Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Capsule, Oral, as fenofibrate:
Antara: 30 mg [contains fd&c blue #2 (indigotine), fd&c yellow #10 (quinoline yellow)]
Antara: 90 mg [contains brilliant blue fcf (fd&c blue #1), fd&c yellow #10 (quinoline yellow), fd&c yellow #6 (sunset yellow)]
Lipofen: 50 mg [contains brilliant blue fcf (fd&c blue #1), fd&c blue #2 (indigotine), fd&c red #40, fd&c yellow #10 (quinoline yellow)]
Lipofen: 150 mg
Lofibra: 67 mg [DSC], 134 mg [DSC], 200 mg [DSC]
Generic: 43 mg, 50 mg, 67 mg, 130 mg, 134 mg, 150 mg, 200 mg
Capsule Delayed Release, Oral, as choline fenofibrate:
Trilipix: 45 mg
Trilipix: 135 mg [contains fd&c blue #2 (indigotine)]
Generic: 45 mg, 135 mg
Tablet, Oral, as fenofibrate:
Fenoglide: 40 mg, 120 mg
Lofibra: 54 mg [DSC] [contains fd&c yellow #10 aluminum lake]
Lofibra: 160 mg [DSC]
Tricor: 48 mg [contains fd&c blue #2 aluminum lake, fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake, soybean lecithin]
Tricor: 145 mg [contains soybean lecithin]
Triglide: 160 mg [DSC]
Triglide: 160 mg [contains egg phospholipids (egg lecithin)]
Generic: 40 mg, 48 mg, 54 mg, 120 mg, 145 mg, 160 mg
Tablet, Oral, as fenofibric acid:
Fibricor: 35 mg, 105 mg
Generic: 35 mg [DSC], 105 mg
Pharmacology
Mechanism of Action
Fenofibric acid, an agonist for the nuclear transcription factor peroxisome proliferator-activated receptor-alpha (PPAR-alpha), downregulates apoprotein C-III (an inhibitor of lipoprotein lipase) and upregulates the synthesis of apolipoprotein A-I, fatty acid transport protein, and lipoprotein lipase resulting in an increase in VLDL catabolism, fatty acid oxidation, and elimination of triglyceride-rich particles; as a result of a decrease in VLDL levels, total plasma triglycerides are reduced by 30% to 60%; modest increase in HDL occurs in some hypertriglyceridemic patients.
Pharmacokinetics/Pharmacodynamics
Absorption
Increased when taken with meals
Distribution
Widely to most tissues
Metabolism
Fenofibrate is metabolized in the tissue and plasma via esterases to the active form, fenofibric acid; undergoes inactivation by glucuronidation hepatically or renally
Excretion
Urine (~60% as metabolites); feces (25%); hemodialysis has no effect on removal of fenofibric acid from plasma
Time to Peak
2 to 8 hours
Half-Life Elimination
Half-life elimination: Fenofibric acid: Mean: 20 hours (range: 10 to 35 hours); half-life prolonged in patients with renal impairment
Protein Binding
~99%
Use in Specific Populations
Special Populations: Renal Function Impairment
In patients with severe renal impairment (CrCl ≤30 mL/minute), clearance of fenofibrate is greatly reduced. Clearance is reduced to a lesser degree in patients with mild to moderate renal impairment (CrCl 30 to 80 mL/minute).
Use: Labeled Indications
Hypercholesterolemia or mixed dyslipidemia: Adjunctive therapy to diet for the reduction of low-density lipoprotein cholesterol (LDL-C), total cholesterol (total-C), triglycerides, and apolipoprotein B (apo B), and to increase high-density lipoprotein cholesterol (HDL-C) in adults with primary hypercholesterolemia or mixed dyslipidemia (Fredrickson types IIa and IIb). Use lipid-altering agents in addition to a diet restricted in saturated fat and cholesterol when response to diet and nonpharmacological interventions alone has been inadequate.
Note: While FDA-approved for hypercholesterolemia, fenofibrate is not a first- or second-line choice; other agents may be more suitable (ACC/AHA [Stone 2013]). In addition, use is not recommended to lower LDL-C or raise HDL-C in the absence of hypertriglyceridemia.
Hypertriglyceridemia: Adjunctive therapy to diet for treatment of adult patients with severe hypertriglyceridemia (Fredrickson types IV and V hyperlipidemia).
