Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Capsule Extended Release 12 Hour, Oral, as hydrochloride:
Generic: 60 mg, 90 mg, 120 mg
Capsule Extended Release 24 Hour, Oral, as hydrochloride:
Cardizem CD: 120 mg, 180 mg, 240 mg, 300 mg, 360 mg [contains brilliant blue fcf (fd&c blue #1)]
Cartia XT: 120 mg, 180 mg, 240 mg
Cartia XT: 300 mg [contains brilliant blue fcf (fd&c blue #1), fd&c blue #1 aluminum lake, fd&c blue #2 aluminum lake, fd&c red #40, fd&c red #40 aluminum lake, fd&c yellow #10 (quinoline yellow), fd&c yellow #10 aluminum lake]
Dilt-XR: 120 mg, 180 mg, 240 mg [contains brilliant blue fcf (fd&c blue #1), fd&c red #40, fd&c yellow #10 (quinoline yellow)]
dilTIAZem CD: 120 mg [DSC]
dilTIAZem CD: 180 mg [DSC] [contains brilliant blue fcf (fd&c blue #1), fd&c yellow #10 (quinoline yellow)]
dilTIAZem CD: 240 mg [DSC] [contains fd&c yellow #10 (quinoline yellow)]
Taztia XT: 120 mg [contains brilliant blue fcf (fd&c blue #1), fd&c blue #1 aluminum lake, fd&c blue #2 aluminum lake, fd&c red #40, fd&c red #40 aluminum lake, fd&c yellow #10 aluminum lake]
Taztia XT: 180 mg [contains brilliant blue fcf (fd&c blue #1), fd&c blue #1 aluminum lake, fd&c blue #2 aluminum lake, fd&c red #40 aluminum lake, fd&c yellow #10 (quinoline yellow), fd&c yellow #10 aluminum lake, fd&c yellow #6 (sunset yellow)]
Taztia XT: 240 mg [contains brilliant blue fcf (fd&c blue #1), fd&c blue #1 aluminum lake, fd&c blue #2 aluminum lake, fd&c red #40, fd&c red #40 aluminum lake, fd&c yellow #10 aluminum lake]
Taztia XT: 300 mg [contains brilliant blue fcf (fd&c blue #1), corn starch, fd&c blue #1 aluminum lake, fd&c blue #2 aluminum lake, fd&c red #40, fd&c red #40 aluminum lake, fd&c yellow #10 (quinoline yellow), fd&c yellow #10 aluminum lake, fd&c yellow #6 (sunset yellow)]
Taztia XT: 360 mg [contains brilliant blue fcf (fd&c blue #1), fd&c blue #1 aluminum lake, fd&c blue #2 aluminum lake, fd&c red #40 aluminum lake, fd&c yellow #10 aluminum lake]
Tiadylt ER: 120 mg [contains brilliant blue fcf (fd&c blue #1), fd&c red #40]
Tiadylt ER: 180 mg [contains brilliant blue fcf (fd&c blue #1)]
Tiadylt ER: 240 mg, 300 mg [contains brilliant blue fcf (fd&c blue #1), fd&c red #40]
Tiadylt ER: 360 mg [contains brilliant blue fcf (fd&c blue #1)]
Tiadylt ER: 420 mg
Tiazac: 120 mg, 180 mg, 240 mg, 300 mg, 360 mg, 420 mg [contains brilliant blue fcf (fd&c blue #1), fd&c red #40]
Generic: 120 mg, 180 mg, 240 mg, 300 mg, 360 mg, 420 mg
Solution, Intravenous, as hydrochloride:
Generic: 25 mg/5 mL (5 mL); 50 mg/10 mL (10 mL); 125 mg/25 mL (25 mL)
Solution, Intravenous, as hydrochloride [preservative free]:
Generic: 25 mg/5 mL (5 mL)
Solution Reconstituted, Intravenous, as hydrochloride:
Generic: 100 mg (1 ea)
Tablet, Oral, as hydrochloride:
Cardizem: 30 mg [contains fd&c blue #1 aluminum lake, fd&c yellow #10 aluminum lake]
Cardizem: 60 mg [scored; contains fd&c blue #1 aluminum lake, fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake, methylparaben]
Cardizem: 120 mg [scored; contains fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake, methylparaben]
Generic: 30 mg, 60 mg, 90 mg, 120 mg
Tablet Extended Release 24 Hour, Oral, as hydrochloride:
Cardizem LA: 120 mg, 180 mg, 240 mg, 300 mg, 360 mg, 420 mg
Matzim LA: 180 mg, 240 mg, 300 mg, 360 mg, 420 mg
Generic: 180 mg, 240 mg, 300 mg, 360 mg, 420 mg
Pharmacology
Mechanism of Action
Inhibits calcium ion from entering the “slow channels” or select voltage-sensitive areas of vascular smooth muscle and myocardium during depolarization; produces relaxation of coronary vascular smooth muscle and coronary vasodilation; increases myocardial oxygen delivery in patients with vasospastic angina.
Pharmacokinetics/Pharmacodynamics
Absorption
Immediate release tablet: ~98%; Extended release capsule: ~93% to >95%
Distribution
Vd: 3 to 13 L/kg
Metabolism
Hepatic (extensive first-pass effect) via CYP-450 and conjugation; forms metabolites N-monodesmethyldiltiazem, desacetyldiltiazem, desacetyl-Nmonodesmethyldiltiazem, desacetyl-O-desmethyldiltiazem, and desacetyl-N, O-desmethyldiltiazem following single IV injection, plasma concentrations of N-monodesmethyldiltiazem and desacetyldiltiazem are typically undetectable; however, these metabolites accumulate to detectable concentrations following 24-hour constant rate infusion.
Excretion
Urine (2% to 4% as unchanged drug); feces
Onset of Action
Oral: Immediate release tablet: 30 to 60 minutes; IV: Bolus: 3 minutes
Time to Peak
Serum: Immediate release tablet: 2 to 4 hours; Extended release tablet: 11 to 18 hours; Extended release capsule: 10 to 14 hours
Duration of Action
IV: Bolus: 1 to 3 hours; Continuous infusion (after discontinuation): 0.5 to 10 hours
Half-Life Elimination
Immediate release tablet: 3 to 4.5 hours; Extended release tablet: 6 to 9 hours; Extended release capsules: 4 to 9.5 hours; IV: single dose: ~3.4 hours; continuous infusion: 4 to 5 hours
Protein Binding
70% to 80%
Use in Specific Populations
Special Populations: Hepatic Function Impairment
Bioavailability is increased, and half-life is prolonged.
Use: Labeled Indications
Oral: Hypertension, chronic stable angina, vasospastic angina
Injection: Atrial fibrillation or atrial flutter for acute ventricular rate control, conversion of supraventricular tachycardia
Use: Off Label
Atrial fibrillation or atrial flutter, chronic ventricular rate controlyes
Based on the 2014 American Heart Association/American College of Cardiology/Heart Rhythm Society (AHA/ACC/HRS) guideline for the management of patients with atrial fibrillation (AF), the use of nondihydropyridine calcium channel blockers, including diltiazem, for ventricular rate control in patients with paroxysmal, persistent, or permanent AF is effective and recommended for this condition.
Chest pain associated with cocaine ingestion, with or without evidence of acute coronary syndromec
Clinical experience suggests that nondihydropyridine calcium channel blockers (eg, diltiazem) may be useful as adjunctive therapy in patients with recurrent symptoms of ischemia despite optimal therapy with nitroglycerin Morgan 2019.
Hypertrophic cardiomyopathyyes
Based on the 2011 American College of Cardiology Foundation/American Heart Association (ACCF/AHA) guideline for the diagnosis and treatment of hypertrophic cardiomyopathy, diltiazem is an effective and recommended alternative agent for the treatment of symptoms (eg, angina, dyspnea) in patients with obstructive or nonobstructive hypertrophic cardiomyopathy who do not tolerate or are unresponsive to beta-blockers or verapamil.
Idiopathic ventricular tachycardiacyes
Data from a small, prospective observational study showed that diltiazem can suppress ventricular tachycardia (VT) in patients with idiopathic VT Gill 1992.
Based on the 2017 American Heart Association/American College of Cardiology/Heart Rhythm Society (AHA/ACC/HRS) guideline for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death, diltiazem is an effective and recommended therapy for termination and prevention of recurrence of idiopathic VT originating from the right ventricular outflow tract or related to interfascicular reentry. Note: Calcium channel blockers should not be given to patients with VT and heart failure with a reduced ejection fraction. Calcium channel blockers are not effective for all forms of VT and may be harmful in some cases. These agents should not be given to patients with VT of unknown origin.
