Boxed Warning
Aplastic anemia:
The use of felbamate is associated with a marked increase in the incidence of aplastic anemia. Accordingly, felbamate should only be used in patients whose epilepsy is so severe that the risk of aplastic anemia is deemed acceptable in light of the benefits conferred by its use. Ordinarily, a patient should not be placed on and/or continued on felbamate without consideration of appropriate expert hematologic consultation.
Among felbamate-treated patients, aplastic anemia (pancytopenia in the presence of a bone marrow largely depleted of hematopoietic precursors) occurs at an incidence that may be more than a 100-fold greater than that seen in the untreated population (ie, 2 to 5 per million persons per year). The risk of death in patients with aplastic anemia generally varies as a function of its severity and etiology; current estimates of the overall case fatality rate are in the range of 20% to 30%, but rates as high as 70% have been reported in the past.
There are too few felbamate-associated cases, and too little known about them to provide a reliable estimate of the syndrome's incidence or its case fatality rate or to identify the factors, if any, that might conceivably be used to predict who is at greater or lesser risk.
In managing patients on felbamate, the clinical manifestation of aplastic anemia may not be seen until after a patient has been taking felbamate for several months (eg, onset of aplastic anemia among felbamate-exposed patients for whom data are available has ranged from 5 to 30 weeks). However, the injury to bone marrow stem cells that is held to be ultimately responsible for the anemia may occur weeks to months earlier. Accordingly, patients who are discontinued from felbamate remain at risk for developing anemia for a variable, and unknown, period afterwards.
It is not known whether the risk of developing aplastic anemia changes with duration of exposure. Consequently, it is not safe to assume that a patient who has been on felbamate without signs of hematologic abnormality for long periods of time is without risk.
It is not known whether the dose of felbamate affects the incidence of aplastic anemia.
It is not known whether concomitant use of antiepileptic drugs (AEDs) and/or other drugs affects the incidence of aplastic anemia.
Aplastic anemia typically develops without premonitory clinical or laboratory signs; the full blown syndrome presents with signs of infection, bleeding, or anemia. Accordingly, routine blood testing cannot be reliably used to reduce the incidence of aplastic anemia, but, it will, in some cases, allow the detection of the hematologic changes before the syndrome declares itself clinically. Discontinue felbamate if any evidence of bone marrow depression occurs.
Hepatic failure:
Evaluation of postmarketing experience suggests that acute liver failure is associated with the use of felbamate. The reported rate in the United States has been approximately 6 cases of liver failure leading to death or transplant per 75,000 patient-years of use. This rate is an underestimate because of underreporting, and the true rate could be considerably greater than this. For example, if the reporting rate is 10%, the true rate would be 1 case per 1,250 patient-years of use.
Of the cases reported, approximately 67% resulted in death or liver transplantation, usually within 5 weeks of the onset of signs and symptoms of liver failure. The earliest onset of severe hepatic dysfunction followed subsequently by liver failure was 3 weeks after initiation of felbamate. Although some reports described dark urine and nonspecific prodromal symptoms (eg, anorexia, malaise, GI symptoms), in other reports it was not clear if any prodromal symptoms preceded the onset of jaundice.
It is not known whether the risk of developing hepatic failure changes with duration of exposure.
It is not known whether the dosage of felbamate affects the incidence of hepatic failure.
It is not known whether concomitant use of other AEDs and/or other drugs affects the incidence of hepatic failure.
Felbamate should not be prescribed for anyone with a history of hepatic dysfunction.
Treatment with felbamate should be initiated only in individuals without active liver disease and with normal baseline serum transaminases. It has not been proved that periodic serum transaminase testing will prevent serious injury, but it is generally believed that early detection of drug-induced hepatic injury along with immediate withdrawal of the suspect drug enhances the likelihood for recovery. There is no information available that documents how rapidly patients can progress from normal liver function to liver failure, but other drugs known to be hepatotoxins can cause liver failure rapidly (eg, from normal enzymes to liver failure in 2 to 4 weeks). Accordingly, monitoring of serum transaminase levels (AST and ALT) is recommended at baseline and periodically thereafter. While more frequent monitoring increases the chances of early detection, the precise schedule for monitoring is a matter of clinical judgment.
