Boxed Warning
Congestive heart failure:
Itraconazole can cause or exacerbate congestive heart failure (CHF). When itraconazole was administered intravenously (IV) to dogs and healthy human volunteers, negative inotropic effects were seen. Do not administer itraconazole for the treatment of onychomycosis in patients with evidence of ventricular dysfunction, such as CHF or a history of CHF. If signs or symptoms of CHF occur during administration of itraconazole oral solution or capsule (65 mg [Tolsura]), reassess continued itraconazole use. If signs or symptoms of CHF occur during administration of itraconazole capsules (100 mg [Sporanox]) or tablets, discontinue administration.
Drug interactions:
Coadministration of the following drugs is contraindicated with itraconazole: methadone, disopyramide, dofetilide, dronedarone, quinidine, isavuconazole, ergot alkaloids (eg, dihydroergotamine, ergometrine [ergonovine], ergotamine, methylergometrine [methylergonovine]), irinotecan, lurasidone, oral midazolam, pimozide, triazolam, felodipine, nisoldipine, ivabradine, ranolazine, eplerenone, cisapride, naloxegol, lomitapide, lovastatin, simvastatin, avanafil, and ticagrelor. In addition, coadministration with colchicine, fesoterodine, and solifenacin is contraindicated in patients with varying degrees of renal or hepatic impairment, and coadministration with eliglustat is contraindicated in patients who are poor or intermediate metabolizers of CYP2D6 and in patients taking strong or moderate CYP2D6 inhibitors. Coadministration with itraconazole can cause elevated plasma concentrations of these drugs and may increase or prolong both the pharmacologic effects and/or adverse reactions to these drugs. For example, increased plasma concentrations of some of these drugs can lead to QT prolongation and ventricular tachyarrhythmias including occurrences of torsades de pointes, a potentially fatal arrhythmia.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Capsule, Oral:
Sporanox: 100 mg [contains brilliant blue fcf (fd&c blue #1), corn starch, d&c red #22 (eosine), fd&c blue #2 (indigotine)]
Sporanox Pulsepak: 100 mg [contains brilliant blue fcf (fd&c blue #1), corn starch, d&c red #22 (eosine), fd&c blue #2 (indigotine)]
Tolsura: 65 mg
Generic: 100 mg
Solution, Oral:
Sporanox: 10 mg/mL (150 mL) [contains propylene glycol, saccharin sodium, sorbitol]
Generic: 10 mg/mL (150 mL)
Tablet, Oral:
Onmel: 200 mg [DSC]
Pharmacology
Mechanism of Action
Interferes with cytochrome P450 activity, decreasing ergosterol synthesis (principal sterol in fungal cell membrane) and inhibiting cell membrane formation
Pharmacokinetics/Pharmacodynamics
Absorption
Capsule (100 mg [Sporanox]), tablet, oral solution: Requires gastric acidity; capsule or tablet better absorbed with food, solution better absorbed on empty stomach
Capsule (65 mg [Tolsura]): Absorption increased with reduced gastric acidity and decreased with a high-fat meal
Distribution
Vd (average): >700 L; highly lipophilic and tissue concentrations are higher than plasma concentrations. The highest concentrations: adipose, omentum, endometrium, cervical and vaginal mucus, and skin/nails. Aqueous fluids (eg, CSF and urine) contain negligible amounts; distributes into bronchial exudate and sputum
Metabolism
Extensively hepatic via CYP3A4 into >30 metabolites including hydroxy-itraconazole (major metabolite); appears to have in vitro antifungal activity. Main metabolic pathway is oxidation; may undergo saturation metabolism with multiple dosing.
Excretion
Urine (<1% active drug, 35% as inactive metabolites); feces (54%; ~3% to 18% as unchanged drug)
Time to Peak
Plasma: Capsules/tablets: 2 to 5 hours; Oral solution: 2.5 hours
Half-Life Elimination
Children (6 months to 12 years): Oral solution: ~36 hours; Metabolite hydroxy-itraconazole: ~18 hours
Adults: Oral: Single dose: 16 to 28 hours, Multiple doses: 34 to 42 hours; Cirrhosis (single dose): 37 hours (range: 20 to 54 hours)
Protein Binding
Plasma: 99.8%; metabolite hydroxy-itraconazole: 99.6%
Use in Specific Populations
Special Populations: Renal Function Impairment
Bioavailability is slightly reduced.
