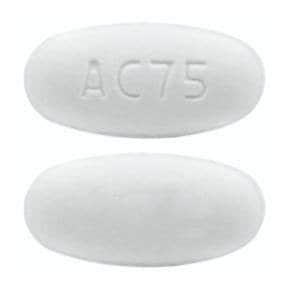
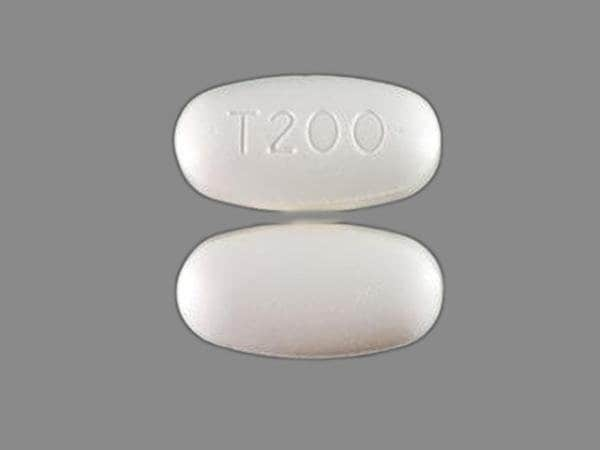
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral:
Intelence: 25 mg [scored]
Intelence: 100 mg, 200 mg
Pharmacology
Mechanism of Action
As a non-nucleoside reverse transcriptase inhibitor, etravirine has activity against HIV-1 by binding to reverse transcriptase. It consequently blocks the RNA-dependent and DNA-dependent DNA polymerase activities, including HIV-1 replication. It does not require intracellular phosphorylation for antiviral activity.
Pharmacokinetics/Pharmacodynamics
Absorption
Increased 50% with food
Metabolism
Hepatic, primarily by CYP3A4, 2C9, and 2C19; major metabolites exhibit ~10% of parent drug activity against wild-type HIV
Excretion
Feces (94%, up to 86% as unchanged drug); urine (1%)
Time to Peak
2.5 to 4 hours
Half-Life Elimination
41 hours (± 20 hours)
Protein Binding
99.9%; primarily to albumin and alpha1-acid glycoprotein
Use: Labeled Indications
HIV-1 infection: Treatment of HIV-1 infection in combination with other antiretroviral agents in treatment-experienced patients 2 years of age and older
Contraindications
There are no contraindications listed in the manufacturer's US labeling.
Canadian labeling: Hypersensitivity to etravirine or any component of the formulation; concomitant use with the hepatitis C combination regimen of ombitasvir, paritaprevir, ritonavir and with drugs containing dasabuvir.
Dosage and Administration
Dosing: Adult
HIV-1 infection: Oral: 200 mg twice daily
Dosing: Pediatric
Note: Gene mutation and ARV resistance patterns should be evaluated (refer to https://www.iasusa.org/ for more information) when necessary.
HIV-1 infection, treatment: Use in combination with other antiretroviral agents.
Children ≥2 years weighing at least 10 kg and Adolescents, antiretroviral-experienced: Oral:
10 kg to <20 kg: 100 mg twice daily
20 kg to <25 kg: 125 mg twice daily
25 kg to <30 kg: 150 mg twice daily
≥30 kg: 200 mg twice daily
Administration
Oral: Administer after meals. If unable to swallow tablets, may disperse tablets in water (5 mL [at least enough to cover tablets]); stir well (until water looks milky), then add ~15 mL of water, milk, or orange juice, and drink immediately. Tablets should not be placed in orange juice or milk without first adding water. Rinse glass several times (with water, milk or orange juice) and swallow entire contents to ensure administration of dose. Do not use carbonated beverages or warm (>40°C) water.
Dietary Considerations
Take after meals.
Storage
Store at USP controlled room temperature of 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Protect from moisture.