Discontinue felbamate if serum AST or serum ALT levels become increased at least 2 times the upper limit of normal, or if clinical signs and symptoms suggest liver failure. Patients who develop evidence of hepatocellular injury while taking felbamate and are withdrawn from the drug for any reason should be presumed to be at increased risk for liver injury if felbamate is reintroduced. Accordingly, such patients should not be considered for re-treatment.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Suspension, Oral:
Felbatol: 600 mg/5 mL (237 mL, 946 mL)
Generic: 600 mg/5 mL (237 mL, 240 mL, 473 mL, 946 mL)
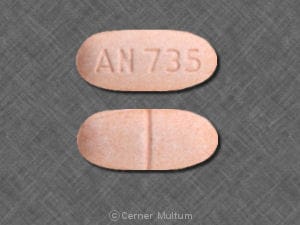
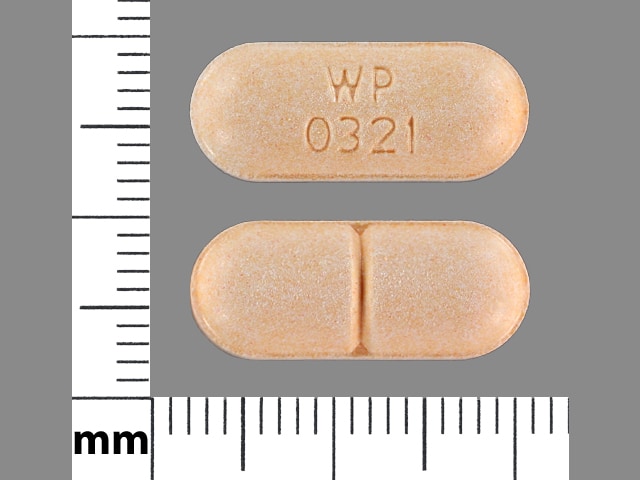
Tablet, Oral:
Felbatol: 400 mg, 600 mg [scored]
Generic: 400 mg, 600 mg
Pharmacology
Mechanism of Action
Mechanism of action is unknown but has properties in common with other marketed anticonvulsants; has weak inhibitory effects on GABA-receptor binding, benzodiazepine receptor binding, and is devoid of activity at the MK-801 receptor binding site of the NMDA receptor-ionophore complex.
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid and almost complete; food has no effect upon the tablet's absorption
Distribution
Vd: 0.7 to 0.91 L/kg (Patsalos 2018).
Excretion
Urine (40% to 50% as unchanged drug, 40% as inactive metabolites)
Clearance: Decreased in renal impairment (40% to 50%). Clearance faster in children than adults (20% to 65%) (Perucca 2006), particularly younger children (Carmant 1994)
Children 2 to 9 years: 61.3 ± 8.2 mL/kg/hour
Children 10 to 12 years: 34.3 ± 4.3 mL/kg/hour
Time to Peak
Serum: 2 to 6 hours (Patsalos 2018).
Half-Life Elimination
20 to 23 hours (average); prolonged by 9 to 15 hours in patients with renal impairment
Protein Binding
22% to 48% (Patsalos 2017), primarily to albumin.
Use: Labeled Indications
Partial seizures (monotherapy or adjunctive): Monotherapy or adjunctive therapy in the treatment of partial seizures (with and without generalization) in adults and adolescents 14 years and older
Lennox-Gastaut syndrome: Adjunctive therapy in the treatment of partial and generalized seizures associated with Lennox-Gastaut syndrome in children
Limitations of use: Not indicated for use as first-line treatment
Contraindications
Hypersensitivity to felbamate, carbamates, or any component of the formulation; history of any blood dyscrasia or hepatic dysfunction
Dosage and Administration
Dosing: Adult
Partial seizures, monotherapy: Oral:
Initial: 1,200 mg/day in 3 to 4 divided doses; titrate previously untreated patients under close clinical supervision, increasing the dosage in 600 mg increments every 2 weeks to 2400 mg/day based on clinical response and thereafter to 3,600 mg/day if clinically indicated
Conversion to monotherapy: Initiate at 1,200 mg/day in 3 to 4 divided doses; reduce the dosage of the concomitant anticonvulsant(s) by 33% at the initiation of felbamate therapy; at week 2, increase the felbamate dosage to 2,400 mg/day while reducing the dosage of the other anticonvulsant(s) up to an additional 33% of their original dosage; at week 3, increase the felbamate dosage up to 3,600 mg/day and continue to reduce the dosage of the other anticonvulsant(s) as clinically indicated
Partial seizures, adjunctive therapy: Oral: Initial: 1,200 mg/day in 3 to 4 divided doses; increase once per week by 1,200 mg/day increments up to 3,600 mg/day in 3 to 4 divided doses.
