Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Solution, Injection, as sulfate:
Generic: 50 mg/mL (1 mL [DSC])
Solution, Injection, as sulfate [preservative free]:
Generic: 50 mg/mL (1 mL)
Solution, Intravenous, as sulfate:
Akovaz: 50 mg/mL (1 mL)
Generic: 50 mg/mL (1 mL)
Solution, Intravenous, as sulfate [preservative free]:
Generic: 50 mg/mL (1 mL)
Pharmacology
Mechanism of Action
Releases tissue stores of norepinephrine and thereby produces an alpha- and beta-adrenergic stimulation; longer-acting and less potent than epinephrine
Pharmacokinetics/Pharmacodynamics
Absorption
IV: Rapid, complete
Metabolism
Minimally hepatic; metabolites include p-hydroxyephedrine, p-hydroxynorephedrine, norephedrine
Excretion
Urine (primarily unchanged; dependent upon urinary pH with greatest excretion in acid pH)
Onset of Action
IM: Within 10 to 20 minutes.
Duration of Action
Pressor/cardiac effects: SubQ: 1 hour
Half-Life Elimination
Dependent upon urinary pH; Urine pH 5: ~3 hours; Urine pH 6.3: ~6 hours
Use in Specific Populations
Special Populations: Renal Function Impairment
Elimination half-life may be increased.
Use: Labeled Indications
Hypotension, anesthesia-induced: Treatment of anesthesia-induced hypotension
Note: The use of ephedrine for the treatment of acute bronchospasm, Stokes-Adams syndrome (ie, presyncope/syncope) with complete heart block, narcolepsy, depression, or myasthenia gravis has fallen out of favor given the availability of more effective agents for these conditions.
Use: Off Label
Postoperative nausea and vomiting (prevention)yesb
Data from two randomized controlled studies suggests that patients given post-operative ephedrine had lower postoperative nausea and vomiting (PONV) scores early in the post-operative period without significant hemodynamic changes Rothenberg 1991, Hagemann 2000. Additional trials may be necessary to further define the role of ephedrine in this setting.
Based on the Society of Ambulatory Anesthesia (SAMBA) guidelines for the management of PONV, ephedrine is a recommended pharmacologic antiemetic among other agents for prophylaxis in adults at moderate to severe risk for PONV. Other agents include 5HT3 antagonists (eg, ondansetron, granisetron), steroids (eg, dexamethasone), phenothiazines (eg, promethazine, prochlorperazine), butyrophenones (eg, droperidol, haloperidol), antihistamines (eg, dimenhydrinate), and anticholinergics (eg, transdermal scopolamine) SAMBA [Gan 2007].
Contraindications
Hypersensitivity to ephedrine, other sympathomimetics, or any component of the formulation; angle-closure glaucoma; coadministration with myocardial sensitizing anesthetics (cyclopropane or halothane).
Dosage and Administration
Dosing: Adult
Hypotension, anesthesia-induced: IV: 5 to 25 mg/dose slow IV push; repeat as needed to maintain blood pressure (maximum total dose: 50 mg)
Postoperative nausea and vomiting (prevention) (off-label use): IM: 0.5 mg/kg at the end of surgery (Hagemann 2000; SAMBA [Gan 2007])
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Approved ages and uses in pediatric population may vary with formulations; consult product specific labeling.
Hypotension, anesthesia-induced: Use the smallest effective dose:
Infants, Children, and Adolescents ≤15 years: Limited data available: Slow IV push: 0.1 to 0.3 mg/kg/dose, repeat as needed to maintain blood pressure; maximum dose: 25 mg/dose; maximum total dose: 50 mg (Atchabahian 2013; Taguchi 1996)
Adolescents >15 years: IV: 5 to 25 mg/dose slow IV push repeated as needed to maintain blood pressure; maximum total dose: 50 mg
Reconstitution
IV: Dilute to 5 or 10 mg/mL with D5W or NS.
