Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral:
Vytorin 10/10: Ezetimibe 10 mg and simvastatin 10 mg
Vytorin 10/20: Ezetimibe 10 mg and simvastatin 20 mg
Vytorin 10/40: Ezetimibe 10 mg and simvastatin 40 mg
Vytorin 10/80: Ezetimibe 10 mg and simvastatin 80 mg
Generic: 10/10: Ezetimibe 10 mg and simvastatin 10 mg, 10/20: Ezetimibe 10 mg and simvastatin 20 mg, 10/40: Ezetimibe 10 mg and simvastatin 40 mg, 10/80: Ezetimibe 10 mg and simvastatin 80 mg
Pharmacology
Mechanism of Action
Ezetimibe: Inhibits absorption of cholesterol at the brush border of the small intestine, leading to a decreased delivery of cholesterol to the liver. Ezetimibe inhibits the enzyme Niemann-Pick C1-Like1 (NPC1L1), a sterol transporter.
Simvastatin: A methylated derivative of lovastatin that acts by competitively inhibiting 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase, the enzyme that catalyzes the rate-limiting step in cholesterol biosynthesis. In addition to the ability of HMG-CoA reductase inhibitors to decrease levels of high-sensitivity C-reactive protein (hsCRP), they also possess pleiotropic properties including improved endothelial function, reduced inflammation at the site of the coronary plaque, inhibition of platelet aggregation, and anticoagulant effects (de Denus 2002; Ray 2005).
Use: Labeled Indications
Homozygous familial hypercholesterolemia: As an adjunct to diet for the reduction of elevated total cholesterol (total-C) and low-density lipoprotein cholesterol (LDL-C) in patients with homozygous familial hypercholesterolemia, as an adjunct to other lipid-lowering treatments (eg, LDL apheresis), or if such treatments are unavailable
Primary hyperlipidemia: As an adjunct to diet for the reduction of elevated total-C, LDL-C, apolipoprotein B (apo B), triglycerides, and non-high-density lipoprotein cholesterol (HDL-C), and to increase HDL-C in patients with primary (heterozygous familial and nonfamilial) hyperlipidemia or mixed hyperlipidemia
Guideline recommendations:
Simvastatin: Primary and secondary prevention of atherosclerotic cardiovascular disease (ASCVD) to reduce the risk of ASCVD in select adult patients (ACC/AHA [Stone 2013]; ADA 2017a; NLA [Jacobson 2015]; USPSTF 2016). Refer to respective guideline for specific recommendations.
Limitations of use: No incremental benefit of ezetimibe/simvastatin on cardiovascular morbidity and mortality over and above that demonstrated for simvastatin has been established. Ezetimibe/simvastatin has not been studied in Fredrickson type I, III, IV, and V dyslipidemias.
Contraindications
Hypersensitivity to ezetimibe, simvastatin, or any component of this medication; coadministration with strong CYP3A4 inhibitors (eg, itraconazole, ketoconazole, posaconazole, voriconazole, HIV protease inhibitors, boceprevir, telaprevir, erythromycin, clarithromycin, telithromycin, nefazodone, cobicistat-containing products), gemfibrozil, cyclosporine, or danazol; active liver disease or unexplained persistent elevations in hepatic transaminases; pregnancy or use in women who may become pregnant; breastfeeding
Dosage and Administration
Dosing: Adult
Note: Dosing limitation: Simvastatin 80 mg is limited to patients that have been taking this dose for >12 consecutive months without evidence of myopathy and are not currently taking or beginning a simvastatin dose-limiting or contraindicated interacting medication. If patient is unable to achieve low-density lipoprotein-cholesterol (LDL-C) goal using the 40 mg dose of simvastatin, increasing to 80 mg dose is not recommended. Instead, switch patient to an alternative LDL-C-lowering treatment providing greater LDL-C reduction. After initiation or titration, monitor lipid response after ≥2 weeks and adjust dose as necessary.
Homozygous familial hypercholesterolemia: Oral: Ezetimibe 10 mg and simvastatin 40 mg once daily in the evening.
Primary hyperlipidemia: Oral: Initial: Ezetimibe 10 mg and simvastatin 10 to 20 mg once daily in the evening. Start patients who require >55% reduction in LDL-C at ezetimibe 10 mg and simvastatin 40 mg once daily in the evening. Dosing range: Ezetimibe 10 mg and simvastatin 10 to 40 mg once daily.