Note: Decrease dose of concomitant carbamazepine (and carbamazepine metabolites), phenobarbital, phenytoin, or valproic acid by 20% when initiating felbamate therapy. Further dosage reductions may be necessary as dose of felbamate is increased.
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Anticonvulsant, adjunctive therapy: Adolescents ≥14 years: Oral: Initial: 1,200 mg/day in 3 or 4 divided doses; increase dose in 1,200 mg/day increments at weekly intervals; maximum daily dose: 3,600 mg/day. Note: At initiation of felbamate, decrease dose of concomitant carbamazepine, phenytoin, phenobarbital, or valproic acid by 20%. Further dosage reductions may be necessary as dose of felbamate is increased.
Anticonvulsant, monotherapy: Adolescents ≥14 years: Oral:
Initial: 1,200 mg/day in divided doses 3 or 4 times daily; titrate previously untreated patients under close clinical supervision, increasing the dose in 600 mg/day increments every 2 weeks to 2,400 mg/day based on clinical response and thereafter to 3,600 mg/day if clinically indicated
Conversion to monotherapy: Initial: 1,200 mg/day in divided doses 3 or 4 times daily, reduce the dosage of the concomitant anticonvulsant(s) by 33% at the initiation of felbamate therapy; at week 2, increase felbamate daily dose to 2,400 mg/day in divided doses while reducing the dosage of the other anticonvulsant(s) up to an additional 33% of their original dose; at week 3, increase the felbamate dosage up to a maximum daily dose: 3,600 mg/day and continue to reduce the dosage of the other anticonvulsant(s) as clinically indicated
Lennox-Gastaut syndrome; adjunctive therapy: Children and Adolescents 2 to 14 years: Oral: Initial: 15 mg/kg/day in 3 or 4 divided doses; increase dose by 15 mg/kg/day increments at weekly intervals; maximum daily dose: 45 mg/kg/day or 3,600 mg/day whichever is less. Note: At initiation of felbamate, decrease dose of concomitant carbamazepine, phenytoin, phenobarbital, or valproic acid by 20%. Further dosage reductions may be necessary as dose of felbamate is increased.
Administration
Administer with or without food. Shake suspension prior to use.
Storage
Store in tightly closed container at controlled room temperature of 20°C to 25°C (68°F to 77°F).
Felbamate Images
Drug Interactions
Alcohol (Ethyl): CNS Depressants may enhance the CNS depressant effect of Alcohol (Ethyl). Monitor therapy
Alizapride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Aprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Azelastine (Nasal): CNS Depressants may enhance the CNS depressant effect of Azelastine (Nasal). Avoid combination
Barbiturates: Felbamate may increase the serum concentration of Barbiturates. Barbiturates may decrease the serum concentration of Felbamate. Management: Monitor for elevated barbiturate concentrations/toxicity if felbamate is initiated/dose increased, or reduced concentrations/effects if felbamate is discontinued/dose decreased. Refer to phenobarbital dosing guidelines for patients receiving that agent. Monitor therapy
Blonanserin: CNS Depressants may enhance the CNS depressant effect of Blonanserin. Consider therapy modification
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Brexanolone: CNS Depressants may enhance the CNS depressant effect of Brexanolone. Monitor therapy
Brimonidine (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromopride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromperidol: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Buprenorphine: CNS Depressants may enhance the CNS depressant effect of Buprenorphine. Management: Consider reduced doses of other CNS depressants, and avoiding such drugs in patients at high risk of buprenorphine overuse/self-injection. Initiate buprenorphine at lower doses in patients already receiving CNS depressants. Consider therapy modification
Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Cannabis: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
CarBAMazepine: May decrease the serum concentration of Felbamate. Felbamate may decrease the serum concentration of CarBAMazepine. Management: In patients receiving carbamazepine, initiate felbamate at 1200 mg/day in divided doses 3-4 times daily while reducing carbamazepine dose by 20%. Monitor for reduced concentrations/effects of both drugs. Consider therapy modification
Chlormethiazole: May enhance the CNS depressant effect of CNS Depressants. Management: Monitor closely for evidence of excessive CNS depression. The chlormethiazole labeling states that an appropriately reduced dose should be used if such a combination must be used. Consider therapy modification
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Clofazimine: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CNS Depressants: May enhance the adverse/toxic effect of other CNS Depressants. Monitor therapy