Special Populations: Hepatic Function Impairment
Cmax was reduced by 47% and resulted in a twofold increase in half-life (capsules).
Use: Labeled Indications
Aspergillosis (capsules): Treatment of pulmonary and extrapulmonary aspergillosis in immunocompromised and nonimmunocompromised patients who are intolerant of or refractory to amphotericin B therapy. Note: IDSA Aspergillosis guidelines recommend amphotericin B formulations for invasive aspergillosis (initial or salvage) only when voriconazole is contraindicated or not tolerated (IDSA [Patterson 2016]).
Blastomycosis (capsules): Treatment of pulmonary and extrapulmonary blastomycosis in immunocompromised and nonimmunocompromised patients.
Histoplasmosis (capsules): Treatment of histoplasmosis, including chronic cavitary pulmonary disease and disseminated, nonmeningeal histoplasmosis in immunocompromised and nonimmunocompromised patients.
Onychomycosis:
Capsules (100 mg [Sporanox]): Treatment of onychomycosis of the toenail, with or without fingernail involvement, and onychomycosis of the fingernail caused by dermatophytes (tinea unguium) in nonimmunocompromised patients
Tablets: Treatment of onychomycosis of the toenail caused by Trichophyton rubrum or Trichophyton mentagrophytes in nonimmunocompromised patients
Oropharyngeal/Esophageal candidiasis (oral solution): Treatment of oropharyngeal and esophageal candidiasis
Canadian labeling: Oral capsules: Additional indications (not in US labeling):
Candidiasis, oral and/or esophageal: Treatment of oral and/or esophageal candidiasis in immunocompromised and immunocompetent patients
Chromomycosis: Treatment of chromomycosis in immunocompromised and immunocompetent patients
Dermatomycoses: Treatment of dermatomycoses due to tinea pedis, tinea cruris, tinea corporis, and of pityriasis versicolor in patients for whom oral therapy is appropriate
Onychomycosis: Treatment of onychomycosis in immunocompromised and immunocompetent patients
Paracoccidioidomycosis: Treatment of paracoccidioidomycosis in immunocompromised and immunocompetent patients
Sporotrichosis: Treatment of cutaneous and lymphatic sporotrichosis in immunocompromised and immunocompetent patients
Use: Off Label
Candidiasis, vulvovaginal in HIV-infected patientsyes
Based on the US Department of Health and Human Services (HHS) Guidelines for Prevention and Treatment of Opportunistic Infections in HIV-Infected Adults and Adolescents, itraconazole oral solution is an effective and recommended alternative agent in the management of vulvovaginal candidiasis in HIV-infected patients.
Coccidioidal meningitis in HIV-infected patientsyes
Based on the US Department of Health and Human Services (HHS) Guidelines for Prevention and Treatment of Opportunistic Infections in HIV-Infected Adults and Adolescents, itraconazole is an effective and recommended alternative agent in the treatment of and as chronic suppressive therapy of coccidioidal meningitis in HIV-infected patients.
Coccidioidal pneumonia in HIV-infected patientsyes
Based on the US Department of Health and Human Services (HHS) Guidelines for Prevention and Treatment of Opportunistic Infections in HIV-Infected Adults and Adolescents, itraconazole is an effective and recommended agent in the treatment of coccidioidal pneumonia (focal pneumonia) in HIV-infected patients.
Coccidioidomycosis (non-HIV infected)yes
Based on the Infectious Diseases Society of America (IDSA) guidelines for the treatment of coccidioidomycosis, itraconazole is an effective and recommended agent for the treatment of coccidioidomycosis, including coccidioidal meningitis and certain types of pulmonary and extrapulmonary infections.
Cryptococcosis in HIV-infected patientsyes
Based on the HHS Guidelines for the Prevention and Treatment of Opportunistic Infections in HIV-Infected Adults and Adolescents, itraconazole is an effective and recommended alternative agent in the treatment (consolidation therapy) of cryptococcal meningitis in HIV-infected patients.
Microsporidiosis, disseminated in HIV-infected patientsyes
Based on the US Department of Health and Human Services (HHS) Guidelines for Prevention and Treatment of Opportunistic Infections in HIV-Infected Adults and Adolescents, itraconazole is an effective and recommended agent in the management of disseminated microsporidiosis caused by Trachipleistophora or Anncaliia in HIV-infected patients.
