Boxed Warning
Endometrial cancer:
There is an increased risk of endometrial cancer in a woman with a uterus who uses unopposed estrogens. Adding a progestin to estrogen therapy has been shown to reduce the risk of endometrial hyperplasia, which may be a precursor to endometrial cancer. Adequate diagnostic measures, including directed or random endometrial sampling when indicated, should be taken to rule out malignancy in all cases of undiagnosed persistent or recurring abnormal genital bleeding.
Cardiovascular disease:
Estrogen-alone therapy should not be used for the prevention of cardiovascular disease. The Women's Health Initiative (WHI) estrogen-alone substudy reported increased risks of stroke and deep vein thrombosis (DVT) in postmenopausal women (50 to 79 years of age) during 7.1 years of treatment with daily oral conjugated estrogens (0.625 mg) alone, relative to placebo.
Estrogen plus progestin therapy should not be used for the prevention of cardiovascular disease. The WHI estrogen plus progestin substudy reported increased risks of DVT, pulmonary embolism (PE), stroke, and myocardial infarction (MI) in postmenopausal women (50 to 79 years of age) during 5.6 years of treatment with daily oral conjugated estrogens (0.625 mg) combined with medroxyprogesterone acetate (2.5 mg), relative to placebo.
Breast cancer:
The Women's Health Initiative (WHI) estrogen plus progestin substudy demonstrated an increased risk of invasive breast cancer
Dementia:
Estrogen-alone therapy should not be used for the prevention of dementia. The WHI Memory Study (WHIMS) estrogen-alone ancillary study of the WHI reported an increased risk of developing probable dementia in postmenopausal women 65 years and older during 5.2 years of treatment with daily conjugated estrogens (0.625 mg) alone, relative to placebo. It is unknown whether this finding applies to younger postmenopausal women.
Estrogen plus progestin therapy should not be used for the prevention of dementia. The WHIMS estrogen plus progestin ancillary study of the WHI reported an increased risk of developing probable dementia in postmenopausal women 65 years or older during 4 years of treatment with daily conjugated estrogens (0.625 mg) combined with medroxyprogesterone acetate (2.5 mg), relative to placebo. It is unknown whether this finding applies to younger postmenopausal women.
Risk vs benefits:
In the absence of comparable data, these risks should be assumed to be similar for other doses of conjugated estrogens (with or without medroxyprogesterone acetate) and other dosage forms of estrogens (with or without progestins). Estrogens with or without progestins should be prescribed at the lowest effective doses and for the shortest duration consistent with treatment goals and risks for the individual woman.
Secondary exposure (Evamist):
Breast budding and breast masses in prepubertal females and gynecomastia and breast masses in prepubertal males have been reported following unintentional secondary exposure to Evamist by women using this product. In most cases, the condition resolved with removal of Evamist exposure. Women should ensure that children do not come into contact with the site(s) where Evamist is applied. Advise patients to strictly adhere to recommended instructions for use.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Gel, Transdermal:
Divigel: 0.25 mg/0.25 g (1 ea); 0.5 mg/0.5 g (1 ea); 0.75 mg/0.75 g (1 ea); 1 mg/g (1 g) [contains propylene glycol, trolamine (triethanolamine)]
Divigel: 1.25 mg/1.25 g (1.25 g) [contains alcohol, usp, propylene glycol, trolamine (triethanolamine)]
Elestrin: 0.06% (26 g) [contains edetate disodium, propylene glycol, trolamine (triethanolamine)]
Estrogel: 0.06% (50 g) [contains alcohol, usp, trolamine (triethanolamine)]
Oil, Intramuscular, as cypionate:
Depo-Estradiol: 5 mg/mL (5 mL) [contains chlorobutanol (chlorobutol)]
Oil, Intramuscular, as valerate:
Delestrogen: 10 mg/mL (5 mL) [contains chlorobutanol (chlorobutol), sesame oil]
Delestrogen: 20 mg/mL (5 mL); 40 mg/mL (5 mL) [contains benzyl alcohol, benzyl benzoate, castor oil (ricine oil)]
Generic: 20 mg/mL (5 mL); 40 mg/mL (5 mL)
Patch Twice Weekly, Transdermal:
Alora: 0.025 mg/24 hr (1 ea, 8 ea); 0.05 mg/24 hr (1 ea, 8 ea); 0.075 mg/24 hr (1 ea, 8 ea); 0.1 mg/24 hr (1 ea, 8 ea)
Dotti: 0.025 mg/24 hr (1 ea, 8 ea); 0.0375 mg/24 hr (1 ea, 8 ea); 0.05 mg/24 hr (1 ea, 8 ea); 0.075 mg/24 hr (1 ea, 8 ea); 0.1 mg/24 hr (1 ea, 8 ea)
Minivelle: 0.025 mg/24 hr (1 ea, 8 ea); 0.0375 mg/24 hr (1 ea, 8 ea); 0.05 mg/24 hr (1 ea, 8 ea); 0.075 mg/24 hr (1 ea, 8 ea); 0.1 mg/24 hr (1 ea, 8 ea)
Vivelle-Dot: 0.025 mg/24 hr (1 ea, 8 ea); 0.0375 mg/24 hr (1 ea, 8 ea); 0.05 mg/24 hr (1 ea, 8 ea); 0.075 mg/24 hr (1 ea, 8 ea); 0.1 mg/24 hr (1 ea, 8 ea)