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May increase the metabolism of CYP3A4 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
CYP3A4 Inhibitors (Moderate): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CYP3A4 Inhibitors (Strong): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Consider therapy modification
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Dimethindene (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Doxylamine: May enhance the CNS depressant effect of CNS Depressants. Management: The manufacturer of Diclegis (doxylamine/pyridoxine), intended for use in pregnancy, specifically states that use with other CNS depressants is not recommended. Monitor therapy
Dronabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Droperidol: May enhance the CNS depressant effect of CNS Depressants. Management: Consider dose reductions of droperidol or of other CNS agents (eg, opioids, barbiturates) with concomitant use. Exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Consider therapy modification
Duvelisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Esketamine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Estrogen Derivatives (Contraceptive): Felbamate may decrease the serum concentration of Estrogen Derivatives (Contraceptive). Contraceptive failure is possible. Management: Use of a nonhormonal contraceptive is recommended. Consider therapy modification
Flunitrazepam: CNS Depressants may enhance the CNS depressant effect of Flunitrazepam. Consider therapy modification
Fosaprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosnetupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosphenytoin: May decrease the serum concentration of Felbamate. Felbamate may increase the serum concentration of Fosphenytoin. Management: Decreased phenytoin dose will likely be needed when adding felbamate; some reports suggest an empiric 20% decrease in phenytoin dose. Additional reductions may be needed if felbamate dose is increased or as otherwise guided by monitoring. Consider therapy modification
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
HYDROcodone: CNS Depressants may enhance the CNS depressant effect of HYDROcodone. Management: Avoid concomitant use of hydrocodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
HydrOXYzine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Kava Kava: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Larotrectinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Lemborexant: May enhance the CNS depressant effect of CNS Depressants. Management: Dosage adjustments of lemborexant and of concomitant CNS depressants may be necessary when administered together because of potentially additive CNS depressant effects. Close monitoring for CNS depressant effects is necessary. Consider therapy modification
Lofexidine: May enhance the CNS depressant effect of CNS Depressants. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Magnesium Sulfate: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Mefloquine: May diminish the therapeutic effect of Anticonvulsants. Mefloquine may decrease the serum concentration of Anticonvulsants. Management: Mefloquine is contraindicated for malaria prophylaxis in persons with a history of convulsions. Monitor anticonvulsant concentrations and treatment response closely with concurrent use. Consider therapy modification
Methotrimeprazine: CNS Depressants may enhance the CNS depressant effect of Methotrimeprazine. Methotrimeprazine may enhance the CNS depressant effect of CNS Depressants. Management: Reduce adult dose of CNS depressant agents by 50% with initiation of concomitant methotrimeprazine therapy. Further CNS depressant dosage adjustments should be initiated only after clinically effective methotrimeprazine dose is established. Consider therapy modification
MetyroSINE: CNS Depressants may enhance the sedative effect of MetyroSINE. Monitor therapy
Mianserin: May diminish the therapeutic effect of Anticonvulsants. Monitor therapy
MiFEPRIStone: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Minimize doses of CYP3A4 substrates, and monitor for increased concentrations/toxicity, during and 2 weeks following treatment with mifepristone. Avoid cyclosporine, dihydroergotamine, ergotamine, fentanyl, pimozide, quinidine, sirolimus, and tacrolimus. Consider therapy modification
Minocycline (Systemic): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Nabilone: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Netupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Opioid Agonists: CNS Depressants may enhance the CNS depressant effect of Opioid Agonists. Management: Avoid concomitant use of opioid agonists and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Orlistat: May decrease the serum concentration of Anticonvulsants. Monitor therapy