IM: For PONV (off-label use), dilute with NS (Hagemann 2000).
Administration
Administer diluted solution as a slow IV push. For PONV (off-label use), administer IM (Hagemann 2000; SAMBA [Gan 2007]).
Storage
Store at room temperature; protect from light.
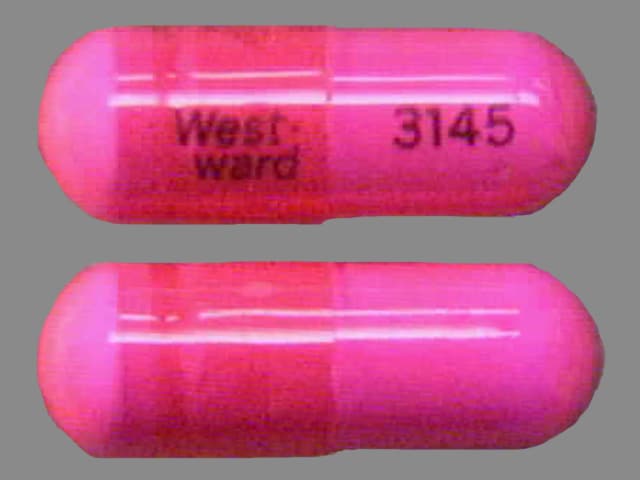
EPHEDrine (Systemic) Images
Drug Interactions
Alkalinizing Agents: May increase the serum concentration of Alpha-/Beta-Agonists (Indirect-Acting). Monitor therapy
Alpha1-Blockers: May diminish the vasoconstricting effect of Alpha-/Beta-Agonists. Similarly, Alpha-/Beta-Agonists may antagonize Alpha1-Blocker vasodilation. Monitor therapy
AtoMOXetine: May enhance the hypertensive effect of Sympathomimetics. AtoMOXetine may enhance the tachycardic effect of Sympathomimetics. Monitor therapy
Atropine (Systemic): May enhance the therapeutic effect of EPHEDrine (Systemic). Monitor therapy
Benzylpenicilloyl Polylysine: Alpha-/Beta-Agonists may diminish the diagnostic effect of Benzylpenicilloyl Polylysine. Management: Consider use of a histamine skin test as a positive control to assess a patient's ability to mount a wheal and flare response. Consider therapy modification
Bretylium: May enhance the therapeutic effect of Alpha-/Beta-Agonists (Direct-Acting). Monitor therapy
Cannabinoid-Containing Products: May enhance the tachycardic effect of Sympathomimetics. Exceptions: Cannabidiol. Monitor therapy
Carbonic Anhydrase Inhibitors: May increase the serum concentration of Alpha-/Beta-Agonists (Indirect-Acting). Monitor therapy
Cardiac Glycosides: EPHEDrine (Systemic) may enhance the arrhythmogenic effect of Cardiac Glycosides. Monitor therapy
Chloroprocaine: May enhance the hypertensive effect of Alpha-/Beta-Agonists. Monitor therapy
CloNIDine: May enhance the therapeutic effect of EPHEDrine (Systemic). Monitor therapy
CloZAPine: May diminish the therapeutic effect of Alpha-/Beta-Agonists. Monitor therapy
Cocaine (Topical): May enhance the hypertensive effect of Sympathomimetics. Management: Consider alternatives to use of this combination when possible. Monitor closely for substantially increased blood pressure or heart rate and for any evidence of myocardial ischemia with concurrent use. Consider therapy modification
Doxofylline: Sympathomimetics may enhance the adverse/toxic effect of Doxofylline. Monitor therapy
Droxidopa: EPHEDrine (Systemic) may enhance the hypertensive effect of Droxidopa. Monitor therapy
Ergot Derivatives: May enhance the hypertensive effect of Alpha-/Beta-Agonists. Ergot Derivatives may enhance the vasoconstricting effect of Alpha-/Beta-Agonists. Exceptions: Ergoloid Mesylates; Nicergoline. Avoid combination
FentaNYL: Alpha-/Beta-Agonists (Indirect-Acting) may decrease the serum concentration of FentaNYL. Specifically, fentanyl nasal spray serum concentrations may decrease and onset of effect may be delayed. Monitor therapy
Guanethidine: May enhance the arrhythmogenic effect of Sympathomimetics. Guanethidine may enhance the hypertensive effect of Sympathomimetics. Monitor therapy