Generic: 0.025 mg/24 hr (1 ea, 8 ea); 0.0375 mg/24 hr (1 ea, 8 ea); 0.05 mg/24 hr (1 ea, 8 ea); 0.075 mg/24 hr (1 ea, 8 ea); 0.1 mg/24 hr (1 ea, 8 ea)
Patch Weekly, Transdermal:
Climara: 0.025 mg/24 hr (4 ea); 0.0375 mg/24 hr (4 ea); 0.05 mg/24 hr (1 ea, 4 ea); 0.06 mg/24 hr (4 ea); 0.075 mg/24 hr (4 ea); 0.1 mg/24 hr (1 ea, 4 ea)
Menostar: 14 mcg/24 hr (4 ea)
Generic: 0.025 mg/24 hr (1 ea, 4 ea); 0.0375 mg/24 hr (1 ea, 4 ea); 0.05 mg/24 hr (1 ea, 4 ea); 0.06 mg/24 hr (1 ea, 4 ea); 0.075 mg/24 hr (1 ea, 4 ea); 0.1 mg/24 hr (1 ea, 4 ea)
Ring, Vaginal, as acetate:
Femring: 0.05 mg/24 hr (1 ea); 0.1 mg/24 hr (1 ea)
Solution, Transdermal:
Evamist: 1.53 mg/spray (8.1 mL)
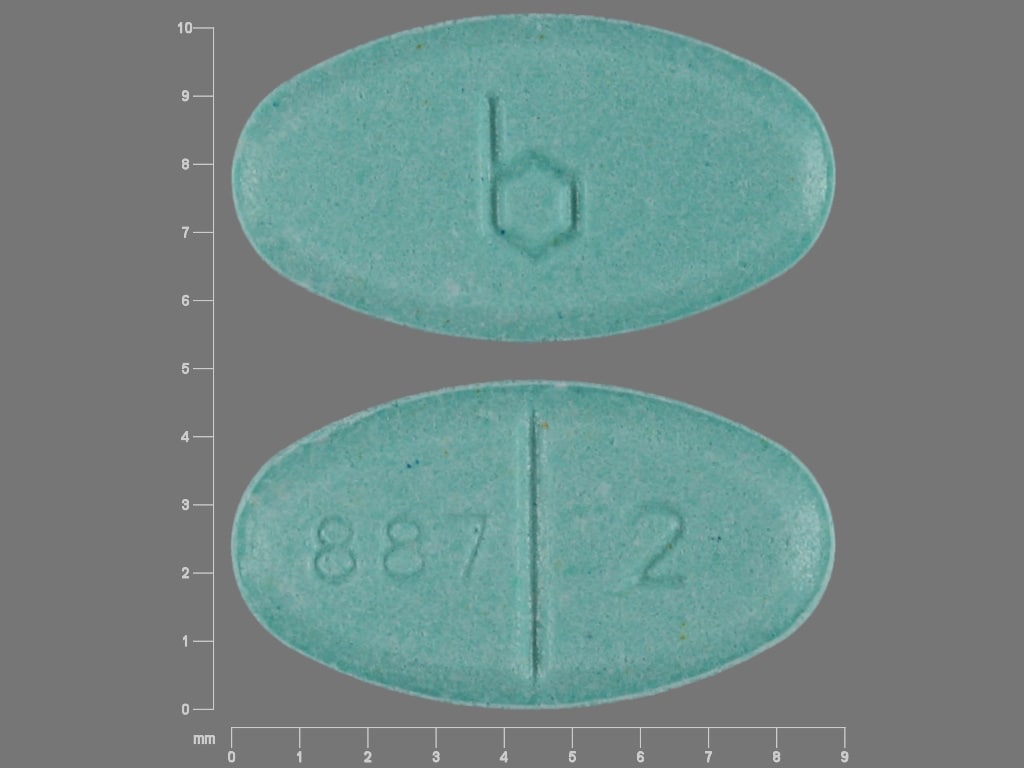
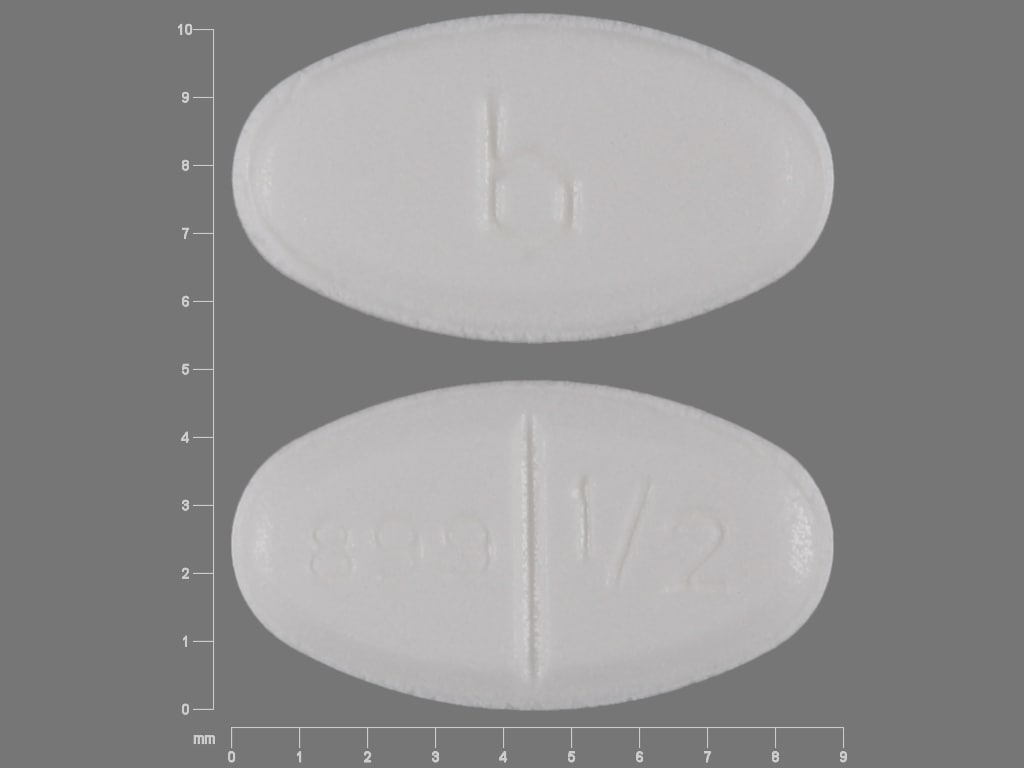
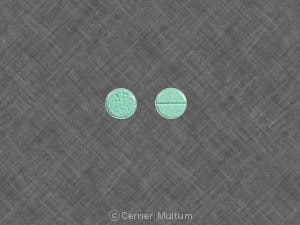
Tablet, Oral:
Estrace: 0.5 mg, 1 mg, 2 mg [scored]
Generic: 0.5 mg, 1 mg, 2 mg
Pharmacology
Mechanism of Action
Estrogens are responsible for the development and maintenance of the female reproductive system and secondary sexual characteristics. Estradiol is the principle intracellular human estrogen and is more potent than estrone and estriol at the receptor level; it is the primary estrogen secreted prior to menopause. Following menopause, estrone and estrone sulfate are more highly produced. Estrogens modulate the pituitary secretion of gonadotropins, luteinizing hormone, and follicle-stimulating hormone through a negative feedback system; estrogen replacement reduces elevated levels of these hormones in postmenopausal women.
Pharmacokinetics/Pharmacodynamics
Absorption
Well absorbed from the gastrointestinal tract, mucous membranes, and the skin. Average serum estradiol concentrations (Cavg) vary by product
Injection: Estradiol valerate and estradiol cypionate are absorbed over several weeks following IM injection
Topical:
Alora: Cavg: 41 to 98 pg/mL
Climara: Cavg: 22 to 106 pg/mL
Divigel: Cavg: 9.8 to 30.5 pg/mL
Elestrin: Cavg: 15.4 to 39.2 pg/mL; Exposure increased by 55% with application of sunscreen 10 minutes prior to dose
Estrogel: Cavg on day 14 of therapy: 28.3 pg/mL. Cmax of estradiol is altered by repeated daily application (for 7 days) of sunscreen (decreased by 16%) or lotion (increased by 73%) when applied 1 hour after the dose.
Evamist: Cavg: 19.6 to 30.9 pg/mL
Menostar: Cavg: 13.7 pg/mL
Vivelle-Dot: Cavg: 34 to 104 pg/mL
Vaginal (Femring): Rapid during the first hour following application, then declines to a steady rate over 3 months; Cavg: 40.6 to 76 pg/mL
Distribution
Widely distributed; high concentrations in the sex hormone target organs
Metabolism
Hepatic; partial metabolism via CYP3A4 enzymes; estradiol is reversibly converted to estrone and estriol; oral estradiol also undergoes enterohepatic recirculation by conjugation in the liver, followed by excretion of sulfate and glucuronide conjugates into the bile, then hydrolysis in the intestine and estrogen reabsorption. Sulfate conjugates are the primary form found in postmenopausal women. With transdermal application, less estradiol is metabolized leading to higher circulating concentrations of estradiol and lower concentrations of estrone and conjugates.
Excretion
Primarily urine (as estradiol, estrone, estriol and their glucuronide and sulfate conjugates)
Protein Binding
Bound to sex hormone-binding globulin and albumin
Use: Labeled Indications
Breast cancer, metastatic: Treatment of metastatic breast cancer (palliation) in appropriately selected men and postmenopausal women.
Hypoestrogenism (female): Treatment of hypoestrogenism due to hypogonadism, castration, or primary ovarian failure
Osteoporosis prevention (female): Prevention of postmenopausal osteoporosis
Limitations of use: For use only in women at significant risk of postmenopausal osteoporosis; consider use of nonestrogen medications.
Prostate cancer, advanced: Treatment of androgen dependent advanced prostatic cancer (palliation)
Vasomotor symptoms associated with menopause: Treatment of moderate to severe vasomotor symptoms associated with menopause.
Vulvar and vaginal atrophy associated with menopause: Treatment of moderate to severe vulvar and vaginal atrophy associated with menopause.
Limitations of use: When used solely for the treatment of vulvar and vaginal atrophy, topical vaginal products should be considered.
Note: The International Society for the Study of Women’s Sexual Health and The North American Menopause Society have endorsed the term genitourinary syndrome of menopause (GSM) as new terminology for vulvovaginal atrophy. The term GSM encompasses all genital and urinary signs and symptoms associated with a loss of estrogen due to menopause Portman 2014.
