Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Capsule, Oral, as pamoate:
Vistaril: 25 mg, 50 mg
Generic: 25 mg, 50 mg, 100 mg
Solution, Intramuscular, as hydrochloride:
Generic: 25 mg/mL (1 mL); 50 mg/mL (1 mL, 2 mL, 10 mL [DSC])
Syrup, Oral, as hydrochloride:
Generic: 10 mg/5 mL (25 mL, 118 mL, 473 mL)
Tablet, Oral, as hydrochloride:
Generic: 10 mg, 25 mg, 50 mg
Pharmacology
Mechanism of Action
Competes with histamine for H1-receptor sites on effector cells in the gastrointestinal tract, blood vessels, and respiratory tract (Simons 1994). Possesses skeletal muscle relaxing, bronchodilator, antihistamine, antiemetic, and analgesic properties.
Pharmacokinetics/Pharmacodynamics
Absorption
Oral: Rapid
Distribution
Children and Adolescents 1 to 14 years: 18.5 ± 8.6 L/kg (Simons F 1984a); Adults: Vd: 16 ± 3 L/kg (Simons F 1984); Elderly: ~23 L/kg (Simons K 1989); Hepatic dysfunction: ~23 L/kg (Simons F 1989)
Metabolism
Hepatic to multiple metabolites, including cetirizine (active) (Simons F 1989)
Excretion
Urine; active metabolite (cetirizine) is renally eliminated (Simons F 1994)
Onset of Action
Oral: 15 to 30 minutes; IM: Rapid
Time to Peak
Oral administration: Serum: ~2 hours; Peak suppression of antihistamine-induced wheal and flare: 4 to 12 hours (Simons F 1984)
Duration of Action
Decreased histamine-induced wheal and flare areas: 2 to ≥36 hours; Suppression of pruritus: 1 to 12 hours (Simon F 1984)
Half-Life Elimination
Children and Adolescents 1 to 14 years (mean age: 6.1 ± 4.6 years): 7.1 ± 2.3 hours; Note: Half-life increased with increasing age and was 4 hours in patients 1-year old and 11 hours in a 14-year old patient (Simons F 1984a)
Adults: ~20 hours (Simons 1984); Elderly: ~29 hours (Simons K 1989); Hepatic dysfunction: ~37 hours (Simons F 1989)
Use: Labeled Indications
Oral:
Anxiety: Symptomatic relief of anxiety and tension associated with psychoneurosis; adjunct in organic disease states in which anxiety is manifested.
Perioperative adjunct: As a sedative when used as premedication and following general anesthesia
Pruritus: Management of pruritus due to allergic conditions (eg, chronic urticaria, atopic and contact dermatoses) and in histamine-mediated pruritus.
Intramuscular:
Allergic conditions: Adjunctive therapy in allergic conditions with strong emotional overlay (eg, asthma, chronic urticaria, pruritus).
Antiemetic: Control of nausea and vomiting.
Anxiety: Management of anxiety, tension, and psychomotor agitation in conditions of emotional stress, in preparation for dental procedures, and as adjunctive therapy in alcoholism; management of anxiety associated with organic disturbances. Note: Should not be used as the sole treatment of psychosis or of clearly demonstrated cases of depression.
Perioperative adjunct: As pre- and postoperative adjunctive medication to permit reduction in opioid dosage, allay anxiety, and control emesis.
Peripartum adjunct: As pre- and postpartum adjunctive medication to permit reduction in opioid dosage, allay anxiety, and control emesis.
Contraindications
Hypersensitivity to hydroxyzine or any component of the formulation; early pregnancy; prolonged QT interval
Additional contraindications:
Oral: Hypersensitivity to cetirizine or levocetirizine
Injection: SubQ, intra-arterial, or IV administration
Canadian labeling: Additional contraindications (not in US labeling): Oral: Hypersensitivity to other piperazine derivatives, aminophylline or ethylenediamine; history of history of cardiac arrhythmias; significant electrolyte imbalance (eg, hypokalemia, hypomagnesemia); significant bradycardia; family history of sudden cardiac death; concomitant use with other QT interval prolonging drugs or with CYP3A4/5 inhibitors; asthmatics who have previously experienced a serious anti-histamine induced adverse bronchopulmonary effect; porphyria.