Nonsustained ventricular tachycardia or ventricular premature beats, symptomaticcyes
Based on the 2017 American Heart Association/American College of Cardiology/Heart Rhythm Society (AHA/ACC/HRS) guideline for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death and recommendations from other experts Zimetbaum 2019, diltiazem may be used to treat symptoms (eg, palpitations) associated with nonsustained ventricular tachycardia or ventricular premature beats.
Pulmonary arterial hypertension (group 1)cyes
Data from a limited number of patients from retrospective, observational studies suggest that diltiazem may be beneficial for the treatment of group 1 pulmonary arterial hypertension in patients with a positive vasoreactivity test Montani 2010, Sitbon 2005.
Based on the 2019 American College of Chest Physicians (ACCP) guideline on pharmacologic therapy for pulmonary arterial hypertension, 2009 American College of Cardiology/American Heart Association (ACC/AHA) consensus document on pulmonary hypertension, and 2015 European Society of Cardiology/European Respiratory Society (ESC/ERS) guidelines for the diagnosis and treatment of pulmonary hypertension, the use of diltiazem is an effective and recommended treatment option for patients with group 1 pulmonary hypertension who have a positive vasoreactivity test.
Supraventricular tachycardia (eg, atrioventricular nodal reentrant tachycardia, atrioventricular reentrant tachycardia, focal atrial tachycardia, multifocal atrial tachycardia)yes
Based on the 2015 American College of Cardiology/American Heart Association/Heart Rhythm Society (ACC/AHA/HRS) guideline for the management of patients with supraventricular arrhythmias, diltiazem is effective and recommended for the management of hemodynamically stable patients with symptomatic supraventricular tachycardia without preexcitation. Diltiazem may be used for acute management when vagal maneuvers or adenosine are ineffective and/or for chronic maintenance therapy.
Contraindications
Oral: Hypersensitivity to diltiazem or any component of the formulation; sick sinus syndrome (except in patients with a functioning artificial pacemaker); second- or third-degree AV block (except in patients with a functioning artificial pacemaker); hypotension (systolic <90 mm Hg); acute MI and pulmonary congestion
Intravenous (IV): Hypersensitivity to diltiazem or any component of the formulation; sick sinus syndrome (except in patients with a functioning artificial pacemaker); second- or third-degree AV block (except in patients with a functioning artificial pacemaker); severe hypotension; cardiogenic shock; administration concomitantly or within a few hours of the administration of IV beta-blockers; atrial fibrillation or flutter associated with accessory bypass tract (eg, Wolff-Parkinson-White syndrome, short PR syndrome); ventricular tachycardia (with wide-complex tachycardia [QRS ≥0.12 seconds], must determine whether origin is supraventricular or ventricular)
Canadian labeling: Additional contraindications (not in US labeling): Pregnancy; use in women of childbearing potential; concurrent use with IV dantrolene; concurrent use with ivabradine; severe bradycardia (<40 beats per minute).
Dosage and Administration
Dosing: Adult
Notes: Safety: Due to its negative inotropic and chronotropic effects, use is generally avoided in patients taking a beta-blocker or who have heart failure with reduced ejection fraction. Unless a functioning pacemaker has been placed, avoid use in patients with sinus node dysfunction, or second- or third-degree atrioventricular block. Dosage forms: Available preparations include: Oral immediate-release (usually dosed 4 times daily), 12-hour extended-release (ER) (dosed 2 times daily), and 24-hour extended-release (dosed once daily) formulations and an IV injection. For conversion between oral immediate-release, 12- and 24-hour extended-release, and parenteral formulations, refer to conversion section below.
Angina pectoris:
Chronic stable angina (alternative agent): Note: A beta-blocker is the preferred initial therapy; if there are ongoing symptoms on beta-blocker therapy, a calcium channel blocker (typically a dihydropyridine [eg, amlodipine]) may be added with close monitoring of heart rate; diltiazem may be used as an alternative therapy if there are contraindications or unacceptable adverse effects with beta-blockade (ACCF/AHA [Fihn 2012]).
Oral:
Immediate release: Initial: 30 mg 4 times daily; increase as needed at 1- to 2-day intervals to effective antianginal dose; usual effective dose: 240 to 360 mg/day in 3 to 4 divided doses (Kannam 2019).
12-hour (twice-daily) formulations (off-label): Initial: 60 mg twice daily; increase as needed at 7- to 14-day intervals to effective antianginal dose; usual effective dose: 240 to 360 mg/day in 2 divided doses (Kannam 2019; Weiner 1986).
24-hour (once-daily) formulations: Initial 120 to 180 mg once daily; increase as needed at 7- to 14-day intervals to effective antianginal dose; usual effective dose: 240 to 360 mg/day (Kannam 2019).
Vasospastic angina: Note: May use alone or in combination with nitrates (ACCF/AHA [Fihn 2012]). Some experts suggest initiating therapy with a 24-hour (once-daily) formulation (Pinto 2019).
Oral:
Immediate release: Initial: 30 mg 4 times daily; increase as needed at 1- to 2-day intervals to effective antianginal dose; usual effective dose: 240 to 360 mg/day in 3 to 4 divided doses.
12-hour (twice-daily) formulations (off-label): Initial: 60 mg twice daily; increase as needed at 7- to 14-day intervals to effective antianginal dose; usual effective dose: 240 to 360 mg/day in 2 divided doses (Pinto 2019).
24-hour (once-daily) formulations: Initial 120 to 180 mg once daily; increase as needed at 7- to 14-day intervals to effective antianginal dose; usual effective dose: 240 to 360 mg/day (Pinto 2019).
Chest pain associated with cocaine ingestion, with or without evidence of acute coronary syndrome (off-label use): Note: Adjunct or alternative to nitroglycerin.
IV: Initial bolus: 0.25 mg/kg (actual body weight) over 2 minutes (average dose: 20 mg); may repeat after 15 minutes if needed. Patients who respond after 1 or 2 bolus doses can be started on a continuous infusion for ongoing symptoms despite optimal therapy with nitroglycerin (Morgan 2019).
Atrial fibrillation or atrial flutter, rate control: Note: For rate control in hemodynamically stable patients. Do not use in patients with preexcitation associated with an accessory pathway, as this can lead to ventricular arrhythmias (AHA/ACC/HRS [January 2014]).
Acute ventricular rate control:
IV:
Bolus dose: 0.25 mg/kg (actual body weight) over 2 minutes (average dose: 20 mg); if rate control is insufficient after 15 minutes, a repeat bolus dose of 0.35 mg/kg over 2 minutes may be given (average dose: 25 mg). Patients who respond after 1 or 2 bolus doses can be started on a continuous infusion.
Continuous infusion following bolus(es): Initial: 5 to 10 mg/hour; infusion rate may be increased in 5 mg/hour increments according to ventricular response, up to a maximum of 15 mg/hour. Note: When increasing the infusion rate, an additional bolus dose can be used to provide more immediate onset (Ellenbogen 1991). In general, the use of a continuous infusion >24 hours or >15 mg/hour is not recommended due to potential for drug accumulation. See conversion section below to switch from IV infusion to oral.
Chronic ventricular rate control (off-label use):
Oral:
Immediate release: Initial: 30 mg 4 times daily; increase as needed to achieve ventricular rate control; usual dose: 120 to 480 mg/day in 3 or 4 divided doses (Ganz 2019).
Extended release: Initial: 120 mg once daily or in 2 divided doses depending on formulation; increase as needed to achieve ventricular rate control; usual dose: 120 to 480 mg/day (AHA/ACC/HRS [January 2014]; Ganz 2019).
Hypertension (alternative agent): Note: For initial treatment in patients with blood pressure ≥20/10 mm Hg above goal, may be used in combination with another appropriate agent (eg, ACE inhibitor, ARB, thiazide diuretic). For patients <20/10 mm Hg above goal, some experts recommend an initial trial of monotherapy; however, over time, many patients will require combination therapy (ACC/AHA [Whelton 2018]; Mann 2019). Some experts reserve nondihydropyridine calcium channel blockers for patients with a relevant comorbidity (eg, rate control in atrial fibrillation or flutter) (Mann 2019).
Oral:
12-hour (twice-daily) formulations: Initial: 60 to 120 mg twice daily; increase dose as needed after ~7 to 14 days; usual dose: 240 to 360 mg/day in 2 divided doses.
24-hour (once-daily) formulations: Initial: 120 to 240 mg once daily; increase dose as needed after ~7 to 14 days; usual dose: 120 to 360 mg once daily (ACC/AHA [Whelton 2018]).