Use: Off Label
Primary biliary cholangitiscyes
Data from a single-center, retrospective cohort study support the use of fenofibrate (in combination with ursodiol) in patients with primary biliary cholangitis (PBC) who have had an incomplete biochemical response to ursodiol monotherapy and showed significant improvement in alkaline phosphatase, a reduction in hepatic decompensation, and transplant-free survival improvement Cheung 2016. Data from a small, open-label pilot study support the use of fenofibrate (in combination with ursodiol) in patients with PBC who have had an incomplete biochemical response to ursodiol monotherapy and showed improvement in liver biochemistries (ie, alkaline phosphatase) and IgM and lowered levels of proinflammatory cytokines Levy 2011.
Based on the 2018 primary biliary cholangitis practice guidance from the American Association for the Study of Liver Disease (AASLD), fenofibrate may be considered an alternative to ursodiol in patients with PBC who have had an inadequate biochemical response to ursodiol monotherapy Lindor 2019.
Contraindications
Hypersensitivity to fenofibrate or fenofibric acid or any component of the formulation; active liver disease, including primary biliary cirrhosis and unexplained, persistent liver function abnormality; severe renal impairment or end-stage renal disease (ESRD), including those receiving dialysis; preexisting gallbladder disease; breastfeeding
Documentation of allergenic cross-reactivity for fibrates is limited. However, because of similarities in chemical structure and/or pharmacologic actions, the possibility of cross-sensitivity cannot be ruled out with certainty.
Canadian labeling: Additional contraindications (not in US labeling): Pregnancy; known photoallergy or phototoxic reaction during treatment with fibrates or ketoprofen
Lipidil EZ, Lipidil Supra: Additional contraindications: Allergy to soya lecithin, peanut or arachis oil, or related products; chronic or acute pancreatitis; patients <18 years of age; coadministration with HMG-CoA reductase inhibitors in patients with a predisposition for myopathy.
Dosage and Administration
Dosing: Adult
Note: At least 2 to 3 months of therapy is required to determine efficacy.
Hypertriglyceridemia: Oral: Initial:
Antara (micronized): 30 to 90 mg once daily; maximum dose: 90 mg/day
Fenofibrate (micronized): 43 to 130 mg once daily; maximum dose: 130 mg/day
Fenoglide: 40 to 120 mg once daily; maximum dose: 120 mg/day
Fibricor: 35 to 105 mg once daily; maximum dose: 105 mg/day
Lipidil EZ [Canadian product]: 145 mg once daily; maximum dose: 145 mg/day
Lipidil Supra [Canadian product]: 160 mg once daily; maximum dose: 200 mg/day
Lipofen: 50 to 150 mg once daily; maximum dose: 150 mg/day
Lofibra (micronized): 67 to 200 mg once daily; maximum dose: 200 mg/day
Lofibra (tablets): 54 to 160 mg once daily; maximum dose: 160 mg/day
TriCor: 48 to 145 mg once daily; maximum dose: 145 mg/day
Triglide: 160 mg once daily
Trilipix: 45 to 135 mg once daily; maximum dose: 135 mg/day
Hypercholesterolemia or mixed hyperlipidemia: Oral: Initial:
Antara (micronized): 90 mg once daily; maximum dose: 90 mg/day
Fenofibrate (micronized): 130 mg once daily; maximum dose: 130 mg/day
Fenoglide: 120 mg once daily
Fibricor: 105 mg once daily
Lipidil EZ [Canadian product]: 145 mg once daily; maximum dose: 145 mg/day
Lipidil Supra [Canadian product]: 160 mg once daily; maximum dose: 200 mg/day
Lipofen: 150 mg once daily
Lofibra (micronized): 200 mg once daily
Lofibra (tablets): 160 mg once daily
TriCor: 145 mg once daily
Triglide: 160 mg once daily
Trilipix: 135 mg once daily
Primary biliary cholangitis (off-label use): Oral: Note: For use in patients with incomplete biochemical response to ursodiol monotherapy. Do not initiate in patients with decompensated liver disease (Child-Pugh B or C) (AASLD [Lindor 2019]; Cheung 2016).
145 to 160 mg once daily in combination with ursodiol (AASLD [Lindor 2019]; Cheung 2016; Levy 2011).
Dosing: Geriatric
Oral: Initial: Adjust dosage based on renal function; additional product-specific recommendations for initial dose:
Lipidil EZ [Canadian product]: 48 mg once daily
Lofibra (micronized): 67 mg once daily
Lofibra (tablets): 54 mg once daily
Dosing: Adjustment for Toxicity
Cholelithiasis: Discontinue if gallstones are found upon gallbladder studies.