Use: Off Label
Functional hypothalamic amenorrhea with low bone density (young adult females)yes
Based on the Endocrine Society clinical practice guideline for the diagnosis and treatment of functional hypothalamic amenorrhea (FHA), short-term hormone replacement with transdermal estradiol (with cyclic oral progestin) is a suggested therapy in adolescents and women with low bone density and/or evidence of skeletal fragility who have not had a resumption of menses after 6 to 12 months of nutritional (calorie optimization; calcium, vitamin D, other nutrient supplementation), psychological, and/or modified exercise interventions. However, if nutritional deficits persist, hormone replacement may not protect bone health.
Hormone therapy for transgender females (male-to-female)yes
Based on the Endocrine Society guidelines for the endocrine treatment of gender dysphoric/gender incongruent persons, estradiol as monotherapy or combination therapy, is effective for elevating serum estradiol levels and suppressing serum testosterone levels into the normal range for females, resulting in decreased hair growth, muscle mass, sexual desire, sperm production, spontaneous erections, and testicular volume, as well as breast growth, male sexual dysfunction, redistribution of body fat, and skin and voice changes. In many cases, estrogen therapy will need to be augmented with a second compound to suppress androgen secretion, such as spironolactone or a gonadotropin hormone-releasing agonist ES [Hembree 2017].
Contraindications
Angioedema, anaphylactic reaction, or hypersensitivity to estradiol or any component of the formulation; undiagnosed abnormal genital bleeding; DVT or PE (current or history of); active or history of arterial thromboembolic disease (eg, stroke, MI); breast cancer (known, suspected or history of), except in appropriately selected patients being treated for metastatic disease; estrogen-dependent tumor (known or suspected); hepatic impairment or disease; known protein C, protein S, antithrombin deficiency or other known thrombophilic disorders; pregnancy (Note: Products approved for use only in postmenopausal women are not appropriate for use in pregnancy; use of some products is specifically contraindicated in the manufacturer's labeling).
Documentation of allergenic cross-reactivity for estrogens is limited. However, because of similarities in chemical structure and/or pharmacologic actions, the possibility of cross-sensitivity cannot be ruled out with certainty.
Canadian labeling: Additional contraindications (not in US labeling): Note: May be dosage form dependent (consult product labeling): Breastfeeding; endometrial hyperplasia; active thrombophlebitis; partial or complete loss of vision or diplopia due to ophthalmic vascular disease; presence or history of hepatic tumors (benign or malignant); porphyria; classical migraine.
Dosage and Administration
Dosing: Adult
General dosing guidelines: When treating symptoms of menopause, hormone therapy should be evaluated routinely for appropriate dose, duration, and route of administration for each individual patient based on treatment goals, risk factors, and overall health (NAMS 2017). Combined estrogen/progestin therapy is indicated for postmenopausal persons with a uterus to decrease the risk of endometrial cancer. Individuals who have had a hysterectomy generally do not need a progestin; however, one may be needed if there is a history of endometriosis. Adjust dose based on patient response.
Breast cancer, metastatic: Oral (Estrace): Males and postmenopausal females: 10 mg 3 times/day or (off-label dosing) postmenopausal women: 2 mg 3 times/day (Ellis 2009)
Hormone therapy for transgender females (male-to-female), monotherapy or combination therapy (off-label use) (ES [Hembree 2017]):
IM:
Cypionate: 2 to 10 mg every week
Valerate: 5 to 30 mg every 2 weeks
Oral: 2 to 6 mg/day
Transdermal: Apply 0.025 to 0.2 mg/day patch every 3 to 5 days. Note: Apply two 0.1 mg patches to create a 0.2 mg/day dose.
Note: Adjust dose with a goal of elevating serum estradiol levels and suppressing serum testosterone levels into the normal range for females.
Hypoestrogenism (female) due to hypogonadism, castration, or primary ovarian failure:
Oral (Estrace): 1 to 2 mg/day; titrate as necessary to control symptoms using minimal effective dose for maintenance therapy
IM: Valerate (Delestrogen): 10 to 20 mg every 4 weeks
Transdermal (Alora, Climara, Vivelle-Dot): Refer to transdermal product-specific dosing (below).
Hypoestrogenism (female) due to hypogonadism: IM: Cypionate (Depo-Estradiol): 1.5 to 2 mg monthly
Osteoporosis prevention (females):
Oral (Estrace): Lowest effective dose has not been determined; doses of at least 0.5 mg/day were used in clinical studies evaluating bone mineral density (NAMS 2017).
Transdermal (Alora, Climara, Menostar, Minivelle, Vivelle-Dot): Refer to transdermal product-specific dosing (below).
Prostate cancer, advanced:
IM: Valerate (Delestrogen): 30 mg or more every 1 to 2 weeks
Oral (Estrace): 1 to 2 mg 3 times/day
Vasomotor symptoms (moderate to severe) associated with menopause:
Oral (Estrace): 0.5 to 1 mg once daily (AACE [Goodman 2011]; ACOG 141 2014). Dosage range: 0.5 to 2 mg/day (ES [Stuenkel 2015]).
IM: Cypionate (Depo-Estradiol): 1 to 5 mg every 3 to 4 weeks
IM: Valerate (Delestrogen): 10 to 20 mg every 4 weeks
Topical gel:
Divigel: Initial: 0.25 g/day; adjust dose based on patient response
Elestrin: Initial: 0.87 g/day applied at the same time each day; adjust dose based on patient response.
EstroGel: 1.25 g/day applied at the same time each day
Topical spray (Evamist): Initial: One spray (1.53 mg) per day. Adjust dose based on patient response. Dosing range: 1 to 3 sprays per day.
Transdermal (Alora, Climara, Minivelle, Vivelle-Dot): Refer to transdermal product-specific dosing (below).
Vaginal ring (Femring): Initial: 0.05 mg intravaginally; following insertion, dose is released daily for 3 months. Usual dose: 0.05 mg to 0.1 mg intravaginally every 3 months.
Vulvar and vaginal atrophy (moderate to severe) associated with menopause:
IM: Valerate (Delestrogen): 10 to 20 mg every 4 weeks
Intravaginal: Vaginal ring (Femring): Initial: 0.05 mg intravaginally; following insertion, dose is released daily for 3 months. Usual dose: 0.05 mg to 0.1 mg intravaginally every 3 months.
Oral (Estrace): 0.5 to 1 mg/day (ACOG 141 2014)
Topical gel (EstroGel): 1.25 g/day applied at the same time each day
Transdermal (Alora, Climara, Vivelle-Dot): Refer to transdermal product-specific dosing (below).
Transdermal product-specific dosing:
Note: Indicated dose may be used continuously in patients without a uterus. Continuous or cyclic schedules (3 weeks on, 1 week off) may be used in women with a uterus (indication and product specific; refer to manufacturers labeling). When changing patients from oral to transdermal therapy, start transdermal patch 1 week after discontinuing oral hormone (may begin sooner if symptoms reappear within 1 week):
Hypoestrogenism (female) due to hypogonadism, castration, or primary ovarian failure: Adjust dose as necessary to control symptoms.
Alora: Initial: Initial: Apply 0.05 mg/day patch twice weekly.
Climara: Initial: Apply 0.025 mg/day patch once weekly.
Vivelle-Dot: Initial: Apply 0.025 mg/day patch twice weekly.
Functional hypothalamic amenorrhea with low bone density (adolescent and young adult female; off-label use): The Endocrine Society guidelines are unable to recommend an optimal dose due to insufficient data (Gordon 2017). Application of 0.1 mg/day patch twice weekly (with cyclic progesterone for endometrial protection) improved spine and hip bone mineral density (BMD) in adolescent girls (bone age ≥15 years) with anorexia nervosa-associated low BMD (Misra 2011).
Osteoporosis prevention (female):
Alora, Minivelle, Vivelle-Dot: Initial: Apply 0.025 mg/day patch twice weekly. Adjust dose as necessary.