Etravirine Images
Drug Interactions
Abemaciclib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Abemaciclib. Avoid combination
Alpelisib: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Monitor therapy
Amiodarone: Etravirine may decrease the serum concentration of Amiodarone. Monitor therapy
Antifungal Agents (Azole Derivatives, Systemic): May increase the serum concentration of Etravirine. Applicable Isavuconazonium considerations are addressed in separate monographs. Etravirine may decrease the serum concentration of Antifungal Agents (Azole Derivatives, Systemic). This would be anticipated with itraconazole or ketoconazole. Etravirine may increase the serum concentration of Antifungal Agents (Azole Derivatives, Systemic). This would be anticipated with voriconazole. Management: Monitor for increased effects/toxicity of etravirine. Antifungal dose adjustment may be needed for ketoconazole, itraconazole, or posaconazole but specific dosing guidelines are lacking. Exceptions: Isavuconazonium Sulfate. Consider therapy modification
Antihepaciviral Combination Products: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Antihepaciviral Combination Products. Avoid combination
Artemether: Etravirine may decrease serum concentrations of the active metabolite(s) of Artemether. Specifically, concentrations of dihydroartemisinin may be decreased. Artemether may increase the serum concentration of Etravirine. Etravirine may increase the serum concentration of Artemether. Monitor therapy
Asunaprevir: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Asunaprevir. Avoid combination
Atazanavir: May increase the serum concentration of Etravirine. Etravirine may decrease the serum concentration of Atazanavir. Management: The combination of etravirine and atazanavir should be avoided unless atazanavir is boosted with ritonavir. The use of cobicistat instead of ritonavir has not been evaluated and is not recommended. Consider therapy modification
Avapritinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Avapritinib. Avoid combination
Axitinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Axitinib. Avoid combination
Bedaquiline: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Bedaquiline. Avoid combination
Benzhydrocodone: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Benzhydrocodone. Specifically, the serum concentrations of hydrocodone may be reduced. Monitor therapy
Bepridil: Etravirine may decrease the serum concentration of Bepridil. Monitor therapy
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Bosutinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Bosutinib. Avoid combination
Brigatinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Brigatinib. Management: Avoid concurrent use of brigatinib with moderate CYP3A4 inducers when possible. If combined, increase the daily dose of brigatinib in 30 mg increments after 7 days of treatment with the current brigatinib dose, up to maximum of twice the dose. Consider therapy modification
Buprenorphine: Etravirine may decrease the serum concentration of Buprenorphine. Monitor therapy
Clarithromycin: CYP3A4 Inducers (Moderate) may increase serum concentrations of the active metabolite(s) of Clarithromycin. CYP3A4 Inducers (Moderate) may decrease the serum concentration of Clarithromycin. Management: Consider alternative antimicrobial therapy for patients receiving a CYP3A inducer. Drugs that enhance the metabolism of clarithromycin into 14-hydroxyclarithromycin may alter the clinical activity of clarithromycin and impair its efficacy. Consider therapy modification
Clopidogrel: Etravirine may decrease serum concentrations of the active metabolite(s) of Clopidogrel. Management: Consider alternatives to clopidogrel in patients treated with etravirine. If combined, monitor for reduced clopidogrel effectiveness. Consider therapy modification
CloZAPine: CYP3A4 Inducers (Moderate) may decrease the serum concentration of CloZAPine. Monitor therapy
Cobimetinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Cobimetinib. Avoid combination
Codeine: CYP3A4 Inducers (Moderate) may decrease serum concentrations of the active metabolite(s) of Codeine. Monitor therapy
CYP2C19 Inducers (Moderate): May decrease the serum concentration of CYP2C19 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May decrease the serum concentration of Etravirine. Avoid combination