Hyaluronidase: May enhance the vasoconstricting effect of Alpha-/Beta-Agonists. Management: Avoid the use of hyaluronidase to enhance dispersion or absorption of alpha-/beta-agonists. Use of hyaluronidase for other purposes in patients receiving alpha-/beta-agonists may be considered as clinically indicated. Consider therapy modification
Inhalational Anesthetics: EPHEDrine (Systemic) may enhance the arrhythmogenic effect of Inhalational Anesthetics. Avoid combination
Iobenguane Radiopharmaceutical Products: Alpha-/Beta-Agonists (Indirect-Acting) may diminish the therapeutic effect of Iobenguane Radiopharmaceutical Products. Management: Discontinue all drugs that may inhibit or interfere with catecholamine transport or uptake for at least 5 biological half-lives before iobenguane administration. Do not administer these drugs until at least 7 days after each iobenguane dose. Avoid combination
Linezolid: May enhance the hypertensive effect of Sympathomimetics. Management: Reduce initial doses of sympathomimetic agents, and closely monitor for enhanced pressor response, in patients receiving linezolid. Specific dose adjustment recommendations are not presently available. Consider therapy modification
Monoamine Oxidase Inhibitors: May enhance the hypertensive effect of Alpha-/Beta-Agonists (Indirect-Acting). While linezolid is expected to interact via this mechanism, management recommendations differ from other monoamine oxidase inhibitors. Refer to linezolid specific monographs for details. Exceptions: Linezolid. Avoid combination
Oxytocin: May enhance the hypertensive effect of EPHEDrine (Systemic). Monitor therapy
Propofol: May enhance the therapeutic effect of EPHEDrine (Systemic). Monitor therapy
QuiNIDine: EPHEDrine (Systemic) may diminish the therapeutic effect of QuiNIDine. QuiNIDine may diminish the therapeutic effect of EPHEDrine (Systemic). Monitor therapy
Rocuronium: EPHEDrine (Systemic) may enhance the therapeutic effect of Rocuronium. Monitor therapy
Serotonin/Norepinephrine Reuptake Inhibitors: May enhance the tachycardic effect of Alpha-/Beta-Agonists. Serotonin/Norepinephrine Reuptake Inhibitors may enhance the vasopressor effect of Alpha-/Beta-Agonists. Consider therapy modification
Solriamfetol: Sympathomimetics may enhance the hypertensive effect of Solriamfetol. Monitor therapy
Spironolactone: May diminish the vasoconstricting effect of Alpha-/Beta-Agonists. Monitor therapy
Sympathomimetics: May enhance the adverse/toxic effect of other Sympathomimetics. Monitor therapy
Tedizolid: May enhance the hypertensive effect of Sympathomimetics. Tedizolid may enhance the tachycardic effect of Sympathomimetics. Monitor therapy
Tricyclic Antidepressants: May enhance the vasopressor effect of Alpha-/Beta-Agonists. Management: Avoid, if possible, the use of alpha-/beta-agonists in patients receiving tricyclic antidepressants. If combined, monitor for evidence of increased pressor effects and consider reductions in initial dosages of the alpha-/beta-agonist. Consider therapy modification
Urinary Acidifying Agents: May decrease the serum concentration of Alpha-/Beta-Agonists (Indirect-Acting). Monitor therapy
Test Interactions
Can cause a false-positive amphetamine EMIT assay
Adverse Reactions
Frequency not defined.
