Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Solution, Intravenous:
Generic: 100 mg/50 mL in NaCl 0.9% (50 mL [DSC]); 200 mg (100 mL); 200 mg/100 mL in NaCl 0.9% (100 mL); 400 mg (200 mL)
Solution, Intravenous [preservative free]:
Generic: 200 mg (100 mL); 200 mg/100 mL in NaCl 0.9% (100 mL); 400 mg (200 mL); 400 mg/200 mL in NaCl 0.9% (200 mL)
Suspension Reconstituted, Oral:
Diflucan: 10 mg/mL (35 mL); 40 mg/mL (35 mL) [orange flavor]
Generic: 10 mg/mL (35 mL); 40 mg/mL (35 mL)
Tablet, Oral:
Diflucan: 50 mg, 100 mg, 150 mg, 200 mg
Generic: 50 mg, 100 mg, 150 mg, 200 mg
Pharmacology
Mechanism of Action
Interferes with fungal cytochrome P450 activity (lanosterol 14-α-demethylase), decreasing ergosterol synthesis (principal sterol in fungal cell membrane) and inhibiting cell membrane formation
Pharmacokinetics/Pharmacodynamics
Absorption
Oral: Well absorbed; food does not affect extent of absorption
Distribution
Vd: ~0.6 L/kg; widely throughout body with good penetration into CSF, eye, peritoneal fluid, sputum, skin, and urine
Relative diffusion blood into CSF: Adequate with or without inflammation (exceeds usual MICs)
CSF:blood level ratio: Normal meninges: 50% to 90%; Inflamed meninges: ~80%
Excretion
Urine (80% as unchanged drug)
Time to Peak
Oral: 1 to 2 hours
Half-Life Elimination
Normal renal function: ~30 hours (range: 20 to 50 hours); Elderly: 46.2 hours; Neonates (gestational age 26 to 29 weeks): 73.6 to 46.6 hours (decreases with increasing postnatal age); Pediatric patients 9 months to 15 years: 19.5 to 25 hours
Protein Binding
Plasma: 11% to 12%
Use in Specific Populations
Special Populations: Renal Function Impairment
Pharmacokinetics are markedly affected; there is an inverse relationship between half-life and creatinine clearance.
Use: Labeled Indications
Treatment of candidiasis (esophageal, oropharyngeal, peritoneal, urinary tract, vaginal); systemic candida infections (eg, candidemia, disseminated candidiasis, pneumonia); and cryptococcal meningitis; and antifungal prophylaxis in allogeneic hematopoietic cell transplant recipients
Use: Off Label
Blastomycosiscyes
Data from a randomized, multicenter, open-label study comparing fluconazole 400 mg versus 800 mg suggest that the use of fluconazole at each of these doses is effective for the treatment of non-life-threatening blastomycosis Pappas 1997.
Based on the IDSA clinical practice guidelines for the management of blastomycosis, fluconazole is an effective and recommended agent for consolidation treatment of CNS disease and an effective and recommended alternative agent for treatment of pulmonary disease.
Candida intertrigob
Data from case reports and a multicenter, randomized, double-blind, double-dummy trial support the use of fluconazole for the treatment of candida intertrigo refractory to topical therapy Coldiron 1991, Nozickova 1998, Stengel 1994.
Candidiasis, empiric therapy (non-neutropenic patients in the ICU)yes
Based on the IDSA clinical practice guideline for the management of candidiasis, fluconazole is an effective and recommended alternative agent for empiric therapy of suspected invasive candidiasis in non-neutropenic patients in the ICU. It should not be used for patients with previous azole exposure or those colonized with azole-resistant Candida spp.
Candidiasis, prophylaxis in high-risk ICU patients (in units with high incidence of invasive candidiasis)yes
Based on the IDSA clinical practice guideline for the management of candidiasis, fluconazole may be considered for prophylaxis against invasive candidiasis in high-risk patients in adult ICUs with a high rate of invasive candidiasis (>5%).
Candidiasis, prophylaxis in hematologic malignancy patientsbyes
Data from an open-label, randomized trial support the use of fluconazole for the prevention of invasive fungal infection in patients with hematologic malignancy during neutropenia Glasmacher 2006.
Based on the American Society of Clinical Oncology (ASCO) and the IDSA clinical practice guidelines for antimicrobial prophylaxis for adult patients with cancer-related immunosuppression, fluconazole is recommended for prophylaxis for patients with hematologic malignancy who do not require mold-active prophylaxis.
Candidiasis, prophylaxis in solid organ transplant recipientscyes
Based on the American Society of Health-System Pharmacists (ASHP), IDSA, Surgical Infection Society (SIS), and Society for Healthcare Epidemiology of America (SHEA) guidelines for antimicrobial prophylaxis in surgery, fluconazole is recommended for surgical prophylaxis (perioperative) in select high-risk solid organ transplant patients. Clinical experience also suggests the utility of fluconazole for prophylaxis in high-risk solid organ transplant recipients Silveira 2013.
Coccidioidomycosisyes
Based on the IDSA clinical practice guideline for the treatment of coccidioidomycosis and the US Department of Health and Human Services (HHS) guidelines for prevention and treatment of opportunistic infections in HIV-infected adults and adolescents, fluconazole is an effective and recommended agent in the treatment of coccidioidomycosis as well as in the prophylaxis (initial or chronic suppressive therapy) of coccidioidomycosis in HIV-infected patients and solid organ transplant recipients undergoing transplantation in endemic areas and/or from infected donors.
Cryptococcosis, pulmonary infectionyes
Based on the IDSA clinical practice guidelines for management of cryptococcal disease, fluconazole is effective and recommended for the treatment of cryptococcal pneumonia IDSA [Perfect 2010].
Tineac
Data from multiple noncomparative trials suggest that the use of fluconazole is effective for the treatment of tinea corporis or cruris tinea pedis Kotogyan 1996, Montero-Gei 1992, Stary 1998. In addition, data from one noncomparative trial suggest that the use of fluconazole is effective for the treatment of tinea versicolor Karakas 2005.
Contraindications
Hypersensitivity to fluconazole or any component of the formulation (cross-reaction with other azole antifungal agents may occur, but has not been established; use caution); coadministration of terfenadine in adult patients receiving multiple doses of 400 mg or higher or with CYP3A4 substrates which may lead to QTc prolongation (eg, astemizole, cisapride, erythromycin, pimozide, or quinidine)
Dosage and Administration
Dosing: Adult
Blastomycosis (off-label use):
CNS disease (alternative agent): Step-down therapy: Oral: 800 mg once daily for ≥12 months and until resolution of cerebrospinal (CSF) abnormalities (Bradsher 2018; IDSA [Chapman 2008])
Pulmonary disease (alternative agent if unable to tolerate itraconazole): Oral: 400 to 800 mg once daily for 6 to 12 months (IDSA [Chapman 2008]; Pappas 1997)
Candidiasis, treatment: Note: Consider weight-based dosing for patients <50 kg or >90 kg (Rex 1994; Rex 2003). A maximum dose has not been established, but based on a small number of patients, doses up to 1,600 mg/day appear to be well tolerated (Anaissie 1995).
Candidemia (neutropenic and non-neutropenic patients):
Initial therapy (alternative to echinocandin if no previous azole exposure, noncritically ill, and not at high risk of fluconazole-resistant isolate): IV, Oral: Loading dose of 800 mg (12 mg/kg) on day 1, then 400 mg (6 mg/kg) once daily; if fluconazole-susceptible Candida glabrata isolated, transition to 800 mg (12 mg/kg) once daily (IDSA [Pappas 2016]).
Step-down therapy:
Isolates other than C. glabrata: Oral: 400 mg (6 mg/kg) once daily (IDSA [Pappas 2016])
Isolates of C. glabrata (if fluconazole-susceptible or susceptible dose-dependent): Oral: 800 mg (12 mg/kg) once daily (IDSA [Pappas 2016]; Kauffman 2018a)
Duration: Continue for ≥14 days after first negative blood culture and resolution of signs/symptoms (longer duration required in patients with metastatic complications); step-down therapy to oral fluconazole (eg, after initial therapy with an echinocandin) is recommended after 5 to 7 days in stable patients with negative repeat cultures and fluconazole-susceptible isolates (IDSA [Pappas 2016]; Kauffman 2018a).
Candidiasis, invasive (empiric therapy) and/or critically ill non-neutropenic patients in the ICU at risk of invasive candidiasis with fever and unidentified etiology (alternative to echinocandin if no previous azole exposure and not colonized with fluconazole-resistant isolate): IV, Oral: Loading dose of 800 mg (12 mg/kg) on day 1, then 400 mg (6 mg/kg) once daily; continue for ≥14 days in patients with clinical improvement. Consider discontinuing after 4 to 5 days in patients with no clinical response and no evidence of invasive candidiasis (IDSA [Pappas 2016]; Kauffman 2018a).