Nonsustained ventricular tachycardia or ventricular premature beats, symptomatic (alternative agent) (off-label use): Note: A beta-blocker is the preferred initial therapy; if there are ongoing symptoms on beta-blocker therapy, diltiazem may be added with close monitoring of heart rate; diltiazem may be used as an alternative therapy if beta-blockade cannot be tolerated (Zimetbaum 2019).
Oral: Initial: 120 to 180 mg once daily or in divided doses depending on the drug formulation; usual effective dose: 240 to 360 mg/day (Zimetbaum 2019).
Pulmonary arterial hypertension (group 1) (alternative agent) (off-label use): Note: Only used for rigorously selected group 1 pulmonary arterial hypertension patients with a positive vasoreactivity test and under the care of a pulmonary hypertension specialist (ACCP [Klinger 2019; Taichman 2014]; ESC/ERS [Galiè 2016]).
Oral: 24-hour (once-daily) formulations: 120 mg once daily; titrate gradually and with close hemodynamic monitoring; reported daily dose range: 240 to 720 mg/day (ACCP [Taichman 2014]; ESC/ERS [Galiè 2016]; Montani 2010; Sitbon 2005)
Supraventricular tachycardia (eg, atrioventricular nodal reentrant tachycardia, atrioventricular reentrant tachycardia, focal atrial tachycardia, multifocal atrial tachycardia) (alternative agent): Note: For hemodynamically stable patients if vagal maneuvers and/or adenosine are unsuccessful. Do not use in patients with preexcitation associated with an accessory pathway, as this can lead to ventricular arrhythmias (ACC/AHA/HRS [Page 2016]; Prutkin 2019).
Acute treatment:
IV: Bolus dose: 0.25 mg/kg (actual body weight) over 2 minutes (average dose: 20 mg); if response is insufficient after ≥15 minutes, a repeat bolus dose of 0.35 mg/kg over 2 minutes may be given (average dose: 25 mg). If bolus(es) do not terminate the arrhythmia, consider alternative therapy.
Chronic maintenance (off-label use):
Oral:
Immediate release: Initial: 30 mg 4 times daily; increase as needed for heart rate control; usual effective dose: 360 mg/day in divided doses (ACC/AHA/HRS [Page 2016])
Extended release: Initial: 120 mg once daily or in 2 divided doses depending on formulation; increase as needed for heart rate control; usual effective dose: 360 mg/day (ACC/AHA/HRS [Page 2016])
Conversion between dosage forms:
Conversion from immediate-release to extended-release formulations: Patients stabilized on a maintenance regimen between 120 and 360 mg of immediate-release tablets may be switched to an extended-release formulation at the same daily dose administered in 1 or 2 divided doses depending on formulation. In some patients, the dosage of the extended-release formulation may require adjustment following conversion.
Conversion from IV infusion to oral: Immediate release can be started ~1 hour before stopping infusion. Oral daily dose may be estimated from the IV infusion rate by using the equation below. Round oral doses to the nearest appropriate strength and formulation.
Oral dose (mg per day) = [infusion rate (mg/hour) × 3 + 3] × 10
5 mg/hour = 180 mg/day
10 mg/hour = 300 to 360 mg/day
15 mg/hour = 480 mg/day
Dosing: Geriatric
Refer to adult dosing. In the management of hypertension, consider lower initial doses (eg, 120 mg once daily using extended-release capsule) and titrate to response (Aronow 2011).
Dosing: Pediatric
Atrial tachyarrhythmias, rate control (bridge to therapy): Very limited data available: Infants ≥6 months, Children, and Adolescents: IV: Initial bolus: 0.25 mg/kg over 5 minutes (maximum dose: 20 mg/dose [average adult dose]) followed by a continuous IV infusion; reported rate range in one study was 0.05 to 0.15 mg/kg/hour. Note: Usual adult infusion rate for arrhythmia is 5 to 15 mg/hour. Dose should be individualized based on patient response. Dosing based on a small study of 10 patients with atrial tachycardia (age range: 6 months to 21 years; most patients were adolescents) who received an initial bolus of 0.25 mg/kg/dose followed by a continuous infusion titrated to effect, reported effective range was 0.05 to 0.15 mg/kg/hour (mean infusion rate: 0.11 mg/kg/hour). Rate control was achieved in 9 of the 10 patients within 10 minutes of dosing. One patient required an additional bolus of 0.25 mg/kg. Median ventricular rate of study group prior to initial bolus was 275 ± 50 beats per minute (BPM) (range: 185 to 500 BPM), which decreased to a median of 166 BPM prior to initiation of continuous infusion and decreased to a median of 123 BPM after 10 minutes of continuous infusion; blood pressure was not significantly affected by diltiazem; qualitative systolic function did not worsen in the seven patients studied (Pass 2000). Note: In adult patients, infusions >24 hours are not recommended; with administration of diltiazem infusion >24 hours, the possibility of decreased diltiazem clearance, prolonged elimination half-life, and increased diltiazem and/or diltiazem metabolite plasma concentrations should be considered. In trial of 10 pediatric patients, the median duration was 45 hours (mean: 54 hours; range: 14 to 126 hours) (Pass 2000)
Hypertension: Limited data available:
Infants and Children: Oral: Immediate-release formulations: Initial: 1.5 to 2 mg/kg/day in 3 to 4 divided doses (Flynn 2000; Park 2014); increase gradually, at 1- to 2-day intervals until optimum response is obtained; usual maximum daily dose: 3.5 mg/kg/day (Park 2014); some experts recommend a higher maximum daily dose of 6 mg/kg/day up to 360 mg/day; whichever is less (Flynn 2000). Note: Once patient is established on a total daily dose, may convert to an extended release dosage form at the appropriate interval (once or twice daily) in children able to swallow capsules whole and receiving adequate mg amount (Flynn 2000).
Adolescents (Park 2014): Oral:
Immediate-release formulations: 30 to 120 mg/dose administered 3 to 4 times daily; usual daily dosage range: 180 to 360 mg/day
Extended-release formulations:
Capsule, extended release (once daily dosing; eg, Cardizem CD, Tiazac): 120 to 300 mg once daily
Capsule, extended release (twice daily dosing; eg, Cardizem SR): 120 to 300 mg/day in 2 divided doses
Reconstitution
Solution for injection: Continuous IV infusion: Further dilute with NS, D5W, or D51/2NS to a maximum final concentration of 1 mg/mL.
Solution reconstituted, IV (ADD-Vantage): Refer to manufacturer’s labeling.
Extemporaneously Prepared
A 12 mg/mL oral suspension may be made from tablets (regular, not extended release) and one of three different vehicles (cherry syrup, a 1:1 mixture of Ora-Sweet® and Ora-Plus®, or a 1:1 mixture of Ora-Sweet® SF and Ora-Plus®). Crush sixteen 90 mg tablets in a mortar and reduce to a fine powder. Add 10 mL of the chosen vehicle and mix to a uniform paste; mix while adding the vehicle in incremental proportions to almost 120 mL; transfer to a calibrated bottle, rinse mortar with vehicle, and add quantity of vehicle sufficient to make 120 mL. Label “shake well” and “protect from light". Stable for 60 days when stored in amber plastic prescription bottles in the dark at room temperature or refrigerated. Note: The tablets used within the supportive study were tablets manufactured using a direct compression technique and were not film-coated. Use of film-coated tablets to prepare an oral suspension has not been formally evaluated and may result in an unsuitable suspension. The manufacturers of the film-coated tablets do not recommend crushing. Brand name Cardizem tablets are prepared using a direct compression technique and may be crushed.
Allen LV and Erickson MA, “Stability of Baclofen, Captopril, Diltiazem Hydrochloride, Dipyridamole, and Flecainide Acetate in Extemporaneously Compounded Oral Liquids,” Am J Health Syst Pharm, 1996, 53(18):2179-84.8879325
Administration
Oral:
Immediate release tablet (eg, Cardizem): Administer before meals and at bedtime. The manufacturers of the film-coated tablets recommend to swallow the tablet whole; do not split, crush, or chew. According to these manufacturers, crushing immediate release tablets may alter pharmacokinetics. However, crushing tablets that are prepared using a direct compression technique is acceptable. An oral suspension has been made using the immediate release tablets manufactured using a direct compression technique (Allen 1996). Brand name Cardizem tablets are prepared using a direct compression technique and may be crushed.
Long acting dosage forms: Do not open, chew, or crush; swallow whole. Administer at same time of day either morning or evening.
Cardizem CD, Cardizem LA, Cartia XT, Matzim LA: Administer without regard to meals.