Orphenadrine: CNS Depressants may enhance the CNS depressant effect of Orphenadrine. Avoid combination
Oxomemazine: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
OxyCODONE: CNS Depressants may enhance the CNS depressant effect of OxyCODONE. Management: Avoid concomitant use of oxycodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Paraldehyde: CNS Depressants may enhance the CNS depressant effect of Paraldehyde. Avoid combination
Perampanel: May enhance the CNS depressant effect of CNS Depressants. Management: Patients taking perampanel with any other drug that has CNS depressant activities should avoid complex and high-risk activities, particularly those such as driving that require alertness and coordination, until they have experience using the combination. Consider therapy modification
PHENobarbital: May decrease the serum concentration of Felbamate. Felbamate may increase the serum concentration of PHENobarbital. Management: In patients receiving phenobarbital, initiate felbamate at 1200 mg/day in divided doses 3-4 times daily and reduce phenobarbital dose by 20%. Monitor for increased phenobarbital concentrations/effects and decreased felbamate concentrations/effects. Consider therapy modification
Phenytoin: Felbamate may increase the serum concentration of Phenytoin. Phenytoin may decrease the serum concentration of Felbamate. Management: Decreased phenytoin dose will likely be needed when adding felbamate; some reports suggest an empiric 20% decrease in phenytoin dose. Additional reductions may be needed if felbamate dose is increased or as otherwise guided by monitoring. Consider therapy modification
Piribedil: CNS Depressants may enhance the CNS depressant effect of Piribedil. Monitor therapy
Pramipexole: CNS Depressants may enhance the sedative effect of Pramipexole. Monitor therapy
Primidone: Felbamate may increase serum concentrations of the active metabolite(s) of Primidone. Specifically, phenobarbital concentrations may increase. Primidone may decrease the serum concentration of Felbamate. Management: In patients receiving primidone, initiate felbamate at 1200 mg/day in divided doses 3-4 times daily and reduce primidone dose by 20%. Monitor for increased phenobarbital concentrations/effects and decreased felbamate concentrations/effects. Consider therapy modification
Progestins (Contraceptive): Felbamate may decrease the serum concentration of Progestins (Contraceptive). Management: Contraceptive failure is possible. Use of an alternative, nonhormonal method of contraception is recommended. Consider therapy modification
ROPINIRole: CNS Depressants may enhance the sedative effect of ROPINIRole. Monitor therapy
Rotigotine: CNS Depressants may enhance the sedative effect of Rotigotine. Monitor therapy
Rufinamide: May enhance the adverse/toxic effect of CNS Depressants. Specifically, sleepiness and dizziness may be enhanced. Monitor therapy
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Selective Serotonin Reuptake Inhibitors: CNS Depressants may enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk of psychomotor impairment may be enhanced. Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Sodium Oxybate: May enhance the CNS depressant effect of CNS Depressants. Management: Consider alternatives to combined use. When combined use is needed, consider minimizing doses of one or more drugs. Use of sodium oxybate with alcohol or sedative hypnotics is contraindicated. Consider therapy modification
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
Suvorexant: CNS Depressants may enhance the CNS depressant effect of Suvorexant. Management: Dose reduction of suvorexant and/or any other CNS depressant may be necessary. Use of suvorexant with alcohol is not recommended, and the use of suvorexant with any other drug to treat insomnia is not recommended. Consider therapy modification
Tapentadol: May enhance the CNS depressant effect of CNS Depressants. Management: Avoid concomitant use of tapentadol and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Tetrahydrocannabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Thalidomide: CNS Depressants may enhance the CNS depressant effect of Thalidomide. Avoid combination
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Trimeprazine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Ulipristal: Felbamate may decrease the serum concentration of Ulipristal. Avoid combination
Valproate Products: Felbamate may increase the serum concentration of Valproate Products. Consider therapy modification
Zolpidem: CNS Depressants may enhance the CNS depressant effect of Zolpidem. Management: Reduce the Intermezzo brand sublingual zolpidem adult dose to 1.75 mg for men who are also receiving other CNS depressants. No such dose change is recommended for women. Avoid use with other CNS depressants at bedtime; avoid use with alcohol. Consider therapy modification
Adverse Reactions
>10%:
Central nervous system: Drowsiness (children: 48%; adults: 19%), headache (adults: 7% to 37%; children: 7%), dizziness (18%), insomnia (9% to 18%), fatigue (7% to 17%), nervousness (children: 16%; adults: 7%)
Gastrointestinal: Anorexia (children: 55%; adults: 19%), vomiting (children: 39%; adults: 9% to 17%), nausea (adults: 34%; children: 7%), dyspepsia (9% to 12%), constipation (7% to 11%)
Hematologic & oncologic: Purpura (children: 13%)
Respiratory: Upper respiratory infection (children: 45%; adults: 5% to 9%)
Miscellaneous: Fever (children: 23%; adults: 3%)
1% to 10%:
Cardiovascular: Chest pain (3%), facial edema (3%), palpitations (≥1%), tachycardia (≥1%)
Central nervous system: Abnormal gait (children: 10%; adults: 5%), abnormality in thinking (children: 7%), ataxia (children: 7%; adults: 4%), emotional lability (children: 7%), pain (children: 7%), anxiety (5%), depression (5%), paresthesia (4%), stupor (3%), aggressive behavior (≥1%), agitation (≥1%), malaise (≥1%), psychological disorder (≥1%), attempted suicide (≤1%), dystonia (≤1%), euphoria (≤1%), hallucination (≤1%), migraine (≤1%)
Dermatologic: Skin rash (children: 10%; adults: 3% to 4%), acne vulgaris (3%), pruritus (≥1%), bullous rash (≤1%), urticaria (≤1%)
Endocrine and metabolic: Menstrual disease (3%), hypophosphatemia (≤3%), hypokalemia (≤1%), hyponatremia (≤1%), increased lactate dehydrogenase (≤1%)
Gastrointestinal: Hiccups (children: 10%), weight loss (children: 7%; adults: 3%), dysgeusia (6%), abdominal pain (5%), diarrhea (5%), xerostomia (3%), weight gain (≥1%), esophagitis (≤1%), increased appetite (≤1%)
Genitourinary: Urinary tract infection (3%)
Hematologic & oncologic: Leukopenia (children: 7%; adults: ≤1%), granulocytopenia (≤1%), leukocytosis (≤1%), lymphadenopathy (≤1%), thrombocytopenia (≤1%)
Hepatic: Increased liver enzymes (1% to 5%), increased serum alkaline phosphatase (≤1%)
Neuromuscular & skeletal: Tremor (6%), myalgia (3%), weakness (≥1%)
Ophthalmic: Miosis (children: 7%), diplopia (3% to 6%), visual disturbance (5%)
Otic: Otitis media (children: 10%; adults: 3%)
Respiratory: Pharyngitis (children: 10%; adults: 3%), cough (children: 7%), rhinitis (7%), sinusitis (4%), flu-like symptoms (≥1%)
<1%, postmarketing, and/or case reports: Acute renal failure, agranulocytosis, alopecia, anaphylactoid reaction, anemia, apathy, aphthous stomatitis, aplastic anemia, atrial arrhythmia, atrial fibrillation, blood coagulation disorder, blood platelet disorder, body odor, bradycardia, brain disease, buccal mucous membrane swelling, cardiac failure, cerebral edema, cerebrovascular disease, choreoathetosis, coma, confusion, delusions, diaphoresis, disseminated intravascular coagulation (DIC), dysarthria, dyskinesia, dysphagia, dyspnea, dysuria, embolism, enteritis, eosinophilia, epistaxis, exacerbation of asthma, extrapyramidal reaction, flatulence, flushing, gastric ulcer, gastritis, gastroesophageal reflux disease, gastrointestinal hemorrhage, gingival hemorrhage, glossitis, hematemesis, hematuria, hemianopia, hemolytic anemia, hepatic failure, hepatitis, hepatorenal syndrome, hyperammonemia, hyperglycemia, hypernatremia, hypersensitivity reaction, hypertension, hypocalcemia, hypoglycemia, hypomagnesemia, hypotension, hypoxia, IgA vasculitis, increased creatine phosphokinase, intestinal obstruction, jaundice, lack of concentration, leukemia, lichen planus, livedo reticularis, manic reaction, nephrosis, neuritis (mononeuritis), nystagmus, pancreatitis, pancytopenia, paralysis, paranoia, peripheral ischemia (potentially leading to necrosis), pleural effusion, pneumonitis, psychosis, pulmonary hemorrhage, rectal hemorrhage, renal insufficiency, respiratory depression, rhabdomyolysis, SIADH (syndrome of inappropriate antidiuretic hormone secretion), skin photosensitivity, status epilepticus, Stevens-Johnson syndrome, suicidal ideation, suicidal tendencies, supraventricular tachycardia, thrombophlebitis, torsades de pointes, toxic epidermal necrolysis, urinary retention, urticaria, vaginal hemorrhage
Warnings/Precautions
Concerns related to adverse effects:
- Aplastic anemia: [US Boxed Warning]: Felbamate is associated with a significant increased risk of aplastic anemia. Risk may be more than 100 fold greater than in untreated population. Current estimates of fatality are 20% to 30%, but higher rates (up to 70%) have been reported in the past. Aplastic anemia can develop at any point during therapy and for an unknown period of time after discontinuation of therapy. It is not known if dose, duration therapy, or concomitant medication use affects risk. Routine blood monitoring may be helpful in detecting hematologic changes before any clinical onset of signs/symptoms of the disease, however, aplastic anemia often develops without any prior indication or warnings. Discontinue use if any evidence of bone-marrow suppression occurs.