CYP3A4 Substrates (High risk with Inducers): CYP3A4 Inducers (Moderate) may decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Exceptions: Apixaban; Rivaroxaban. Monitor therapy
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dabrafenib: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP2C9 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dabrafenib: May decrease the serum concentration of CYP2C19 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP2C19 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Daclatasvir: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Daclatasvir. Management: Increase the daclatasvir dose to 90 mg once daily if used with a moderate CYP3A4 inducer. Consider therapy modification
Darunavir: May decrease the serum concentration of Etravirine. Management: No action is required if etravirine is combined with darunavir/ritonavir. The combination of etravirine and darunavir/cobicistat should be avoided. Consider therapy modification
Dasabuvir: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Dasabuvir. Avoid combination
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Deflazacort: CYP3A4 Inducers (Moderate) may decrease serum concentrations of the active metabolite(s) of Deflazacort. Avoid combination
DiazePAM: Etravirine may decrease the serum concentration of DiazePAM. Etravirine may increase the serum concentration of DiazePAM. Monitor therapy
Digoxin: Etravirine may increase the serum concentration of Digoxin. Management: Monitor serum digoxin concentrations and adjust dose as needed. In patients initiating a regimen of digoxin with etravirine, digoxin should be initiated at the lowest dose. Monitor therapy
Disopyramide: Etravirine may decrease the serum concentration of Disopyramide. Monitor therapy
Dolutegravir: Etravirine may decrease the serum concentration of Dolutegravir. Management: Avoid etravirine with dolutegravir unless with atazanavir/ritonavir, darunavir/ritonavir or lopinavir/ritonavir; avoid use with Dovato brand combination. Canada recommends using dolutegravir 50 mg twice daily when with etravirine without a boosted PI. Consider therapy modification
Doravirine: Etravirine may decrease the serum concentration of Doravirine. Avoid combination
Efavirenz: Reverse Transcriptase Inhibitors (Non-Nucleoside) may increase the serum concentration of Efavirenz. Reverse Transcriptase Inhibitors (Non-Nucleoside) may decrease the serum concentration of Efavirenz. Avoid combination
Elbasvir: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Elbasvir. Avoid combination
Elexacaftor, Tezacaftor, and Ivacaftor: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Elexacaftor, Tezacaftor, and Ivacaftor. Monitor therapy
Encorafenib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Encorafenib. Avoid combination
Entrectinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Entrectinib. Avoid combination
Erdafitinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Erdafitinib. Management: Dose modifications of erdafitinib may be required. See full monograph for details. Consider therapy modification
Ergonovine: Reverse Transcriptase Inhibitors (Non-Nucleoside) may increase the serum concentration of Ergonovine. Specifically, this would be most likely with delavrdine, while other Non-Nucleoside Reverse Transcriptase Inhibitors may be more likely to decrease the concentration of Ergonovine. Avoid combination
Estriol (Systemic): CYP3A4 Inducers (Moderate) may decrease the serum concentration of Estriol (Systemic). Monitor therapy
Estriol (Topical): CYP3A4 Inducers (Moderate) may decrease the serum concentration of Estriol (Topical). Monitor therapy
Fedratinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Fedratinib. Avoid combination
FentaNYL: CYP3A4 Inducers (Moderate) may decrease the serum concentration of FentaNYL. Monitor therapy
Flecainide: Etravirine may decrease the serum concentration of Flecainide. Monitor therapy
Flibanserin: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Flibanserin. Avoid combination
Fluvastatin: Etravirine may increase the serum concentration of Fluvastatin. Monitor therapy
Fosamprenavir: Etravirine may increase serum concentrations of the active metabolite(s) of Fosamprenavir. Specifically, amprenavir concentrations may increase. Avoid combination