Cardiac device infection (eg, implantable cardiac defibrillator, pacemaker, ventricular assist device [VAD]): Step-down therapy: IV, Oral: 400 to 800 mg (6 to 12 mg/kg) once daily for 4 to 6 weeks after device removal (4 weeks for infections limited to generator pockets and ≥6 weeks for infections involving wires). Note: If VAD cannot be removed, chronic suppressive therapy with fluconazole 400 to 800 mg (6 to 12 mg/kg) once daily should be used (IDSA [Pappas 2016]).
Chronic, disseminated (hepatosplenic): Step-down therapy: Oral: 400 mg (6 mg/kg) once daily; continue until lesion resolution (usually several months) and through periods of immunosuppression (IDSA [Pappas 2016]).
CNS: Step-down therapy (fluconazole-susceptible isolates): IV, Oral: 400 to 800 mg (6 to 12 mg/kg) once daily; continue until signs/symptoms and CSF/radiologic abnormalities have resolved (IDSA [Pappas 2016]; IDSA [Tunkel 2017]).
Endocarditis, native or prosthetic valve: Step-down therapy (fluconazole-susceptible isolates): IV, Oral: 400 to 800 mg (6 to 12 mg/kg) once daily for ≥6 weeks after valve replacement surgery (longer durations recommended in patients with perivalvular abscesses or other complications). Note: In patients who cannot undergo valve replacement surgery or with prosthetic valve endocarditis, chronic suppressive therapy with fluconazole 400 to 800 mg (6 to 12 mg/kg) once daily should be used (IDSA [Pappas 2016]).
Endophthalmitis, endogenous (with or without vitritis) (fluconazole-susceptible isolates): IV, Oral: Loading dose of 800 mg (12 mg/kg) on day 1, then 400 to 800 mg (6 to 12 mg/kg) once daily for ≥4 to 6 weeks and until examination indicates resolution (longer duration may be needed for patients with vitritis); for patients with vitritis or macular involvement, intravitreal antifungal therapy is also recommended (IDSA [Pappas 2016]; Kauffman 2018b).
Esophageal: IV, Oral: Loading dose of 400 mg (6 mg/kg) on day 1, then 200 to 400 mg (3 to 6 mg/kg) once daily for 14 to 21 days; for HIV-infected patients with recurrent infections who have not attained immune reconstitution on antiretroviral therapy, chronic suppressive therapy of 100 to 200 mg 3 times weekly may be used (IDSA [Pappas 2016]; Kauffman 2018c).
Intertrigo, refractory to topical therapy (off-label use): Oral: 150 mg once weekly for 4 weeks (Brodell 2018; Nozickova 1998; Stengel 1994)
Intra-abdominal infections (alternative to echinocandin if no previous azole exposure, noncritically ill, and not at high risk of fluconazole-resistant isolate): IV, Oral: Loading dose of 800 mg (12 mg/kg) on day 1, then 400 mg (6 mg/kg) once daily; duration is for ≥2 weeks and until all signs of infection have resolved. Step-down therapy (after patient has responded to initial therapy [eg, echinocandin]) with fluconazole is recommended in stable patients with a fluconazole-susceptible isolate (IDSA [Pappas 2016]; Kauffman 2018d).
Oropharyngeal: IV, Oral: Loading dose of 200 mg on day 1, then 100 to 200 mg once daily for 7 to 14 days; recommended for patients unresponsive to topical therapy or those with moderate to severe infection, recurrent infection, or risk for esophageal candidiasis (eg, HIV-infected patients with CD4 counts <100 cells/mm3). In patients with recurrent infection, chronic suppressive therapy (100 mg 3 times weekly) may be considered, but is usually unnecessary (IDSA [Pappas 2016]; Kauffman 2018c).
Osteoarticular (osteomyelitis or septic arthritis) (fluconazole-susceptible isolates): Initial or step-down therapy: IV, Oral: 400 mg (6 mg/kg) once daily. Duration for osteomyelitis is 6 to 12 months and for septic arthritis is 6 weeks. Course may include 2 weeks of initial treatment with a lipid formulation of amphotericin B or an echinocandin. For prosthetic joints that cannot be removed, chronic suppressive therapy with fluconazole 400 mg (6 mg/kg) once daily is recommended (IDSA [Pappas 2016]).
Peritonitis, associated with peritoneal dialysis: Note: Use for empiric treatment if no prior azole exposure or for directed therapy against fluconazole-susceptible isolates (Glickman 2019):
IV, Oral: 200 mg on day 1, then 100 to 200 mg once daily for 2 to 4 weeks (Chen 2004; Glickman 2019; ISPD [Li 2016]; Wang 2000).
Thrombophlebitis, suppurative: Initial or step-down therapy: IV, Oral: 400 to 800 mg (6 to 12 mg/kg) once daily for ≥2 weeks after candidemia (if present) has cleared (IDSA [Pappas 2016]).
Urinary tract infection (UTI):
Candiduria (asymptomatic):
Patients with neutropenia: Treat as if patient has candidemia (Georgiadou 2013; IDSA [Pappas 2016]).
Patients undergoing a urologic procedure: Oral: 400 mg (6 mg/kg) once daily several days before and after the procedure (IDSA [Pappas 2016])
Cystitis (symptomatic): Oral: 200 mg (3 mg/kg) once daily for 2 weeks (IDSA [Pappas 2016])
Pyelonephritis: Oral: 200 to 400 mg (3 to 6 mg/kg) once daily for 2 weeks (IDSA [Pappas 2016])
UTI associated with fungus balls: Oral: 200 to 400 mg (3 to 6 mg/kg) once daily; concomitant amphotericin B deoxycholate irrigation via nephrostomy tubes, if present, is also recommended, along with surgical management (IDSA [Pappas 2016]).
Vaginal/Vulvovaginal:
Uncomplicated: Oral: 150 mg as a single dose (manufacturer's labeling)
Complicated or severe: Oral: 150 mg every 72 hours for 2 or 3 doses (CDC [Workowski 2015]; IDSA [Pappas 2016])
Recurrent: Oral: 150 mg every 72 hours for 10 to 14 days, followed by 150 mg once weekly for 6 months (IDSA [Pappas 2016]; Sobel 2004) or 100 mg, 150 mg, or 200 mg every 72 hours for 3 doses, then 100 mg, 150 mg, or 200 mg once weekly for 6 months (CDC [Workowski 2015]).
Candidiasis, prophylaxis:
Hematologic malignancy patients (off-label use) or hematopoietic cell transplant (HCT) recipients who do not warrant mold-active prophylaxis (off-label use): Oral: 400 mg once daily. Duration is at least until resolution of neutropenia and/or through day 75 in allogeneic HCT recipients (ASBMT [Tomblyn 2009]; ASCO/IDSA [Taplitz 2018]; Glasmacher 2006; Wingard 2019).
ICU patients (high risk) in units with a high rate (>5%) of invasive candidiasis (off-label use): Oral, IV: Loading dose of 800 mg (12 mg/kg) once on day 1, then 400 mg (6 mg/kg) once daily (IDSA [Pappas 2016]). Note: Some experts do not routinely use prophylaxis in this setting (Kauffman 2018a).
Peritoneal dialysis-associated infection (concurrently treated with antibacterials), prevention of secondary fungal infection: Oral: 200 mg every other day or 100 mg once daily (Burkart 2018; Glickman 2018; Restrepo 2010)
Solid organ transplant recipients (selected patients at high-risk for Candida infection) (off-label use): Oral, IV: 400 mg (6 mg/kg) given perioperatively and continued once daily postoperatively; indications and duration vary among transplant centers (ASHP/IDSA/SIS/SHEA [Bratzler 2013]; Fishman 2018; Silveira 2013; Winston 2002).
Coccidioidomycosis, treatment (off-label use):
Bone and/or joint infection: Initial or step-down therapy: Oral: 800 mg once daily for ≥3 years; in some cases, lifelong treatment is needed; duration depends on severity and host immunocompetence (IDSA [Galgiani 2016]).
Meningitis: Oral: 400 to 1,200 mg once daily, depending on severity; continue lifelong as there is a high relapse rate when the dose is decreased or treatment is discontinued (HHS [OI adult 2018]; IDSA [Galgiani 2016]).
Pneumonia, primary infection: Note: Only for patients with significantly debilitating illness, extensive pulmonary involvement, concurrent diabetes, frailty due to age or comorbidities, or HIV (HHS [OI adult 2018]; IDSA [Galgiani 2016]):
Oral: Usual dose: 400 mg once daily; IDSA guidelines state that some experts recommend 800 mg once daily. Duration of therapy is 3 to 6 months for immunocompetent patients; immunocompromised patients require a longer duration of therapy (sometimes lifelong) (HHS [adult OI 2018]; IDSA [Galgiani 2016]).
Pneumonia, symptomatic chronic cavitary and/or cavitary disease in immunocompromised patients: Oral: 400 mg once daily for ≥12 months. In patients with ruptured cavities, the duration may be shorter, but depends upon the postoperative course (IDSA [Galgiani 2016]; Jaroszewski 2018).