Dosage adjustment with concomitant medications: Oral: Note: Patients currently tolerating and requiring a dose of simvastatin 80 mg who require initiation of an interacting drug with a dose cap for simvastatin should be switched to an alternative statin with less potential for drug-drug interaction.
Diltiazem, dronedarone, or verapamil: Simvastatin dose should not exceed 10 mg once daily.
Amiodarone, amlodipine, or ranolazine: Simvastatin dose should not exceed 20 mg once daily.
Lomitapide: Reduce simvastatin dose by 50% when initiating lomitapide. Simvastatin dose should not exceed 20 mg once daily (or 40 mg once daily for those who previously tolerated simvastatin 80 mg daily for ≥1 year without evidence of muscle toxicity).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: A lower, conservative dosing regimen may be necessary in patient populations predisposed to myopathy, including patients of Chinese descent or those concurrently receiving other lipid-lowering agents (eg, niacin, fibric acid derivatives), amiodarone, amlodipine, diltiazem, dronedarone, ranolazine, verapamil (see the following conservative, maximum adult doses)
Heterozygous familial hypercholesterolemia: Limited data available: Children ≥10 years and Adolescents (males and postmenarchal females): Oral: Initial: Ezetimibe 10 mg and simvastatin 10 to 20 mg once daily in the evening. Reported final dosing range: Ezetimibe 10 mg and simvastatin 10 to 40 mg once daily (van der Graaf, 2008); maximum dose: Ezetimibe 10 mg and simvastatin 40 mg
Dosing adjustment with concomitant medications: There are no recommendations in the manufacturer's labeling for patients <18 years. In adolescents ≥18 years, the following have been suggested:
Amiodarone or amlodipine: Maximum daily simvastatin dose: 20 mg/day
Diltiazem or verapamil: Maximum daily simvastatin dose: 10 mg/day
Administration
Oral: May be administered without regard to meals. Administer in the evening for maximal efficacy. Ezetimibe/simvastatin should be taken ≥2 hours before or ≥4 hours after administration of a bile acid sequestrant.
Dietary Considerations
Before initiation of therapy, patients should be placed on a standard cholesterol-lowering diet for 3 to 6 months and the diet should be continued during drug therapy. Simvastatin serum concentration may be increased when taken with grapefruit juice; avoid concurrent intake of grapefruit juice.
Red yeast rice contains variable amounts of several compounds that are structurally similar to HMG-CoA reductase inhibitors, primarily monacolin K (or mevinolin) which is structurally identical to lovastatin; concurrent use of red yeast rice with HMG-CoA reductase inhibitors may increase the incidence of adverse and toxic effects (Lapi 2008; Smith 2003).
Storage
Store at 20°C to 25°C (68°F to 77°F).
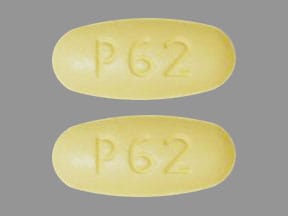
Ezetimibe and Simvastatin Images
Drug Interactions
Acipimox: May enhance the myopathic (rhabdomyolysis) effect of HMG-CoA Reductase Inhibitors (Statins). Monitor therapy
Amiodarone: May increase the serum concentration of Simvastatin. Management: Consider using a non-interacting statin (pravastatin) in patients on amiodarone. If combined, limit the adult simvastatin dose to 20 mg daily and monitor for evidence of simvastatin toxicities (eg, myalgia, liver function test elevations, rhabdomyolysis). Consider therapy modification
AmLODIPine: May increase the serum concentration of Simvastatin. Management: Avoid the concurrent use of amlodipine with simvastatin when possible. If used together, avoid doses of simvastatin greater than 20 mg/day (for adults). Consider therapy modification
Aprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Asunaprevir: May increase the serum concentration of HMG-CoA Reductase Inhibitors (Statins). Monitor therapy
Azithromycin (Systemic): May enhance the myopathic (rhabdomyolysis) effect of Simvastatin. Monitor therapy
Bezafibrate: May enhance the adverse/toxic effect of Ezetimibe. Specifically, the risk of myopathy and cholelithiasis may be increased. Avoid combination
Bile Acid Sequestrants: May decrease the absorption of Ezetimibe. Management: Administer ezetimibe at least 2 hours before or 4 hours after any bile acid sequestrant. Consider therapy modification
Bosentan: May decrease the serum concentration of Simvastatin. Monitor therapy
Cilostazol: May increase the serum concentration of Simvastatin. Monitor therapy
Ciprofibrate: May enhance the adverse/toxic effect of HMG-CoA Reductase Inhibitors (Statins). Management: Avoid the use of HMG-CoA reductase inhibitors and ciprofibrate if possible. If concomitant therapy is considered, benefits should be carefully weighed against the risks, and patients should be monitored closely for signs/symptoms of muscle toxicity. Consider therapy modification