Dilt XR: Administer on an empty stomach in the morning.
Taztia XT, Tiazac: Capsules may be opened and sprinkled on a spoonful of applesauce. Applesauce should not be hot and should be swallowed without chewing, followed by drinking a glass of water.
Tiazac XC [Canadian product]: Administer at bedtime
IV: Bolus doses given over 2 minutes with continuous ECG and blood pressure monitoring. Continuous infusion should be via infusion pump. May increase infusion rate in 5 mg/hour increments as needed (maximum: 15 mg/hour). Response to bolus may require several minutes to reach maximum. Response may persist for several hours after infusion is discontinued.
Storage
Capsule, tablet: Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Protect from light. Avoid excessive heat (>30°C) and humidity.
Solution for injection: Store in refrigerator at 2°C to 8°C (36°F to 46°F); do not freeze. May be stored at room temperature for up to 1 month. Following dilution to ≤1 mg/mL with D51/2NS, D5W, or NS, solution is stable for 24 hours at room temperature (15°C to 30°C (59°F to 86°F) or under refrigeration).
Solution reconstituted, intravenous (ADD-Vantage): Store at 20°C to 25°C (68°F to 77°F); do not freeze. Following reconstitution, solution is stable for 24 hours at room temperature or under refrigeration (2°C to 8°C [36°F to 46°F]).
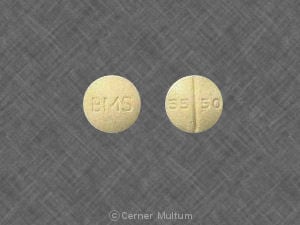
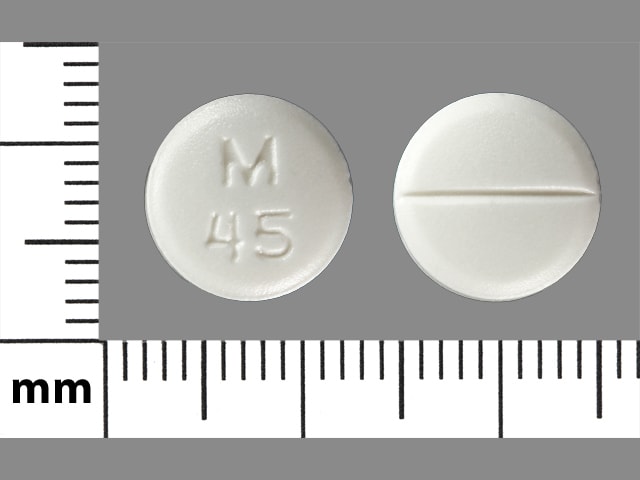
Diltiazem Images
Drug Interactions
Abemaciclib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Abemaciclib. Monitor therapy
Acalabrutinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Acalabrutinib. Management: Reduce acalabrutinib dose to 100 mg once daily with concurrent use of a moderate CYP3A4 inhibitor. Monitor patient closely for both acalabrutinib response and evidence of adverse effects with any concurrent use. Consider therapy modification
Alfentanil: DilTIAZem may increase the serum concentration of Alfentanil. Monitor therapy
Alfuzosin: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Alpha1-Blockers: May enhance the hypotensive effect of Calcium Channel Blockers. Monitor therapy
Amifostine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Amifostine. Management: When amifostine is used at chemotherapy doses, blood pressure lowering medications should be withheld for 24 hours prior to amifostine administration. If blood pressure lowering therapy cannot be withheld, amifostine should not be administered. Consider therapy modification
Amiodarone: Calcium Channel Blockers (Nondihydropyridine) may enhance the bradycardic effect of Amiodarone. Sinus arrest has been reported. Monitor therapy
AmLODIPine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of AmLODIPine. Monitor therapy
Amphetamines: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Antifungal Agents (Azole Derivatives, Systemic): May enhance the adverse/toxic effect of Calcium Channel Blockers. Specifically, itraconazole may enhance the negative inotropic effects of verapamil or diltiazem. Antifungal Agents (Azole Derivatives, Systemic) may decrease the metabolism of Calcium Channel Blockers. Fluconazole and isavuconazonium likely exert weaker effects than other azoles and are addressed in separate monographs. Management: Concurrent use of felodipine or nisoldipine with itraconazole is specifically contraindicated. Frequent monitoring is warranted with any such combination; calcium channel blocker dose reductions may be required. Exceptions: Fluconazole; Isavuconazonium Sulfate. Consider therapy modification
Antipsychotic Agents (Second Generation [Atypical]): Blood Pressure Lowering Agents may enhance the hypotensive effect of Antipsychotic Agents (Second Generation [Atypical]). Monitor therapy
Apixaban: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Apixaban. Monitor therapy
Aprepitant: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Aprepitant. Avoid combination
ARIPiprazole: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of ARIPiprazole. Management: Monitor for increased aripiprazole pharmacologic effects. Aripiprazole dose adjustments may or may not be required based on concomitant therapy and/or indication. Consult full interaction monograph for specific recommendations. Monitor therapy
ARIPiprazole: CYP2D6 Inhibitors (Weak) may increase the serum concentration of ARIPiprazole. Management: Monitor for increased aripiprazole pharmacologic effects. Aripiprazole dose adjustments may or may not be required based on concomitant therapy and/or indication. Consult full interaction monograph for specific recommendations. Monitor therapy
Aspirin: Calcium Channel Blockers (Nondihydropyridine) may enhance the antiplatelet effect of Aspirin. Monitor therapy
Asunaprevir: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Asunaprevir. Avoid combination
AtorvaSTATin: May increase the serum concentration of DilTIAZem. DilTIAZem may increase the serum concentration of AtorvaSTATin. Management: Consider using lower atorvastatin doses when used together with diltiazem. Consider therapy modification
Atosiban: Calcium Channel Blockers may enhance the adverse/toxic effect of Atosiban. Specifically, there may be an increased risk for pulmonary edema and/or dyspnea. Monitor therapy
Avanafil: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Avanafil. Management: The maximum avanafil adult dose is 50 mg per 24-hour period when used together with a moderate CYP3A4 inhibitor. Patients receiving such a combination should also be monitored more closely for evidence of adverse effects. Consider therapy modification
Avapritinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Avapritinib. Management: Avoid use of moderate CYP3A4 inhibitors with avapritinib. If this combination cannot be avoided, reduce the avapritinib dose from 300 mg once daily to 100 mg once daily. Consider therapy modification
Axitinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Axitinib. Monitor therapy
Barbiturates: May increase the metabolism of Calcium Channel Blockers. Management: Monitor for decreased therapeutic effects of calcium channel blockers with concomitant barbiturate therapy. Calcium channel blocker dose adjustments may be necessary. Nimodipine Canadian labeling contraindicates concomitant use with phenobarbital. Monitor therapy
Barbiturates: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Benperidol: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Benzhydrocodone: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Benzhydrocodone. Specifically, the concentration of hydrocodone may be increased. Monitor therapy
Beta-Blockers: Calcium Channel Blockers (Nondihydropyridine) may enhance the hypotensive effect of Beta-Blockers. Bradycardia and signs of heart failure have also been reported. Calcium Channel Blockers (Nondihydropyridine) may increase the serum concentration of Beta-Blockers. Exceptions: Levobunolol; Metipranolol. Monitor therapy
Blonanserin: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Blonanserin. Monitor therapy
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Bosentan: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Bosentan. Management: Concomitant use of both a CYP2C9 inhibitor and a CYP3A inhibitor or a single agent that inhibits both enzymes with bosentan is likely to cause a large increase in serum concentrations of bosentan and is not recommended. See monograph for details. Monitor therapy
Bosutinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Bosutinib. Avoid combination
Bradycardia-Causing Agents: May enhance the bradycardic effect of other Bradycardia-Causing Agents. Monitor therapy
Brexpiprazole: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Brexpiprazole. Management: The brexpiprazole dose should be reduced to 25% of usual if used together with both a moderate CYP3A4 inhibitor and a strong or moderate CYP2D6 inhibitor, or if a moderate CYP3A4 inhibitor is used in a CYP2D6 poor metabolizer. Monitor therapy
Brigatinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Brigatinib. Management: Avoid concurrent use of brigatinib with moderate CYP3A4 inhibitors when possible. If such a combination cannot be avoided, reduce the dose of brigatinib by approximately 40% (ie, from 180 mg to 120 mg, from 120 mg to 90 mg, or from 90 mg to 60 mg). Consider therapy modification
Brimonidine (Topical): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Bromocriptine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Bromocriptine. Management: The bromocriptine dose should not exceed 1.6 mg daily with use of a moderate CYP3A4 inhibitor. The Cycloset brand specifically recommends this dose limitation, but other bromocriptine products do not make such specific recommendations. Consider therapy modification
Bromperidol: Blood Pressure Lowering Agents may enhance the hypotensive effect of Bromperidol. Bromperidol may diminish the hypotensive effect of Blood Pressure Lowering Agents. Avoid combination
Budesonide (Systemic): CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Budesonide (Systemic). Avoid combination
Budesonide (Topical): CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Budesonide (Topical). Management: Per US prescribing information, avoid this combination. Canadian product labeling does not recommend strict avoidance. If combined, monitor for excessive glucocorticoid effects as budesonide exposure may be increased. Consider therapy modification
BusPIRone: Calcium Channel Blockers (Nondihydropyridine) may increase the serum concentration of BusPIRone. Monitor therapy
Calcium Channel Blockers (Dihydropyridine): May enhance the hypotensive effect of Calcium Channel Blockers (Nondihydropyridine). Calcium Channel Blockers (Nondihydropyridine) may increase the serum concentration of Calcium Channel Blockers (Dihydropyridine). Monitor therapy
Calcium Salts: May diminish the therapeutic effect of Calcium Channel Blockers. Monitor therapy
Cannabidiol: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Cannabidiol. Monitor therapy