Glecaprevir and Pibrentasvir: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Glecaprevir and Pibrentasvir. Monitor therapy
Grazoprevir: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Grazoprevir. Avoid combination
GuanFACINE: CYP3A4 Inducers (Moderate) may decrease the serum concentration of GuanFACINE. Management: Increase the guanfacine dose by up to double when initiating guanfacine in a patient taking a moderate CYP3A4 inducer. Increase guanfacine dose gradually over 1 to 2 weeks if initiating a moderate CYP3A4 inducer in a patient already taking guanfacine. Consider therapy modification
HMG-CoA Reductase Inhibitors (Statins): Etravirine may decrease the serum concentration of HMG-CoA Reductase Inhibitors (Statins). This applies to atorvastatin, lovastatin and simvastatin. Exceptions: Fluvastatin; Pitavastatin; Pravastatin; Rosuvastatin. Monitor therapy
HYDROcodone: CYP3A4 Inducers (Moderate) may decrease the serum concentration of HYDROcodone. Monitor therapy
Ibrutinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Ibrutinib. Monitor therapy
Ifosfamide: CYP3A4 Inducers (Moderate) may decrease serum concentrations of the active metabolite(s) of Ifosfamide. CYP3A4 Inducers (Moderate) may increase serum concentrations of the active metabolite(s) of Ifosfamide. Monitor therapy
Istradefylline: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Istradefylline. Monitor therapy
Ivacaftor: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Ivacaftor. Monitor therapy
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Lefamulin: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Lefamulin. Management: Avoid concomitant use of lefamulin with moderate CYP3A4 inducers unless the benefits outweigh the risks. Consider therapy modification
Lefamulin (Intravenous): CYP3A4 Inducers (Moderate) may decrease the serum concentration of Lefamulin (Intravenous). Management: Avoid concomitant use of lefamulin (intravenous) with moderate CYP3A4 inducers unless the benefits outweigh the risks. Consider therapy modification
Lemborexant: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Lemborexant. Avoid combination
Letermovir: Etravirine may decrease the serum concentration of Letermovir. Avoid combination
Lidocaine (Systemic): Etravirine may decrease the serum concentration of Lidocaine (Systemic). Monitor therapy
Lorlatinib: CYP3A4 Inducers (Moderate) may enhance the hepatotoxic effect of Lorlatinib. CYP3A4 Inducers (Moderate) may decrease the serum concentration of Lorlatinib. Management: Avoid use of lorlatinib with moderate CYP3A4 inducers. If such a combination must be used, monitor AST, ALT, and bilirubin within 48 hours of starting the combination and at least three times within the first week of combined use. Consider therapy modification
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Lumateperone: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Lumateperone. Avoid combination
Lurasidone: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Lurasidone. Management: Monitor for decreased lurasidone effects if combined with moderate CYP3A4 inducers and consider increasing the lurasidone dose if coadministered with a moderate CYP3A4 inducer for 7 or more days. Consider therapy modification
Macimorelin: Etravirine may diminish the diagnostic effect of Macimorelin. Monitor therapy
Maraviroc: Etravirine may decrease the serum concentration of Maraviroc. Of note, this effect only applies in the absence of a strong CYP3A4 inhibitor Management: Increase maraviroc adult dose to 600 mg twice daily if used with etravirine. This does not apply to patients also receiving strong CYP3A4 inhibitors. This combination is contraindicated in patients with CrCl less than 30 mL/min. Consider therapy modification
Meperidine: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Meperidine. Monitor therapy
Methadone: Etravirine may decrease the serum concentration of Methadone. Monitor therapy
Mexiletine: Etravirine may decrease the serum concentration of Mexiletine. Monitor therapy
Mirodenafil: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Mirodenafil. Monitor therapy
Naldemedine: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Naldemedine. Monitor therapy
Neratinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Neratinib. Avoid combination