Clarithromycin: May increase the serum concentration of Simvastatin. Avoid combination
Clofazimine: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Colchicine: May enhance the myopathic (rhabdomyolysis) effect of HMG-CoA Reductase Inhibitors (Statins). Colchicine may increase the serum concentration of HMG-CoA Reductase Inhibitors (Statins). Consider therapy modification
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
CycloSPORINE (Systemic): May increase the serum concentration of Simvastatin. Avoid combination
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May increase the metabolism of CYP3A4 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
CYP3A4 Inhibitors (Moderate): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CYP3A4 Inhibitors (Strong): May increase the serum concentration of Simvastatin. Avoid combination
Cyproterone: May increase the serum concentration of HMG-CoA Reductase Inhibitors (Statins). Management: Avoid use of statins metabolized by CYP3A4 (eg, simvastatin) and consider avoiding fluvastatin as well in patients receiving high dose cyproterone (300 mg/day). Consider use of pravastatin, rosuvastatin, or pitavastatin if statin therapy is needed. Consider therapy modification
Dabigatran Etexilate: Simvastatin may enhance the anticoagulant effect of Dabigatran Etexilate. Monitor therapy
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Daclatasvir: May increase the serum concentration of HMG-CoA Reductase Inhibitors (Statins). Monitor therapy
Danazol: May increase the serum concentration of Simvastatin. Avoid combination
DAPTOmycin: Simvastatin may enhance the adverse/toxic effect of DAPTOmycin. Avoid combination
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
DilTIAZem: Simvastatin may increase the serum concentration of DilTIAZem. DilTIAZem may increase the serum concentration of Simvastatin. Management: Avoid concurrent use of diltiazem with simvastatin when possible. If used together, limit adult doses to simvastatin 10 mg/day and diltiazem 240 mg/day; avoid Simcor (simvastatin/niacin) because fixed simvastatin doses exceed the maximum. Consider therapy modification
Dronedarone: May increase the serum concentration of Simvastatin. Management: Limit simvastatin to a max of 10 mg/day (in adults). Increase monitoring for signs of simvastatin toxicity (e.g., myositis, rhabdomyolysis). Consider therapy modification
Duvelisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Efavirenz: May decrease the serum concentration of Simvastatin. Monitor therapy
Elbasvir: May increase the serum concentration of Simvastatin. Monitor therapy
Eltrombopag: May increase the serum concentration of OATP1B1/1B3 (SLCO1B1/1B3) Substrates. Monitor therapy
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Erythromycin (Systemic): May increase the serum concentration of Simvastatin. Avoid combination
Eslicarbazepine: May decrease the serum concentration of Simvastatin. Monitor therapy
Etravirine: May decrease the serum concentration of HMG-CoA Reductase Inhibitors (Statins). This applies to atorvastatin, lovastatin and simvastatin. Monitor therapy
Fenofibrate and Derivatives: May enhance the adverse/toxic effect of Ezetimibe. Specifically, the risk of myopathy and cholelithiasis may be increased. Monitor therapy
Fluconazole: May increase the serum concentration of Simvastatin. Monitor therapy
Fosaprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosnetupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosphenytoin: May decrease the serum concentration of HMG-CoA Reductase Inhibitors (Statins). Consider therapy modification
Fostamatinib: May increase the serum concentration of Simvastatin. Monitor therapy
Fusidic Acid (Systemic): May enhance the adverse/toxic effect of HMG-CoA Reductase Inhibitors (Statins). Specifically, the risk for muscle toxicities, including rhabdomyolysis may be significantly increased. Management: Avoid concurrent use whenever possible. Use is listed as contraindicated in product characteristic summaries in several countries, although UK labeling suggests that use could be considered under exceptional circumstances and with close supervision. Avoid combination
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Gemfibrozil: May enhance the myopathic (rhabdomyolysis) effect of Simvastatin. Gemfibrozil may increase the serum concentration of Simvastatin. Concentrations of the active simvastatin acid metabolite may also be increased by gemfibrozil. Avoid combination
Gemfibrozil: May enhance the adverse/toxic effect of Ezetimibe. Specifically, the risk of myopathy and cholelithiasis may be increased. Gemfibrozil may increase the serum concentration of Ezetimibe. Avoid combination