Cannabis: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Cannabis. More specifically, tetrahydrocannabinol and cannabidiol serum concentrations may be increased. Monitor therapy
CarBAMazepine: Calcium Channel Blockers (Nondihydropyridine) may increase the serum concentration of CarBAMazepine. CarBAMazepine may decrease the serum concentration of Calcium Channel Blockers (Nondihydropyridine). Management: Consider empiric reductions in carbamazepine dose with initiation of nondihydropyridine calcium channel blockers. Monitor for increased toxic effects of carbamazepine and reduced therapeutic effects of the calcium channel blocker. Consider therapy modification
Cardiac Glycosides: Calcium Channel Blockers (Nondihydropyridine) may enhance the AV-blocking effect of Cardiac Glycosides. Calcium Channel Blockers (Nondihydropyridine) may increase the serum concentration of Cardiac Glycosides. Monitor therapy
Ceritinib: Bradycardia-Causing Agents may enhance the bradycardic effect of Ceritinib. Management: If this combination cannot be avoided, monitor patients for evidence of symptomatic bradycardia, and closely monitor blood pressure and heart rate during therapy. Exceptions are discussed in separate monographs. Consider therapy modification
Cilostazol: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Cilostazol. Management: Consider reducing the cilostazol dose to 50 mg twice daily in adult patients who are also receiving moderate inhibitors of CYP3A4. Consider therapy modification
Cimetidine: May increase the serum concentration of Calcium Channel Blockers. Management: Consider alternatives to cimetidine. If no suitable alternative exists, monitor for increased effects of calcium channel blockers following cimetidine initiation/dose increase, and decreased effects following cimetidine discontinuation/dose decrease. Consider therapy modification
Clofazimine: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CloNIDine: May enhance the AV-blocking effect of Calcium Channel Blockers (Nondihydropyridine). Sinus node dysfunction may also be enhanced. Monitor therapy
Clopidogrel: Calcium Channel Blockers may diminish the therapeutic effect of Clopidogrel. Monitor therapy
Cobimetinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Cobimetinib. Management: Avoid the concomitant use of cobimetinib and moderate CYP3A4 inhibitors. If concurrent short term (14 days or less) use cannot be avoided, reduce the cobimetinib dose to 20 mg daily. Avoid combination
Codeine: CYP3A4 Inhibitors (Moderate) may increase serum concentrations of the active metabolite(s) of Codeine. Monitor therapy
Colchicine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Colchicine. Management: Reduce colchicine dose as directed when using with a moderate CYP3A4 inhibitor, and increase monitoring for colchicine-related toxicity. See full monograph for details. Use extra caution in patients with impaired renal and/or hepatic function. Consider therapy modification
Colestipol: May decrease the absorption of DilTIAZem. Monitor therapy
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Corticosteroids (Systemic): DilTIAZem may increase the serum concentration of Corticosteroids (Systemic). Monitor therapy
CycloSPORINE (Systemic): Calcium Channel Blockers (Nondihydropyridine) may decrease the metabolism of CycloSPORINE (Systemic). CycloSPORINE (Systemic) may decrease the metabolism of Calcium Channel Blockers (Nondihydropyridine). Consider therapy modification
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May increase the metabolism of CYP3A4 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
CYP3A4 Inhibitors (Moderate): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CYP3A4 Inhibitors (Strong): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Consider therapy modification
CYP3A4 Substrates (High risk with Inhibitors): CYP3A4 Inhibitors (Moderate) may decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Exceptions: Alitretinoin (Systemic); Praziquantel; Trabectedin; Vinorelbine. Monitor therapy
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dantrolene: May enhance the hyperkalemic effect of Calcium Channel Blockers (Nondihydropyridine). Dantrolene may enhance the negative inotropic effect of Calcium Channel Blockers (Nondihydropyridine). Management: This interaction has only been described with intravenous dantrolene administration. Avoid combination
Dapoxetine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Dapoxetine. Management: The dose of dapoxetine should be limited to 30 mg per day when used together with a moderate inhibitor of CYP3A4. Consider therapy modification
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Deflazacort: CYP3A4 Inhibitors (Moderate) may increase serum concentrations of the active metabolite(s) of Deflazacort. Management: Administer one third of the recommended deflazacort dose when used together with a strong or moderate CYP3A4 inhibitor. Consider therapy modification
Dexmethylphenidate: May diminish the therapeutic effect of Antihypertensive Agents. Monitor therapy
Diazoxide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Disopyramide: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Disopyramide. Monitor therapy
Dofetilide: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Dofetilide. Monitor therapy
Domperidone: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Domperidone. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Avoid combination
DOXOrubicin (Conventional): CYP3A4 Inhibitors (Moderate) may increase the serum concentration of DOXOrubicin (Conventional). Management: Seek alternatives to moderate CYP3A4 inhibitors in patients treated with doxorubicin whenever possible. One U.S. manufacturer (Pfizer Inc.) recommends that these combinations be avoided. Consider therapy modification
Dronabinol: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Dronabinol. Monitor therapy
Dronedarone: Calcium Channel Blockers (Nondihydropyridine) may enhance the AV-blocking effect of Dronedarone. Other electrophysiologic effects of Dronedarone may also be increased. Calcium Channel Blockers (Nondihydropyridine) may increase the serum concentration of Dronedarone. Dronedarone may increase the serum concentration of Calcium Channel Blockers (Nondihydropyridine). Management: Use lower starting doses of the nondihydropyridine calcium channel blockers (i.e., verapamil, diltiazem), and only consider increasing calcium channel blocker dose after obtaining ECG-based evidence that the combination is being well-tolerated. Consider therapy modification
DULoxetine: Blood Pressure Lowering Agents may enhance the hypotensive effect of DULoxetine. Monitor therapy
Duvelisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Efavirenz: May decrease the serum concentration of DilTIAZem. Monitor therapy
Eletriptan: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Eletriptan. Management: The use of eletriptan within 72 hours of a moderate CYP3A4 inhibitor should be avoided. Consider therapy modification
Elexacaftor, Tezacaftor, and Ivacaftor: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Elexacaftor, Tezacaftor, and Ivacaftor. Management: When combined with moderate CYP3A4 inhibitors, two elexacaftor/tezacaftor/ivacaftor (100 mg/50 mg/75 mg) tablets should be given in the morning, every other day. Ivacaftor (150 mg) should be given in the morning, every other day on alternate days. Consider therapy modification
Eliglustat: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Eliglustat. Management: Use should be avoided under some circumstances. See full drug interaction monograph for details. Consider therapy modification
Encorafenib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Encorafenib. Management: Avoid concomitant use of encorafenib and moderate CYP3A4 inhibitors whenever possible. If concomitant administration is unavoidable, decrease the encorafenib dose prior to initiation of the CYP3A4 inhibitor. See full monograph for details. Consider therapy modification
Entrectinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Entrectinib. Management: Avoid moderate CYP3A4 inhibitors during treatment with entrectinib. Reduce dose to 200 mg/day if combination cannot be avoided in adults and those 12 yrs of age or older with a BSA of at least 1.5 square meters. No alternative dosing provided for others. Consider therapy modification
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Eplerenone: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Eplerenone. Management: When used concomitantly with moderate inhibitors of CYP3A4, eplerenone dosing recommendations vary by indication and international labeling. See full drug interaction monograph for details. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Erdafitinib: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Esmolol: Calcium Channel Blockers (Nondihydropyridine) may enhance the bradycardic effect of Esmolol. Management: Administration of IV verapamil or diltiazem together with esmolol is contraindicated if one agent is given while the effects of the other are still present. Canadian esmolol labeling specifies that use within 24 hours is contraindicated. Consider therapy modification
Estrogen Derivatives: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Estrogen Derivatives. Monitor therapy
Everolimus: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Everolimus. Management: Everolimus dose reductions are required for most indications. See full monograph or prescribing information for specific dose adjustment and monitoring recommendations. Consider therapy modification
FentaNYL: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of FentaNYL. Management: Monitor patients closely for several days following initiation of this combination, and adjust fentanyl dose as necessary. Consider therapy modification
Fexinidazole [INT]: Bradycardia-Causing Agents may enhance the arrhythmogenic effect of Fexinidazole [INT]. Avoid combination
Fingolimod: DilTIAZem may enhance the bradycardic effect of Fingolimod. Monitor therapy
Flibanserin: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Flibanserin. Avoid combination