Dosage and Administration
Dosing: Adult
Antiemetic: IM: 25 to 100 mg/dose
Anxiety:
Oral:
Manufacturer’s labeling: 50 to 100 mg 4 times daily
Alternative recommendations (off-label dosing): 37.5 to 75 mg daily in divided doses (WFSBP [Bandelow 2008]; WFSBP [Bandelow 2012])
IM: Initial: 50 to 100 mg, then every 4 to 6 hours as needed
Peripartum adjunct: IM: 25 to 100 mg
Perioperative adjunct:
Oral: 50 to 100 mg
IM: 25 to 100 mg
Pruritus: Oral: 25 mg 3 to 4 times daily
Dosing: Geriatric
Avoid use (Beers Criteria [AGS 2019]).
Dosing: Pediatric
Antiemetic: Note: Expert recommendations for postoperative nausea and vomiting (PONV) management do not suggest hydroxyzine as a therapeutic option; use has typically been replaced by newer agents with an improved safety profile (SAA [Gan 2014]). Infants, Children, and Adolescents: IM: 1.1 mg/kg/dose; maximum dose: 100 mg/dose.
Anxiety: Note: Although FDA approved for use in anxiety, data in pediatric patients are sparse; expert recommendations for pediatric patients do not consider hydroxyzine a therapeutic option for the management of anxiety disorders (eg, generalized anxiety disorder, separation anxiety, specific phobias, panic disorder, PTSD); use has generally been replaced by newer, more effective agents (AACAP [Connolly 2007]; Bushnell 2018; Gale 2016)
Children and Adolescents: Oral: 0.5 mg/kg/dose every 6 hours; maximum dose is age-dependent: Age <6 years: 12.5 mg/dose; age ≥6 years: 25 mg/dose (Kliegman 2016; Nelson 1996; manufacturer's labeling). Note: In pediatric patients, some experts have recommended lower initial doses, although reported experience is lacking. In adults, experts suggest a lower daily dosing regimen of 37.5 to 75 mg/day in divided doses (WFSBP [Bandelow 2008]; WFSBP [Bandelow 2012]).
Pruritus; associated with allergic conditions or chronic urticaria: Children and Adolescents:
Age-directed dosing:
Children <6 years: Oral: 12.5 mg 3 to 4 times daily (Nelson 1996; manufacturer's labeling)
Children ≥6 years and Adolescents: Oral: 12.5 to 25 mg 3 to 4 times daily (Nelson 1996; manufacturer's labeling). Note: Based on pharmacokinetic studies, dosing once daily (at bedtime) or twice daily may be adequate due to the long half-life (Simons 1984a).
Weight-directed dosing:
Patient weight ≤40 kg: Oral: 2 mg/kg/day divided every 6 to 8 hours as needed; maximum dose: 25 mg/dose. Note: Based on pharmacokinetic studies, dosing once daily (at bedtime) or twice daily may be adequate due to the long half-life (Nelson 1996; Simons 1984; Simons 1984a; Simons 1994).
Patient weight >40 kg: Oral: 25 to 50 mg once daily at bedtime or twice daily (Simons 1984a; Simons 1994)
Pruritus; associated with opioid use: Limited data available: Children and Adolescents: IM, Oral: 0.5 mg/kg/dose every 6 hours as needed; usual maximum dose: 50 mg/dose (Berde 1990; Kliegman 2016)
Sedation; pre-/postoperative, adjunctive therapy: Note: Although FDA approved, pre-/postoperative hydroxyzine use has largely been replaced by other agents.