Climara: Initial: Apply 0.025 mg/day patch once weekly; adjust dosage based on response to therapy.
Estradot [Canadian product]: There are no specific initial dosage recommendations provided in the manufacturer's labeling; individualize dose per clinical status, BMD status and 17-beta estradiol levels (maintain levels at 50 picogram/mL).
Menostar: Apply 0.014 mg/day patch once weekly. In women with a uterus, also administer a progestin for 14 days every 6 to 12 months.
Vasomotor symptoms associated with menopause: Note: Adjust dose as necessary.
Alora, Estradot [Canadian product]: Initial: Apply 0.05 mg/day patch twice weekly.
Climara: Initial: Apply 0.025 mg/day patch once weekly.
Minivelle, Vivelle-Dot: Initial: Apply 0.0375 mg/day patch twice weekly.
Oesclim [Canadian product]: Initial: Apply 0.025 to 0.05 mg/day patch twice weekly.
Vulvar and vaginal atrophy (moderate to severe) associated with menopause: Note: Adjust dose as necessary.
Alora: Initial: Apply 0.05 mg/day patch twice weekly.
Climara: Initial: Apply 0.025 mg/day patch once weekly.
Vivelle-Dot: Initial: Apply 0.0375 mg/day patch twice weekly.
Dosing: Geriatric
Note: Women >65 years of age should be assessed for benefits and risks of treatment; possible adjustments to safer lower-dose and/or route of administration should be considered (ACOG 565 2013; NAMS 2017). The Beers Criteria recommends avoiding systemic estrogen therapy in patients ≥65 years of age (independent of diagnosis or condition) (Beers Criteria [AGS 2019]).
Refer to adult dosing.
Dosing: Pediatric
Note: Estrasorb has been discontinued in the US for more than 1 year. Use lowest effective dose for shortest duration possible that is consistent with an individual's treatment goals and risks; all dosage needs to be adjusted based upon the patient's response.
Constitutional delay of growth and puberty (CDGP) (females): Limited data available: Children ≥12 years and Adolescents: Note: Begin with the lowest available dose and gradually increase. Obtain bone age every 6 months to avoid premature epiphyseal closure. If treatment continues beyond 1 year or breast growth is significant and has plateaued or breakthrough bleeding occurs, add cyclic progesterone. Continue until menstruation has been established, or longer if clinically indicated (Palmert 2012; Santos 2014; Sperling 2014).
Oral (micronized, Estrace): Initial dose: 5 mcg/kg once daily; after 6 to 12 months of therapy, may increase to 10 mcg/kg once daily (Palmert 2012). Using currently available dosage forms, some have recommended starting at a fixed dose of 0.25 mg once daily (1/2 of the 0.5 mg tablet) and increasing to 0.5 mg once daily after 6 to 12 months.
Transdermal: Initial dose: 3.1 to 6.2 mcg/day patch (eg, 1/8 to 1/4 of a 25 mcg/day patch), apply at night, remove in the morning. Increase by 3.1 to 6.2 mcg/day patch every 6 months (Palmert 2012). Note: The practice of cutting patches to achieve low doses is cited frequently in the literature (Ankarberg-Lindgren 2001; Davenport 2010; Hindmarsh 2009; Palmert 2012); however, product specific data may not be available for all transdermal products due to product availability/manufacturing changes.
Hypogonadism (females): Limited data available: Children ≥12 years and Adolescents: Note: Begin with the lowest available dose and gradually increase. Obtain bone age every 6 months to avoid premature epiphyseal closure. Once breast growth is significant and has plateaued or breakthrough bleeding occurs, add cyclic progesterone. Continue until menstruation has been established, or longer if clinically indicated (Palmert 2012; Sperling 2014).
Oral (micronized): Initial dose: 5 mcg/kg once daily for 6 to 12 months; may then increase to 10 mcg/kg/day for 6 to 12 months; dose may be increased at every 6 to 12 month intervals by 5 mcg/kg/day, up to 20 mcg/kg/day. Do not exceed adult dose of 2 mg daily (Palmert 2012).
Transdermal: Initial dose: 3.1 to 6.2 mcg/day patch (eg, 1/8 to 1/4 of a 25 mcg/day patch), apply at night, remove in the morning. Increase by 3.1 to 6.2 mcg/day patch every 6 months; Do not exceed adult dose of 50 to 100 mcg/24 hours (Palmert 2012). Note: The practice of cutting patches to achieve low doses is cited frequently in the literature (Ankarberg-Lindgren 2001; Davenport 2010; Hindmarsh 2009; Palmert 2012); however, product specific data may not be available for all transdermal products due to product availability/manufacturing changes.
Turner syndrome (females): Limited data available: Children ≥12 years and Adolescents: Begin at ~12 years of age using a low dose and gradually increase dose over 2 to 4 years to full adult dose. After 2 years of estrogen or when breakthrough bleeding occurs, add cyclic progesterone. Note: Full dose estrogen will be needed until at least age 30 years (Bondy 2007).
IM: Cypionate (Depot-Estradiol): Initial: 0.2 to 0.4 mg every 4 weeks, slowly increase dose over about 2 years to the goal adult dose: 3 mg/month; one trial started at 0.2 mg/dose, then increased dose at 6 month intervals in 0.2 mg/dose increments until dose of 1 mg reached and then increased in 0.5 mg/dose increments thereafter to a final dose of 3 mg (Bondy 2007; Rosenfield 2005)
Oral (micronized, Estrace): Initial dose: 5 mcg/kg once daily for the first 2 years, followed by 7.5 mcg/kg for the 3rd year, then 10 mcg/kg thereafter; once final height is attained, increase to adult dose of 1 to 2 mg/day (Bannink 2009). A fixed dose of 0.25 mg once daily; increasing to the adult dose of 2 to 4 mg/day over the course of 2 years has also been suggested (Bondy 2007). Note: Due to extensive first-pass metabolism, other routes of administration may be preferable.
Topical gel (Divigel): Initial: 0.1 mg of estradiol once daily for the first year, 0.2 mg of estradiol once daily for the second year, 0.5 mg of estradiol once daily for the third year, 1 mg of estradiol once daily for the fourth year, and 1.5 mg of estradiol once daily for the fifth year. Dosing based on a trial of 23 girls that followed development for 5 years; long-term dose is unknown. Due to lack of commercially available product for lower doses, individual sachets of 0.1 mg estradiol were prepared (Piippo 2004).
Transdermal patch: Initial: 6.25 mcg/day patch; slowly increase over about 2 years to the goal adult dose: 100 to 200 mcg/day patch (Bondy 2007)
Note: The lowest-dose commercially available patches deliver 14 and 25 μg daily; preferred dose fractionation method has not been established (eg, administering a partial patch, limiting to overnight use, or administering whole patches for 7 to 10 days per month). Product specific data may not be available for splitting/cutting some transdermal patches; one center has used the following titration method using Vivelle-Dot product (Davenport 2010):
Treatment month:
0 to <6 months of treatment: 3.125 mcg to 4.17 mcg/dose (equals 1/8 to 1/6 of a 25 mcg/day patch), apply at night, remove in the morning (not continuous)
6 to <12 months of treatment: 3.125 mcg to 4.17 mcg/dose (equals 1/8 to 1/6 of a 25 mcg/day patch) apply twice weekly (continuous)
12 to <18 months of treatment: 6.25 mcg to 8.33 mcg/dose (equals 1/4 to 1/3 of a 25 mcg/day patch), apply twice weekly (continuous)
18 to <24 months of treatment: 12.5 mcg/dose (equals 1/2 of a 25 mcg/day patch), apply twice weekly (continuous)
≥24 months of treatment: 25 mcg/day patch, apply twice weekly (continuous); then increase by one patch strength every 6 months to a final goal of 100 mcg/day continuously
Administration
The use of a progestin should be considered when administering estrogens to postmenopausal women with a uterus.
Injection formulation: Intramuscular use only.