Fluconazole: May increase the serum concentration of Calcium Channel Blockers. Monitor therapy
Fosaprepitant: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Fosaprepitant. Avoid combination
Fosnetupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosphenytoin: Calcium Channel Blockers may increase the serum concentration of Fosphenytoin. Management: Monitor for phenytoin toxicity with concomitant use of a calcium channel blocker (CCB) or decreased phenytoin effects with CCB discontinuation. Monitor for decreased CCB therapeutic effects. Nimodipine Canadian labeling contraindicates use with phenytoin. Consider therapy modification
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Grapefruit Juice: May increase the serum concentration of DilTIAZem. Monitor therapy
GuanFACINE: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of GuanFACINE. Management: Reduce the guanfacine dose by 50% when initiating this combination. Consider therapy modification
Halofantrine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Halofantrine. Management: Extreme caution, with possibly increased monitoring of ECGs, should be used if halofantrine is combined with moderate CYP3A4 inhibitors. Drugs listed as exceptions to this monograph are discussed in separate drug interaction monographs. Monitor therapy
Herbs (Hypertensive Properties): May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Herbs (Hypotensive Properties): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
HYDROcodone: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of HYDROcodone. Monitor therapy
Hypotension-Associated Agents: Blood Pressure Lowering Agents may enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Ibrutinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Ibrutinib. Management: When treating B-cell malignancies, decrease ibrutinib to 280 mg daily when combined with moderate CYP3A4 inhibitors. When treating graft versus host disease, monitor patients closely and reduce the ibrutinib dose as needed based on adverse reactions. Consider therapy modification
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Ifosfamide: CYP3A4 Inhibitors (Moderate) may decrease serum concentrations of the active metabolite(s) of Ifosfamide. Monitor therapy
Imatinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Imatinib. Monitor therapy
Ivabradine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Ivabradine. Avoid combination
Ivabradine: Calcium Channel Blockers (Nondihydropyridine) may enhance the bradycardic effect of Ivabradine. Ivabradine may enhance the QTc-prolonging effect of Calcium Channel Blockers (Nondihydropyridine). Specifically, the QTc prolonging effects of bepridil may be enhanced. Calcium Channel Blockers (Nondihydropyridine) may increase the serum concentration of Ivabradine. Specifically, verapamil or diltiazem may increase serum ivabradine concentrations. Avoid combination
Ivacaftor: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Ivacaftor. Management: Ivacaftor dose reductions may be required; consult full monograph content for age- and weight-specific dosage recommendations. Consider therapy modification
Ivosidenib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Ivosidenib. Management: Avoid use of moderate CYP3A4 inhibitors with ivosidenib whenever possible. If combined, monitor for increased ivosidenib toxicities. Drugs listed as exceptions are discussed in further detail in separate drug interaction monographs. Consider therapy modification
Lacosamide: Bradycardia-Causing Agents may enhance the AV-blocking effect of Lacosamide. Monitor therapy
Larotrectinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Lasmiditan: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Avoid combination
Lefamulin: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Lefamulin. Management: Monitor for lefamulin adverse effects during coadministration of lefamulin tablets with moderate CYP3A4 inhibitors. Monitor therapy
Lemborexant: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Lemborexant. Avoid combination
Levamlodipine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Levamlodipine. Monitor therapy
Levodopa-Containing Products: Blood Pressure Lowering Agents may enhance the hypotensive effect of Levodopa-Containing Products. Monitor therapy
Lithium: Calcium Channel Blockers (Nondihydropyridine) may enhance the neurotoxic effect of Lithium. Calcium Channel Blockers (Nondihydropyridine) may increase the serum concentration of Lithium. Decreased or unaltered lithium concentrations have also been reported with this combination. Monitor therapy
Lomitapide: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Lomitapide. Avoid combination
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Lormetazepam: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Lovastatin: May increase the serum concentration of DilTIAZem. DilTIAZem may increase the serum concentration of Lovastatin. Management: Initiate lovastatin at a maximum adult dose of 10 mg/day, and do not exceed 20 mg/day, in patients receiving diltiazem. Monitor closely for signs of HMG-CoA reductase inhibitor toxicity (e.g., myositis, rhabdomyolysis). Consider therapy modification
Lumateperone: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Lumateperone. Avoid combination
Lurasidone: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Lurasidone. Management: Lurasidone US labeling recommends reducing lurasidone dose by half with a moderate CYP3A4 inhibitor. Some non-US labeling recommends initiating lurasidone at 20 mg/day and limiting dose to 40 mg/day; avoid concurrent use of grapefruit products. Consider therapy modification
Macrolide Antibiotics: May decrease the metabolism of Calcium Channel Blockers. Management: Consider using a noninteracting macrolide. Felodipine Canadian labeling specifically recommends avoiding its use in combination with clarithromycin. Exceptions: Azithromycin (Systemic); Fidaxomicin; Roxithromycin; Spiramycin. Consider therapy modification
Magnesium Salts: Calcium Channel Blockers may enhance the adverse/toxic effect of Magnesium Salts. Magnesium Salts may enhance the hypotensive effect of Calcium Channel Blockers. Monitor therapy
Manidipine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Manidipine. Monitor therapy
Meperidine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Meperidine. Monitor therapy
Methylphenidate: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Midodrine: May enhance the bradycardic effect of Bradycardia-Causing Agents. Monitor therapy
Midostaurin: DilTIAZem may increase the serum concentration of Midostaurin. Management: Seek alternatives to the concomitant use of midostaurin and diltiazem if possible. If concomitant use cannot be avoided, monitor patients for increased risk of adverse reactions. Consider therapy modification
MiFEPRIStone: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Minimize doses of CYP3A4 substrates, and monitor for increased concentrations/toxicity, during and 2 weeks following treatment with mifepristone. Avoid cyclosporine, dihydroergotamine, ergotamine, fentanyl, pimozide, quinidine, sirolimus, and tacrolimus. Consider therapy modification
Mirodenafil: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Mirodenafil. Monitor therapy
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Molsidomine: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Naftopidil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Naldemedine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Naldemedine. Monitor therapy
Nalfurafine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Nalfurafine. Monitor therapy
Naloxegol: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Naloxegol. Avoid combination
Neratinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Neratinib. Avoid combination
Netupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Neuromuscular-Blocking Agents (Nondepolarizing): Calcium Channel Blockers may enhance the neuromuscular-blocking effect of Neuromuscular-Blocking Agents (Nondepolarizing). Monitor therapy
Nicergoline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicorandil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
NiMODipine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of NiMODipine. Monitor therapy
Nitroprusside: Blood Pressure Lowering Agents may enhance the hypotensive effect of Nitroprusside. Monitor therapy
Obinutuzumab: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Management: Consider temporarily withholding blood pressure lowering medications beginning 12 hours prior to obinutuzumab infusion and continuing until 1 hour after the end of the infusion. Consider therapy modification
Olaparib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Olaparib. Management: Avoid use of moderate CYP3A4 inhibitors in patients being treated with olaparib, if possible. If such concurrent use cannot be avoided, the dose of olaparib should be reduced to 150 mg twice daily. Consider therapy modification
Opioids (Anilidopiperidine): May enhance the bradycardic effect of Calcium Channel Blockers (Nondihydropyridine). Opioids (Anilidopiperidine) may enhance the hypotensive effect of Calcium Channel Blockers (Nondihydropyridine). Monitor therapy
OxyCODONE: CYP3A4 Inhibitors (Moderate) may enhance the adverse/toxic effect of OxyCODONE. CYP3A4 Inhibitors (Moderate) may increase the serum concentration of OxyCODONE. Serum concentrations of the active metabolite Oxymorphone may also be increased. Monitor therapy
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Pentoxifylline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Perhexiline: CYP2D6 Inhibitors (Weak) may increase the serum concentration of Perhexiline. Monitor therapy
Pexidartinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Pexidartinib. Monitor therapy
P-glycoprotein/ABCB1 Inducers: May decrease the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inducers may also further limit the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Monitor therapy