Soft tissue infection (not associated with bone infection): Oral: 400 mg once daily; some experts give up to 800 mg once daily; duration is for ≥6 to 12 months (IDSA [Galgiani 2016]).
Coccidioidomycosis, prophylaxis (off-label use):
HIV-infected patients: Note: Primary prophylaxis is not recommended; yearly or twice-yearly serologic testing should be performed in patients living in endemic areas.
Patients with a CD4 count <250 cells/mm3 who have a new positive serology: Oral: 400 mg once daily until antiretroviral therapy has fully suppressed HIV replication and the CD4 count is ≥250 cells/mm3 (HHS [OI adult 2018]).
Solid organ transplant recipients:
Seronegative patients in endemic areas (regardless of clinical history of coccidioidomycosis): Oral: 200 mg once daily for 6 to 12 months following transplantation (Ampel 2018; IDSA [Galgiani 2016])
Seropositive patients in endemic areas: Oral: 400 mg once daily for 6 to 12 months following transplantation (IDSA [Galgiani 2016])
Cryptococcal meningitis: Note: Treatment involves induction, consolidation, and maintenance phases of therapy.
HIV-infected patients:
Induction: Oral:
Resource-rich settings, alternative regimens:
If flucytosine is unavailable or not tolerated: 800 mg once daily in combination with amphotericin B (lipid formulation preferred) for ≥2 weeks (HHS [OI adult 2018]); or
If amphotericin B is unavailable or not tolerated: 800 to 1,200 mg once daily in combination with flucytosine for ≥2 weeks (IDSA [Perfect 2010]; Molloy 2018; Nussbaum 2010); or
If flucytosine and amphotericin B are unavailable or not tolerated: 1,200 mg once daily as monotherapy for ≥2 weeks (HHS [OI adult 2018]).
Resource-limited settings:
Amphotericin B deoxycholate in combination with flucytosine for 1 week followed by fluconazole 1,200 mg once daily for 1 week (preferred regimen) (WHO 2018); or
If IV therapy is difficult to administer: 1,200 mg once daily as a 2-week induction regimen in combination with flucytosine for 2 weeks (WHO 2018); or
If flucytosine is unavailable: 1,200 mg once daily in combination with amphotericin B deoxycholate for 2 weeks (WHO 2018)
Note: Induction therapy should be continued beyond the durations listed above if clinical improvement is not observed and/or if CSF cultures remain positive (Cox 2018a).
Consolidation: Oral: 400 mg once daily for ≥8 weeks following induction with the preferred regimen of amphotericin B and flucytosine (HHS [OI adult 2018]; IDSA [Perfect 2010]); patients receiving any other induction regimen should receive 800 mg once daily for ≥8 weeks (Cox 2018a; IDSA [Perfect 2010]; WHO 2018).
Maintenance (suppression): Oral: 200 mg once daily for ≥12 months; may discontinue if completed induction, consolidation, and ≥12 months of maintenance therapy, patient remains asymptomatic, and CD4 count has been ≥100 cells/mm3 for ≥3 months and HIV RNA is suppressed in response to effective antiretroviral therapy (HHS [OI adult 2018]).
HIV-uninfected patients:
Induction (alternative regimens): Oral:
If flucytosine is unavailable or not tolerated: 800 mg once daily in combination with amphotericin B for 2 weeks (Cox 2018b); or
If amphotericin B is unavailable or not tolerated: 800 to 1,200 mg once daily in combination with flucytosine for 2 to 10 weeks, depending on severity and response to therapy (Cox 2018b); or
If amphotericin B and flucytosine are unavailable or not tolerated: 800 to 1,200 mg once daily as monotherapy for ≥10 weeks (Cox 2018b)
Consolidation: Oral: 400 to 800 mg once daily for 8 weeks (800 mg once daily preferred for patients who receive a 2-week induction course) (Baddley 2013; Cox 2018b; IDSA [Perfect 2010])
Maintenance (suppression): Oral: 200 to 400 mg once daily for 6 to 12 months (Baddley 2013; IDSA [Perfect 2010]) (a longer duration may be warranted for patients on high-dose steroids or biologic agent [eg, alemtuzumab], or with radiographic evidence of cryptococcoma [Cox 2018b])
Cryptococcosis, pulmonary infection (off-label use):
Mild to moderate symptoms (if severe pneumonia, treat like CNS infection): Immunocompetent or immunocompromised patients without diffuse pulmonary infiltrates or disseminated infection: Oral: 400 mg (6 mg/kg) once daily for 6 to 12 months (Cox 2018c; IDSA [Perfect 2010]); for HIV-infected patients, some experts recommend a duration of 12 months (HHS [OI adult 2018]). Chronic suppressive therapy may be warranted for patients with ongoing immunosuppression (Cox 2018c; HHS [OI adult 2018]).
Tinea:
Tinea corporis or cruris: Oral: 150 to 200 mg once weekly for 2 to 4 weeks (Goldstein 2018; Kotogyan 1996; Montero-Gei 1992; Stary 1998)
Tinea pedis: Oral: 150 mg once weekly for 2 to 6 weeks (Gupta 2008; Kotogyan 1996; Montero-Gei 1992)
Tinea versicolor: Oral: 300 mg once weekly for 2 weeks (Karakas 2005)
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
General dosing, susceptible infection: Infants, Children, and Adolescents: IV, Oral: Initial: 6 to 12 mg/kg/dose, followed by 3 to 12 mg/kg/dose once daily; duration and dosage depends on severity of infection; the manufacturer suggests limiting dose to 600 mg/dose.
Candida infections, prophylaxis:
Oncology patients at high risk of invasive candidiasis (eg, AML, recurrent ALL, myelodysplastic syndrome [MDS], HSCT recipients): Limited data available: Infants, Children, and Adolescents: IV, Oral: 6 to 12 mg/kg/dose once daily; maximum dose: 400 mg/dose; duration dependent upon type of transplant and/or chemotherapy, consult institution-specific protocols (ESCMID [Hope 2012]; Science 2014).
Surgical prophylaxis, high-risk patients undergoing liver, pancreas, kidney, or pancreas-kidney transplantation: Infants, Children, and Adolescents: IV: 6 mg/kg as a single dose 60 minutes before procedure; maximum dose: 400 mg/dose; time of initiation and duration varies with transplant type, consult institution-specific protocols (ASHP/IDSA [Bratzler 2013]).
Candidiasis, systemic (including Candidemia and invasive candidiasis), treatment: Infants, Children, and Adolescents: IV, Oral: 12 mg/kg/dose once daily; maximum dose: 800 mg/dose; continue treatment for 14 days after documented clearance and resolution of symptoms (ESCMID [Hope 2012]; IDSA [Pappas 2016]; Red Book [AAP 2018]).
Candidiasis, chronic, disseminated (hepatosplenic), step-down therapy: Infants, Children, and Adolescents: Oral: 6 mg/kg/dose once daily following several weeks of initial therapy with an amphotericin B lipid formulation or an echinocandin; treatment should continue until lesion resolution (usually several months); maximum dose: 400 mg/dose (IDSA [Pappas 2016]).
Candidiasis, CNS candidiasis, step-down therapy: Infants, Children, and Adolescents: Oral, IV: 12 mg/kg/dose once daily following initial therapy with liposomal amphotericin B (with or without flucytosine); maximum dose: 800 mg/dose; treatment should continue until all signs, symptoms, and CSF and radiological abnormalities have resolved (IDSA [Pappas 2016]; IDSA [Tunkel 2017]; Red Book [AAP 2018]).
Candidiasis, endophthalmitis, treatment: Oral, IV: Infants, Children, and Adolescents: 12 mg/kg/dose on day 1 followed by 6 to 12 mg/kg/dose once daily for at least 4 to 6 weeks until examination indicates resolution; maximum dose 800 mg/dose. Note: Use in combination with intravitreal injection of voriconazole or amphotericin B deoxycholate when vitritis or macular involvement is present (IDSA [Pappas 2016]).
Candidiasis, esophageal, treatment:
Non-HIV-exposed/-positive: Infants, Children, and Adolescents: IV, Oral: 6 mg/kg/dose once daily for 14 to 21 days. Note: Usual adult dose is 200 to 400 mg/day (IDSA [Pappas 2016]; Red Book [AAP 2018]).
HIV-exposed/-positive:
Infants and Children: IV, Oral: 6 to 12 mg/kg/dose once daily for 14 days following symptom resolution (minimum duration: 21 days); maximum dose: 600 mg/dose (HHS [OI pediatric 2018]).
Adolescents: IV, Oral: 100 to 400 mg once daily for 14 to 21 days; may follow with chronic suppressive therapy of 100 to 200 mg once daily for patients with frequent or severe recurrences (HHS [OI adult 2018]).