Glecaprevir and Pibrentasvir: May increase the serum concentration of Simvastatin. Avoid combination
Grapefruit Juice: May increase the serum concentration of Simvastatin. Avoid combination
Grazoprevir: May increase the serum concentration of Simvastatin. Monitor therapy
Green Tea: May increase the serum concentration of Simvastatin. Specifically, Simvastatin lactone concentrations may be increased. Monitor therapy
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Imatinib: May decrease the metabolism of Simvastatin. Monitor therapy
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Lanthanum: HMG-CoA Reductase Inhibitors (Statins) may decrease the serum concentration of Lanthanum. Management: Administer HMG-CoA reductase inhibitors at least two hours before or after lanthanum. Consider therapy modification
Larotrectinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Lercanidipine: May increase the serum concentration of Simvastatin. Management: Administer lercanidipine in the morning and simvastatin in the evening in patients receiving these drugs in combination. Consider therapy modification
Letermovir: May increase the serum concentration of Simvastatin. Avoid combination
Levamlodipine: May increase the serum concentration of Simvastatin. Management: Avoid the concurrent use of amlodipine with simvastatin when possible. If used together, avoid doses of simvastatin greater than 20 mg/day (for adults). Consider therapy modification
Lomitapide: May increase the serum concentration of Simvastatin. Management: Reduce the recommended simvastatin dose by 50%. Generally, limit the maximum adult simvastatin dose to 20 mg/day. A 40 mg/day dose can be considered in patients who previously received 80 mg/day for at least a year without evidence of muscle toxicity. Consider therapy modification
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
MiFEPRIStone: May increase the serum concentration of Simvastatin. Management: Avoid simvastatin during and 2 weeks following mifepristone for treatment of hyperglycemia in Cushing's syndrome. The interaction magnitude could be lower with single doses used to terminate pregnancy, but neither effect has been studied clinically. Avoid combination
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Netupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Niacin: May enhance the myopathic (rhabdomyolysis) effect of Simvastatin. Niacin may increase the serum concentration of Simvastatin. Management: Use of simvastatin with niacin should be avoided in Chinese patients; some non-US labeling state this combination is not recommended in any Asian patients. Consider therapy modification
Niacinamide: May enhance the adverse/toxic effect of HMG-CoA Reductase Inhibitors (Statins). Monitor therapy
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
PAZOPanib: Simvastatin may enhance the adverse/toxic effect of PAZOPanib. Specifically, the risk for ALT/AST elevations may be increased. Monitor therapy
Phenytoin: May decrease the serum concentration of HMG-CoA Reductase Inhibitors (Statins). Consider therapy modification
Protease Inhibitors: May increase the serum concentration of Simvastatin. Avoid combination
QuiNINE: May increase the serum concentration of HMG-CoA Reductase Inhibitors (Statins). Monitor therapy
Raltegravir: May enhance the myopathic (rhabdomyolysis) effect of HMG-CoA Reductase Inhibitors (Statins). Monitor therapy
Ranolazine: May increase the serum concentration of Simvastatin. Management: Avoid the concurrent use of ranolazine with simvastatin when possible. If used together, avoid doses of simvastatin greater than 20 mg/day. Consider therapy modification
Red Yeast Rice: May enhance the adverse/toxic effect of HMG-CoA Reductase Inhibitors (Statins). Avoid combination
Repaglinide: HMG-CoA Reductase Inhibitors (Statins) may increase the serum concentration of Repaglinide. Monitor therapy
Rifamycin Derivatives: May decrease the serum concentration of HMG-CoA Reductase Inhibitors (Statins). Management: Consider use of noninteracting antilipemic agents (note: pitavastatin concentrations may increase with rifamycin treatment). Monitor for altered HMG-CoA reductase inhibitor effects. Rifabutin and fluvastatin, or possibly pravastatin, may pose lower risk. Consider therapy modification
Rupatadine: May enhance the adverse/toxic effect of HMG-CoA Reductase Inhibitors (Statins). Specifically, the risk for increased CPK and/or other muscle toxicities may be increased. Monitor therapy
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: May increase the serum concentration of Simvastatin. Monitor therapy