Cardiovascular: Angina pectoris, bradycardia, cardiac arrhythmia, hypertension, palpitations, pulse irregularity, tachycardia, ventricular ectopy, visceral vasoconstriction (renal)
Central nervous system: Anxiety, confusion, delirium, dizziness, hallucination, headache, insomnia, intracranial hemorrhage, nervousness, precordial pain, restlessness, tension, vertigo
Dermatologic: Diaphoresis, pallor
Gastrointestinal: Anorexia, nausea, vomiting
Genitourinary: Dysuria, oliguria, urinary retention (males with prostatism)
Neuromuscular & skeletal: Tremor, vesicle sphincter spasm, weakness
Respiratory: Dyspnea
Miscellaneous: Tachyphylaxis
Warnings/Precautions
Concerns related to adverse effects:
- Cardiovascular effects: May cause hypertension resulting in intracranial hemorrhage. May also induce anginal pain in patients with coronary insufficiency or ischemic heart disease and induce potentially fatal arrhythmias in patients with heart disease or who are receiving drugs that sensitize the myocardium.
- Urine output: Constriction of renal blood vessels may occur, decreasing urine output.
Disease-related concerns:
- Cardiovascular disease: Ephedrine should not ordinarily be used where vasopressor drugs may be contraindicated, such as hypertension and other cardiovascular disorders (eg angina pectoris, coronary artery disease, arrhythmias); use with caution.
- Diabetes: Ephedrine should not ordinarily be used in cases where vasopressor drugs may be contraindicated, such as diabetes; use with caution.
- Prostatic hyperplasia/urinary stricture: Use with caution in patients with prostatic hyperplasia and/or urinary stricture.
- Renal impairment: Use with caution in patients with renal impairment; increased elimination half-life may occur. Carefully monitor patients with renal impairment for adverse reactions.
- Thyroid dysfunction: Ephedrine should not ordinarily be used where vasopressor drugs may be contraindicated, such as thyrotoxicosis. Use with caution in patients with thyroid dysfunction.
- Vasomotor symptoms: Use with caution in patients with unstable vasomotor symptoms.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Elderly: Use with caution in the elderly.
Dosage form specific issues:
- Injectable: Blood volume depletion should be corrected before IV therapy is instituted.
Other warnings/precautions:
- Bronchodilator use: Avoid as a bronchodilator; ephedrine is generally not used as a bronchodilator since other beta2 agonists are less toxic.
- Long-term use: Prolonged use may cause anxiety and symptoms of paranoid schizophrenia (eg, tachycardia, poor nutrition and hygiene, fever, cold sweat and dilated pupils).
- Tolerance: Tachyphylaxis and tolerance may develop with repeated, prolonged, or excessive administration; temporary cessation of therapy restores its effectiveness.
Monitoring Parameters
Blood pressure, pulse, respiratory symptoms; monitor patients with renal impairment for adverse reactions.
Pregnancy
Pregnancy Risk Factor
C
Pregnancy Considerations
Animal reproduction studies have not been conducted. Ephedrine crosses the placenta (Hughes, 1985). Ephedrine injection is used at delivery for the prevention and/or treatment of maternal hypotension associated with spinal anesthesia in women undergoing cesarean section (ASA, 2007). Serious postpartum hypertension and possibly stroke may occur if administered with oxytocic medications. Metabolic acidosis has been reported in neonates following maternal use of ephedrine; monitor.
Patient Education
What is this drug used for?
- It is used to treat low blood pressure.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Sweating a lot
- Agitation
- Trouble sleeping
- Nausea
- Vomiting
- Lack of appetite
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Severe headache
- Vision changes
- Chest pain
- Fast heartbeat
- Slow heartbeat
- Abnormal heartbeat
- Severe dizziness
- Passing out
- Severe anxiety
- Unable to pass urine
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.