Candidiasis, oropharyngeal:
Non-HIV-exposed/-positive: Infants, Children, and Adolescents: IV, Oral: 6 mg/kg/dose on day 1 followed by 3 to 6 mg/kg/dose once daily for 7 to 14 days (IDSA [Pappas 2016]; Red Book [AAP 2018]). Note: Usual adult dose is 100 to 200 mg/day.
HIV-exposed/-positive:
Treatment:
Infants and Children: IV, Oral: 6 to 12 mg/kg/dose once daily for 7 to 14 days; maximum dose: 400 mg/dose (HHS [OI pediatric 2018]).
Adolescents: Oral: 100 mg once daily for 7 to 14 days; may follow with chronic suppressive therapy of 100 mg once daily or 3 times weekly for patients with frequent or severe recurrences (HHS [OI adult 2018]).
Secondary prophylaxis, recurrent severe: Infants and Children: Oral: 3 to 6 mg/kg/dose once daily; maximum dose: 200 mg/dose (HHS [OI pediatric 2018]).
Candidiasis, peritoneal dialysis-related infections (ISPD [Warady 2012]):
Peritonitis:
Treatment: Intraperitoneal, IV, Oral: 6 to 12 mg/kg/dose every 24 to 48 hours; maximum dose: 400 mg/dose.
Prophylaxis for high-risk situations (eg, during antibiotic therapy or PEG placement): IV, Oral: 3 to 6 mg/kg/dose every 24 to 48 hours; maximum dose: 200 mg/dose.
Exit-site or tunnel infection, treatment: Oral: 6 mg/kg/dose every 24 to 48 hours; maximum dose: 400 mg/dose.
Candidiasis, vulvovaginal infection:
Uncomplicated infections, treatment (independent of HIV status): Adolescents: Oral: 150 mg as a single dose (CDC [Workowski 2015]; HHS [OI adult 2018]).
Severe infections, treatment:
Non-HIV-exposed/-positive: Adolescents: Oral: 150 mg every 72 hours for 2 to 3 doses (CDC [Workowski 2015]; IDSA [Pappas 2016]).
HIV-exposed/-positive: Adolescents: Oral: 100 to 200 mg once daily for ≥7 days; may follow with chronic suppressive therapy of 150 mg once weekly (HHS [OI adult 2018]).
Recurrent infection, treatment:
Non HIV-exposed/-positive: Adolescents: Oral: Initial: 100 to 200 mg every 72 hours for 3 doses; followed by maintenance of 100 to 200 mg once weekly for 6 months (CDC [Workowski 2015]; IDSA [Pappas 2016]).
HIV-exposed/-positive: Adolescents: Oral: 100 to 200 mg once daily for ≥ 7 days; may follow with chronic suppressive therapy of 150 mg once weekly (HHS [OI adult 2018]).
Coccidioidomycosis (HIV-exposed/-positive) (HHS [OI adult 2018]; HHS [OI pediatric 2018]):
Mild to moderate non-meningeal infection (eg, focal pneumonia):
Infants and Children: IV, Oral: 6 to 12 mg/kg/dose once daily; maximum dose: 400 mg/dose.
Adolescents: Oral: 400 mg once daily for ≥6 months.
Severe illness (diffuse pulmonary or disseminated non-meningitic disease) initial therapy if unable to use amphotericin or as step-down therapy: Infants and Children: IV, Oral: 12 mg/kg/dose once daily; maximum dose: 800 mg/dose for a total of 1 year of treatment followed by secondary prophylaxis.
Meningeal infection:
Infants and Children: IV, Oral: 12 mg/kg/dose once daily; maximum dose: 800 mg/dose, followed by lifelong secondary prophylaxis.
Adolescents: IV, Oral: 400 to 800 mg once daily, followed by lifelong suppressive therapy.
Secondary prophylaxis/chromic suppressive therapy: Infants, Children, and Adolescents: Oral: 6 mg/kg/dose once daily; maximum dose: 400 mg/dose.
Cryptococcal infection:
Mild to moderate localized infection including pneumonia (not CNS), treatment:
Non HIV-exposed/-positive: Infants, Children, and Adolescents: Oral: 6 to 12 mg/kg/dose once daily for 6 to 12 months. Usual adult dose is 400 mg/dose (IDSA [Perfect 2010]).
HIV-exposed/-positive:
Infants and Children: IV, Oral: 12 mg/kg on day 1, then 6 to 12 mg/kg/dose once daily; maximum dose: 600 mg/dose; duration depends on severity and clinical response (HHS [OI pediatric 2018].
Adolescents: Oral: 400 mg daily for 12 months (HHS [OI adult 2018]).
CNS, severe pulmonary or disseminate infection, treatment:
Induction therapy: HIV-exposed/-positive (not first-line therapy):
Infants and Children: IV: 12 mg/kg on day 1, then 10 to 12 mg/kg/dose once daily in combination with amphotericin B or flucytosine for ≥14 days; maximum dose: 800 mg/dose (HHS [OI pediatric 2018]).
Adolescents: IV, Oral: 400 to 800 mg once daily in combination with flucytosine for ≥14 days or 800 mg once daily in combination with amphotericin for ≥14 days or 1,200 mg once daily as monotherapy for at least 2 weeks (HHS [OI adult 2018]).
Consolidation:
Non-HIV-exposed/-positive: Infants, Children, and Adolescents: IV, Oral: 10 to 12 mg/kg/day once daily or in divided doses twice daily for 8 weeks; maximum dose: 800 mg/dose (IDSA [Perfect 2010]; Red Book [AAP 2018]).
HIV-exposed/-positive:
Infants and Children: IV, Oral: 12 mg/kg on day 1, then 10 to 12 mg/kg/day once daily for ≥8 weeks; maximum daily dose: 800 mg/dose (HHS [OI pediatric 2018]).
Adolescents: IV, Oral: 400 mg once daily for ≥8 weeks (HHS [OI adult 2018]).
Secondary prophylaxis/chronic suppressive maintenance therapy:
Non-HIV-exposed/-positive: Infants, Children, and Adolescents: Oral: 6 mg/kg/dose once daily for 6 to 12 months; maximum dose: 200 mg/dose (IDSA [Perfect 2010]).
HIV-exposed/-positive: Infants, Children, and Adolescents: Oral: 6 mg/kg/dose once daily for ≥12 months; maximum dose: 200 mg/dose (HHS [OI adult 2018]; HHS [OI pediatric 2018]).
Histoplasmosis: HIV-exposed/-positive patients, alternative therapy (HHS [OI adult 2018]; HHS [OI pediatric 2018]):
Pulmonary, acute primary disease: Infants and Children: Oral: 3 to 6 mg/kg/dose once daily; maximum dose: 200 mg/dose.
Disseminated disease, mild to moderate:
Infants and Children: IV, Oral: 5 to 6 mg/kg/dose twice daily for 12 months; maximum dose: 300 mg/dose.
Adolescents: Oral: 800 mg once daily.
Secondary prophylaxis/chronic suppressive therapy:
Infants and Children: Oral: 3 to 6 mg/kg/dose once daily for ≥12 months; maximum dose: 200 mg/dose.
Adolescents: Oral: 400 mg once daily for ≥12 months.
Administration
IV: Do not use if cloudy or precipitated. Infuse over ~1 to 2 hours; do not exceed 200 mg/hour.
Oral: May be administered without regard to meals.
Storage
Tablet: Store at <30°C (86°F).
Powder for oral suspension: Store dry powder at <30°C (86°F). Following reconstitution, store at 5°C to 30°C (41°F to 86°F). Discard unused portion after 2 weeks. Do not freeze.
Injection: Store injection in glass at 5°C to 30°C (41°F to 86°F). Store injection in plastic flexible containers with overwrap at 20°C to 25°C (68°F to 77°F). Do not freeze. Do not unwrap unit until ready for use.
