Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral, as hydrochloride:
Generic: 100 mg
Pharmacology
Mechanism of Action
Synthetic antispasmotic with similar actions to that of propantheline; it exerts a direct relaxant effect on smooth muscles via phosphodiesterase inhibition, providing relief to a variety of smooth muscle spasms; it is especially useful for the treatment of bladder spasticity, whereby it produces an increase in urinary capacity
Pharmacokinetics/Pharmacodynamics
Excretion
Urine (57%) within 24 hours
Onset of Action
55 minutes
Use: Labeled Indications
Antispasmodic to provide symptomatic relief of dysuria, nocturia, suprapubic pain, urgency, frequency and incontinence in patients with cystitis, urethritis, urethrocystitis, urethrotrigonitis, and prostatitis
Contraindications
Pyloric or duodenal obstruction; gastrointestinal hemorrhage; obstructive intestinal lesions; ileus; achalasia; obstructive uropathies of lower urinary tract (eg, BPH)
Dosage and Administration
Dosing: Adult
Urinary spasms: Oral: 100-200 mg 3-4 times daily; reduce the dose when symptoms improve.
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Children >12 years: Refer to adult dosing.
Storage
Store at 20°C to 25°C (68°F to 77°F). Protect from light.
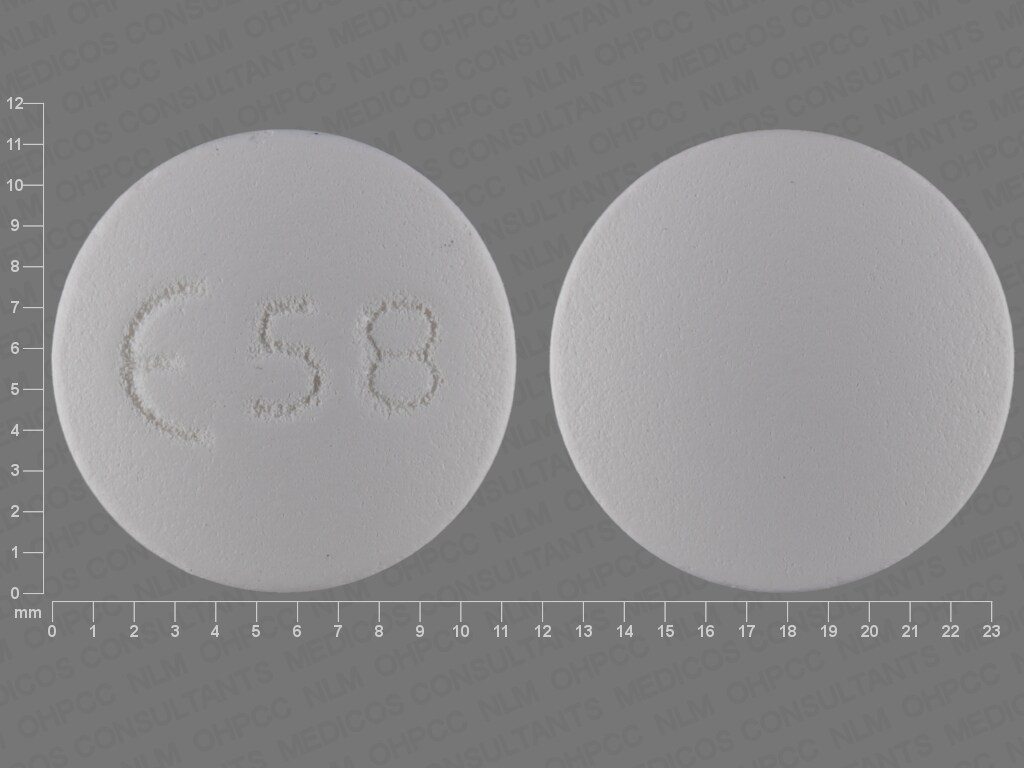
FlavoxATE Images
Drug Interactions
Acetylcholinesterase Inhibitors: May diminish the therapeutic effect of Anticholinergic Agents. Anticholinergic Agents may diminish the therapeutic effect of Acetylcholinesterase Inhibitors. Monitor therapy
Aclidinium: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Amantadine: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Anticholinergic Agents: May enhance the adverse/toxic effect of other Anticholinergic Agents. Monitor therapy
Botulinum Toxin-Containing Products: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Cannabinoid-Containing Products: Anticholinergic Agents may enhance the tachycardic effect of Cannabinoid-Containing Products. Exceptions: Cannabidiol. Monitor therapy
Chloral Betaine: May enhance the adverse/toxic effect of Anticholinergic Agents. Monitor therapy
Cimetropium: Anticholinergic Agents may enhance the anticholinergic effect of Cimetropium. Avoid combination
Eluxadoline: Anticholinergic Agents may enhance the constipating effect of Eluxadoline. Avoid combination
Gastrointestinal Agents (Prokinetic): Anticholinergic Agents may diminish the therapeutic effect of Gastrointestinal Agents (Prokinetic). Monitor therapy
Glucagon: Anticholinergic Agents may enhance the adverse/toxic effect of Glucagon. Specifically, the risk of gastrointestinal adverse effects may be increased. Monitor therapy
Glycopyrrolate (Oral Inhalation): Anticholinergic Agents may enhance the anticholinergic effect of Glycopyrrolate (Oral Inhalation). Avoid combination
Glycopyrronium (Topical): May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Ipratropium (Oral Inhalation): May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Itopride: Anticholinergic Agents may diminish the therapeutic effect of Itopride. Monitor therapy
Levosulpiride: Anticholinergic Agents may diminish the therapeutic effect of Levosulpiride. Avoid combination
Mianserin: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Mirabegron: Anticholinergic Agents may enhance the adverse/toxic effect of Mirabegron. Monitor therapy
Nitroglycerin: Anticholinergic Agents may decrease the absorption of Nitroglycerin. Specifically, anticholinergic agents may decrease the dissolution of sublingual nitroglycerin tablets, possibly impairing or slowing nitroglycerin absorption. Monitor therapy
Opioid Agonists: Anticholinergic Agents may enhance the adverse/toxic effect of Opioid Agonists. Specifically, the risk for constipation and urinary retention may be increased with this combination. Monitor therapy