Estradiol cypionate: Shake or gently warm vial to redissolve crystals that may have formed during storage.
Estradiol valerate: Should be injected into the upper outer quadrant of the gluteal muscle; administer with a dry needle (solution may become cloudy with wet needle).
Gel: Apply to clean, dry, unbroken skin at the same time each day. Wash hands after application. Gel is flammable; avoid fire or flame until skin is dry.
Divigel: Do not apply to face, breasts, vaginal area or irritated skin. The entire contents of packet should be applied to right or left upper thigh each day (alternate sites). Apply over an area ~5 x 7 inches. Do not wash application site for 1 hour. Allow gel to dry before dressing.
Elestrin: Do not apply to breasts or vaginal area. The entire dose should be applied to upper arm and shoulder area using two fingers to spread gel. Allow skin to dry for ≥5 minutes prior to dressing. Prior to first use, pump must be primed. After priming, the pump contains 30 metered doses; discard pump after 30 doses even though container may not be empty. If >1 dose is needed, wait 5 seconds before pumping next dose. To avoid secondary exposure, do not allow others to contact the application site for 2 hours after gel is applied. Allow at least 2 hours between applying gel and going swimming. Wait at least 25 minutes before applying sunscreen to application area. When sunscreen and gel are applied to the same site for >7 consecutive days, the absorption of estradiol is increased; do not apply sunscreen to an area where the gel was applied for ≥7 consecutive days.
EstroGel: Do not apply to breasts or vaginal area. Apply dose into the palm of hand and then apply gel to the other arm, from the wrist to the shoulder. Spread gel as thinly as possible over one arm but do not massage or rub in gel. Allow skin to dry for 5 minutes before dressing. Prior to first use, pump must be primed. After priming, the pump contains 32 daily doses (50 g canister) or 14 daily doses (25 g canister). Discard pump after allotted doses even though container may not be empty. To avoid secondary exposure, do not allow others to contact the application site for ≥1 hour after gel is applied. Wait as long as possible between applying gel and going swimming. When sunscreen was applied 1 hour after the gel to the same site for >7 consecutive days, the absorption of estradiol was decreased; when moisturizing lotion was applied 1 hour after the gel to the same site for >7 consecutive days, the absorption of estradiol was increased. The effect of applying sunscreen or lotion prior to the gel has not been studied.
Spray: Evamist: Prior to first use, prime pump by spraying 3 sprays with the cover on. To administer dose, hold container upright and vertical and rest the plastic cone flat against the skin while spraying. Spray to the inner surface of the forearm, starting near the elbow. If more than one spray is needed, apply to adjacent but not overlapping areas. Apply at the same time each day. Allow spray to dry for ~2 minutes; do not rub into skin; do not cover with clothing until dry. Do not wash application site for at least 60 minutes. Apply to clean, dry, unbroken skin. Do not apply to skin other than that of the forearm. Make sure that children do not come in contact with any skin area where the drug was applied. If contact with children is unavoidable, wear a garment with long sleeves that covers the site of application. If direct exposure should occur, wash the child in the area of exposure with soap and water as soon as possible. Solution contained in the spray is flammable; avoid fire, flame, or smoking until spray has dried. If needed, sunscreen should be applied ~1 hour prior to application of Evamist.
Transdermal patch: General administration instructions (also refer to product labeling): Apply patch immediately after removing from protective pouch to lower abdomen or buttocks. Apply to clean, dry, healthy skin that is free of oil, powder, or lotion. Avoid waistline or other areas where tight clothing may rub the patch off; do not apply to breasts. After application, hold patch in place using palm of hand for 10 seconds. Rotate application sites allowing a 1-week interval between applications at a particular site. In general, if patch falls off, the same patch may be reapplied or a new system may be used for the remainder of the dosing interval. When replacing patch, reapply to a new site. Remove patch slowly after use to avoid skin irritation. If any adhesive remains on the skin after removal, first allow skin to dry for 15 minutes, then gently rub area with an oil-based cream or lotion. Dispose of any used or unused patches by folding adhesive ends together, replace in pouch or sealed container, and discard properly in trash away from children and pets.
Climara, Menostar: Swimming, bathing, or wearing patch while in a sauna have not been studied
Vaginal ring: Exact positioning is not critical for efficacy; however, patient should not feel anything once inserted. In case of discomfort, ring should be pushed further into vagina. If ring is expelled prior to 90 days, it may be rinsed off with warm water and reinserted. Ensure proper vaginal placement of the ring to avoid inadvertent urinary bladder insertion. If vaginal infection develops, Femring may remain in place during local treatment of a vaginal infection.
Dietary Considerations
Ensure adequate calcium and vitamin D intake when used for the prevention of osteoporosis.
Storage
Store all products at controlled room temperature. In addition:
Depo-Estradiol: Protect from light.
Evamist: Do not freeze.
Femring: Store in pouch.
Transdermal patch (all products): Store in protective pouch.
Climara, Menostar: Do not store >30°C (>86°F).
Estradiol (Systemic) Images
Drug Interactions
Ajmaline: Estrogen Derivatives may enhance the adverse/toxic effect of Ajmaline. Specifically, the risk for cholestasis may be increased. Monitor therapy
Anastrozole: Estrogen Derivatives may diminish the therapeutic effect of Anastrozole. Avoid combination
Anthrax Immune Globulin (Human): Estrogen Derivatives may enhance the thrombogenic effect of Anthrax Immune Globulin (Human). Monitor therapy
Anticoagulants: Estrogen Derivatives may diminish the anticoagulant effect of Anticoagulants. More specifically, the potential prothrombotic effects of some estrogens and progestin-estrogen combinations may counteract anticoagulant effects. Management: Carefully weigh the prospective benefits of estrogens against the potential increased risk of procoagulant effects and thromboembolism. Use is considered contraindicated under some circumstances. Refer to related guidelines for specific recommendations. Consider therapy modification
Antidiabetic Agents: Hyperglycemia-Associated Agents may diminish the therapeutic effect of Antidiabetic Agents. Monitor therapy
Ascorbic Acid: May increase the serum concentration of Estrogen Derivatives. Monitor therapy
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
C1 inhibitors: Estrogen Derivatives may enhance the thrombogenic effect of C1 inhibitors. Monitor therapy
Chenodiol: Estrogen Derivatives may diminish the therapeutic effect of Chenodiol. Management: Monitor clinical response to chenodiol closely when used together with any estrogen derivative. Monitor therapy
CloZAPine: CYP1A2 Inhibitors (Weak) may increase the serum concentration of CloZAPine. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Corticosteroids (Systemic): Estrogen Derivatives may increase the serum concentration of Corticosteroids (Systemic). Monitor therapy
Cosyntropin: Estrogen Derivatives may diminish the diagnostic effect of Cosyntropin. Management: Discontinue estrogen containing drugs 4 to 6 weeks prior to cosyntropin (ACTH) testing. Consider therapy modification
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May increase the metabolism of CYP3A4 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
CYP3A4 Inhibitors (Moderate): May increase the serum concentration of Estrogen Derivatives. Monitor therapy
CYP3A4 Inhibitors (Strong): May increase the serum concentration of Estrogen Derivatives. Monitor therapy
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dantrolene: Estrogen Derivatives may enhance the hepatotoxic effect of Dantrolene. Monitor therapy
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Dehydroepiandrosterone: May enhance the adverse/toxic effect of Estrogen Derivatives. Avoid combination
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Exemestane: Estrogen Derivatives may diminish the therapeutic effect of Exemestane. Avoid combination
Hemin: Estrogen Derivatives may diminish the therapeutic effect of Hemin. Avoid combination
Herbs (Estrogenic Properties): May enhance the adverse/toxic effect of Estrogen Derivatives. Monitor therapy