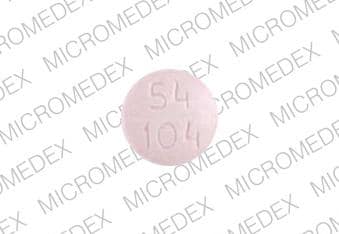
Fluconazole Images
Drug Interactions
Abemaciclib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Abemaciclib. Monitor therapy
Acalabrutinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Acalabrutinib. Management: Reduce acalabrutinib dose to 100 mg once daily with concurrent use of a moderate CYP3A4 inhibitor. Monitor patient closely for both acalabrutinib response and evidence of adverse effects with any concurrent use. Consider therapy modification
Alfentanil: Fluconazole may increase the serum concentration of Alfentanil. Management: Monitor for increased anesthetic and respiratory depressant effects if alfentanil is combined with fluconazole. Consider using lower initial doses of alfentanil or an alternative anesthetic. Consider therapy modification
Amiodarone: QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may enhance the QTc-prolonging effect of Amiodarone. QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of Amiodarone. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Amitriptyline: May enhance the QTc-prolonging effect of Fluconazole. Fluconazole may increase the serum concentration of Amitriptyline. Monitor therapy
AmLODIPine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of AmLODIPine. Monitor therapy
Amphotericin B: Antifungal Agents (Azole Derivatives, Systemic) may diminish the therapeutic effect of Amphotericin B. Monitor therapy
Apixaban: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Apixaban. Monitor therapy
Aprepitant: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Aprepitant. Avoid combination
ARIPiprazole: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of ARIPiprazole. Management: Monitor for increased aripiprazole pharmacologic effects. Aripiprazole dose adjustments may or may not be required based on concomitant therapy and/or indication. Consult full interaction monograph for specific recommendations. Monitor therapy
Astemizole: Fluconazole may enhance the QTc-prolonging effect of Astemizole. Fluconazole may increase the serum concentration of Astemizole. Avoid combination
Asunaprevir: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Asunaprevir. Avoid combination
AtorvaSTATin: Fluconazole may increase the serum concentration of AtorvaSTATin. Monitor therapy
Avanafil: Fluconazole may increase the serum concentration of Avanafil. Management: Limit avanafil to a maximum dose of 50 mg per 24-hour period in any patient who is also receiving a moderate inhibitor of CYP3A4 such as fluconazole. Consider therapy modification
Avapritinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Avapritinib. Management: Avoid use of moderate CYP3A4 inhibitors with avapritinib. If this combination cannot be avoided, reduce the avapritinib dose from 300 mg once daily to 100 mg once daily. Consider therapy modification
Avatrombopag: Fluconazole may increase the serum concentration of Avatrombopag. Management: Management of this interaction varies based on avatrombopag indication. Dose adjustments are required for patients using avatrombopag for chronic immune thrombocytopenia. See monograph for details. Consider therapy modification
Axitinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Axitinib. Monitor therapy
Benzhydrocodone: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Benzhydrocodone. Specifically, the concentration of hydrocodone may be increased. Monitor therapy
Blonanserin: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Blonanserin. Monitor therapy
Bosentan: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Bosentan. Management: Concomitant use of both a CYP2C9 inhibitor and a CYP3A inhibitor or a single agent that inhibits both enzymes with bosentan is likely to cause a large increase in serum concentrations of bosentan and is not recommended. See monograph for details. Monitor therapy
Bosentan: CYP2C9 Inhibitors (Moderate) may increase the serum concentration of Bosentan. Management: Concomitant use of both a CYP2C9 inhibitor and a CYP3A inhibitor or a single agent that inhibits both enzymes with bosentan is likely to cause a large increase in serum concentrations of bosentan and is not recommended. See monograph for details. Monitor therapy
Bosutinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Bosutinib. Avoid combination
Brexpiprazole: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Brexpiprazole. Management: The brexpiprazole dose should be reduced to 25% of usual if used together with both a moderate CYP3A4 inhibitor and a strong or moderate CYP2D6 inhibitor, or if a moderate CYP3A4 inhibitor is used in a CYP2D6 poor metabolizer. Monitor therapy
Brigatinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Brigatinib. Management: Avoid concurrent use of brigatinib with moderate CYP3A4 inhibitors when possible. If such a combination cannot be avoided, reduce the dose of brigatinib by approximately 40% (ie, from 180 mg to 120 mg, from 120 mg to 90 mg, or from 90 mg to 60 mg). Consider therapy modification
Bromocriptine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Bromocriptine. Management: The bromocriptine dose should not exceed 1.6 mg daily with use of a moderate CYP3A4 inhibitor. The Cycloset brand specifically recommends this dose limitation, but other bromocriptine products do not make such specific recommendations. Consider therapy modification
Budesonide (Systemic): CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Budesonide (Systemic). Avoid combination
Budesonide (Topical): CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Budesonide (Topical). Management: Per US prescribing information, avoid this combination. Canadian product labeling does not recommend strict avoidance. If combined, monitor for excessive glucocorticoid effects as budesonide exposure may be increased. Consider therapy modification
Busulfan: Antifungal Agents (Azole Derivatives, Systemic) may increase the serum concentration of Busulfan. Isavuconazonium considerations are addressed in separate monographs. Monitor therapy
Calcium Channel Blockers: Fluconazole may increase the serum concentration of Calcium Channel Blockers. Exceptions: Clevidipine. Monitor therapy
Cannabidiol: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Cannabidiol. Monitor therapy
Cannabidiol: CYP2C19 Inhibitors (Strong) may increase the serum concentration of Cannabidiol. Monitor therapy
Cannabis: CYP2C9 Inhibitors (Moderate) may increase the serum concentration of Cannabis. More specifically, tetrahydrocannabinol serum concentrations may be increased. Monitor therapy
Cannabis: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Cannabis. More specifically, tetrahydrocannabinol and cannabidiol serum concentrations may be increased. Monitor therapy
CarBAMazepine: Fluconazole may increase the serum concentration of CarBAMazepine. Monitor therapy
Carvedilol: CYP2C9 Inhibitors (Moderate) may increase the serum concentration of Carvedilol. Specifically, concentrations of the S-carvedilol enantiomer may be increased. Monitor therapy
Ceritinib: QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may enhance the QTc-prolonging effect of Ceritinib. Ceritinib may enhance the QTc-prolonging effect of QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk). QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of Ceritinib. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Cilostazol: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Cilostazol. Management: Consider reducing the cilostazol dose to 50 mg twice daily in adult patients who are also receiving moderate inhibitors of CYP3A4. Consider therapy modification
Cilostazol: CYP2C19 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of Cilostazol. CYP2C19 Inhibitors (Strong) may increase the serum concentration of Cilostazol. Management: Reduce the cilostazol dose to 50 mg twice daily in patients who are also receiving strong inhibitors of CYP2C19. Monitor clinical response to cilostazol closely. Consider therapy modification
Citalopram: Fluconazole may enhance the QTc-prolonging effect of Citalopram. Fluconazole may increase the serum concentration of Citalopram. Management: Limit citalopram dose to a maximum of 20 mg/day if used with fluconazole, which is a strong CYP2C19 inhibitor. Consider therapy modification
Clopidogrel: CYP2C19 Inhibitors (Strong) may decrease serum concentrations of the active metabolite(s) of Clopidogrel. Management: Due to a risk for impaired clopidogrel effectiveness with such a combination, carefully consider the need for a strong CYP2C19 inhibitor in patients receiving clopidogrel. Monitor patients closely for evidence of a diminished response to clopidogrel. Consider therapy modification
Cobimetinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Cobimetinib. Management: Avoid the concomitant use of cobimetinib and moderate CYP3A4 inhibitors. If concurrent short term (14 days or less) use cannot be avoided, reduce the cobimetinib dose to 20 mg daily. Avoid combination
Codeine: CYP3A4 Inhibitors (Moderate) may increase serum concentrations of the active metabolite(s) of Codeine. Monitor therapy
Colchicine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Colchicine. Management: Reduce colchicine dose as directed when using with a moderate CYP3A4 inhibitor, and increase monitoring for colchicine-related toxicity. See full monograph for details. Use extra caution in patients with impaired renal and/or hepatic function. Consider therapy modification
Crizotinib: QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may enhance the QTc-prolonging effect of Crizotinib. QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of Crizotinib. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
CycloSPORINE (Systemic): Fluconazole may increase the serum concentration of CycloSPORINE (Systemic). Monitor therapy
CYP2C19 Substrates (High risk with Inhibitors): CYP2C19 Inhibitors (Strong) may decrease the metabolism of CYP2C19 Substrates (High risk with Inhibitors). Consider therapy modification
CYP2C9 Substrates (High risk with Inhibitors): CYP2C9 Inhibitors (Moderate) may decrease the metabolism of CYP2C9 Substrates (High risk with Inhibitors). Monitor therapy
CYP3A4 Substrates (High risk with Inhibitors): CYP3A4 Inhibitors (Moderate) may decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Exceptions: Alitretinoin (Systemic); Praziquantel; Trabectedin; Vinorelbine. Monitor therapy
Dabigatran Etexilate: Fluconazole may enhance the anticoagulant effect of Dabigatran Etexilate. Monitor therapy
Dapoxetine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Dapoxetine. Management: The dose of dapoxetine should be limited to 30 mg per day when used together with a moderate inhibitor of CYP3A4. Consider therapy modification