Oral: Children and Adolescents: 0.6 mg/kg/dose; maximum dose: 100 mg/dose
IM: Infants, Children, and Adolescents: 1.1 mg/kg/dose; maximum dose: 100 mg/dose
Sedation; procedural, adjunctive therapy (eg, dental, echocardiography): Limited data available: Children 2 to 12 years: Oral: 1 mg/kg/dose as a single dose 30 to 45 minutes prior to procedure in combination with other sedatives (eg, midazolam, chloral hydrate) has been used in children prior to dental procedures or echocardiograms; maximum dose: 100 mg/dose (Chowdhury 2005; Olacke 2018; Roach 2010)
Administration
IM: For IM use only. Aspirate before injection to avoid inadvertent injection into a blood vessel. Do NOT administer IV, SubQ, or intra-arterially (contraindicated). Administer IM deep in large muscle. The preferred site is the upper outer quadrant of the buttock or midlateral thigh. The upper outer quadrant of the gluteal region should be used only when necessary to minimize potential damage to the sciatic nerve. The deltoid region should be only used with caution to avoid radial nerve injury. Injections should not be made in the lower or mid-third of the upper arm.
Oral: Administer without regard to food. Shake suspension vigorously prior to use.
Storage
Injection: Store at 20°C to 25°C (68°F to 77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Protect from light.
Oral: Store at 20°C to 25°C (68°F to 77°F). Protect oral solution from light; do not freeze.
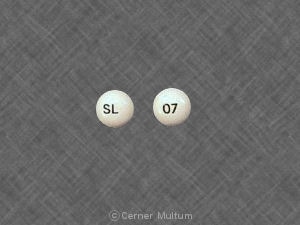
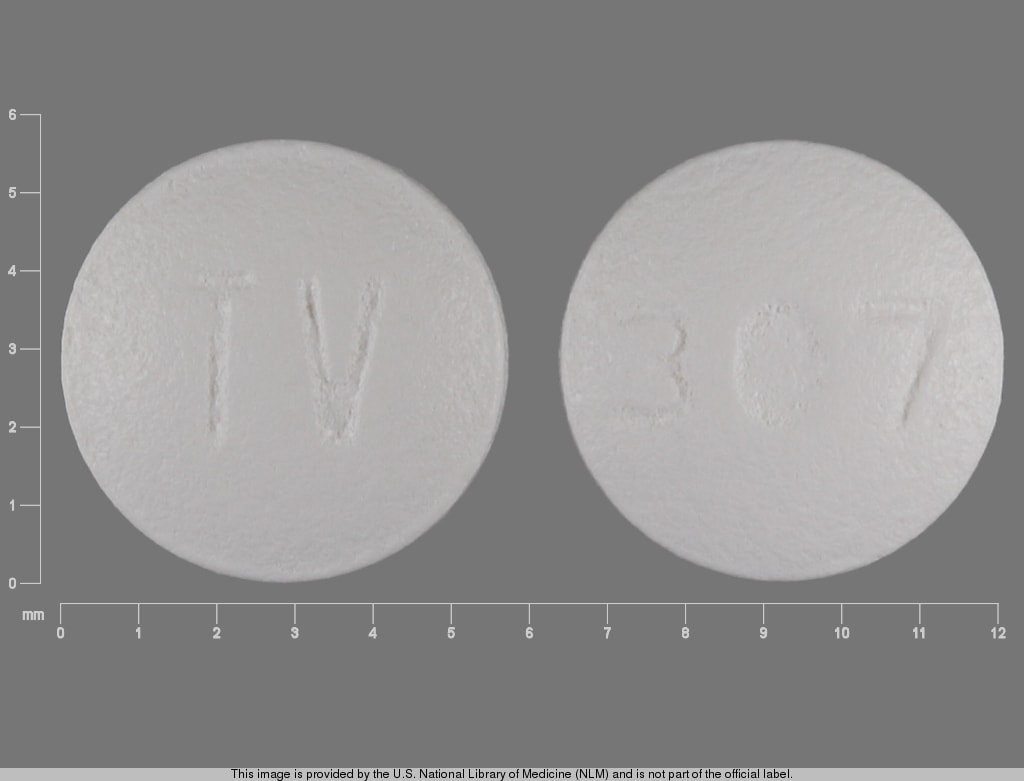
HydrOXYzine Images
Drug Interactions
Acetylcholinesterase Inhibitors: May diminish the therapeutic effect of Anticholinergic Agents. Anticholinergic Agents may diminish the therapeutic effect of Acetylcholinesterase Inhibitors. Monitor therapy
Aclidinium: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Alcohol (Ethyl): CNS Depressants may enhance the CNS depressant effect of Alcohol (Ethyl). Monitor therapy
Alizapride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Amantadine: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Amezinium: Antihistamines may enhance the stimulatory effect of Amezinium. Monitor therapy
Amphetamines: May diminish the sedative effect of Antihistamines. Monitor therapy
Anticholinergic Agents: May enhance the adverse/toxic effect of other Anticholinergic Agents. Monitor therapy
Azelastine (Nasal): CNS Depressants may enhance the CNS depressant effect of Azelastine (Nasal). Avoid combination
Barbiturates: HydrOXYzine may enhance the CNS depressant effect of Barbiturates. Management: Consider a decrease in the barbiturate dose, as appropriate, when used together with hydroxyzine. With concurrent use, monitor patients closely for excessive response to the combination. Consider therapy modification
Benzylpenicilloyl Polylysine: Antihistamines may diminish the diagnostic effect of Benzylpenicilloyl Polylysine. Management: Suspend systemic H1 antagonists for benzylpenicilloyl-polylysine skin testing and delay testing until systemic antihistaminic effects have dissipated. A histamine skin test may be used to assess persistent antihistaminic effects. Consider therapy modification
Betahistine: Antihistamines may diminish the therapeutic effect of Betahistine. Monitor therapy
Blonanserin: CNS Depressants may enhance the CNS depressant effect of Blonanserin. Consider therapy modification
Botulinum Toxin-Containing Products: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Brexanolone: CNS Depressants may enhance the CNS depressant effect of Brexanolone. Monitor therapy
Brimonidine (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromopride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromperidol: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Buprenorphine: CNS Depressants may enhance the CNS depressant effect of Buprenorphine. Management: Consider reduced doses of other CNS depressants, and avoiding such drugs in patients at high risk of buprenorphine overuse/self-injection. Initiate buprenorphine at lower doses in patients already receiving CNS depressants. Consider therapy modification
Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Cannabis: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Chloral Betaine: May enhance the adverse/toxic effect of Anticholinergic Agents. Monitor therapy
Chlormethiazole: May enhance the CNS depressant effect of CNS Depressants. Management: Monitor closely for evidence of excessive CNS depression. The chlormethiazole labeling states that an appropriately reduced dose should be used if such a combination must be used. Consider therapy modification
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Cimetropium: Anticholinergic Agents may enhance the anticholinergic effect of Cimetropium. Avoid combination
CNS Depressants: HydrOXYzine may enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Dimethindene (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Doxylamine: May enhance the CNS depressant effect of CNS Depressants. Management: The manufacturer of Diclegis (doxylamine/pyridoxine), intended for use in pregnancy, specifically states that use with other CNS depressants is not recommended. Monitor therapy
Dronabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Droperidol: May enhance the CNS depressant effect of CNS Depressants. Management: Consider dose reductions of droperidol or of other CNS agents (eg, opioids, barbiturates) with concomitant use. Exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Consider therapy modification
Eluxadoline: Anticholinergic Agents may enhance the constipating effect of Eluxadoline. Avoid combination
Esketamine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Flunitrazepam: CNS Depressants may enhance the CNS depressant effect of Flunitrazepam. Consider therapy modification
Gastrointestinal Agents (Prokinetic): Anticholinergic Agents may diminish the therapeutic effect of Gastrointestinal Agents (Prokinetic). Monitor therapy
Glucagon: Anticholinergic Agents may enhance the adverse/toxic effect of Glucagon. Specifically, the risk of gastrointestinal adverse effects may be increased. Monitor therapy
Glycopyrrolate (Oral Inhalation): Anticholinergic Agents may enhance the anticholinergic effect of Glycopyrrolate (Oral Inhalation). Avoid combination
Glycopyrronium (Topical): May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Haloperidol: QT-prolonging Agents (Indeterminate Risk - Caution) may enhance the QTc-prolonging effect of Haloperidol. Monitor therapy
Hyaluronidase: Antihistamines may diminish the therapeutic effect of Hyaluronidase. Management: Patients receiving antihistamines (particularly at larger doses) may not experience the desired clinical response to standard doses of hyaluronidase. Larger doses of hyaluronidase may be required. Consider therapy modification
HYDROcodone: CNS Depressants may enhance the CNS depressant effect of HYDROcodone. Management: Avoid concomitant use of hydrocodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Ipratropium (Oral Inhalation): May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Itopride: Anticholinergic Agents may diminish the therapeutic effect of Itopride. Monitor therapy
Kava Kava: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Lemborexant: May enhance the CNS depressant effect of CNS Depressants. Management: Dosage adjustments of lemborexant and of concomitant CNS depressants may be necessary when administered together because of potentially additive CNS depressant effects. Close monitoring for CNS depressant effects is necessary. Consider therapy modification
Levosulpiride: Anticholinergic Agents may diminish the therapeutic effect of Levosulpiride. Avoid combination
Lofexidine: May enhance the CNS depressant effect of CNS Depressants. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Magnesium Sulfate: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Meperidine: HydrOXYzine may enhance the CNS depressant effect of Meperidine. Management: Consider a decrease in meperidine dose, as appropriate, when used together with hydroxyzine. With concurrent use, monitor patients closely for excessive response to the combination. Consider therapy modification
