Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Capsule, Oral, as hydrochloride:
Bentyl: 10 mg [DSC] [contains brilliant blue fcf (fd&c blue #1), corn starch, fd&c red #40]
Generic: 10 mg
Solution, Intramuscular, as hydrochloride:
Bentyl: 10 mg/mL (2 mL) [pyrogen free]
Generic: 10 mg/mL (2 mL)
Solution, Intramuscular, as hydrochloride [preservative free]:
Generic: 10 mg/mL (2 mL)
Solution, Oral, as hydrochloride:
Generic: 10 mg/5 mL (473 mL)
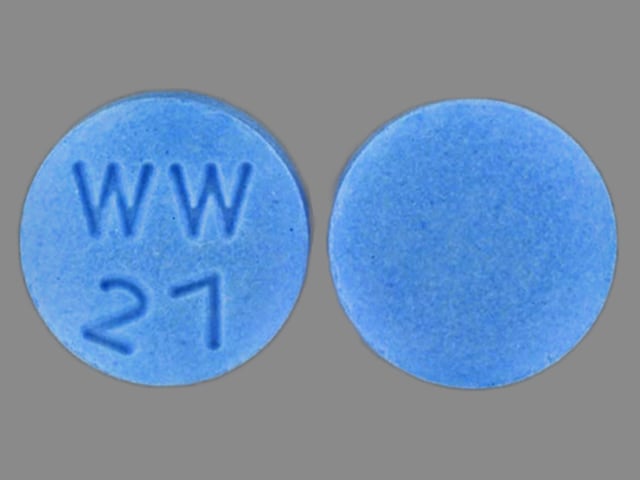
Tablet, Oral, as hydrochloride:
Bentyl: 20 mg [DSC] [contains brilliant blue fcf (fd&c blue #1), corn starch]
Generic: 20 mg
Pharmacology
Mechanism of Action
Blocks the action of acetylcholine at parasympathetic sites in smooth muscle, secretory glands and the CNS
Pharmacokinetics/Pharmacodynamics
Absorption
Oral: Rapid and well absorbed
Distribution
Vd: 3.65 L/kg
Metabolism
Extensive
Excretion
Urine (80%, small amounts as unchanged drug); feces (8%)
Onset of Action
1 to 2 hours
Time to Peak
Oral: 60 to 90 minutes
Duration of Action
Up to 4 hours
Half-Life Elimination
Initial phase: ~1.8 hours; Terminal phase: Undetermined, but somewhat longer than the initial phase
Use: Labeled Indications
Irritable bowel syndrome: Treatment of irritable bowel syndrome-associated abdominal pain.
Contraindications
Obstructive diseases of the GI tract; severe ulcerative colitis; reflux esophagitis; unstable cardiovascular status in acute hemorrhage; obstructive uropathy; glaucoma; myasthenia gravis; breastfeeding women; infants <6 months of age
Canadian labeling: Additional contraindications (not in US labeling): Hypersensitivity to dicyclomine or any component of the formulation
Dosage and Administration
Dosing: Adult
Irritable bowel syndrome-associated abdominal pain: Oral: Initial: 20 mg up to 4 times daily; some experts recommend only administering as needed or in anticipation of a stressor that triggers abdominal pain (Wald 2019); intended for short-term use; scheduled dosing for >2 weeks has not been studied (Ford 2014; manufacturer's labeling)
Note: According to the manufacturer's labeling, may titrate dose after 1 week, based on response and tolerability, up to 40 mg 4 times daily; however, some experts do not recommend doses >20 mg due to anticholinergic adverse effects (Wald 2019).
Dosing: Geriatric
Avoid use (Beers Criteria [AGS 2019]).
Dosing: Pediatric
Gastrointestinal motility disorders/irritable bowel: Limited data available (Bentylol Canadian prescribing information 2012):
Infants ≥6 months and Children <2 years: Oral: 5 to 10 mg 3 to 4 times daily administered 15 minutes before feeding
Children ≥2 years Oral: 10 mg 3 to 4 times daily
Adolescents: Oral: 10 to 20 mg 3 to 4 times daily. If efficacy not achieved in 2 weeks, therapy should be discontinued.
Administration
Oral: May be taken with or without food.