P-glycoprotein/ABCB1 Inhibitors: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inhibitors may also enhance the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Monitor therapy
Phenytoin: Calcium Channel Blockers may increase the serum concentration of Phenytoin. Phenytoin may decrease the serum concentration of Calcium Channel Blockers. Management: Avoid use of nimodipine or nifedipine with phenytoin. Monitor for phenytoin toxicity and/or decreased calcium channel blocker effects with any concurrent use. Consider therapy modification
Pholcodine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Pholcodine. Monitor therapy
Phosphodiesterase 5 Inhibitors: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Pimecrolimus: CYP3A4 Inhibitors (Moderate) may decrease the metabolism of Pimecrolimus. Monitor therapy
Pimozide: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Pimozide. Avoid combination
Propafenone: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Propafenone. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Prostacyclin Analogues: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Protease Inhibitors: May decrease the metabolism of Calcium Channel Blockers (Nondihydropyridine). Increased serum concentrations of the calcium channel blocker may increase risk of AV nodal blockade. Management: Avoid concurrent use when possible. If used, monitor for CCB toxicity. The manufacturer of atazanavir recommends a 50% dose reduction for diltiazem be considered. Saquinavir, tipranavir, and darunavir/cobicistat use with bepridil is contraindicated. Consider therapy modification
Quinagolide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
QuiNIDine: DilTIAZem may increase the serum concentration of QuiNIDine. Monitor therapy
Ranolazine: Calcium Channel Blockers (Nondihydropyridine) may increase the serum concentration of Ranolazine. Management: Limit ranolazine dose to a maximum of 500 mg twice daily when used with diltiazem or verapamil. Consider therapy modification
Ranolazine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Ranolazine. Management: Limit the ranolazine adult dose to a maximum of 500 mg twice daily in patients concurrently receiving moderate CYP3A4 inhibitors (e.g., diltiazem, verapamil, erythromycin, etc.). Consider therapy modification
Red Yeast Rice: Calcium Channel Blockers (Nondihydropyridine) may increase the serum concentration of Red Yeast Rice. Specifically, concentrations of lovastatin (and possibly other related compounds) may be increased. Monitor therapy
Regorafenib: May enhance the bradycardic effect of Calcium Channel Blockers (Nondihydropyridine). Monitor therapy
RifAMPin: May decrease the serum concentration of DilTIAZem. Avoid combination
Rifamycin Derivatives: May decrease the serum concentration of Calcium Channel Blockers. This primarily affects oral forms of calcium channel blockers. Management: The labeling for some US and Canadian calcium channel blockers contraindicate use with rifampin, however recommendations vary. Consult appropriate labeling. Consider therapy modification
Rupatadine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Rupatadine. Monitor therapy
Ruxolitinib: May enhance the bradycardic effect of Bradycardia-Causing Agents. Management: Ruxolitinib Canadian product labeling recommends avoiding use with bradycardia-causing agents to the extent possible. Monitor therapy
Ruxolitinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Ruxolitinib. Monitor therapy
Salmeterol: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Salmeterol. Monitor therapy
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
SAXagliptin: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of SAXagliptin. Monitor therapy
Sildenafil: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Sildenafil. Monitor therapy
Silodosin: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Silodosin. Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Simeprevir. Avoid combination
Simvastatin: May increase the serum concentration of DilTIAZem. DilTIAZem may increase the serum concentration of Simvastatin. Management: Avoid concurrent use of diltiazem with simvastatin when possible. If used together, limit adult doses to simvastatin 10 mg/day and diltiazem 240 mg/day; avoid Simcor (simvastatin/niacin) because fixed simvastatin doses exceed the maximum. Consider therapy modification
Sincalide: Drugs that Affect Gallbladder Function may diminish the therapeutic effect of Sincalide. Management: Consider discontinuing drugs that may affect gallbladder motility prior to the use of sincalide to stimulate gallbladder contraction. Consider therapy modification
Siponimod: Bradycardia-Causing Agents may enhance the bradycardic effect of Siponimod. Management: Avoid coadministration of siponimod with drugs that may cause bradycardia. Consider therapy modification
Sirolimus: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Sirolimus. Management: Monitor for increased serum concentrations of sirolimus if combined with a moderate CYP3A4 inhibitor. Lower initial sirolimus doses or sirolimus dose reductions will likely be required. Consider therapy modification
Sonidegib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Sonidegib. Management: Avoid concomitant use of sonidegib and moderate CYP3A4 inhibitors when possible. When concomitant use cannot be avoided, limit CYP3A4 inhibitor use to less than 14 days and monitor for sonidegib toxicity (particularly musculoskeletal adverse reactions). Consider therapy modification
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
Suvorexant: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Suvorexant. Management: The recommended dose of suvorexant is 5 mg daily in patients receiving a moderate CYP3A4 inhibitor. The dose can be increased to 10 mg daily (maximum dose) if necessary for efficacy. Consider therapy modification
Tacrolimus (Systemic): Calcium Channel Blockers (Nondihydropyridine) may decrease the metabolism of Tacrolimus (Systemic). Monitor therapy
Tacrolimus (Topical): Calcium Channel Blockers (Nondihydropyridine) may decrease the metabolism of Tacrolimus (Topical). Monitor therapy
Tamsulosin: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Tamsulosin. Monitor therapy
Tazemetostat: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Tazemetostat. Management: Avoid coadministration of tazemetostat and moderate CYP3A4 inhibitors. If coadministration cannot be avoided, dose reductions are required. See full monograph for dosing recommendations. Consider therapy modification
Terlipressin: May enhance the bradycardic effect of Bradycardia-Causing Agents. Monitor therapy
Tetrahydrocannabinol: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Tetrahydrocannabinol. Monitor therapy
Tezacaftor and Ivacaftor: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Tezacaftor and Ivacaftor. Management: When combined with moderate CYP3A4 inhibitors, tezacaftor/ivacaftor should be given in the morning, every other day. Ivacaftor alone should be given in the morning, every other day on alternate days. Consider therapy modification
Ticagrelor: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Ticagrelor. Monitor therapy
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Tofacitinib: May enhance the bradycardic effect of Bradycardia-Causing Agents. Monitor therapy
Tofacitinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Tofacitinib. Monitor therapy
Tolvaptan: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Tolvaptan. Management: Jynarque dose requires adjustment when used with a moderate CYP3A4 inhibitor. See labeling or full interaction monograph for specific recommendations. Use of Samsca with moderate CYP3A4 ihibitors should generally be avoided. Consider therapy modification
Trabectedin: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Trabectedin. Monitor therapy
Triazolam: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Triazolam. Management: Consider triazolam dose reduction in patients receiving concomitant moderate CYP3A4 inhibitors. Consider therapy modification
Ubrogepant: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Ubrogepant. Management: Use an initial ubrogepant dose of 50 mg and avoid a second dose for 24 hours when used with moderate CYP3A4 inhibitors. Consider therapy modification
Udenafil: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Udenafil. Monitor therapy
Ulipristal: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Ulipristal. Management: This is specific for when ulipristal is being used for signs/symptoms of uterine fibroids (Canadian indication). When ulipristal is used as an emergency contraceptive, patients receiving this combination should be monitored for ulipristal toxicity. Avoid combination
Venetoclax: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Venetoclax. Management: Reduce the venetoclax dose by at least 50% in patients requiring these combinations. Consider therapy modification
Vilazodone: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Vilazodone. Monitor therapy
Vindesine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Vindesine. Monitor therapy
Yohimbine: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Zanubrutinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Zanubrutinib. Management: Decrease the zanubrutinib dose to 80 mg twice daily during coadministration with a moderate CYP3A4 inhibitor. Further dose adjustments may be required for zanubrutinib toxicities, refer to prescribing information for details. Consider therapy modification
Zopiclone: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Zopiclone. Management: The starting adult dose of zopiclone should not exceed 3.75 mg if combined with a moderate CYP3A4 inhibitor. Monitor patients for signs and symptoms of zopiclone toxicity if these agents are combined. Consider therapy modification
Zuclopenthixol: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Zuclopenthixol. Monitor therapy
Adverse Reactions
Frequencies represent ranges for various dosage forms. Patients with impaired ventricular function and/or conduction abnormalities may have higher incidence of adverse reactions.