Methotrimeprazine: CNS Depressants may enhance the CNS depressant effect of Methotrimeprazine. Methotrimeprazine may enhance the CNS depressant effect of CNS Depressants. Management: Reduce adult dose of CNS depressant agents by 50% with initiation of concomitant methotrimeprazine therapy. Further CNS depressant dosage adjustments should be initiated only after clinically effective methotrimeprazine dose is established. Consider therapy modification
MetyroSINE: CNS Depressants may enhance the sedative effect of MetyroSINE. Monitor therapy
Mianserin: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Minocycline (Systemic): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Mirabegron: Anticholinergic Agents may enhance the adverse/toxic effect of Mirabegron. Monitor therapy
Nabilone: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Nitroglycerin: Anticholinergic Agents may decrease the absorption of Nitroglycerin. Specifically, anticholinergic agents may decrease the dissolution of sublingual nitroglycerin tablets, possibly impairing or slowing nitroglycerin absorption. Monitor therapy
Opioid Agonists: CNS Depressants may enhance the CNS depressant effect of Opioid Agonists. Management: Avoid concomitant use of opioid agonists and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Orphenadrine: CNS Depressants may enhance the CNS depressant effect of Orphenadrine. Avoid combination
Oxatomide: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Oxomemazine: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
OxyCODONE: CNS Depressants may enhance the CNS depressant effect of OxyCODONE. Management: Avoid concomitant use of oxycodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Paraldehyde: CNS Depressants may enhance the CNS depressant effect of Paraldehyde. Avoid combination
Perampanel: May enhance the CNS depressant effect of CNS Depressants. Management: Patients taking perampanel with any other drug that has CNS depressant activities should avoid complex and high-risk activities, particularly those such as driving that require alertness and coordination, until they have experience using the combination. Consider therapy modification
Piribedil: CNS Depressants may enhance the CNS depressant effect of Piribedil. Monitor therapy
Pitolisant: Antihistamines may diminish the therapeutic effect of Pitolisant. Avoid combination
Potassium Chloride: Anticholinergic Agents may enhance the ulcerogenic effect of Potassium Chloride. Management: Patients on drugs with substantial anticholinergic effects should avoid using any solid oral dosage form of potassium chloride. Avoid combination
Potassium Citrate: Anticholinergic Agents may enhance the ulcerogenic effect of Potassium Citrate. Avoid combination
Pramipexole: CNS Depressants may enhance the sedative effect of Pramipexole. Monitor therapy
Pramlintide: May enhance the anticholinergic effect of Anticholinergic Agents. These effects are specific to the GI tract. Consider therapy modification
QT-prolonging Agents (Highest Risk): QT-prolonging Agents (Indeterminate Risk - Caution) may enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Ramosetron: Anticholinergic Agents may enhance the constipating effect of Ramosetron. Monitor therapy
Revefenacin: Anticholinergic Agents may enhance the anticholinergic effect of Revefenacin. Avoid combination
ROPINIRole: CNS Depressants may enhance the sedative effect of ROPINIRole. Monitor therapy
Rotigotine: CNS Depressants may enhance the sedative effect of Rotigotine. Monitor therapy
Rufinamide: May enhance the adverse/toxic effect of CNS Depressants. Specifically, sleepiness and dizziness may be enhanced. Monitor therapy