CPK elevation, myopathy, and/or myositis: Discontinue therapy if the patient develops markedly elevated CPK concentrations or if myopathy/myositis is suspected or diagnosed.
HDL-C reductions: Permanently discontinue therapy if HDL-C becomes severely depressed; monitor HDL-C concentrations until returned to baseline.
Administration
Oral:
Antara, fenofibrate (micronized), Fibricor, Lipidil EZ [Canadian product], Lofibra tablets, TriCor, Triglide, Trilipix: Administer with or without food. Swallow whole; do not open (capsules), crush, dissolve, or chew.
Lofibra (micronized) capsules: Administer with meals.
Fenoglide, Lipofen, Lipidil Supra [Canadian product], Lipidil Supra [Canadian product]: Administer with meals. Swallow whole; do not open (capsules), crush, dissolve, or chew.
Dietary Considerations
Antara, Fibricor, Lipidil EZ [Canadian product], Lofibra tablets, TriCor, Triglide, Trilipix: May be taken with or without food.
Fenoglide, Lipidil Supra [Canadian product], Lipofen, Lofibra (micronized capsules): Take with meals.
Storage
Store at 25°C (77°F); excursions are permitted between 15°C and 30°C (59°F and 86°F). Protect Fibricor, Lipofen, Lofibra, TriCor, Triglide, and Trilipix from moisture. Protect Fibricor, Lofibra tablets, Lipofen, and Triglide from light.
Lipidil EZ, Lipidil Supra [Canadian products]: Store at 15°C to 30°C (59°F to 86°F). Protect from light and moisture.
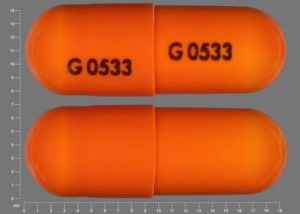
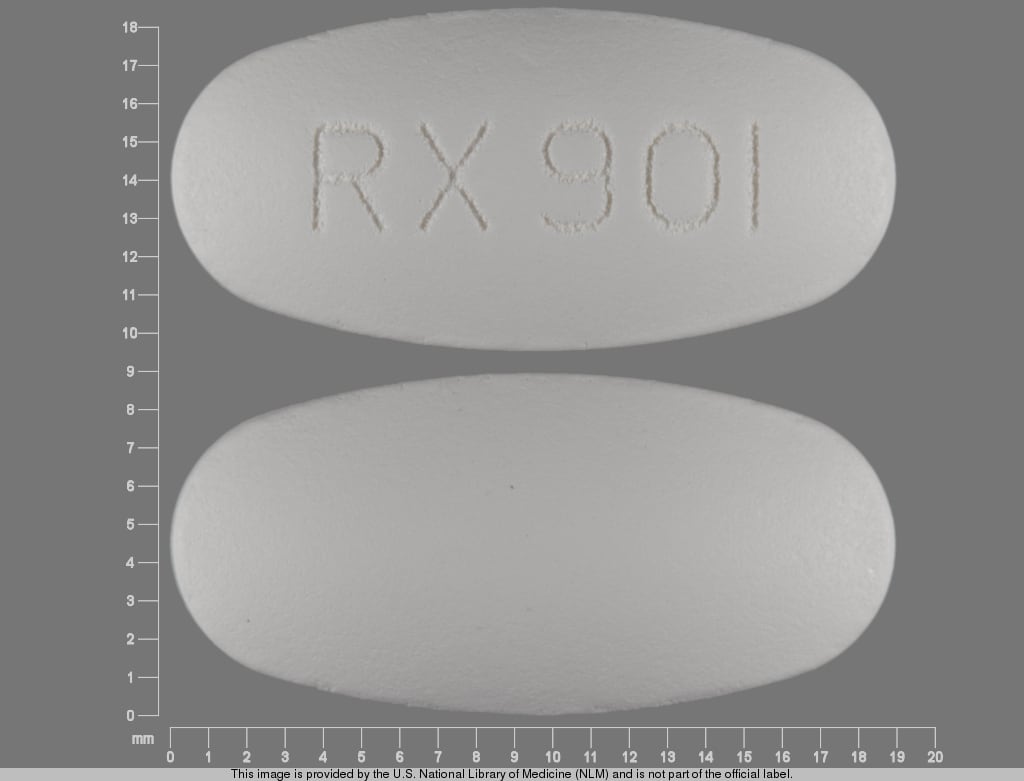
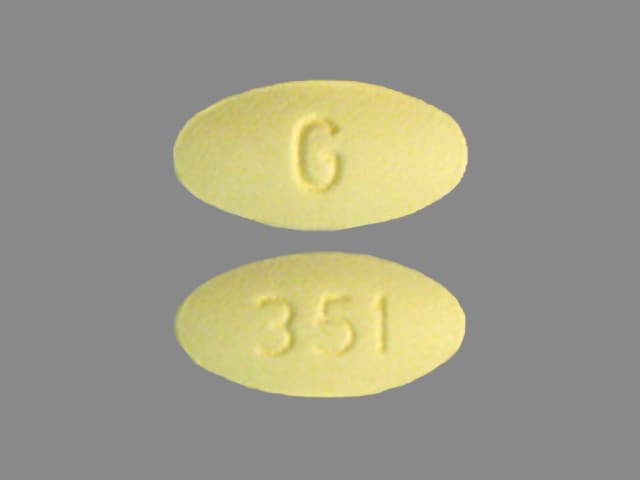
Fenofibrate and Derivatives Images
Drug Interactions
Acipimox: May enhance the myopathic (rhabdomyolysis) effect of Fibric Acid Derivatives. Monitor therapy
Bile Acid Sequestrants: May decrease the absorption of Fibric Acid Derivatives. Management: Separate doses by at least 2 hours to minimize this interaction; fenofibric acid labeling recommends administration one hour prior to or 4-6 hours after a bile acid sequestrant. Exceptions: Colesevelam. Consider therapy modification
Chenodiol: Fibric Acid Derivatives may diminish the therapeutic effect of Chenodiol. Management: Monitor clinical response to chenodiol closely when used together with any fibric acid derivative. Monitor therapy
Ciprofibrate: May enhance the adverse/toxic effect of Fibric Acid Derivatives. Avoid combination
Colchicine: Fibric Acid Derivatives may enhance the myopathic (rhabdomyolysis) effect of Colchicine. Monitor therapy
CycloSPORINE (Systemic): May enhance the nephrotoxic effect of Fibric Acid Derivatives. Fibric Acid Derivatives may decrease the serum concentration of CycloSPORINE (Systemic). Management: Careful consideration of the risks and benefits should be undertaken prior to use of this combination; extra monitoring of renal function and cyclosporine concentrations will likely be required. Adjustment of cyclosporine dose may be necessary. Consider therapy modification
