Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Capsule, Inhalation:
Seebri Neohaler: 15.6 mcg [contains lactose monohydrate, milk protein]
Seebri Neohaler: 15.6 mcg [DSC] [contains milk protein]
Solution, Inhalation:
Lonhala Magnair Refill Kit: 25 mcg/mL (1 mL)
Lonhala Magnair Starter Kit: 25 mcg/mL (1 mL)
Pharmacology
Mechanism of Action
Competitively and reversibly inhibits the action of acetylcholine at muscarinic receptor subtypes 1 to 3 (greater affinity for subtypes 1 and 3) in bronchial smooth muscle thereby causing bronchodilation
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid
Distribution
Vd: Steady state: 83 L; Terminal phase: 376 L
Metabolism
Hepatic (minimal)
Excretion
Urine; bile
Time to Peak
Plasma: Dry powder inhaler (capsule): 5 minutes; Nebulization solution: <20 minutes
Half-Life Elimination
33 to 53 hours
Protein Binding
38% to 41%
Use: Labeled Indications
Chronic obstructive pulmonary disease: Maintenance treatment of airflow obstruction in patients with chronic obstructive pulmonary disease (COPD), including chronic bronchitis and/or emphysema.
Contraindications
Hypersensitivity to glycopyrrolate or any component of the formulation.
Canadian labeling: Additional contraindications (not in US labeling): Severe hypersensitivity to milk proteins.
Dosage and Administration
Dosing: Adult
Chronic obstructive pulmonary disease (COPD): Inhalation:
Dry powder inhaler (capsule): One capsule (15.6 mcg) inhaled twice daily (maximum: 15.6 mcg twice daily)
Seebri Breezhaler [Canadian product]: One capsule (50 mcg) inhaled once daily
Nebulization solution: One vial (25 mcg) inhaled twice daily (maximum: 25 mcg twice daily)
Dosing: Geriatric
Refer to adult dosing.
Administration
Inhalation: For oral inhalation only.
Dry powder inhaler (capsule): Do not swallow capsules. Administer at the same time each day; use only with the Neohaler device. Do not remove capsules from blister until immediately before use. Use the new inhaler included with each prescription. Discard any capsules that are exposed to air and not used immediately. Refer to manufacturer's product labeling for additional administration instructions.
Nebulization solution: Do not inject or swallow solution; use only with Magnair device. Remove vials from foil pouch immediately before use. Administer once in morning and once in evening at the same time each day. Refer to manufacturer's product labeling for additional administration instructions.
Storage
Dry powder inhaler (capsule): Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Protect from moisture. Remove capsule from blister pack immediately before use; discard capsule if not used immediately.
Nebulization solution: Store in foil pouch at 20°C to 25°C (68°F to 77°F). After opening protective foil pouch, unused vials should be returned to and stored in opened foil pouch; discard vials if not used within 7 days of opening foil pouch. Use opened vials immediately.
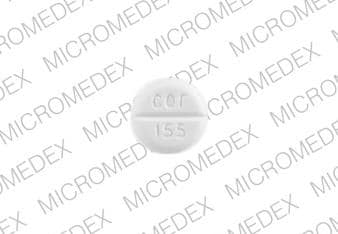
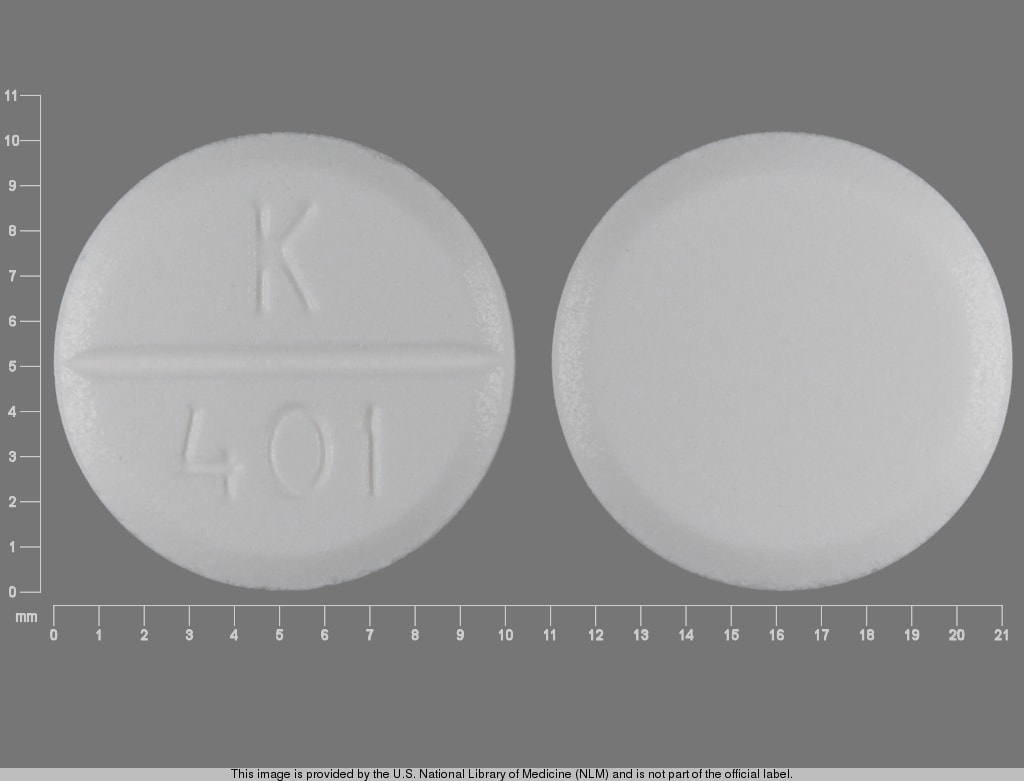
Glycopyrrolate (Oral Inhalation) Images
Drug Interactions
Acetylcholinesterase Inhibitors: May diminish the therapeutic effect of Anticholinergic Agents. Anticholinergic Agents may diminish the therapeutic effect of Acetylcholinesterase Inhibitors. Monitor therapy
Aclidinium: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Amantadine: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Anticholinergic Agents: May enhance the anticholinergic effect of Glycopyrrolate (Oral Inhalation). Avoid combination
Botulinum Toxin-Containing Products: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Cannabinoid-Containing Products: Anticholinergic Agents may enhance the tachycardic effect of Cannabinoid-Containing Products. Exceptions: Cannabidiol. Monitor therapy