Deflazacort: CYP3A4 Inhibitors (Moderate) may increase serum concentrations of the active metabolite(s) of Deflazacort. Management: Administer one third of the recommended deflazacort dose when used together with a strong or moderate CYP3A4 inhibitor. Consider therapy modification
Dichlorphenamide: Antifungal Agents (Azole Derivatives, Systemic) may enhance the hypokalemic effect of Dichlorphenamide. Monitor therapy
Diclofenac (Systemic): CYP2C9 Inhibitors (Moderate) may increase the serum concentration of Diclofenac (Systemic). Management: Consider using a reduced dose of diclofenac when used together with moderate CYP2C9 inhibitors. Arthrotec (diclofenac and misoprostol) prescribing information recommends a maximum dose of 50 mg twice daily. Consider therapy modification
Didanosine: May decrease the absorption of Antifungal Agents (Azole Derivatives, Systemic). Enteric coated didanosine capsules are not expected to affect these antifungals. Consider therapy modification
Domperidone: May enhance the QTc-prolonging effect of QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk). QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of Domperidone. Avoid combination
DOXOrubicin (Conventional): CYP3A4 Inhibitors (Moderate) may increase the serum concentration of DOXOrubicin (Conventional). Management: Seek alternatives to moderate CYP3A4 inhibitors in patients treated with doxorubicin whenever possible. One U.S. manufacturer (Pfizer Inc.) recommends that these combinations be avoided. Consider therapy modification
Dronabinol: CYP2C9 Inhibitors (Moderate) may increase the serum concentration of Dronabinol. Monitor therapy
Dronabinol: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Dronabinol. Monitor therapy
Dronedarone: QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may enhance the QTc-prolonging effect of Dronedarone. QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of Dronedarone. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Eletriptan: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Eletriptan. Management: The use of eletriptan within 72 hours of a moderate CYP3A4 inhibitor should be avoided. Consider therapy modification
Elexacaftor, Tezacaftor, and Ivacaftor: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Elexacaftor, Tezacaftor, and Ivacaftor. Management: When combined with moderate CYP3A4 inhibitors, two elexacaftor/tezacaftor/ivacaftor (100 mg/50 mg/75 mg) tablets should be given in the morning, every other day. Ivacaftor (150 mg) should be given in the morning, every other day on alternate days. Consider therapy modification
Eliglustat: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Eliglustat. Management: Use should be avoided under some circumstances. See full drug interaction monograph for details. Consider therapy modification
Encorafenib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Encorafenib. Management: Avoid concomitant use of encorafenib and moderate CYP3A4 inhibitors whenever possible. If concomitant administration is unavoidable, decrease the encorafenib dose prior to initiation of the CYP3A4 inhibitor. See full monograph for details. Consider therapy modification
Encorafenib: May enhance the QTc-prolonging effect of QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk). QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of Encorafenib. Management: Avoid using moderate CYP3A4 inhibitors together with encorafenib if possible. If the combination must be used, reduce the encorafenib dose prior to initiation of the moderate CYP3A4 inhibitor and monitor QT interval. See full monograph for details. Consider therapy modification
Entrectinib: May enhance the QTc-prolonging effect of QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk). QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of Entrectinib. Avoid combination
Eplerenone: Fluconazole may increase the serum concentration of Eplerenone. Management: Reduce the starting dose of eplerenone to 25 mg/day; monitor patients closely for increased eplerenone effects. Consider therapy modification
Erdafitinib: Fluconazole may increase the serum concentration of Erdafitinib. Management: Avoid concomitant use of erdafitinib and fluconazole when possible. If combined, monitor closely for erdafitinib adverse reactions and consider dose modifications accordingly. Consider therapy modification
Erythromycin (Systemic): Fluconazole may enhance the QTc-prolonging effect of Erythromycin (Systemic). Fluconazole may increase the serum concentration of Erythromycin (Systemic). Avoid combination
Estrogen Derivatives: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Estrogen Derivatives. Monitor therapy
Etravirine: Antifungal Agents (Azole Derivatives, Systemic) may increase the serum concentration of Etravirine. Applicable Isavuconazonium considerations are addressed in separate monographs. Etravirine may decrease the serum concentration of Antifungal Agents (Azole Derivatives, Systemic). This would be anticipated with itraconazole or ketoconazole. Etravirine may increase the serum concentration of Antifungal Agents (Azole Derivatives, Systemic). This would be anticipated with voriconazole. Management: Monitor for increased effects/toxicity of etravirine. Antifungal dose adjustment may be needed for ketoconazole, itraconazole, or posaconazole but specific dosing guidelines are lacking. Consider therapy modification
Everolimus: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Everolimus. Management: Everolimus dose reductions are required for most indications. See full monograph or prescribing information for specific dose adjustment and monitoring recommendations. Consider therapy modification
Fedratinib: Fluconazole may increase the serum concentration of Fedratinib. Avoid combination
FentaNYL: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of FentaNYL. Management: Monitor patients closely for several days following initiation of this combination, and adjust fentanyl dose as necessary. Consider therapy modification
Fexinidazole [INT]: May enhance the QTc-prolonging effect of QT-prolonging Agents (Moderate Risk). Avoid combination
Flibanserin: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Flibanserin. Avoid combination
Fluvastatin: Fluconazole may increase the serum concentration of Fluvastatin. Management: Limit fluvastatin maximum adult dose to 20 mg twice daily, and monitor for toxic effects of fluvastatin (e.g., myalgia, rhabdomyolysis, liver function test abnormalities), during concomitant treatment. Consider therapy modification
Fosaprepitant: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Fosaprepitant. Avoid combination
Fosphenytoin: Fluconazole may increase the serum concentration of Fosphenytoin. Consider therapy modification
GuanFACINE: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of GuanFACINE. Management: Reduce the guanfacine dose by 50% when initiating this combination. Consider therapy modification
Haloperidol: QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may enhance the QTc-prolonging effect of Haloperidol. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
HYDROcodone: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of HYDROcodone. Monitor therapy
Ibrutinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Ibrutinib. Management: When treating B-cell malignancies, decrease ibrutinib to 280 mg daily when combined with moderate CYP3A4 inhibitors. When treating graft versus host disease, monitor patients closely and reduce the ibrutinib dose as needed based on adverse reactions. Consider therapy modification
Ifosfamide: CYP3A4 Inhibitors (Moderate) may decrease serum concentrations of the active metabolite(s) of Ifosfamide. Monitor therapy
Imatinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Imatinib. Monitor therapy
Ivabradine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Ivabradine. Avoid combination
Ivacaftor: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Ivacaftor. Management: Ivacaftor dose reductions may be required; consult full monograph content for age- and weight-specific dosage recommendations. Consider therapy modification
Ivosidenib: May enhance the QTc-prolonging effect of QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk). QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of Ivosidenib. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Lefamulin: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Lefamulin. Management: Monitor for lefamulin adverse effects during coadministration of lefamulin tablets with moderate CYP3A4 inhibitors. Monitor therapy
Lemborexant: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Lemborexant. Avoid combination
Lesinurad: CYP2C9 Inhibitors (Moderate) may increase the serum concentration of Lesinurad. Monitor therapy
Levamlodipine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Levamlodipine. Monitor therapy
Levomethadone: Fluconazole may increase the serum concentration of Levomethadone. Monitor therapy
Lomitapide: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Lomitapide. Avoid combination
Lornoxicam: CYP2C9 Inhibitors (Moderate) may increase the serum concentration of Lornoxicam. Monitor therapy
Losartan: Fluconazole may decrease the serum concentration of Losartan. Specifically, fluconazole may decrease the serum concentration of E3174, the more potent active metabolite of losartan. Monitor therapy
Lovastatin: Fluconazole may increase the serum concentration of Lovastatin. Monitor therapy
Lumateperone: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Lumateperone. Avoid combination
Lurasidone: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Lurasidone. Management: Lurasidone US labeling recommends reducing lurasidone dose by half with a moderate CYP3A4 inhibitor. Some non-US labeling recommends initiating lurasidone at 20 mg/day and limiting dose to 40 mg/day; avoid concurrent use of grapefruit products. Consider therapy modification
Manidipine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Manidipine. Monitor therapy
Meloxicam: CYP2C9 Inhibitors (Moderate) may increase the serum concentration of Meloxicam. Monitor therapy
Meperidine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Meperidine. Monitor therapy
Methadone: May enhance the QTc-prolonging effect of QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk). QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of Methadone. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Mirodenafil: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Mirodenafil. Monitor therapy
Mizolastine: Antifungal Agents (Azole Derivatives, Systemic) may increase the serum concentration of Mizolastine. Avoid combination
Naldemedine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Naldemedine. Monitor therapy