Injection: There is an injectable formulation for IM administration available intended for short-term use (<2 days) in patients unable to take oral medications; however, pain and necrosis have been reported in a case report following IM administration (Greenky 2017), and most experts would avoid use (Wald 2019). Do not administer IV (intravenous administration may result in thrombosis or thrombophlebitis).
Storage
Capsule, tablet: Store at room temperature, preferably below 30°C (86°F). Protect tablet from direct sunlight.
Oral solution: Store at 20°C to 25°C (68°F to 77°F); protect from excessive heat.
Solution for injection: Store at room temperature, preferably below 30°C (86°F); protect from freezing.
Dicyclomine Images
Drug Interactions
Acetylcholinesterase Inhibitors: May diminish the therapeutic effect of Anticholinergic Agents. Anticholinergic Agents may diminish the therapeutic effect of Acetylcholinesterase Inhibitors. Monitor therapy
Aclidinium: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Amantadine: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Anticholinergic Agents: May enhance the adverse/toxic effect of other Anticholinergic Agents. Monitor therapy
Botulinum Toxin-Containing Products: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Cannabinoid-Containing Products: Anticholinergic Agents may enhance the tachycardic effect of Cannabinoid-Containing Products. Exceptions: Cannabidiol. Monitor therapy
Chloral Betaine: May enhance the adverse/toxic effect of Anticholinergic Agents. Monitor therapy
Cimetropium: Anticholinergic Agents may enhance the anticholinergic effect of Cimetropium. Avoid combination
Eluxadoline: Anticholinergic Agents may enhance the constipating effect of Eluxadoline. Avoid combination
Gastrointestinal Agents (Prokinetic): Anticholinergic Agents may diminish the therapeutic effect of Gastrointestinal Agents (Prokinetic). Monitor therapy
Glucagon: Anticholinergic Agents may enhance the adverse/toxic effect of Glucagon. Specifically, the risk of gastrointestinal adverse effects may be increased. Monitor therapy
Glycopyrrolate (Oral Inhalation): Anticholinergic Agents may enhance the anticholinergic effect of Glycopyrrolate (Oral Inhalation). Avoid combination
Glycopyrronium (Topical): May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Ipratropium (Oral Inhalation): May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Itopride: Anticholinergic Agents may diminish the therapeutic effect of Itopride. Monitor therapy
Levosulpiride: Anticholinergic Agents may diminish the therapeutic effect of Levosulpiride. Avoid combination
Mianserin: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Mirabegron: Anticholinergic Agents may enhance the adverse/toxic effect of Mirabegron. Monitor therapy
Nitroglycerin: Anticholinergic Agents may decrease the absorption of Nitroglycerin. Specifically, anticholinergic agents may decrease the dissolution of sublingual nitroglycerin tablets, possibly impairing or slowing nitroglycerin absorption. Monitor therapy
Opioid Agonists: Anticholinergic Agents may enhance the adverse/toxic effect of Opioid Agonists. Specifically, the risk for constipation and urinary retention may be increased with this combination. Monitor therapy
Oxatomide: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Potassium Chloride: Anticholinergic Agents may enhance the ulcerogenic effect of Potassium Chloride. Management: Patients on drugs with substantial anticholinergic effects should avoid using any solid oral dosage form of potassium chloride. Avoid combination
Potassium Citrate: Anticholinergic Agents may enhance the ulcerogenic effect of Potassium Citrate. Avoid combination
Pramlintide: May enhance the anticholinergic effect of Anticholinergic Agents. These effects are specific to the GI tract. Consider therapy modification
Ramosetron: Anticholinergic Agents may enhance the constipating effect of Ramosetron. Monitor therapy
Revefenacin: Anticholinergic Agents may enhance the anticholinergic effect of Revefenacin. Avoid combination
Secretin: Anticholinergic Agents may diminish the therapeutic effect of Secretin. Management: Avoid concomitant use of anticholinergic agents and secretin. Discontinue anticholinergic agents at least 5 half-lives prior to administration of secretin. Consider therapy modification
Sincalide: Drugs that Affect Gallbladder Function may diminish the therapeutic effect of Sincalide. Management: Consider discontinuing drugs that may affect gallbladder motility prior to the use of sincalide to stimulate gallbladder contraction. Consider therapy modification
Thiazide and Thiazide-Like Diuretics: Anticholinergic Agents may increase the serum concentration of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Tiotropium: Anticholinergic Agents may enhance the anticholinergic effect of Tiotropium. Avoid combination
Topiramate: Anticholinergic Agents may enhance the adverse/toxic effect of Topiramate. Monitor therapy
Umeclidinium: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Adverse Reactions
>10%:
Central nervous system: Dizziness (40%)
Gastrointestinal: Xerostomia (33%), nausea (14%)
Ophthalmic: Blurred vision (27%)
1% to 10%:
Central nervous system: Drowsiness (9%), nervousness (6%)
Neuromuscular & skeletal: Weakness (7%)
Postmarketing and/or case reports: Abdominal distention, abdominal pain, anaphylactic shock, angioedema, confusion, constipation, cycloplegia, decreased lactation, delirium, dermatitis (allergic), dyspepsia, dyspnea, erythema, facial edema, fatigue, hallucination, headache, hypersensitivity, insomnia, malaise, mydriasis, nasal congestion, palpitations, skin rash, syncope, tachyarrhythmia, vomiting
Warnings/Precautions
Concerns related to adverse effects:
- CNS effects: May cause drowsiness and/or blurred vision, which may impair physical or mental abilities; patients must be cautioned about performing tasks which require mental alertness (eg, operating machinery or driving).