>10%: Cardiovascular: Peripheral edema (5% to 15%)
1% to 10%:
Cardiovascular: Lower extremity edema (5% to 8%), bradycardia (3% to 4%), first-degree atrioventricular block (3% to 4%), hypotension (3% to 4%), edema (2% to 3%), vasodilation (2% to 3%), extrasystoles (2%), palpitations (1% to 2%), angina pectoris (<2%), bundle branch block (<2%), cardiac failure (<2%), complete atrioventricular block (<2%), ECG abnormality (<2%), second degree atrioventricular block (<2%), syncope (<2%), tachycardia (<2%), ventricular premature contractions (<2%), cardiac arrhythmia (1%)
Central nervous system: Dizziness (2% to 10%), headache (2% to 8%), pain (6%), fatigue (5%), nervousness (2%), abnormal dreams (<2%), abnormal gait (<2%), amnesia (<2%), depression (<2%), drowsiness (<2%), hallucination (<2%), insomnia (<2%), paresthesia (<2%), personality changes (<2%)
Dermatologic: Skin rash (1% to 2%), pruritus (<2%), skin photosensitivity (<2%)
Endocrine & metabolic: Gout (1% to 2%), albuminuria (<2%), gynecomastia (<2%), hyperglycemia (<2%), hyperuricemia (<2%), increased lactate dehydrogenase (<2%), increased thirst (<2%), weight gain (<2%)
Gastrointestinal: Dyspepsia (1% to 6%), abdominal enlargement (2%), nausea (2%), diarrhea (1% to 2%), anorexia (<2%), constipation (<2%), dysgeusia (<2%), vomiting (<2%), xerostomia (<2%)
Genitourinary: Impotence (2%), crystalluria (<2%), nocturia (<2%), sexual difficulty (<2%)
Hematologic & oncologic: Petechia (<2%)
Hepatic: Increased serum alanine aminotransferase (<2%), increased serum alkaline phosphatase (<2%), increased serum aspartate transaminase (<2%)
Hypersensitivity: Hypersensitivity reaction (<2%)
Infection: Infection (1% to 6%)
Local: Burning sensation at injection site (≤4%), itching at injection site (≤4%)
Neuromuscular & skeletal: Asthenia (1% to 4%), myalgia (2%), increased creatine phosphokinase in blood specimen (<2%), muscle cramps (<2%), neck stiffness (<2%), osteoarthritis (<2%), tremor (<2%)
Ophthalmic: Conjunctivitis (2%), amblyopia (<2%), eye irritation (<2%)
Otic: Tinnitus (<2%)
Renal: Polyuria (<2%)
Respiratory: Pharyngitis (6%), dyspnea (1% to 6%), bronchitis (1% to 4%), flu-like symptoms (2%), cough (1% to 2%), paranasal sinus congestion (1% to 2%), epistaxis (<2%), rhinitis (<2%)
<1%: Atrial flutter, chest pain, sinus node dysfunction, urticaria, ventricular fibrillation, ventricular tachycardia
Frequency not defined: Hepatic: Hepatic injury, increased serum bilirubin
Postmarketing: Acute generalized exanthematous pustulosis, alopecia, angioedema, asystole, cutaneous lupus erythematosus (Crowson 1995; Srivastava 2003), erythema multiforme, exfoliative dermatitis, extrapyramidal reaction, gingival hyperplasia, hemolytic anemia, hypersensitivity angiitis, leukopenia, myopathy, prolonged bleeding time, purpuric disease, retinopathy, Stevens-Johnson syndrome, thrombocytopenia, toxic epidermal necrolysis
Warnings/Precautions
Concerns related to adverse effects:
- Conduction abnormalities: May cause first-, second-, and third-degree AV block or sinus bradycardia; risk increases with agents known to slow cardiac conduction.
- Dermatologic reactions: Transient dermatologic reactions have been observed with use; if reaction persists, discontinue. Stevens-Johnson syndrome, toxic epidermal necrolysis, erythema multiforme, and/or exfoliative dermatitis have been reported.
- Hepatic effects: Mild elevations of transaminases with and without concomitant elevation in alkaline phosphatase and bilirubin have been observed and frequently resolve spontaneously. Significant elevations in hepatic transaminases (eg, alkaline phosphatase, LDH, AST, ALT) and signs of acute hepatic injury have also been observed 1 to 8 weeks after therapy initiation and have been reversible upon discontinuation.
- Hypotension/syncope: Symptomatic hypotension with or without syncope can rarely occur; blood pressure must be lowered at a rate appropriate for the patient's clinical condition.
Disease-related concerns:
- Accessory bypass tract (eg, Wolff-Parkinson-White [WPW] syndrome): During an episode of atrial fibrillation or flutter in patients with an accessory bypass tract or preexcitation syndrome, use has been associated with increased anterograde conduction down the accessory pathway leading to ventricular fibrillation; avoid use in such patients (ACLS [Neumar 2010]; AHA/ACC/HRS [January 2014]).
- Hepatic impairment: Use with caution in patients with hepatic impairment.
- Left ventricular dysfunction: Use with caution in left ventricular dysfunction; due to negative inotropic effects, may exacerbate condition. Avoid use in patients with heart failure due to lack of benefit and/or worse outcomes with calcium channel blockers in general (ACCF/AHA [Yancy 2013]).
- Renal impairment: Use with caution in patients with renal impairment.
Concurrent drug therapy:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Other warnings/precautions:
- Appropriate use: IV: Unless otherwise contraindicated, appropriate vagal maneuvers should be attempted prior to administration of IV diltiazem. Use with caution in patients hemodynamically compromised; continuously monitor ECG and blood pressure during administration (especially during continuous IV infusion). Initial use should be, if possible, in a setting where monitoring and resuscitation equipment, including DC cardioversion/defibrillation, are present.
Monitoring Parameters
Liver function tests, kidney function, blood pressure, ECG, heart rate; consult individual institutional policies and procedures. Ventricular rate control in patients with atrial fibrillation or flutter: Patients who respond, usually have at least a 20% decrease in ventricular response rate or a rate <100 beats/minute.
Hypertension: The 2017 Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults (ACC/AHA [Whelton 2017]):
Confirmed hypertension and known CVD or 10-year ASCVD risk ≥10%: Target blood pressure <130/80 mm Hg is recommended.
Confirmed hypertension without markers of increased ASCVD risk: Target blood pressure <130/80 mm Hg may be reasonable.
Diabetes and hypertension: The American Diabetes Association (ADA) guidelines (ADA 2019):
Patients 18 to 65 years of age, without ASCVD, and 10-year ASCVD risk <15%: Target blood pressure <140/90 mm Hg is recommended.
Patients 18 to 65 years of age and known ASCVD or 10-year ASCVD risk >15%: Target blood pressure <130/80 mm Hg may be appropriate if it can be safely attained.
Patients >65 years of age (healthy or complex/intermediate health): Target blood pressure <140/90 mm Hg is recommended.
Patients >65 years of age (very complex/poor health): Target blood pressure <150/90 mm Hg is recommended.
Pregnancy
Pregnancy Risk Factor
C
Pregnancy Considerations
Adverse events have been observed in animal reproduction studies.
Chronic maternal hypertension may increase the risk of birth defects, low birth weight, preterm delivery, stillbirth, and neonatal death. Actual fetal/neonatal risks may be related to duration and severity of maternal hypertension. Untreated hypertension may also increase the risks of adverse maternal outcomes, including gestational diabetes, myocardial infarction, preeclampsia, stroke, and delivery complications (ACOG 203 2019).
Calcium channel blockers may be used to treat hypertension in pregnant women; however, agents other than diltiazem are more commonly used (ACOG 203 2019; ESC [Regitz-Zagrosek 2018]). Females with preexisting hypertension may continue their medication during pregnancy unless contraindications exist (ESC [Regitz-Zagrosek 2018]).
Patient Education
What is this drug used for?
- It is used to treat high blood pressure.
- It is used to treat a type of long-term chest pain (stable chest pain) in some people.
- It is used to treat certain types of abnormal heartbeats.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Headache
- Fatigue
- Loss of strength and energy
- Injection site irritation
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin or eyes
- Severe dizziness
- Passing out
- Slow heartbeat
- Abnormal heartbeat
- Heart problems like cough or shortness of breath that is new or worse, swelling of the ankles or legs, abnormal heartbeat, weight gain of more than five pounds in 24 hours, dizziness, or passing out
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.