- Hepatic failure: [US Boxed Warning]: Has been associated with rare cases of hepatic failure (estimated >6 cases per 75,000 patients per year). Of the cases reported in the literature, 67% have resulted in fatality or liver transplant. Onset may or may not be preceded by prodromal symptoms. It is not known whether dose, duration of therapy, or concomitant medication use affects risk. Monitoring of serum transaminases has not been demonstrated to prevent serious hepatic injury, however, early diagnosis and drug withdrawal may improve the likelihood of recovery. Obtain baseline transaminase levels and periodically thereafter; discontinue use if transaminase levels increase to ≥2 times the upper limit of normal or with signs/symptoms suggesting hepatic failure. Therapy should not be initiated or reintroduced in patients with evidence of hepatic damage or who discontinue use for any reason.
- Suicidal ideation: Pooled analysis of trials involving various antiepileptics (regardless of indication) showed an increased risk of suicidal thoughts/behavior (incidence rate: 0.43% treated patients compared to 0.24% of patients receiving placebo); risk observed as early as 1 week after initiation and continued through duration of trials (most trials ≤24 weeks). Monitor all patients for notable changes in behavior that might indicate suicidal thoughts or depression; notify healthcare provider immediately if symptoms occur.
Disease-related concerns:
- Renal impairment: Use with caution in patients with renal impairment; half-life may be increased.
Concurrent drug therapy issues:
- Sedatives: CNS effects may be potentiated when used with other sedative drugs or ethanol.
Other warnings/precautions:
- Appropriate use: Not indicated for use as a first-line antiepileptic treatment; only recommended in those patients who respond inadequately to alternative treatments and whose epilepsy is so severe that a substantial risk of aplastic anemia and/or liver failure is deemed acceptable in light of the benefits conferred by its use.
- Withdrawal: Anticonvulsants should not be discontinued abruptly because of the possibility of increasing seizure frequency; therapy should be withdrawn gradually to minimize the potential of increased seizure frequency, unless safety concerns require a more rapid withdrawal.
Monitoring Parameters
Serum levels of concomitant anticonvulsant therapy; liver function tests (baseline and periodically thereafter); CBC (baseline, frequently during therapy, and for a significant period after discontinuation); suicidality (eg, suicidal thoughts, depression, behavioral changes).
Pregnancy
Pregnancy Risk Factor
C
Pregnancy Considerations
Adverse events have not been observed in animal reproduction studies. Postmarketing case reports in humans include fetal death, genital malformation, anencephaly, encephalocele, and placental disorder.
Patients exposed to felbamate during pregnancy are encouraged to enroll themselves into the North American Antiepileptic Drug (AED) Pregnancy Registry by calling 1-888-233-2334. Additional information is available at www.aedpregnancyregistry.org.
Patient Education
What is this drug used for?
- It is used to treat seizures.
Frequently reported side effects of this drug
- Dizziness
- Fatigue
- Headache
- Nausea
- Vomiting
- Lack of appetite
- Constipation
- Trouble sleeping
- Anxiety
- Diarrhea
- Common cold symptoms
- Tremors
- Abdominal pain
- Change in taste
- Weight loss
- Hiccups
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Infection
- Aplastic anemia like fever, sore throat, mouth sores, infections, bruising, or purple skin splotches
- Liver problems like dark urine, feeling tired, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin or eyes
- Confusion
- Change in balance
- Seizures
- Bruising
- Bleeding
- Vision changes
- Severe loss of strength and energy
- Depression like thoughts of suicide, anxiety, emotional instability, agitation, irritability, panic attacks, mood changes, behavioral changes, or confusion
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.