- Diarrhea: May be a sign of incomplete intestinal obstruction, treatment should be discontinued if this occurs.
- Heat prostration: May occur in the presence of increased environmental temperature; use caution in hot weather and/or exercise.
- Psychosis/delirium: Has been reported in patients with an extreme sensitivity to anticholinergic effects or at excessive dosages, such as the elderly or patients with mental illness.
Disease-related concerns:
- Cardiovascular disease: Use with caution in patients with coronary artery disease, tachyarrhythmias, heart failure, or hypertension; evaluate tachycardia prior to administration.
- Hepatic impairment: Use with caution in patients with hepatic impairment.
- Hyperthyroidism: Use with caution in patients with hyperthyroidism.
- Neuropathy: Use with caution in patients with autonomic neuropathy.
- Prostatic hyperplasia: Use with caution in patients with prostatic hyperplasia (known or suspected).
- Renal impairment: Use with caution in patients with renal impairment.
- Salmonella dysentery: Do not use anticholinergic agents in patients with salmonella dysentery; toxic dilatation of intestine and intestinal perforation may occur.
- Ulcerative colitis: Use with caution in patients with mild-moderate ulcerative colitis. Use is contraindicated in patients with severe ulcerative colitis.
Concurrent drug therapy issues:
- Sedatives: Effects may be potentiated when used with other sedative drugs or ethanol.
Special populations:
- Pediatric: Serious respiratory reactions, central nervous symptoms, and deaths have been reported following administration to infants; use in infants <6 months of age is contraindicated).
Other warnings/precautions:
- Appropriate administration: Injectable formulation is for IM administration only; inadvertent IV administration may cause thrombosis/thrombophlebitis and injection site reactions (eg, pain, edema, skin color change, reflex sympathetic dystrophy).
Monitoring Parameters
Anticholinergic effects, urinary output, GI symptoms
Pregnancy
Pregnancy Considerations
In epidemiologic studies, birth defects were not observed following maternal doses up to 40 mg daily throughout the first trimester; information has not been located when used in pregnant women at recommended doses (80 to 160 mg daily). Agents other than dicyclomine may be preferred for the treatment of irritable bowel syndrome in pregnant women (Enck 2016).
Patient Education
What is this drug used for?
- It is used to treat GI (gastrointestinal) spasms.
- It is used to treat irritable bowel syndrome.
Frequently reported side effects of this drug
- Fatigue
- Blurred vision
- Nausea
- Anxiety
- Loss of strength and energy
- Dry mouth
- Increased thirst
- Flushing
- Constipation
- Trouble sleeping
- Dry skin
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Lack of sweat
- Severe dizziness
- Passing out
- Confusion
- Trouble swallowing
- Trouble speaking
- Change in balance
- Vision changes
- Enlarged pupils
- Sensitivity to light
- Trouble urinating
- Diarrhea
- Slow heartbeat
- Fast heartbeat
- Abnormal heartbeat
- Sensing things that seem real but are not
- Trouble with memory
- Mood changes
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.