Hyaluronidase: Estrogen Derivatives may diminish the therapeutic effect of Hyaluronidase. Management: Patients receiving estrogens (particularly at larger doses) may not experience the desired clinical response to standard doses of hyaluronidase. Larger doses of hyaluronidase may be required. Consider therapy modification
Immune Globulin: Estrogen Derivatives may enhance the thrombogenic effect of Immune Globulin. Monitor therapy
Indium 111 Capromab Pendetide: Estrogen Derivatives may diminish the diagnostic effect of Indium 111 Capromab Pendetide. Avoid combination
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
LamoTRIgine: Estrogen Derivatives may decrease the serum concentration of LamoTRIgine. Monitor therapy
Lasmiditan: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Avoid combination
Lenalidomide: Estrogen Derivatives may enhance the thrombogenic effect of Lenalidomide. Monitor therapy
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Mivacurium: Estrogen Derivatives may increase the serum concentration of Mivacurium. Monitor therapy
Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective): May enhance the thrombogenic effect of Estrogen Derivatives. Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective) may increase the serum concentration of Estrogen Derivatives. Monitor therapy
Ospemifene: Estrogen Derivatives may enhance the adverse/toxic effect of Ospemifene. Estrogen Derivatives may diminish the therapeutic effect of Ospemifene. Avoid combination
P-glycoprotein/ABCB1 Inducers: May decrease the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inducers may also further limit the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Monitor therapy
P-glycoprotein/ABCB1 Inhibitors: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inhibitors may also enhance the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Monitor therapy
Pomalidomide: May enhance the thrombogenic effect of Estrogen Derivatives. Management: Canadian pomalidomide labeling recommends caution with use of hormone replacement therapy and states that hormonal contraceptives are not recommended. US pomalidomide labeling does not contain these specific recommendations. Consider therapy modification
Ranolazine: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
ROPINIRole: Estrogen Derivatives may increase the serum concentration of ROPINIRole. Monitor therapy
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Somatropin: Estrogen Derivatives may diminish the therapeutic effect of Somatropin. Shown to be a concern with oral hormone replacement therapy in postmenopausal women. Management: Monitor for reduced growth hormone efficacy. A larger somatropin dose may be required to reach treatment goal. This interaction does not appear to apply to non-orally administered estrogens (e.g., transdermal, vaginal ring). Consider therapy modification
Succinylcholine: Estrogen Derivatives may increase the serum concentration of Succinylcholine. Monitor therapy
Thalidomide: Estrogen Derivatives may enhance the thrombogenic effect of Thalidomide. Monitor therapy
Theophylline Derivatives: CYP1A2 Inhibitors (Weak) may increase the serum concentration of Theophylline Derivatives. Exceptions: Dyphylline. Monitor therapy
Thyroid Products: Estrogen Derivatives may diminish the therapeutic effect of Thyroid Products. Monitor therapy
Tipranavir: Estrogen Derivatives may enhance the dermatologic adverse effect of Tipranavir. The combination of tipranavir/ritonavir and ethinyl estradiol/norethindrone was associated with a high incidence of skin rash. Tipranavir may decrease the serum concentration of Estrogen Derivatives. Management: Women using hormonal contraceptives should consider alternative, non-hormonal forms of contraception. Consider therapy modification
TiZANidine: CYP1A2 Inhibitors (Weak) may increase the serum concentration of TiZANidine. Management: Avoid these combinations when possible. If combined use is necessary, initiate tizanidine at an adult dose of 2 mg and increase in 2 to 4 mg increments based on patient response. Monitor for increased effects of tizanidine, including adverse reactions. Consider therapy modification
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Ursodiol: Estrogen Derivatives may diminish the therapeutic effect of Ursodiol. Monitor therapy
Test Interactions
Reduced response to metyrapone test.
Adverse Reactions
Frequency not always defined. Some adverse reactions observed with estrogen and/or progestin combination therapy.
Cardiovascular: Edema (10% to 13%), hypertension (3% to 7%), cerebrovascular accident, deep vein thrombosis, local thrombophlebitis, myocardial infarction, pulmonary thromboembolism, retinal thrombosis, thrombophlebitis, venous thromboembolism
Central nervous system: Headache (9% to 50%), pain (6% to 13%), depression (1% to 11%), anxiety (4% to 10%), dizziness (≤8%), migraine (7%), nipple pain (1% to 7%), hypoesthesia (3%), chorea, dementia, exacerbation of epilepsy, irritability, mood disorder, nervousness
Dermatologic: Skin rash (7% to 9%), pruritus (4% to 7%), chloasma, erythema multiforme, erythema nodosum, localized erythema (transdermal patch), loss of scalp hair, skin discoloration (melasma), urticaria
Endocrine & metabolic: Weight gain (4% to 9%), hot flash (6%), hirsutism (≤5%), change in libido, change in menstrual flow (alterations in frequency and flow of bleeding patterns), exacerbation of diabetes mellitus, exacerbation of porphyria, fibrocystic breast changes, fluid retention, galactorrhea, hypocalcemia, increased serum triglycerides, weight loss
Gastrointestinal: Abdominal pain (6% to 16%), dyspepsia (3% to 9%), constipation (4% to 7%), flatulence (3% to 7%), nausea (3% to 7%), gastroenteritis (3% to 4%), diarrhea (3%), abdominal cramps, bloating, carbohydrate intolerance, gallbladder disease, pancreatitis, vomiting
Genitourinary: Mastalgia (5% to 35%), vaginal hemorrhage (33%), breast tenderness (3% to 17%), endometrium disease (15%), breakthrough bleeding (6% to 11%), leukorrhea (2% to 11%), abnormal uterine bleeding (4% to 10%), breast hypertrophy (7%), dysmenorrhea (7%), cervical polyp (6%), vulvovaginal candidiasis (6%), urinary tract infection (4% to 6%), change in cervical ectropion, change in cervical secretions, endometrial hyperplasia, nipple discharge, spotting, uterine fibroids (size increased), uterine pain, vaginal discomfort (vaginal ring; burning, irritation, itching), vaginitis
Hematologic & oncologic: Hemorrhagic eruption, hypercoagulability state, malignant neoplasm of breast, ovarian cancer
Hepatic: Cholestatic jaundice, exacerbation of hepatic hemangioma
Hypersensitivity: Hypersensitivity reaction (4% to 5%), anaphylactoid reaction, anaphylaxis, angioedema
Infection: Infection (3% to 12%), fungal infection (3% to 10%)
Local: Application site reaction (gel, spray, transdermal patch ≤1%)
Neuromuscular & skeletal: Arthralgia (4% to 12%), back pain (3% to 11%), weakness (8%), limb pain (7% to 8%), myalgia (5% to 6%), neck pain (3% to 6%), arthropathy (4% to 5%), exacerbation of systemic lupus erythematosus, leg cramps
Ophthalmic: Conjunctivitis (3%), change in corneal curvature (steepening), contact lens intolerance
Otic: Otitis media (3%)
Respiratory: Nasopharyngitis (4% to 20%), upper respiratory tract infection (6% to 17%), flu-like symptoms (8% to 13%), sinusitis (4% to 13%), sinus headache (9% to 11%), bronchitis (6% to 8%), sinus congestion (7%), pharyngitis (2% to 7%), rhinitis (2% to 6%), cough (3% to 4%), asthma (3%), exacerbation of asthma
Miscellaneous: Accidental injury (7% to 14%), cyst (7%)
Postmarketing and/or case reports: Abnormal gait, abnormal hepatic function tests, aphasia, blindness, bowel obstruction (vaginal ring), chest pain, cholecystitis, cholelithiasis, cognitive dysfunction, dyspnea, emotional lability, fatigue, genitourinary complaint (inadvertent ring insertion into the bladder should be considered with unexplained urinary complaints), hemorrhage, hepatitis, hyperhidrosis, hypermenorrhea, ischemic heart disease, lip swelling, local irritation (transdermal patch), localized erythema (transdermal patch), malaise, mechanical complication of genitourinary device (ring adherence to vaginal or bladder wall), meningioma, muscle spasm, myoclonus, night sweats, oral paresthesia, ovarian cyst, palpitations, paresthesia, peripheral edema, pharyngeal edema, phlebitis, portal vein thrombosis, purpura, retinal vein occlusion, soft tissue sarcoma (malignant mesenchymoma), swollen tongue, tachyphylaxis, toxic shock syndrome (vaginal ring), transient ischemic attacks, unstable angina pectoris, uterine enlargement, uterine neoplasm, vaginal discharge
Warnings/Precautions
Concerns related to adverse effects:
- Anaphylaxis: Anaphylaxis requiring emergency medical management has been reported and may develop at any time during therapy. Angioedema involving the face, feet, hands, larynx, and tongue has also been reported.
