; menstrual changes; bone pain; joint pain; vision changes; mood changes; behavioral changes; depression; seizures; bruising; bleeding; severe abdominal pain; black, tarry, or bloody stools; or vomiting blood (HCAHPS).
- Educate patient about signs of a significant reaction (eg, wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat). Note: This is not a comprehensive list of all side effects. Patient should consult prescriber for additional questions.
Intended Use and Disclaimer: Should not be printed and given to patients. This information is intended to serve as a concise initial reference for health care professionals to use when discussing medications with a patient. You must ultimately rely on your own discretion, experience, and judgment in diagnosing, treating, and advising patients.