Penicilliosis in HIV-infected patientsyes
Based on the US Department of Health and Human Services (HHS) Guidelines for Prevention and Treatment of Opportunistic Infections in HIV-Infected Adults and Adolescents, itraconazole is an effective and recommended agent in the treatment or primary prophylaxis of penicilliosis in HIV-infected patients.
Contraindications
Hypersensitivity to itraconazole or any component of the formulation; concurrent administration with avanafil, cisapride, disopyramide, dofetilide, dronedarone, eplerenone, ergot derivatives, felodipine, irinotecan, isavuconazole, ivabradine, lomitapide, lovastatin, lurasidone, methadone, midazolam (oral), naloxegol, nisoldipine, pimozide, quinidine, ranolazine, simvastatin, ticagrelor, or triazolam; concurrent administration with colchicine, fesoterodine, or solifenacin in patients with varying degrees of renal or hepatic impairment; coadministration with eliglustat in patients who are poor or intermediate metabolizers of CYP2D6 and in patients taking strong or moderate CYP2D6 inhibitors; treatment of onychomycosis (or other non-life-threatening indications) in patients with evidence of ventricular dysfunction, such as congestive heart failure (CHF) or a history of CHF; treatment of onychomycosis in women who are pregnant or contemplating pregnancy
Canadian labeling: Additional contraindications (not in US labeling): Concurrent administration with domperidone, eletriptan, fesoterodine in patients with moderate to severe renal or hepatic impairment, or solifenacin in patients with severe renal impairment or moderate to severe hepatic impairment (capsule, oral solution); Concurrent administration with the following drugs (none of which are available in Canada): Astemizole, bepridil, halofantrine, ivabradine, lercanidipine, levacetylmethadol, mizolastine, telithromycin (in patients with severe renal or hepatic impairment), sertindole, terfenadine (capsule, oral solution); treatment of dermatomycosis (tinea pedis, tinea cruris, tinea corporis, pityriasis versicolor) in women who are pregnant or intend to become pregnant (capsule)
Dosage and Administration
Dosing: Adult
Note: Onmel has been discontinued in the US for more than 1 year.
Note: Formulations are not interchangeable. Generally, oral solution is the preferred formulation because of improved absorption (IDSA [Kauffman 2007]; HHS [OI adult 2017]).
Aspergillosis, invasive (salvage therapy) (alternative agent):
Oral solution: 200 mg twice daily; duration of therapy is a minimum of 6 to 12 weeks, although duration is highly dependent on degree/duration of immunosuppression, disease site, and evidence of disease improvement (IDSA [Patterson 2016])
Oral capsule (65 mg [Tolsura]): 130 mg once or twice daily; for life threatening infections, administer a loading dose of 130 mg 3 times daily for the first 3 days of therapy; treatment should be continued for ≥3 months and until clinical and laboratory resolution.
Blastomycosis:
Oral solution or capsule (100 mg [Sporanox]): 200 mg 3 times daily for 3 days, then 200 mg twice daily for 6 to 12 months; in moderately severe to severe infection, therapy should be initiated with ~2 weeks of amphotericin B (Chapman 2008).
Oral capsule (65 mg [Tolsura]): 130 mg once daily; if no improvement or if there is evidence of progressive fungal infection, increase dose in 65 mg increments to a maximum of 260 mg/day (doses >130 mg/day should be given in 2 divided doses). For life threatening infections, administer a loading dose of 130 mg 3 times daily for the first 3 days of therapy; treatment should be continued for ≥3 months and until clinical and laboratory resolution.