Nalfurafine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Nalfurafine. Monitor therapy
Nalmefene: Fluconazole may increase the serum concentration of Nalmefene. Monitor therapy
Naloxegol: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Naloxegol. Avoid combination
Nateglinide: CYP2C9 Inhibitors (Moderate) may increase the serum concentration of Nateglinide. Monitor therapy
Neratinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Neratinib. Avoid combination
Nevirapine: Fluconazole may increase the serum concentration of Nevirapine. Monitor therapy
NiMODipine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of NiMODipine. Monitor therapy
Olaparib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Olaparib. Management: Avoid use of moderate CYP3A4 inhibitors in patients being treated with olaparib, if possible. If such concurrent use cannot be avoided, the dose of olaparib should be reduced to 150 mg twice daily. Consider therapy modification
Ondansetron: May enhance the QTc-prolonging effect of QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Ospemifene: Fluconazole may increase the serum concentration of Ospemifene. Avoid combination
OxyCODONE: CYP3A4 Inhibitors (Moderate) may enhance the adverse/toxic effect of OxyCODONE. CYP3A4 Inhibitors (Moderate) may increase the serum concentration of OxyCODONE. Serum concentrations of the active metabolite Oxymorphone may also be increased. Monitor therapy
Parecoxib: Fluconazole may increase the serum concentration of Parecoxib. Management: Use the lowest possible dose of parecoxib in patients who are taking fluconazole. Consider therapy modification
Pentamidine (Systemic): May enhance the QTc-prolonging effect of QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Pexidartinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Pexidartinib. Monitor therapy
Phenytoin: Fluconazole may increase the serum concentration of Phenytoin. Consider therapy modification
Pimecrolimus: CYP3A4 Inhibitors (Moderate) may decrease the metabolism of Pimecrolimus. Monitor therapy
Pimozide: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Pimozide. Avoid combination
Pimozide: May enhance the QTc-prolonging effect of QT-prolonging Agents (Moderate Risk). Avoid combination
PredniSONE: Fluconazole may increase the serum concentration of PredniSONE. Monitor therapy
Proton Pump Inhibitors: Fluconazole may increase the serum concentration of Proton Pump Inhibitors. Monitor therapy
QT-prolonging Antidepressants (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk). Exceptions: Citalopram. Monitor therapy
QT-prolonging Antipsychotics (Moderate Risk): QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Pimozide; QUEtiapine. Monitor therapy
QT-prolonging Class IA Antiarrhythmics (Highest Risk): Fluconazole may enhance the QTc-prolonging effect of QT-prolonging Class IA Antiarrhythmics (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: QuiNIDine. Consider therapy modification
QT-prolonging Class IC Antiarrhythmics (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Class III Antiarrhythmics (Highest Risk): May enhance the QTc-prolonging effect of QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk). QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of QT-prolonging Class III Antiarrhythmics (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Dronedarone. Consider therapy modification
QT-prolonging Kinase Inhibitors (Highest Risk): May enhance the QTc-prolonging effect of QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk). QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of QT-prolonging Kinase Inhibitors (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Ivosidenib. Consider therapy modification
QT-prolonging Kinase Inhibitors (Moderate Risk): QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may enhance the QTc-prolonging effect of QT-prolonging Kinase Inhibitors (Moderate Risk). QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of QT-prolonging Kinase Inhibitors (Moderate Risk). Exceptions: Encorafenib; Entrectinib. Monitor therapy
QT-prolonging Miscellaneous Agents (Highest Risk): May enhance the QTc-prolonging effect of Fluconazole. Fluconazole may enhance the QTc-prolonging effect of QT-prolonging Miscellaneous Agents (Highest Risk). Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Astemizole; Terfenadine. Consider therapy modification
QT-prolonging Miscellaneous Agents (Moderate Risk): QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may enhance the QTc-prolonging effect of QT-prolonging Miscellaneous Agents (Moderate Risk). QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of QT-prolonging Miscellaneous Agents (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Domperidone. Monitor therapy
QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk): Fluconazole may enhance the QTc-prolonging effect of QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Crizotinib; Erythromycin (Systemic). Monitor therapy
QT-prolonging Quinolone Antibiotics (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Strong CYP3A4 Inhibitors (Moderate Risk): Fluconazole may enhance the QTc-prolonging effect of QT-prolonging Strong CYP3A4 Inhibitors (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Voriconazole. Monitor therapy
QUEtiapine: QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may enhance the QTc-prolonging effect of QUEtiapine. QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk) may increase the serum concentration of QUEtiapine. Management: Monitor for increased quetiapine toxicities including QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QuiNIDine: Fluconazole may enhance the QTc-prolonging effect of QuiNIDine. Fluconazole may increase the serum concentration of QuiNIDine. Avoid combination
Ramelteon: Fluconazole may increase the serum concentration of Ramelteon. Monitor therapy
Ranolazine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Ranolazine. Management: Limit the ranolazine adult dose to a maximum of 500 mg twice daily in patients concurrently receiving moderate CYP3A4 inhibitors (e.g., diltiazem, verapamil, erythromycin, etc.). Consider therapy modification
Red Yeast Rice: Fluconazole may increase the serum concentration of Red Yeast Rice. Specifically, concentrations of lovastatin and related compounds found in Red Yeast Rice may be increased. Monitor therapy
Rifamycin Derivatives: Antifungal Agents (Azole Derivatives, Systemic) may increase the serum concentration of Rifamycin Derivatives. Only rifabutin appears to be affected. Rifamycin Derivatives may decrease the serum concentration of Antifungal Agents (Azole Derivatives, Systemic). Management: Avoid these combinations when possible. Voriconazole and isavuconazonium are considered contraindicated. Consider therapy modification
Rupatadine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Rupatadine. Monitor therapy
Ruxolitinib: Fluconazole may increase the serum concentration of Ruxolitinib. Management: This combination should be avoided under some circumstances. See monograph for details. Consider therapy modification
Saccharomyces boulardii: Antifungal Agents (Systemic, Oral) may diminish the therapeutic effect of Saccharomyces boulardii. Avoid combination
Salmeterol: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Salmeterol. Monitor therapy
SAXagliptin: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of SAXagliptin. Monitor therapy
Sildenafil: Fluconazole may increase the serum concentration of Sildenafil. Monitor therapy
Silodosin: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Silodosin. Monitor therapy
Simeprevir: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Simeprevir. Avoid combination
Simvastatin: Fluconazole may increase the serum concentration of Simvastatin. Monitor therapy
Siponimod: Fluconazole may increase the serum concentration of Siponimod. Management: Coadministration of siponimod with fluconazole, a moderate inhibitor of CYP2C9 and a moderate inhibitor of CYP3A4 is not recommended. Avoid combination
Sirolimus: Fluconazole may increase the serum concentration of Sirolimus. Management: Monitor for increased serum concentrations of sirolimus if combined with fluconazole. Lower initial sirolimus doses or sirolimus dose reductions will likely be required. Consider therapy modification
Sonidegib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Sonidegib. Management: Avoid concomitant use of sonidegib and moderate CYP3A4 inhibitors when possible. When concomitant use cannot be avoided, limit CYP3A4 inhibitor use to less than 14 days and monitor for sonidegib toxicity (particularly musculoskeletal adverse reactions). Consider therapy modification
Sulfonylureas: Fluconazole may increase the serum concentration of Sulfonylureas. Management: Seek alternatives when possible. If used together, monitor closely for increased effects of sulfonylureas if fluconazole is initiated/dose increased, or decreased effects if fluconazole is discontinued/dose decreased. Consider therapy modification
Suvorexant: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Suvorexant. Management: The recommended dose of suvorexant is 5 mg daily in patients receiving a moderate CYP3A4 inhibitor. The dose can be increased to 10 mg daily (maximum dose) if necessary for efficacy. Consider therapy modification
Tacrolimus (Systemic): Fluconazole may increase the serum concentration of Tacrolimus (Systemic). Management: Monitor tacrolimus concentrations closely and adjust oral tacrolimus dose as necessary when concomitantly administered with fluconazole. Reduced doses of tacrolimus will likely be required. Consider therapy modification
Tadalafil: Fluconazole may increase the serum concentration of Tadalafil. Monitor therapy
Tamsulosin: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Tamsulosin. Monitor therapy
Tazemetostat: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Tazemetostat. Management: Avoid coadministration of tazemetostat and moderate CYP3A4 inhibitors. If coadministration cannot be avoided, dose reductions are required. See full monograph for dosing recommendations. Consider therapy modification
Telithromycin: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Telithromycin. Monitor therapy
Temsirolimus: Fluconazole may increase serum concentrations of the active metabolite(s) of Temsirolimus. Management: Consider temsirolimus dose reductions or alternatives to fluconazole. Monitor sirolimus concentrations in all patients receiving fluconazole or any systemic azole antifungal. Consider therapy modification
Terfenadine: Fluconazole may enhance the QTc-prolonging effect of Terfenadine. Fluconazole may increase the serum concentration of Terfenadine. Management: Concomitant use of fluconazole at doses of 400 mg/day or greater and terfenadine is contraindicated and should be avoided. If lower doses of fluconazole and terfenadine are combined, monitor patients for QT-prolongation. Consider therapy modification