St John's Wort: May increase the metabolism of HMG-CoA Reductase Inhibitors (Statins). Management: Consider avoiding the concomitant administration of St Johns Wort with interacting HMG-CoA reductase inhibitors in order to avoid the potential for decreased antilipemic effects. Monitor for decreased effects during concomitant therapy. Consider therapy modification
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
Telithromycin: May increase the serum concentration of Simvastatin. Avoid combination
Teriflunomide: May increase the serum concentration of OATP1B1/1B3 (SLCO1B1/1B3) Substrates. Monitor therapy
Ticagrelor: May increase the serum concentration of Simvastatin. Management: Avoid using doses of simvastatin greater than 40 mg/day with ticagrelor. This specific recommendation is found in the U.S. prescribing information but not in the Canadian product monograph. Consider therapy modification
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Tolvaptan: May increase the serum concentration of OATP1B1/1B3 (SLCO1B1/1B3) Substrates. Consider therapy modification
Trabectedin: HMG-CoA Reductase Inhibitors (Statins) may enhance the myopathic (rhabdomyolysis) effect of Trabectedin. Monitor therapy
Verapamil: May increase the serum concentration of Simvastatin. Management: Avoid concurrent use of verapamil with simvastatin when possible. If used together, limit adult maximum simvastatin dose to 10 mg/day, and avoid Simcor (simvastatin/niacin) because fixed simvastatin doses in the product exceed this maximum. Consider therapy modification
Vitamin K Antagonists (eg, warfarin): HMG-CoA Reductase Inhibitors (Statins) may enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Voxilaprevir: May increase the serum concentration of HMG-CoA Reductase Inhibitors (Statins). Management: Use the lowest statin dose possible if combined with voxilaprevir and monitor patients for increased statin effects/toxicities. Avoid concomitant use of voxilaprevir with rosuvastatin or pitavastatin, and limit pravastatin doses to 40 mg daily. Consider therapy modification
Adverse Reactions
Incidences refer to combination, Vytorin. Also see individual agents.
1% to 10%:
Central nervous system: Headache (6%)
Gastrointestinal: Diarrhea (3%)
Hepatic: Increased serum ALT (4%)
Infection: Influenza (2%)
Neuromuscular & skeletal: Myalgia (4%), limb pain (2%), myopathy
Respiratory: Upper respiratory infection (4%)
Warnings/Precautions
Concerns related to adverse effects:
- Diabetes mellitus: Increases in HbA1c and fasting blood glucose have been reported with HMG-CoA reductase inhibitors; however, the benefits of statin therapy far outweigh the risk of dysglycemia.
- Hepatotoxicity: Postmarketing reports of fatal and nonfatal hepatic failure are rare. If serious hepatotoxicity with clinical symptoms and/or hyperbilirubinemia or jaundice occurs during treatment, interrupt therapy. If an alternate etiology is not identified, do not restart simvastatin. Liver enzyme tests should be obtained at baseline and as clinically indicated; routine periodic monitoring of liver enzymes is not necessary. Ethanol may enhance the potential of adverse hepatic effects; instruct patients to avoid excessive ethanol consumption.
- Immune-mediated necrotizing myopathy (IMNM): IMNM, an autoimmune-mediated myopathy, has been reported (rarely) with HMG-CoA reductase inhibitor therapy. IMNM presents as proximal muscle weakness with elevated CPK levels, which persists despite discontinuation of HMG-CoA reductase inhibitor therapy; additionally, muscle biopsy may show necrotizing myopathy with limited inflammation. Immunosuppressive therapy (eg, corticosteroids, azathioprine) may be used for treatment.
- Myopathy/rhabdomyolysis: Patients receiving HMG-CoA reductase inhibitors have developed rhabdomyolysis with acute renal failure and/or myopathy; patients should be monitored closely. This risk is dose-related and is increased with high doses (simvastatin 80 mg), concurrent use of other lipid-lowering medications (fibric acid derivatives, or niacin at doses ≥1 g/day), other interacting drugs (eg, moderate-to-strong CYP3A4 inhibitors), age ≥65 years, female gender, uncontrolled hypothyroidism, and renal dysfunction. Use with caution in patients taking other drugs associated with myopathy (eg, colchicine); these patients are predisposed to myopathy. Myopathy and rhabdomyolysis also have been reported with ezetimibe monotherapy. Patients should be instructed to report unexplained muscle pain, tenderness, weakness, or brown urine.
Disease-related concerns:
- Ethanol: Use caution in patients who consume large amounts of alcohol and/or who have a past history of liver disease.
- Hepatic impairment: Use is contraindicated with active liver disease and with unexplained transaminase elevations.