Candidiasis: Oral:
Esophageal:
Oral solution:
Fluconazole-refractory disease: 200 mg once daily for 14 to 21 days (IDSA [Pappas 2016])
HIV-infected patients: 200 mg once daily for 14 to 21 days (HHS [OI adult 2017])
US labeling: Dosing in the prescribing information may not reflect current clinical practice. Oral solution: 100 to 200 mg once daily
Canadian labeling:
Oral solution: 100 to 200 mg once daily for a minimum of 3 weeks; continue dosing for 2 weeks after resolution of symptoms
Oral capsule (100 mg [Sporanox]): 100 mg once daily for 4 weeks
Oropharyngeal:
Oral solution:
Fluconazole-refractory disease: 200 mg once daily for up to 28 days (IDSA [Pappas 2016])
HIV-infected patients (alternative agent): Oral solution: 200 mg once daily for 7 to 14 days (HHS [OI adult 2017])
US labeling: Dosing in the prescribing information may not reflect current clinical practice. Oral solution: 200 mg once daily; in patients unresponsive or refractory to fluconazole: 100 mg twice daily
Canadian labeling:
Oral solution: 200 mg once daily or in divided doses daily for 1 to 2 weeks
Oral capsule (100 mg [Sporanox]): 100 mg once daily for 2 weeks
Vulvovaginal (uncomplicated) in HIV-infected patients (alternative to preferred therapy) (off-label use): Oral solution: 200 mg once daily for 3 to 7 days (HHS [OI adult 2017])
Chromomycosis: Canadian labeling (not in US labeling): Oral capsule (100 mg [Sporanox]): 200 mg once daily for 6 months
Coccidioidomycosis, extrapulmonary (non-HIV infected) (off-label use): Oral:
Soft tissue infection (not associated with bone infection): 200 mg twice daily for at least 6 to 12 months (IDSA [Galgiani 2016])
Bone and/or joint infection: 200 mg twice daily for 3 years to lifetime, depending on severity and host immunocompetence. Note: Amphotericin B may be used initially in severe cases and then switched to itraconazole (IDSA [Galgiani 2016])
Coccidioidal pneumonia (off-label use): Oral:
Non-HIV infected (symptomatic, chronic cavitary): Oral: 200 mg twice daily for at least 12 months (IDSA [Galgiani 2016])
HIV-infected patients (focal pneumonia): 200 mg twice daily (HHS [OI adult 2017])
Coccidioidal meningitis (off-label use):
Non-HIV infected: Oral: 200 mg 2 to 4 times daily; close monitoring required to assure adequate absorption (IDSA [Galgiani 2016])
HIV-infected patients (HHS [OI adult 2017]) (alternative agent): Oral:
Treatment: 200 mg 3 times daily for 3 days, then 200 mg twice daily, followed by chronic suppressive therapy
Chronic suppressive therapy: 200 mg twice daily continued indefinitely, even with increase in CD4 count on ART
Cryptococcosis in HIV-infected patients (off-label use) (alternative agent): Oral: Treatment, consolidation therapy: 200 mg twice daily for ≥8 weeks (HHS [OI adult 2017])
Histoplasmosis:
Treatment:
Oral solution or capsule (100 mg [Sporanox]): 200 mg 3 times daily for 3 days, then 200 mg twice daily (or once daily in mild-moderate disease) for 6 to 12 weeks in mild-moderate disease or ≥12 months in progressive disseminated or chronic cavitary pulmonary histoplasmosis; in moderately severe to severe infection, therapy should be initiated with ~2 weeks of a lipid formation of amphotericin B (Wheat 2007).
Oral capsule (65 mg [Tolsura]): 130 mg once daily; if no improvement or if there is evidence of progressive fungal infection, increase dose in 65 mg increments to a maximum of 260 mg/day (doses >130 mg/day should be given in 2 divided doses). For life threatening infections, administer a loading dose of 130 mg 3 times daily for the first 3 days of therapy; treatment should be continued for ≥3 months and until clinical and laboratory resolution.
HIV-infected patients (oral solution or capsule [100 mg (Sporanox)]):
Mild disseminated disease: Induction and maintenance therapy: 200 mg 3 times daily for 3 days, then 200 mg twice daily for ≥12 months (HHS [OI adult 2017])
Moderate to severe disseminated disease: Maintenance therapy (following at least 2 weeks of induction therapy with an appropriate agent): 200 mg 3 times daily for 3 days, then 200 mg twice daily for ≥12 months (HHS [OI adult 2017])
Meningitis: Maintenance therapy (following 4 to 6 weeks of induction therapy with an appropriate agent): 200 mg 2 to 3 times daily for ≥12 months and until resolution of abnormal CSF findings (HHS [OI adult 2017])
Prophylaxis (off-label use):
Oral solution or capsule (100 mg [Sporanox]):
Primary prophylaxis in HIV-infected patients: 200 mg once daily; primary prophylaxis is indicated when CD4 count <150 cells/mm3 and at increased risk of exposure (HHS [OI adult 2017])
Long-term suppression therapy (secondary prophylaxis) in HIV-infected patients: 200 mg once daily; long-term suppressive therapy is indicated in patients who relapse despite appropriate therapy or in patients with CNS or severe disseminated infection (HHS [OI adult 2017])
Microsporidiosis, disseminated (caused by Trachipleistophora or Anncaliia) in HIV-infected patients (off-label use): Oral: 400 mg once daily in combination with albendazole (HHS [OI adult 2017])
Onychomycosis (fingernail involvement only): Oral capsule (100 mg [Sporanox]): 200 mg twice daily for 1 week; repeat 1-week course after 3-week off-time
Onychomycosis (toenails due to Trichophyton rubrum or T. mentagrophytes): Oral tablet: 200 mg once daily for 12 consecutive weeks.