Tetrahydrocannabinol: CYP2C9 Inhibitors (Moderate) may increase the serum concentration of Tetrahydrocannabinol. Monitor therapy
Tetrahydrocannabinol: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Tetrahydrocannabinol. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: CYP2C9 Inhibitors (Moderate) may increase the serum concentration of Tetrahydrocannabinol and Cannabidiol. Specifically, concentrations of tetrahydrocannabinol may be increased. Monitor therapy
Tezacaftor and Ivacaftor: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Tezacaftor and Ivacaftor. Management: When combined with moderate CYP3A4 inhibitors, tezacaftor/ivacaftor should be given in the morning, every other day. Ivacaftor alone should be given in the morning, every other day on alternate days. Consider therapy modification
Theophylline Derivatives: Fluconazole may increase the serum concentration of Theophylline Derivatives. Exceptions: Dyphylline. Monitor therapy
Ticagrelor: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Ticagrelor. Monitor therapy
Tipranavir: Fluconazole may increase the serum concentration of Tipranavir. Management: Limit fluconazole adult maximum dose to 200 mg/day in patients treated with tipranavir. Consider therapy modification
Tofacitinib: Fluconazole may increase the serum concentration of Tofacitinib. Management: Tofacitinib dose reductions are recommended when combined with fluconazole. Recommended dose adjustments vary by tofacitinib formulation and therapeutic indication. See full monograph for details. Consider therapy modification
Tolvaptan: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Tolvaptan. Management: Jynarque dose requires adjustment when used with a moderate CYP3A4 inhibitor. See labeling or full interaction monograph for specific recommendations. Use of Samsca with moderate CYP3A4 ihibitors should generally be avoided. Consider therapy modification
Torsemide: CYP2C9 Inhibitors (Moderate) may increase the serum concentration of Torsemide. Monitor therapy
Trabectedin: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Trabectedin. Monitor therapy
Triazolam: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Triazolam. Management: Consider triazolam dose reduction in patients receiving concomitant moderate CYP3A4 inhibitors. Consider therapy modification
Ubrogepant: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Ubrogepant. Management: Use an initial ubrogepant dose of 50 mg and avoid a second dose for 24 hours when used with moderate CYP3A4 inhibitors. Consider therapy modification
Udenafil: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Udenafil. Monitor therapy
Ulipristal: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Ulipristal. Management: This is specific for when ulipristal is being used for signs/symptoms of uterine fibroids (Canadian indication). When ulipristal is used as an emergency contraceptive, patients receiving this combination should be monitored for ulipristal toxicity. Avoid combination
Vardenafil: Fluconazole may increase the serum concentration of Vardenafil. Management: Limit vardenafil doses to a maximum of 5 mg per 24-hour period in patients receiving concurrent therapy with a moderate CYP3A4 inhibitor such as fluconazole. Consider therapy modification
Venetoclax: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Venetoclax. Management: Reduce the venetoclax dose by at least 50% in patients requiring these combinations. Consider therapy modification
Vilazodone: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Vilazodone. Monitor therapy
VinCRIStine: Fluconazole may increase the serum concentration of VinCRIStine. Monitor therapy
Vindesine: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Vindesine. Monitor therapy
Vitamin K Antagonists (eg, warfarin): Fluconazole may increase the serum concentration of Vitamin K Antagonists. Consider therapy modification
Voriconazole: Fluconazole may enhance the QTc-prolonging effect of Voriconazole. Fluconazole may increase the serum concentration of Voriconazole. Avoid combination
Voxelotor: Fluconazole may increase the serum concentration of Voxelotor. Management: Avoid concomitant use of voxelotor and fluconazole. If concomitant use is unavoidable, reduce the voxelotor dose to 1,000 mg once daily. Consider therapy modification
Zanubrutinib: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Zanubrutinib. Management: Decrease the zanubrutinib dose to 80 mg twice daily during coadministration with a moderate CYP3A4 inhibitor. Further dose adjustments may be required for zanubrutinib toxicities, refer to prescribing information for details. Consider therapy modification
Zidovudine: Fluconazole may decrease the metabolism of Zidovudine. Monitor therapy
Zopiclone: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Zopiclone. Management: The starting adult dose of zopiclone should not exceed 3.75 mg if combined with a moderate CYP3A4 inhibitor. Monitor patients for signs and symptoms of zopiclone toxicity if these agents are combined. Consider therapy modification
Zuclopenthixol: CYP3A4 Inhibitors (Moderate) may increase the serum concentration of Zuclopenthixol. Monitor therapy
Adverse Reactions
>10%: Central nervous system: Headache (adults: 2% to 13%)
1% to 10%:
Central nervous system: Dizziness (adults: 1%)
Dermatologic: Skin rash (adults: 2%)
Gastrointestinal: Nausea (adults: 4% to 7%; children and adolescents: 2%), abdominal pain (2% to 6%), vomiting (2% to 5%), diarrhea (2% to 3%), dysgeusia (adults: 1%), dyspepsia (adults: 1%)
Frequency not defined: Hepatic: Fulminant hepatitis, hepatitis, increased serum alkaline phosphatase, increased serum aspartate aminotransferase, increased serum transaminases, jaundice
<1%, postmarketing, and/or case reports: Acute generalized exanthematous pustulosis, agranulocytosis, alopecia, anaphylaxis, angioedema, asthenia, cholestasis, diaphoresis, DRESS syndrome, drowsiness, exfoliative dermatitis, fatigue, fever, fixed drug eruption, hepatic failure, hepatotoxicity, hypercholesterolemia, hypertriglyceridemia, hypokalemia, insomnia, leukopenia, malaise, myalgia, neutropenia, paresthesia, prolonged QT interval on ECG, seizure, Stevens-Johnson syndrome, thrombocytopenia, torsades de pointes, toxic epidermal necrolysis, tremor, vertigo, xerostomia
Warnings/Precautions
Concerns related to adverse effects:
- Arrhythmias: Cases of QTc prolongation and torsade de pointes associated with fluconazole use have been reported (usually high dose or in combination with agents known to prolong the QT interval); use caution in patients with concomitant medications or conditions which are arrhythmogenic.
- CNS effects: May occasionally cause dizziness or seizures; use caution driving or operating machinery.
- Hepatotoxicity: Serious (and sometimes fatal) hepatic toxicity (eg, hepatitis, cholestasis, fulminant hepatic failure) has been observed. Monitor patients who develop abnormal liver function tests for the development of more severe hepatic injury; discontinue fluconazole if signs and symptoms consistent with liver disease develop.
- Hypersensitivity reactions: Anaphylaxis has been reported rarely; use with caution in patients with hypersensitivity to other azoles.
- Skin reactions: Rare exfoliative skin disorders have been observed; fatal outcomes have been reported in patients with serious concomitant diseases. Monitor patients with deep seated fungal infections closely for rash development and discontinue if lesions progress. In patients with superficial fungal infections who develop a rash attributable to fluconazole, treatment should also be discontinued.
Disease-related concerns:
- Hepatic impairment: Use with caution in patients with preexisting hepatic impairment; monitor liver function closely and discontinue if symptoms consistent with liver disease develop.
- Renal impairment: Use with caution in patients with renal impairment; dosage adjustment may be necessary.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Dosage form specific issues:
- Benzyl alcohol and derivatives: Some dosage forms may contain sodium benzoate/benzoic acid; benzoic acid (benzoate) is a metabolite of benzyl alcohol; large amounts of benzyl alcohol (≥99 mg/kg/day) have been associated with a potentially fatal toxicity (“gasping syndrome”) in neonates; the “gasping syndrome” consists of metabolic acidosis, respiratory distress, gasping respirations, CNS dysfunction (including convulsions, intracranial hemorrhage), hypotension, and cardiovascular collapse (AAP 1997; CDC 1982); some data suggests that benzoate displaces bilirubin from protein binding sites (Ahlfors 2001); avoid or use dosage forms containing benzyl alcohol derivative with caution in neonates. See manufacturer’s labeling.
- Sucrose: Oral suspension contains sucrose; avoid use in patients with fructose intolerance, glucose-galactose malabsorption, or sucrase-isomaltase insufficiency.
Monitoring Parameters
Periodic liver function tests (AST, ALT, alkaline phosphatase) and renal function tests, potassium
Pregnancy
Pregnancy Considerations
Following exposure during the first trimester, malformations have been noted in humans when fluconazole was used in higher doses (≥400 mg/day). Abnormalities reported include brachycephaly, abnormal facies, abnormal calvarial development, cleft palate, femoral bowing, thin ribs and long bones, arthrogryposis, and congenital heart disease. Use of lower doses (150 mg as a single dose) suggest increased risks to the fetus, however, additional study is needed.
Use of oral fluconazole for vaginal candidiasis is not recommended in pregnant women (HHS [OI adult 2017]; Workowski [CDC 2015]). Most azole antifungals, including fluconazole, are recommended to be avoided during the first trimester of pregnancy (IDSA [Pappas 2016]).
The manufacturer recommends females of childbearing potential taking higher doses (≥400 mg/day) use effective contraception during therapy and for ~1 week after the final fluconazole dose.
Patient Education
What is this drug used for?
- It is used to treat fungal infections.
- It is used to prevent fungal infections.
- This drug is used to treat vaginal yeast infections.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Headache
- Nausea
- Vomiting
- Dizziness
- Abdominal pain
- Diarrhea
- Change in taste
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Adrenal gland problems like severe nausea, vomiting, severe dizziness, passing out, muscle weakness, severe fatigue, mood changes, lack of appetite, or weight loss.
- Fast heartbeat
- Abnormal heartbeat
- Passing out
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.