NiMODipine: CYP3A4 Inducers (Moderate) may decrease the serum concentration of NiMODipine. Monitor therapy
Nisoldipine: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Nisoldipine. Avoid combination
Olaparib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Olaparib. Avoid combination
Orlistat: May decrease the serum concentration of Antiretroviral Agents. Monitor therapy
Palbociclib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Palbociclib. Management: The US label does not provide specific recommendations concerning use with moderate CYP3A4 inducers, but the Canadian label recommends avoiding use of moderate CYP3A4 inducers. Consider therapy modification
Perampanel: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Perampanel. Management: Increase the perampanel starting dose to 4 mg/day when perampanel is used concurrently with moderate and strong CYP3A4 inducers. Consider therapy modification
Pexidartinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Pexidartinib. Monitor therapy
Phosphodiesterase 5 Inhibitors: Etravirine may decrease the serum concentration of Phosphodiesterase 5 Inhibitors. Monitor therapy
Pimavanserin: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Pimavanserin. Avoid combination
Pitavastatin: Etravirine may increase the serum concentration of Pitavastatin. Monitor therapy
Pitolisant: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Pitolisant. Monitor therapy
Pretomanid: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Pretomanid. Avoid combination
Propafenone: Etravirine may decrease the serum concentration of Propafenone. Monitor therapy
Protease Inhibitors: May decrease the serum concentration of Etravirine. This effect is anticipated with darunavir, saquinavir, and lopinavir (with low-dose ritonavir). Etravirine may increase the serum concentration of Protease Inhibitors. This effect is anticipated with nelfinavir. Management: Low-dose ritonavir boosting must be used when any protease inhibitor is used with etravirine. Avoid use of etravirine in combination with atazanavir, fosamprenavir, full-dose ritonavir (600 mg twice daily, in adults), or tipranavir. Exceptions: Atazanavir; Fosamprenavir; Ritonavir; Tipranavir. Monitor therapy
QuiNIDine: Etravirine may decrease the serum concentration of QuiNIDine. Monitor therapy
Raltegravir: Etravirine may decrease the serum concentration of Raltegravir. Management: Concurrent use of etravirine with once-daily raltegravir (Isentress HD) is not recommended. Concurrent use of other raltegravir products with etravirine does not require any dose change. Monitor therapy
Ranolazine: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Ranolazine. Avoid combination
Reverse Transcriptase Inhibitors (Non-Nucleoside): May decrease the serum concentration of Etravirine. This has been observed with the NNRTIs efavirenz and nevirapine. Reverse Transcriptase Inhibitors (Non-Nucleoside) may increase the serum concentration of Etravirine. This has been observed with delavirdine. Avoid combination
Rifabutin: May decrease the serum concentration of Etravirine. Management: Avoid use of rifabutin with etravirine in patients also taking a protease inhibitor/ritonavir. Rifabutin (300 mg daily) may be used with etravirine if etravirine is administered without a protease inhibitor/ritonavir. Avoid combination
Rifapentine: May decrease the serum concentration of Etravirine. Avoid combination
Rilpivirine: Reverse Transcriptase Inhibitors (Non-Nucleoside) may increase the serum concentration of Rilpivirine. This mechanism applies to coadministration of delavirdine. Reverse Transcriptase Inhibitors (Non-Nucleoside) may decrease the serum concentration of Rilpivirine. This mechanism applies to coadministration of efavirenz, etravirine, and nevirapine. Avoid combination
Ritonavir: May decrease the serum concentration of Etravirine. Management: Avoid concomitant use of etravirine with antiviral doses of ritonavir; use with ritonavir-boosted fosamprenavir or with ritonavir-boosted tipranavir is also not recommended. Consider therapy modification
Rolapitant: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Rolapitant. Monitor therapy
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Simeprevir. Avoid combination
Sonidegib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Sonidegib. Avoid combination