- Breast cancer: [US Boxed Warning]: Based on data from the Women’s Health Initiative (WHI) studies, an increased risk of invasive breast cancer was observed in postmenopausal women using conjugated estrogens (CE) in combination with medroxyprogesterone acetate (MPA). Observational studies noted this risk declines once therapy is discontinued. The WHI study did not observe an increased risk of invasive breast cancer in women with a hysterectomy using CE alone. The risk of breast cancer in postmenopausal patients on hormone therapy may depend upon type of estrogen and/or progestin, dose, timing of therapy initiation, duration of therapy, route of administration, and individual patient characteristics (AACE/ACE [Cobin 2017]; NAMS 2017). Hormone therapy may be associated with increased breast density (NAMS 2017); an increase in abnormal mammogram findings requiring further evaluation has been reported with estrogen alone or in combination with progestin therapy. Estrogen use may lead to severe hypercalcemia in patients with breast cancer and bone metastases; discontinue estrogen if hypercalcemia occurs.
- Dementia: [US Boxed Warning]: Estrogens with or without progestin should not be used to prevent dementia. In the Women’s Health Initiative Memory Study (WHIMS), an increased incidence of probable dementia was observed in women ≥65 years of age taking CE alone or in combination with MPA. Because the WHI memory studies were conducted in women ≥65 years of age, it is unknown if these findings apply to younger postmenopausal women. However, hormone therapy is not recommended at any age to prevent or treat cognitive decline or dementia (AACE [Goodman 2011]; NAMS 2017).
- Endometrial cancer: [US Boxed Warning]: The use of unopposed estrogen in women with a uterus is associated with an increased risk of endometrial cancer. The addition of a progestin to estrogen therapy may decrease the risk of endometrial hyperplasia, a precursor to endometrial cancer. Adequate diagnostic measures, including endometrial sampling if indicated, should be performed to rule out malignancy in postmenopausal women with undiagnosed abnormal vaginal bleeding. There is no evidence that the use of natural estrogens results in a different endometrial risk profile than synthetic estrogens at equivalent estrogen doses. The risk of endometrial cancer appears to be dose and duration dependent, greatest with use ≥5 years, and may persist following discontinuation of therapy. The use of a progestin is not generally required when low doses of estrogen are used locally for vaginal atrophy, although long term data (>1 year) supporting this recommendation are lacking (NAMS 2013; NAMS 2017).
- Endometriosis: Estrogens may exacerbate endometriosis. Malignant transformation of residual endometrial implants has been reported posthysterectomy with unopposed estrogen therapy. Consider adding a progestin in women with residual endometriosis posthysterectomy.
- Lipid effects: Estrogen compounds are generally associated with lipid effects such as increased HDL-cholesterol and decreased LDL-cholesterol. Triglycerides may also be increased in women with preexisting hypertriglyceridemia; discontinue if pancreatitis occurs.
- Ovarian cancer: Available information related to the use of menopausal estrogen or estrogen/progestin therapy and risk of ovarian cancer is inconsistent. If an association is present, the absolute risk is likely rare and may be influenced by duration of therapy (AACE [Goodman 2011]; ES [Stuenkel 2015]; NAMS 2017).
- Retinal vascular thrombosis: Estrogens may cause retinal vascular thrombosis; discontinue if migraine, loss of vision, proptosis, diplopia, or other visual disturbances occur; discontinue permanently if papilledema or retinal vascular lesions are observed on examination.
Disease-related concerns:
- Asthma: Use caution with asthma; may exacerbate disease.
- Carbohydrate intolerance: May impair glucose tolerance; use caution in patients with diabetes. Prior to therapy, consider age, cardiovascular and metabolic risk factors in patients previously diagnosed with diabetes (AACE/ACE [Cobin 2017]).
- Cardiovascular disease: [US Boxed Warning]: Estrogens with or without progestin should not be used to prevent cardiovascular disease. Using data from the Women’s Health Initiative (WHI) studies, an increased risk of deep vein thrombosis (DVT) and stroke has been reported with CE and an increased risk of DVT, stroke, pulmonary emboli (PE) and myocardial infarction (MI) has been reported with CE with MPA in postmenopausal women 50 to 79 years of age. Additional risk factors include diabetes mellitus, hypercholesterolemia, hypertension, SLE, obesity, tobacco use, and/or history of venous thromboembolism (VTE). Adverse cardiovascular events have also been reported in males taking estrogens for prostate cancer. Risk factors should be managed appropriately; discontinue use immediately if adverse cardiovascular events occur or are suspected. Due to possible lower risk of thrombotic events, transdermal administration may be preferred for treating vasomotor symptoms of menopause in patients with risk factors for cardiovascular disease (AACE/ACE [Cobin 2017]; ACOG 556 2013; ES [Stuenkel 2015]). Use is contraindicated in women with active DVT, PE, arterial thromboembolic disease (stroke and MI), or a history of these conditions.
- Diseases exacerbated by fluid retention: Use caution with diseases which may be exacerbated by fluid retention, including cardiac or renal dysfunction.
- Epilepsy: Use caution with epilepsy; may exacerbate disease.
- Gallbladder disease: Use of postmenopausal estrogen may be associated with an increased risk of gallbladder disease requiring surgery.
- Hepatic dysfunction: Estrogens are poorly metabolized in patients with hepatic dysfunction. Use caution with a history of cholestatic jaundice associated with prior estrogen use or pregnancy. Discontinue if jaundice develops or if acute or chronic hepatic disturbances occur. Use is contraindicated with hepatic impairment or disease.
- Hepatic hemangiomas: Use caution with hepatic hemangiomas; may exacerbate disease.
- Hereditary angioedema: Exogenous estrogens may exacerbate angioedema symptoms in women with hereditary angioedema.
- Hypoparathyroidism: Use caution with hypoparathyroidism; estrogen-induced hypocalcemia may occur.
- Migraine: Use caution with migraine; may exacerbate disease.
- Porphyria: Use caution with porphyria; may exacerbate disease.
- SLE: Use caution with SLE; may exacerbate disease.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
- Thyroid replacement therapy: Estrogens may increase thyroid-binding globulin (TBG) levels leading to increased circulating total thyroid hormone levels. Women on thyroid replacement therapy may require higher doses of thyroid hormone while receiving estrogens.
Special populations:
- Pediatric: Prior to puberty, estrogens may cause premature closure of the epiphyses. Premature breast development, vaginal bleeding, and vaginal cornification may be induced in girls. Modification of the normal puberty process may occur in boys.
- Surgical patients: Whenever possible, estrogens should be discontinued at least 4 to 6 weeks prior to elective surgery associated with an increased risk of thromboembolism or during periods of prolonged immobilization.
Dosage form specific issues:
- Benzyl alcohol and derivatives: Some dosage forms may contain benzyl alcohol; large amounts of benzyl alcohol (≥99 mg/kg/day) have been associated with a potentially fatal toxicity (“gasping syndrome”) in neonates; the “gasping syndrome” consists of metabolic acidosis, respiratory distress, gasping respirations, CNS dysfunction (including convulsions, intracranial hemorrhage), hypotension and cardiovascular collapse (AAP ["Inactive" 1997]; CDC 1982); some data suggests that benzoate displaces bilirubin from protein binding sites (Ahlfors 2001); avoid or use dosage forms containing benzyl alcohol with caution in neonates. See manufacturer's labeling.