Ezetimibe: Fenofibrate and Derivatives may enhance the adverse/toxic effect of Ezetimibe. Specifically, the risk of myopathy and cholelithiasis may be increased. Monitor therapy
HMG-CoA Reductase Inhibitors (Statins): Fenofibrate and Derivatives may enhance the adverse/toxic effect of HMG-CoA Reductase Inhibitors (Statins). Monitor therapy
Raltegravir: May enhance the myopathic (rhabdomyolysis) effect of Fibric Acid Derivatives. Monitor therapy
Sulfonylureas: Fibric Acid Derivatives may enhance the hypoglycemic effect of Sulfonylureas. Monitor therapy
Tacrolimus (Systemic): May enhance the nephrotoxic effect of Fenofibrate and Derivatives. Monitor therapy
Ursodiol: Fibric Acid Derivatives may diminish the therapeutic effect of Ursodiol. Monitor therapy
Vitamin K Antagonists (eg, warfarin): Fibric Acid Derivatives may enhance the anticoagulant effect of Vitamin K Antagonists. Consider therapy modification
Warfarin: Fenofibrate and Derivatives may enhance the anticoagulant effect of Warfarin. Fenofibrate and Derivatives may increase the serum concentration of Warfarin. Consider therapy modification
Adverse Reactions
>10%: Hepatic: Increased serum transaminases (≥3 x ULN: 5% to 13%)
1% to 10%:
Cardiovascular: Pulmonary embolism (≤5%), thrombophlebitis (≤5%)
Central nervous system: Dizziness (≥3%), pain (≥3%)
Dermatologic: Skin rash (1%), urticaria (1%)
Gastrointestinal: Abdominal pain (5%), diarrhea (≥3%), dyspepsia (≥3%), constipation (2%)
Hepatic: Abnormal hepatic function tests (8%), increased serum alanine aminotransferase (3%), increased serum aspartate aminotransferase (3%)
Neuromuscular & skeletal: Arthralgia (≥3%), limb pain (≥3%), myalgia (≥3%), increased creatine phosphokinase in blood specimen (3%)
Respiratory: Nasopharyngitis (≥3%), sinusitis (≥3%), upper respiratory tract infection (≥3%), rhinitis (2%)
<1%, postmarketing, and/or case reports: Acute renal failure, agranulocytosis, anaphylaxis, anemia, angioedema, asthenia, cholestatic hepatitis, chronic active hepatitis, decreased HDL cholesterol (severe), decreased hematocrit, decreased hemoglobin, decreased white blood cell count, drug reaction with eosinophilia and systemic symptoms, headache, hepatic cirrhosis, hepatitis, hepatocellular hepatitis, hypersensitivity reaction, increased serum creatinine, interstitial pulmonary disease, muscle spasm, myopathy, pancreatitis, renal failure syndrome, rhabdomyolysis, severe dermatological reaction (severe cutaneous adverse reactions [SCAR]), skin photosensitivity, Stevens-Johnson syndrome, thrombocytopenia, toxic epidermal necrolysis
Warnings/Precautions
Concerns related to adverse effects:
- Cholelithiasis: May cause cholelithiasis; discontinue if gallstones are found upon gallbladder studies.