Chloral Betaine: May enhance the adverse/toxic effect of Anticholinergic Agents. Monitor therapy
Cimetropium: Anticholinergic Agents may enhance the anticholinergic effect of Cimetropium. Avoid combination
Eluxadoline: Anticholinergic Agents may enhance the constipating effect of Eluxadoline. Avoid combination
Gastrointestinal Agents (Prokinetic): Anticholinergic Agents may diminish the therapeutic effect of Gastrointestinal Agents (Prokinetic). Monitor therapy
Glucagon: Anticholinergic Agents may enhance the adverse/toxic effect of Glucagon. Specifically, the risk of gastrointestinal adverse effects may be increased. Monitor therapy
Glycopyrronium (Topical): May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Ipratropium (Oral Inhalation): May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Itopride: Anticholinergic Agents may diminish the therapeutic effect of Itopride. Monitor therapy
Levosulpiride: Anticholinergic Agents may diminish the therapeutic effect of Levosulpiride. Avoid combination
Methacholine: Long-acting muscarinic antagonists (LAMAs) may diminish the therapeutic effect of Methacholine. Consider therapy modification
Mianserin: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Mirabegron: Anticholinergic Agents may enhance the adverse/toxic effect of Mirabegron. Monitor therapy
Nitroglycerin: Anticholinergic Agents may decrease the absorption of Nitroglycerin. Specifically, anticholinergic agents may decrease the dissolution of sublingual nitroglycerin tablets, possibly impairing or slowing nitroglycerin absorption. Monitor therapy
Opioid Agonists: Anticholinergic Agents may enhance the adverse/toxic effect of Opioid Agonists. Specifically, the risk for constipation and urinary retention may be increased with this combination. Monitor therapy
Oxatomide: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Potassium Chloride: Anticholinergic Agents may enhance the ulcerogenic effect of Potassium Chloride. Management: Patients on drugs with substantial anticholinergic effects should avoid using any solid oral dosage form of potassium chloride. Avoid combination
Potassium Citrate: Anticholinergic Agents may enhance the ulcerogenic effect of Potassium Citrate. Avoid combination
Pramlintide: May enhance the anticholinergic effect of Anticholinergic Agents. These effects are specific to the GI tract. Consider therapy modification
Ramosetron: Anticholinergic Agents may enhance the constipating effect of Ramosetron. Monitor therapy
Revefenacin: Anticholinergic Agents may enhance the anticholinergic effect of Revefenacin. Avoid combination
Secretin: Anticholinergic Agents may diminish the therapeutic effect of Secretin. Management: Avoid concomitant use of anticholinergic agents and secretin. Discontinue anticholinergic agents at least 5 half-lives prior to administration of secretin. Consider therapy modification
Thiazide and Thiazide-Like Diuretics: Anticholinergic Agents may increase the serum concentration of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Tiotropium: Anticholinergic Agents may enhance the anticholinergic effect of Tiotropium. Avoid combination
Topiramate: Anticholinergic Agents may enhance the adverse/toxic effect of Topiramate. Monitor therapy
Umeclidinium: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Adverse Reactions
1% to 10%:
Cardiovascular: Peripheral edema (<2%)
Central nervous system: Fatigue (≥2%)
Gastrointestinal: Diarrhea (≥2%), nausea (≥2%), upper abdominal pain (≥2%)
Genitourinary: Urinary tract infection (2%)
Neuromuscular & skeletal: Arthralgia (≥2%), back pain (≥2%)
Respiratory: Dyspnea (≤5%), upper respiratory tract infection (2% to 3%), bronchitis (≥2%), nasopharyngitis (≥2%), pneumonia (≥2%), rhinitis (≥2%), wheezing (≥2%), oropharyngeal pain (2%), sinusitis (1%)