- Chlorobutanol: Some products may contain chlorobutanol (a chloral derivative) as a preservative, which may be habit forming.
- Tartrazine: Some products may contain tartrazine.
- Topical gel: Absorption of the topical gel (Elestrin) is increased by application of sunscreen; do not apply sunscreen within close proximity of estradiol. Application of sunscreen after EstroGel decreases absorption of estradiol while application of moisturizer lotion after EstroGel increases the absorption of estradiol; the effect of applying sunscreen or lotion prior to Estrogel has not been studied. Application of Divigel with sunscreen has not been evaluated.
- Topical spray: When sunscreen is applied ~1 hour prior to the topical spray (Evamist), no change in absorption was observed (estradiol absorption was decreased when sunscreen is applied 1 hour after Evamist).
- Transdermal patch: May contain conducting metal (eg, aluminum); remove patch prior to MRI.
- Vaginal ring: Use may not be appropriate in women with narrow vagina, vaginal stenosis, vaginal infections, cervical prolapse, rectoceles, cystoceles, or other conditions which may increase the risk of vaginal irritation, ulceration, or increase the risk of expulsion. Ring should be removed in case of ulceration, erosion, or adherence to vaginal wall; do not reinsert until healing is complete. Ensure proper vaginal placement of the ring to avoid inadvertent urinary bladder insertion.
Other warnings/precautions:
- Duration of use: Extended use of menopausal hormone therapy may be considered for persistent vasomotor symptoms, issues related to quality of life, or for osteoporosis prevention in women at increased risk of fracture. Menopausal hormonal therapy does not need to be routinely discontinued in women >60 years of age and may continue in women >65 years of age after clinical evaluation and discussion of benefits and risks of treatment. Annual exams should be performed with a review of comorbidities; possible adjustments to safer lower-dose and/or route of administration should be discussed (ACOG 565 2013; NAMS 2017).
- Genitourinary syndrome of menopause: Low-dose vaginal estrogen is preferred over systemic therapy for genitourinary syndrome of menopause (GSM) in the absence of vasomotor symptoms due to increased efficacy and decreased systemic effects (eg, cardiovascular effects, cancer risk) (Crandall 2018; NAMS 2013; NAMS 2017).
- Laboratory changes: The use of estrogens and/or progestins may change the results of some laboratory tests (eg, coagulation factors, lipids, glucose tolerance, binding proteins). The dose, route, and the specific estrogen/progestin influence these changes.
- Osteoporosis use: In women with premature menopause, hormone therapy to prevent bone loss may be used unless otherwise contraindicated; therapy should be reassessed when the average age of menopause is reached. It is also an appropriate bone-active therapy for women with vasomotor symptoms who are <60 years of age or within 10 years of menopause onset. Use may be considered for women at high risk of fractures who are not candidates for other osteoporosis therapies (NAMS 2017).
- Risks vs benefits: When used for the relief of menopausal symptoms or increased risk of bone fracture/loss, the benefit-risk of hormone therapy is most favorable if started in patients who have no contraindications to therapy, are <60 years of age, within 10 years of menopause onset, have a favorable lipid profile, and do not have the factor V Leiden genotype or metabolic syndrome. Risk factors for cardiovascular disease should also be considered when evaluating therapy and route of administration (AACE/ACE [Cobin 2017]; NAMS 2017). [US Boxed Warning]: Estrogens with or without progestin should be used for the shortest duration possible at the lowest effective dose consistent with treatment goals and risks for the individual woman. Patients should be reevaluated as clinically appropriate to determine if treatment is still necessary. Available data related to treatment risks are from Women’s Health Initiative (WHI) studies, which evaluated oral CE 0.625 mg with or without MPA 2.5 mg relative to placebo in postmenopausal women. Other combinations and dosage forms of estrogens and progestins were not studied. Outcomes reported from clinical trials using CE with or without MPA should be assumed to be similar for other doses and other dosage forms of estrogens and progestins until comparable data becomes available.
- Secondary exposure: Estradiol may be transferred to another person following skin-to-skin contact with the application site. [US Boxed Warning]: Breast budding and breast masses in prepubertal females and gynecomastia and breast masses in prepubertal males have been reported following unintentional contact with application sites of women using topical estradiol (Evamist). Patients should strictly adhere to instructions for use in order to prevent secondary exposure. In most cases, conditions resolved with removal of estradiol exposure. If unexpected changes in sexual development occur in prepubertal children, the possibility of unintentional estradiol exposure should be evaluated by a health care provider. Discontinue if conditions for the safe use of the topical spray cannot be met.
Monitoring Parameters
Females: Prior to therapy, baseline risk for breast cancer and CVD. During therapy, age appropriate breast and pelvic exams; blood pressure; unscheduled bleeding lasting >6 months for endometrial pathology (sooner in patients who are obese, diabetic, or have a history of endometrial cancer); serum triglycerides (2 weeks after starting therapy in patients with baseline level >200 mg/dL); TSH (6 to 12 weeks after starting oral therapy in patients taking thyroid replacement) (ES [Stuenkel 2015]).
Menopausal symptoms: Efficacy beginning 1 to 3 months after starting therapy, then every 6 to 12 months as appropriate. Duration of treatment should be evaluated at least annually (ES [Stuenkel 2015]).
Note: Monitoring of FSH and serum estradiol is not useful when managing vasomotor symptoms or GSM
Prevention of osteoporosis: Bone density measurement
Menostar: When used in a woman with a uterus, endometrial sampling is recommended at yearly intervals or when clinically indicated.
Transgender hormone therapy: Serum estradiol levels (goal: ≤100 to 200 pg/mL) and serum testosterone levels (goal: <50 ng/dL) every 3 months during the first year and then annually or biannually; prolactin levels (as appropriate); routine cancer and laboratory screening as in non-transgender individuals for all tissues present (ES [Hembree 2017]).
Pregnancy
Pregnancy Considerations
Products approved for use only in postmenopausal women are not appropriate for use in pregnancy; use of some products is specifically contraindicated in the manufacturer's labeling.
In general, the use of estrogen and progestin as in combination hormonal contraceptives has not been associated with teratogenic effects when inadvertently taken early in pregnancy.
Patient Education
What is this drug used for?
- It is used to put off soft, brittle bones (osteoporosis) in women after change of life.
- It is used to prevent or lower the signs of the change of life (menopause).
- It is used to add estrogen to the body when the ovaries have been taken out or do not work the right way.
- Rarely, it is used to treat breast or prostate cancers.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Hair loss
- Nausea
- Vomiting
- Constipation
- Abdominal cramps
- Bloating
- Enlarged breasts
- Tender breasts
- Painful periods
- Common cold symptoms
- Stuffy nose
- Sore throat
- Weight gain
- Joint pain
- Application site irritation
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- High calcium like weakness, confusion, fatigue, headache, nausea and vomiting, constipation, or bone pain
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Gallstones like pain in the upper right abdominal area, right shoulder area, or between the shoulder blades; yellow skin; or fever with chills
- Severe cerebrovascular disease like change in strength on one side is greater than the other, difficulty speaking or thinking, change in balance, or vision changes
- Blood clots like numbness or weakness on one side of the body; pain, redness, tenderness, warmth, or swelling in the arms or legs; change in color of an arm or leg; chest pain; shortness of breath; fast heartbeat; or coughing up blood
- Severe headache
- Severe dizziness
- Passing out
- Severe abdominal pain
- Back pain
- Bulging eyes
- Contact lens discomfort
- Blindness
- Vision changes
- Lump in breast
- Breast soreness or pain
- Nipple discharge
- Vaginal pain, itching, and discharge
- Abnormal vaginal bleeding
- Depression
- Mood changes
- Trouble with memory
- Unable to pass urine
- Change in amount of urine passed
- Painful urination
- Edema
- Toxic shock syndrome like diarrhea, dizziness, passing out, severe muscle pain, nausea, vomiting, or sunburn like rash
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.