- HDL cholesterol: A paradoxical, severe, and reversible decrease in HDL-C (as low as 2 mg/dL) with a simultaneous decrease in apolipoprotein A1 has been reported within 2 weeks to years after initiation of fibrate therapy; clinical significance unknown. Monitor HDL-C within a few months of initiation of therapy and discontinue if HDL-C becomes severely depressed; do not restart therapy.
- Hematologic effects: May cause mild-to-moderate decreases in hemoglobin, hematocrit and WBC upon initiation of therapy which usually stabilizes with long-term therapy. Agranulocytosis and thrombocytopenia have been reported. Periodic monitoring of blood counts is recommended during the first year of therapy.
- Hepatic effects: Hepatic transaminases can become significantly elevated (dose-related); hepatocellular, chronic active, and cholestatic hepatitis have been reported after weeks to several years of therapy. Baseline and regular monitoring of liver function tests is required; discontinue therapy in patients whose enzyme levels persist above 3 times the upper limit of normal.
- Hypersensitivity reactions: Acute hypersensitivity reactions, including anaphylaxis and angioedema, have been reported. Additionally, delayed hypersensitivity reactions, including severe cutaneous adverse reactions such as Stevens-Johnson syndrome (SJS), toxic epidermal necrolysis (TEN), and drug reaction with eosinophilia and systemic symptoms (DRESS) have been reported, occurring days to weeks following fenofibrate initiation. Discontinue immediately for severe acute or delayed hypersensitivity reactions.
- Myopathy/Rhabdomyolysis: Has been associated with rare myositis, myopathy, or rhabdomyolysis; monitor patients closely. Risk increased in the elderly, those receiving concomitant HMG-CoA reductase inhibitors or colchicine, and patients with diabetes mellitus, renal insufficiency, or hypothyroidism. Instruct patients to report unexplained muscle pain, tenderness, weakness, especially if accompanied with malaise or fever; or brown urine. Discontinue therapy in patients who develop markedly elevated CPK concentrations or if myopathy/myositis is suspected or diagnosed.
- Pancreatitis: Pancreatitis has been reported with fenofibrate use; may be secondary to a failure of efficacy in patients with severe hypertriglyceridemia, medication side effect, or due to biliary tract stone or sludge formation from bile duct obstruction.
- Photosensitivity: Photosensitivity reactions have been reported, sometimes days to months after therapy was initiated; some patients reported previous photosensitivity to ketoprofen.
- Renal effects: Increases in serum creatinine (>2 mg/dL) have been observed with use; clinical significance unknown. These elevations tend to return to baseline following discontinuation of fenofibrate. Fenofibrate has been shown to increase creatinine production (unknown mechanism) resulting in an equal increase of creatinuria thereby demonstrating that the increase does not reflect a reduction in creatinine clearance (Hottelart 2002). Monitor renal function in patients with renal impairment; consider monitoring renal function in patients with increased risk for developing renal impairment (eg, elderly and patients with diabetes).
- Venous thromboembolism: Use has been associated with PE and DVT. Use with caution in patients with risk factors for VTE.