<1% postmarketing, and/or case reports: Angioedema, atrial fibrillation, cough, diabetes mellitus, dysuria, gastroenteritis, hypersensitivity reaction, insomnia, limb pain, paradoxical bronchospasm, productive cough, pruritus, skin rash, voice disorder, vomiting
Warnings/Precautions
Concerns related to adverse effects:
- Bronchospasm: Paradoxical bronchospasm may occur with the use of inhaled agents which may be life-threatening; discontinue use immediately and consider other therapy if bronchospasm occurs.
- CNS effects: May cause drowsiness and/or blurred vision, which may impair physical or mental abilities; patients must be cautioned about performing tasks which require mental alertness (eg, operating machinery or driving).
- Hypersensitivity: Immediate hypersensitivity reactions have been reported; if signs suggesting allergic reactions occur, in particular, angioedema (including difficulties in breathing or swallowing, swelling of the tongue, lips, and face), urticaria, or skin rash, discontinue therapy immediately and initiate alternative therapy. Use with caution in patients with severe hypersensitivity to milk proteins.
Disease-related concerns:
- Cardiovascular disease: Cardiovascular effects (eg, atrial fibrillation, tachycardia) may occur after administration. Use with caution in patients with unstable ischemic heart disease, left ventricular failure, history of myocardial infarction, arrhythmia (excluding chronic stable atrial fibrillation), a history of long QT syndrome or whose QTc was prolonged at screening. In some cases, treatment may need to be discontinued.
- Glaucoma: Use with caution in patients with narrow-angle glaucoma. Monitor for signs/symptoms of glaucoma.
- Renal impairment: Use with caution in patients with severe renal impairment, including end stage renal disease (ESRD) requiring dialysis; systemic exposure to glycopyrrolate may be increased.
- Urinary retention: Use with caution in patients with urinary retention. Monitor for signs and symptoms of urinary retention, especially in patients with prostatic hyperplasia or bladder-neck obstruction.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Dosage form specific issues:
- Appropriate use: Not indicated for the initial (rescue) treatment of acute episodes of bronchospasm or with acutely deteriorating or potentially life-threatening COPD; after initiation of therapy, patients should use short-acting bronchodilators only on an as needed basis for acute symptoms.
- Lactose: The dry powder inhaler formulation may contain lactose.
Monitoring Parameters
FEV1, peak flow (or other pulmonary function tests); signs/symptoms of glaucoma; hypersensitivity reactions; urinary retention
Pregnancy
Pregnancy Risk Factor
C
Pregnancy Considerations
Adverse events have been observed in some animal reproduction studies. Small amounts of glycopyrrolate cross the human placenta following IM injection.
Patient Education
What is this drug used for?
- It is used to treat COPD (chronic obstructive pulmonary disease).
- This drug is not to be used to treat intense flare-ups of shortness of breath. Use a rescue inhaler. Talk with the doctor.
Frequently reported side effects of this drug
- Nasal irritation
- Throat irritation
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Urinary tract infection like blood in your urine, burning or painful urination, passing a lot of urine, fever, lower abdominal pain, or pelvic pain
- Severe nausea
- Severe vomiting
- Vision changes
- Eye pain
- Severe eye irritation
- Seeing halos or bright colors around lights
- Eye redness
- Painful urination
- Trouble urinating
- Passing a lot of urine
- Trouble breathing
- Wheezing
- Cough
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.