- Renal impairment: Avoid use in patients with severe renal impairment (creatinine clearance not defined) unless patient has already tolerated simvastatin at a dose ≥5 mg; use doses of simvastatin >20 mg/day with caution and monitor closely for adverse events (eg, myopathy) in patients with moderate-to-severe renal impairment (ie, CrCl <60 mL/minute/1.73 m2). Initial dosage adjustment is not necessary in mild-to-moderate impairment. Renal impairment may also increase risk for myopathy.
Concurrent drug therapy issues:
- High potential for interactions: Use is contraindicated in patients taking strong CYP3A4 inhibitors, cyclosporine, danazol, and gemfibrozil (see Drug Interactions); if concurrent use of a contraindicated interacting medication is unavoidable, treatment with simvastatin should be suspended during use or consider the use of an alternative HMG-CoA reductase inhibitor void of CYP3A4 metabolism. Use caution and/or limit dose with amiodarone, amlodipine, diltiazem, ranolazine, verapamil, other fibrates, and lipid-lowering doses of niacin (≥1g/day).
Special populations:
- Children: Coadministration of ezetimibe with simvastatin at dosages of more than 40 mg/day has not been studied in adolescents. Also, ezetimibe/simvastatin has not been studied in patients <10 years of age or in premenarchal girls.
- Chinese patients: Increased risk of myopathy; use with caution. Coadministration of ezetimibe/simvastatin with niacin ≥1 g/day is not recommended in Chinese patients; it is not known if this also applies to other Asian patients.
- Elderly: Use with caution in patients ≥65 years of age; these patients are predisposed to myopathy.
- Surgical patients: The manufacturer recommends temporary discontinuation for elective major surgery, acute medical or surgical conditions, or in any patient experiencing an acute or serious condition predisposing to renal failure (eg, sepsis, hypotension, trauma, uncontrolled seizures). Based on current research and clinical guidelines (Fleisher, 2009), HMG-CoA reductase inhibitors should be continued in the perioperative period. Postoperative discontinuation of statin therapy is associated with an increased risk of cardiac morbidity and mortality.
Other warnings/precautions:
- Hyperlipidemia: Secondary causes of hyperlipidemia should be ruled out prior to therapy.
Monitoring Parameters
2013 ACC/AHA Blood Cholesterol Guideline recommendations (ACC/AHA [Stone 2013]):
Lipid panel (total cholesterol, HDL, LDL, triglycerides): Baseline lipid panel; fasting lipid profile within 4 to 12 weeks after initiation or dose adjustment and every 3 to 12 months (as clinically indicated) thereafter. If 2 consecutive LDL levels are <40 mg/dL, consider decreasing the dose.
Hepatic transaminase levels: Baseline measurement of hepatic transaminase levels (ie, ALT); measure hepatic function if symptoms suggest hepatotoxicity (eg, unusual fatigue or weakness, loss of appetite, abdominal pain, dark-colored urine or yellowing of skin or sclera) during therapy.
CPK: CPK should not be routinely measured. Baseline CPK measurement is reasonable for some individuals (eg, family history of statin intolerance or muscle disease, clinical presentation, concomitant drug therapy that may increase risk of myopathy). May measure CPK in any patient with symptoms suggestive of myopathy (pain, tenderness, stiffness, cramping, weakness, or generalized fatigue).
Evaluate for new-onset diabetes mellitus during therapy; if diabetes develops, continue statin therapy and encourage adherence to a heart-healthy diet, physical activity, a healthy body weight, and tobacco cessation.
If patient develops a confusional state or memory impairment, may evaluate patient for nonstatin causes (eg, exposure to other drugs), systemic and neuropsychiatric causes, and the possibility of adverse effects associated with statin therapy.
Manufacturer's labeling: Baseline liver function tests and repeat when clinically indicated thereafter. Upon initiation or titration, lipid panel should be analyzed after ≥2 weeks.
Pregnancy
Pregnancy Risk Factor
X
Pregnancy Considerations
Use is contraindicated in pregnant women or women who may become pregnant. See individual monographs for additional information.
Patient Education
What is this drug used for?
- It is used to lower bad cholesterol and raise good cholesterol (HDL).
- It is used to lower triglycerides.
Frequently reported side effects of this drug
- Headache
- Common cold symptoms
- Diarrhea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin
- Unable to pass urine
- Change in amount of urine passed
- Muscle pain
- Muscle tenderness
- Muscle weakness
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.