St John's Wort: May decrease the serum concentration of Reverse Transcriptase Inhibitors (Non-Nucleoside). Specifically, St. Johns Wort may increase the metabolism of Reverse Transcriptase Inhibitors (Non-Nucleoside). Avoid combination
Tazemetostat: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Tazemetostat. Avoid combination
Tezacaftor and Ivacaftor: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Tezacaftor and Ivacaftor. Monitor therapy
Tipranavir: May decrease the serum concentration of Etravirine. Avoid combination
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Ubrogepant: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Ubrogepant. Management: Use an initial ubrogepant dose of 100 mg and second dose (if needed) of 100 mg when used with a moderate CYP3A4 inducer. Consider therapy modification
Upadacitinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Upadacitinib. Monitor therapy
Velpatasvir: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Velpatasvir. Avoid combination
Venetoclax: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Venetoclax. Avoid combination
Voxelotor: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Voxelotor. Management: Avoid concomitant use of voxelotor and moderate CYP3A4 inducers. If concomitant use is unavoidable, increase the voxelotor dose to 2,500 mg once daily. Consider therapy modification
Zanubrutinib: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Zanubrutinib. Avoid combination
Zolpidem: CYP3A4 Inducers (Moderate) may decrease the serum concentration of Zolpidem. Monitor therapy
Adverse Reactions
>10%:
Dermatologic: Skin rash (10% to 15%)
Endocrine & metabolic: Increased serum cholesterol (grades 2/3: 8% to 20%), increased serum glucose (grades 2/3: 4% to 15%), increased LDL cholesterol (13%)
1% to 10%:
Cardiovascular: Angina pectoris (<2%), atrial fibrillation (<2%), facial edema (<2%), myocardial infarction (<2%), syncope (<2%)
Central nervous system: Peripheral neuropathy (4%), abnormal dreams (<2%), amnesia (<2%), anxiety (<2%), confusion (<2%), disorientation (<2%), disturbance in attention (<2%), drowsiness (<2%), hypersomnia (<2%), hypoesthesia (<2%), lethargy (<2%), nervousness (<2%), nightmares (<2%), paresthesia (<2%), seizure (<2%), sleep disturbance (<2%), vertigo (<2%)
Dermatologic: Hyperhidrosis (<2%), night sweats (<2%), prurigo (<2%), xeroderma (<2%)
Endocrine & metabolic: Increased serum triglycerides (grades 2 to 4: 4% to 9%), increased amylase (grade 4: 2%), diabetes mellitus (<2%), dyslipidemia (<2%), gynecomastia (<2%), lipohypertrophy (<2%)
Gastrointestinal: Diarrhea (children and adolescents: ≥2%), abdominal distention (<2%), anorexia (<2%), constipation (<2%), flatulence (<2%), gastritis (<2%), gastroesophageal reflux disease (<2%), hematemesis (<2%), pancreatitis (<2%), retching (<2%), stomatitis (<2%), xerostomia (<2%), increased serum lipase (grade 4: 1%)
Hematologic & oncologic: Hemolytic anemia (<2%), decreased white blood cell count (grade 4: 1%)
Hepatic: Increased serum alanine aminotransferase (grades 2 to 4: 1% to 6%), increased serum aspartate aminotransferase (grade 3: 3%), hepatic failure (<2%), hepatitis (<2%), hepatomegaly (<2%), liver steatosis (<2%)
Hypersensitivity: Hypersensitivity reaction (<2%)
Immunologic: Immune reconstitution syndrome (<2%)
Neuromuscular & skeletal: Tremor (<2%)
Ophthalmic: Blurred vision (<2%)
Renal: Increased serum creatinine (grades 2/3: 2% to 6%), acute renal failure (<2%)
Respiratory: Bronchospasm (<2%), dyspnea on exertion (<2%)
<1%, postmarketing, and/or case reports: Angioedema, DRESS syndrome, erythema multiforme, hemorrhagic stroke, lipodystrophy, rhabdomyolysis, Stevens-Johnson syndrome, toxic epidermal necrolysis
Warnings/Precautions
Concerns related to adverse effects:
- Fat redistribution: May cause redistribution of fat (eg, buffalo hump, peripheral wasting with increased abdominal girth, cushingoid appearance).
- Immune reconstitution syndrome: Patients may develop immune reconstitution syndrome, resulting in the occurrence of an inflammatory response to an indolent or residual opportunistic infection during initial HIV treatment or activation of autoimmune disorders (eg, Graves disease, polymyositis, Guillain-Barré syndrome, autoimmune hepatitis) later in therapy; further evaluation and treatment may be required.