Oxatomide: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Potassium Chloride: Anticholinergic Agents may enhance the ulcerogenic effect of Potassium Chloride. Management: Patients on drugs with substantial anticholinergic effects should avoid using any solid oral dosage form of potassium chloride. Avoid combination
Potassium Citrate: Anticholinergic Agents may enhance the ulcerogenic effect of Potassium Citrate. Avoid combination
Pramlintide: May enhance the anticholinergic effect of Anticholinergic Agents. These effects are specific to the GI tract. Consider therapy modification
Ramosetron: Anticholinergic Agents may enhance the constipating effect of Ramosetron. Monitor therapy
Revefenacin: Anticholinergic Agents may enhance the anticholinergic effect of Revefenacin. Avoid combination
Secretin: Anticholinergic Agents may diminish the therapeutic effect of Secretin. Management: Avoid concomitant use of anticholinergic agents and secretin. Discontinue anticholinergic agents at least 5 half-lives prior to administration of secretin. Consider therapy modification
Thiazide and Thiazide-Like Diuretics: Anticholinergic Agents may increase the serum concentration of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Tiotropium: Anticholinergic Agents may enhance the anticholinergic effect of Tiotropium. Avoid combination
Topiramate: Anticholinergic Agents may enhance the adverse/toxic effect of Topiramate. Monitor therapy
Umeclidinium: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Adverse Reactions
Frequency not defined.
Cardiovascular: Palpitations, tachycardia
Central nervous system: Confusion (especially in the elderly), drowsiness, headache, hyperpyrexia, nervousness, vertigo
Dermatologic: Rash, urticaria
Gastrointestinal: Nausea, vomiting, xerostomia
Genitourinary: Dysuria
Hematologic: Eosinophilia, leukopenia
Ocular: Blurred vision, intraocular pressure increased, ocular accommodation disorder
Warnings/Precautions
Concerns related to adverse effects:
- CNS effects: May cause CNS drowsiness and blurred vision, which may impair physical or mental abilities; patients must be cautioned about performing tasks which require mental alertness (eg, operating machinery or driving).
Disease-related concerns:
- Glaucoma: Use with caution in patients with suspected glaucoma.
Concurrent drug therapy issues:
- Sedatives: CNS effects may be potentiated when used with other sedative drugs or ethanol.
Special populations:
Monitoring Parameters
Monitor I & O closely, anticholinergic signs and symptoms
Pregnancy
Pregnancy Risk Factor
B
Pregnancy Considerations
Adverse events have not been observed in animal reproduction studies.
Patient Education
- Discuss specific use of drug and side effects with patient as it relates to treatment. (HCAHPS: During this hospital stay, were you given any medicine that you had not taken before? Before giving you any new medicine, how often did hospital staff tell you what the medicine was for? How often did hospital staff describe possible side effects in a way you could understand?)
- Patient may experience headache, fatigue, blurred vision, dry mouth, vomiting, or nausea. Have patient report immediately to prescriber severe dizziness, passing out, fast heartbeat, abnormal heartbeat, confusion, chills, sore throat, severe anxiety, vision changes, eye pain, severe eye irritation, or painful urination (HCAHPS).
- Educate patient about signs of a significant reaction (eg, wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat). Note: This is not a comprehensive list of all side effects. Patient should consult prescriber for additional questions.
Intended Use and Disclaimer: Should not be printed and given to patients. This information is intended to serve as a concise initial reference for health care professionals to use when discussing medications with a patient. You must ultimately rely on your own discretion, experience, and judgment in diagnosing, treating, and advising patients.