Disease-related concerns:
- Cardiovascular disease: Fibric acid derivatives have not demonstrated significant efficacy in altering cardiovascular disease mortality in major clinical studies. In two large randomized controlled clinical trials, neither fenofibrate monotherapy (Keech 2005) nor the addition of fenofibrate to simvastatin (ACCORD Study Group 2010) compared to placebo were shown to reduce cardiovascular disease morbidity and mortality in patients with type 2 diabetes.
- Hepatic impairment: Contraindicated in patients with active liver disease, including primary biliary cirrhosis and unexplained persistent liver function abnormalities.
- Renal impairment: Use with caution in patients with mild to moderate renal impairment; dosage adjustment required. Contraindicated in patients with severe renal impairment including those receiving dialysis. Avoid use of Triglide in patients with mild or moderate renal impairment.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
- HMG-CoA reductase inhibitors: Use caution with HMG-CoA reductase inhibitors; may lead to myopathy, rhabdomyolysis. No incremental benefit of combination therapy on cardiovascular morbidity and mortality over statin monotherapy has been established. In combination with HMG-CoA reductase inhibitors, fenofibrate is generally regarded as safer than gemfibrozil due to limited pharmacokinetic interaction with statins. Fenofibrate may be considered in patients on low- or moderate-intensity statin therapy (ie, statin therapy intended to lower LDL-C by <30% or ~30% to 50%, respectively) only if the benefits from atherosclerotic cardiovascular disease (ASCVD) risk reduction or triglyceride lowering when triglycerides are >500 mg/dL, outweigh the potential risk for adverse effects (ACC/AHA [Stone 2013]).
Special populations:
- Elderly: Use with caution in the elderly; dosage adjustment may be required.
Dosage form specific issues:
- Peanut or arachis oil: Some products may contain peanut or arachis oil; use is contraindicated in patients with a peanut or arachis allergy for applicable formulations.
- Soya lecithin: Some products may contain soya lecithin; use is contraindicated in patients with a soya lecithin allergy for applicable formulations.
Other warnings/precautions:
- Appropriate use: Fenofibrate is not a first- or second-line choice in patients with hypercholesterolemia; other agents may be more suitable (ACC/AHA [Stone 2013]). Secondary causes of hyperlipidemia should be ruled out prior to therapy.
- Optimal response: Therapy should be withdrawn if an adequate response is not obtained after 2 to 3 months of therapy at the maximal daily dose. In patients with severe hypertriglyceridemia, the occurrence of pancreatitis may represent a failure of efficacy, a direct effect of the drug, or obstruction of the common bile duct due to biliary tract stone or sludge formation.
Monitoring Parameters
Periodic blood counts during first year of therapy. Monitor lipid profile periodically. Monitor LFTs regularly and discontinue therapy if levels remain >3 times normal limits. Monitor renal function in patients with renal impairment or in those at increased risk for developing renal impairment.
2013 ACC/AHA Blood Cholesterol Guideline recommendations (ACC/AHA [Stone 2013]): Evaluate renal status at baseline, within 3 months after initiation, and every 6 months thereafter.
Pregnancy
Pregnancy Considerations
Triglyceride and lipid concentrations increase during pregnancy as required for normal fetal development. When increases are greater than expected, supervised dietary intervention should be initiated. In women who develop very severe hypertriglyceridemia and are at risk for pancreatitis, use of fenofibrate beginning in the second trimester is one intervention that may be considered. Agents other than fenofibrate should be used for hypercholesterolemia (Avis 2009; Berglund 2012; Jacobson 2015; Wong 2015).
Patient Education
What is this drug used for?
- It is used to lower triglycerides.
- It is used to lower bad cholesterol and raise good cholesterol (HDL).
Frequently reported side effects of this drug
- Headache
- Back pain
- Abdominal pain
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Pancreatitis like severe abdominal pain, severe back pain, severe nausea, or vomiting.
- Gallstones like pain in the upper right abdominal area, right shoulder area, or between the shoulder blades; yellow skin; or fever with chills.
- Blood clots like numbness or weakness on one side of the body; pain, redness, tenderness, warmth, or swelling in the arms or legs; change in color of an arm or leg; chest pain; shortness of breath; fast heartbeat; or coughing up blood.
- Infection
- Muscle pain
- Muscle weakness
- Severe loss of strength and energy
- Severe joint pain
- Severe joint swelling
- Unable to pass urine
- Change in amount of urine passed
- Bruising
- Bleeding
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.