- Skin reactions/hypersensitivity: Severe and possibly life-threatening skin reactions (including Stevens-Johnson syndrome, toxic epidermal necrolysis, and erythema multiforme) and hypersensitivity reactions ranging from rash (including grades 3/4 rash and drug rash with eosinophilia and systemic symptoms) and/or constitutional symptoms to occasional organ dysfunction (including hepatic failure) have been reported. Rash occurs most commonly in the first 6 weeks of therapy and is more frequent in females. Discontinue immediately with signs or symptoms of severe skin reaction or hypersensitivity.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Appropriate use: Not for use in treatment-naive patients, or experienced patients without evidence of viral mutations conferring resistance to nonnucleoside reverse transcriptase inhibitors and protease inhibitors.
Monitoring Parameters
Viral load, CD4 count, cholesterol, triglycerides, hepatic transaminases (if signs or symptoms of hypersensitivity develop); signs of skin rash, signs and symptoms of infection
Pregnancy
Pregnancy Considerations
Etravirine has a variable (moderate to high) level of transfer across the human placenta.
Only limited data have been reported to the antiretroviral pregnancy registry and information is insufficient to evaluate teratogenic effects in humans. Maternal antiretroviral therapy (ART) may be associated with adverse pregnancy outcomes, including preterm delivery, stillbirth, low birth weight, and small for gestational age infants. Actual risks may be influenced by maternal factors, such as disease severity, gestational age at initiation of therapy, and specific ART regimen; therefore, close fetal monitoring is recommended. Because there is clear benefit to appropriate treatment, maternal ART should not be withheld due to concerns for adverse neonatal outcomes. Long-term follow-up is recommended for all infants exposed to antiretroviral medications; children without HIV but who were exposed to ART in utero and develop significant organ system abnormalities of unknown etiology (particularly of the CNS or heart) should be evaluated for potential mitochondrial dysfunction. Hypersensitivity reactions (including hepatic toxicity and rash) are more common in women on nonnucleoside reverse transcriptase inhibitor therapy; it is not known if pregnancy increases this risk.
The Health and Human Services (HHS) perinatal HIV guidelines do not recommend use in antiretroviral-naive pregnant females; use is not recommended (except in special circumstances) in pregnant females who have had ART therapy in the past but are restarting, who require a new ART regimen (due to poor tolerance or poor virologic response of current regimen), and who are not yet pregnant but are trying to conceive. In addition, females who become pregnant while taking etravirine may continue if viral suppression is effective and the regimen is well tolerated. The pharmacokinetics of etravirine are not significantly altered in pregnancy and dosing adjustment is not needed (limited data).
In general, ART is recommended for all pregnant females living with HIV to keep the viral load below the limit of detection and reduce the risk of perinatal transmission. Therapy should be individualized following a discussion of the potential risks and benefits of treatment during pregnancy. Monitoring of pregnant females is more frequent than in nonpregnant adults. ART should be continued postpartum for all females living with HIV and can be modified after delivery.
Health care providers are encouraged to enroll pregnant females exposed to antiretroviral medications as early in pregnancy as possible in the Antiretroviral Pregnancy Registry (1-800-258-4263 or http://www.APRegistry.com). Health care providers caring for pregnant females living with HIV and their infants may contact the National Perinatal HIV Hotline (888-448-8765) for clinical consultation (HHS [perinatal] 2019).
Patient Education
What is this drug used for?
- It is used to treat HIV infection.
Frequently reported side effects of this drug
- Diarrhea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Infection
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin
- Severe loss of strength and energy
- Burning or numbness feeling
- Eye irritation
- Mouth sores
- Severe dizziness
- Passing out
- Muscle pain
- Joint pain
- Shortness of breath
- Change in body fat
- Trouble swallowing
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.