Secretin: Anticholinergic Agents may diminish the therapeutic effect of Secretin. Management: Avoid concomitant use of anticholinergic agents and secretin. Discontinue anticholinergic agents at least 5 half-lives prior to administration of secretin. Consider therapy modification
Selective Serotonin Reuptake Inhibitors: CNS Depressants may enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk of psychomotor impairment may be enhanced. Monitor therapy
Sodium Oxybate: May enhance the CNS depressant effect of CNS Depressants. Management: Consider alternatives to combined use. When combined use is needed, consider minimizing doses of one or more drugs. Use of sodium oxybate with alcohol or sedative hypnotics is contraindicated. Consider therapy modification
Suvorexant: CNS Depressants may enhance the CNS depressant effect of Suvorexant. Management: Dose reduction of suvorexant and/or any other CNS depressant may be necessary. Use of suvorexant with alcohol is not recommended, and the use of suvorexant with any other drug to treat insomnia is not recommended. Consider therapy modification
Tapentadol: May enhance the CNS depressant effect of CNS Depressants. Management: Avoid concomitant use of tapentadol and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Tetrahydrocannabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Thalidomide: CNS Depressants may enhance the CNS depressant effect of Thalidomide. Avoid combination
Thiazide and Thiazide-Like Diuretics: Anticholinergic Agents may increase the serum concentration of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Tiotropium: Anticholinergic Agents may enhance the anticholinergic effect of Tiotropium. Avoid combination
Topiramate: Anticholinergic Agents may enhance the adverse/toxic effect of Topiramate. Monitor therapy
Trimeprazine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Umeclidinium: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Zolpidem: CNS Depressants may enhance the CNS depressant effect of Zolpidem. Management: Reduce the Intermezzo brand sublingual zolpidem adult dose to 1.75 mg for men who are also receiving other CNS depressants. No such dose change is recommended for women. Avoid use with other CNS depressants at bedtime; avoid use with alcohol. Consider therapy modification
Test Interactions
May cause false-positive serum TCA screen (Dasgupta 2007).
Adverse Reactions
Frequency not defined:
Central nervous system: Drowsiness (transient)
Gastrointestinal: Xerostomia
Respiratory: Respiratory depression (high doses)
<1%, postmarketing, and/or case reports: Acute generalized exanthematous pustulosis, fixed drug eruption, hallucination, headache, hypersensitivity reaction, involuntary movements, prolonged Q-T interval on ECG, pruritus, seizure (high doses), skin rash, torsades de pointes, tremor (high doses), urticaria
Warnings/Precautions
Concerns related to adverse effects:
- Acute generalized exanthematous pustulosis: May rarely cause acute generalized exanthematous pustulosis (AGEP), a serious skin reaction involving fever, pustules and large areas of edematous erythema. Discontinue at first sign of skin rash, worsening of pre-existing skin reactions or any other sign of hypersensitivity; if signs or symptoms suggest AGEP, do not resume therapy.
- CNS depression: May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks that require mental alertness (eg, operating machinery, driving).
- QT prolongation/torsades de pointes: Has been reported, with the majority occurring in patients with other risk factors for QT prolongation/torsades de pointes (eg, preexisting cardiac disease, electrolyte imbalances, concomitant arrhythmogenic use). Use with caution in patients with risk factors for QT prolongation, congenital long QT syndrome, a family history of long QT syndrome, other conditions that predispose to QT prolongation and ventricular arrhythmia, as well as recent myocardial infarction, uncompensated heart failure, and bradyarrhythmias. Oral hydroxyzine is contraindicated in patients with a prolonged QT interval.
Disease-related concerns:
- Glaucoma: Use with caution in patients with narrow-angle glaucoma; condition may be exacerbated by cholinergic blockade. Screening is recommended.
- Prostatic hyperplasia/urinary stricture: Use with caution in patients with prostatic hyperplasia and/or urinary stricture.
- Respiratory disease: Use with caution in patients with asthma or chronic obstructive pulmonary disease (COPD).
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
Elderly: May cause over sedation in the elderly; initiate elderly patients on low does and monitor closely.
Dosage form specific issues:
- Benzyl alcohol and derivatives: Some dosage forms may contain benzyl alcohol and/or sodium benzoate/benzoic acid; benzoic acid (benzoate) is a metabolite of benzyl alcohol; large amounts of benzyl alcohol (≥99 mg/kg/day) have been associated with a potentially fatal toxicity ("gasping syndrome") in neonates; the "gasping syndrome" consists of metabolic acidosis, respiratory distress, gasping respirations, CNS dysfunction (including convulsions, intracranial hemorrhage), hypotension and cardiovascular collapse (AAP ["Inactive" 1997]; CDC 1982); some data suggest that benzoate displaces bilirubin from protein binding sites (Ahlfors 2001); avoid or use dosage forms containing benzyl alcohol and/or benzyl alcohol derivative with caution in neonates. See manufacturer's labeling.
- Propylene glycol: Some dosage forms may contain propylene glycol; large amounts are potentially toxic and have been associated with hyperosmolality, lactic acidosis, seizures, and respiratory depression; use caution (AAP 1997; Zar 2007). See manufacturer's labeling.
Other warnings/precautions:
- Appropriate administration: Parenteral: For IM use only. Severe injection-site reactions have been reported with IM administration (eg, extensive tissue damage, necrosis, gangrene) requiring surgical intervention (including debridement, skin grafting, and amputation). SubQ, IV, and intra-arterial routes of administration are contraindicated. Intravascular hemolysis, thrombosis, and digital gangrene have been reported with IV or intra-arterial administration (Baumgartner 1979); SubQ administration may result in significant tissue damage. If inadvertent IV administration results in extravasation, stop infusion immediately and disconnect (leave cannula/needle in place); gently aspirate extravasated solution (do NOT flush the line); remove needle/cannula; elevate extremity.
- Long-term use: The effectiveness of hydroxyzine for long-term use (>4 months) has not been assessed; periodically reassess use.
Monitoring Parameters
Relief of symptoms, mental status, blood pressure
Pregnancy
Pregnancy Considerations
Hydroxyzine crosses the placenta. Possible withdrawal symptoms have been observed in neonates following chronic maternal use of hydroxyzine during pregnancy (Prenner 1977; Serreau 2005).
Hydroxyzine is approved for pre- and postpartum adjunctive therapy to control emesis, reduce opioid dosage, and treat anxiety. However, use in early pregnancy is contraindicated by the manufacturer and other agents are recommended for the treatment of nausea and vomiting of pregnancy (ACOG 189 2018). Hydroxyzine may be used as an antipruritic if systemic therapy is needed (use caution late in pregnancy) (Murase 2014); although other agents may be preferred (Powell 2015; Zuberbier 2014). Antihistamines are not recommended for treatment of pruritus associated with intrahepatic cholestasis in pregnancy (Ambros-Rudolph 2011; Kremer 2014).
Patient Education
What is this drug used for?
- It is used to treat itching.
- It is used to treat anxiety.
- It is used to put you to sleep for surgery.
- It is used to treat mood problems.
- It is used to treat upset stomach and throwing up.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Dry mouth
- Fatigue
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Abnormal heartbeat
- Fast heartbeat
- Severe dizziness
- Passing out
- Abnormal movements
- Pinpoint red spots on skin
- Severe skin irritation
- Injection site burning
- Skin discoloration, pain, edema, or irritation
- Confusion
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.