Onychomycosis (toenails with or without fingernail involvement): Oral capsule (100 mg [Sporanox]): 200 mg once daily for 12 consecutive weeks
Canadian labeling (not in US labeling): Oral capsule (100 mg [Sporanox]): "Pulse-dosing": 200 mg twice daily for 1 week; repeat 1-week course twice with 3-week off-time between each course
Paracoccidioidomycosis: Canadian labeling (not in US labeling): Oral capsule (100 mg [Sporanox]): 100 mg once daily for 6 months
Penicilliosis in HIV-infected patients (off-label use) (HHS [OI adult 2017]): Oral:
Primary prophylaxis: 200 mg once daily for patients with a CD4 count <100 cells/mm3 who spend extensive time in northern Thailand, Vietnam, and Southern China, especially rural areas
Treatment: 200 mg twice daily for 8 weeks (mild disease) or 10 weeks (severe infections), then continue with maintenance therapy. In severely ill patients, initiate therapy with 2 weeks of liposomal amphotericin B.
Chronic maintenance (secondary prophylaxis): 200 mg once daily until CD4 count >100 cells/mm3 for ≥6 months in response to ART
Pityriasis versicolor: Canadian labeling (not in US labeling): Oral capsule (100 mg [Sporanox]): 100 mg twice daily or 200 mg once daily for 5 to 7 days
Sporotrichosis: Oral:
Cutaneous: Canadian labeling (not in US labeling): Oral capsule (100 mg [Sporanox]): 100 to 200 mg once daily for 3 to 6 months (localized lesions); 200 mg twice daily for 3 to 6 months (extensive lesions)
Lymphocutaneous: 200 mg daily for 3 to 6 months (Kauffman 2007)
Canadian labeling (not in US labeling): Oral capsule (100 mg [Sporanox]): 100 to 200 mg once daily for 3 to 6 months (localized lesions); 200 mg twice daily for 3 to 6 months (extensive lesions)
Osteoarticular and pulmonary: 200 mg twice daily for ≥1 years (may use amphotericin B initially for stabilization) (Kauffman 2007)
Tinea corporis or tinea cruris: Canadian labeling (not in US labeling): Oral capsule (100 mg [Sporanox]): 100 mg once daily for 14 consecutive days or 200 mg once daily for 7 consecutive days. Note: Equivalency between regimens not established.
Tinea pedis: Canadian labeling (not in US labeling): Oral capsule (100 mg [Sporanox]): 100 mg once daily for 28 consecutive days or 200 mg twice daily for 7 consecutive days. Note: Equivalency between regimens not established. Patients with chronic resistant infection may benefit from lower dose and extended treatment time (100 mg once daily for 28 days).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Formulations are not interchangeable. Generally, oral solution is the preferred formulation because of improved absorption (Bradley 2018; IDSA [Kauffman 2007]); HHS [OI adult 2018]). Oral absorption varies between patients and as a result, monitoring of serum concentrations is suggested to ensure adequate and nontoxic levels are achieved (Bradley 2018). Onmel (tablets) has been discontinued in the US for >1 year.
General dosing, susceptible infection: Limited data available: Infants, Children, and Adolescents: Oral: 5 mg/kg/dose every 12 hours for treatment; usual maximum daily dose: 200 mg/day; some infections may require up to 400 mg/day (Bradley 2018; Red Book [AAP 2018])
Blastomycosis, non-CNS infections: Limited data available: Infants, Children, and Adolescents: Oral solution: 5 mg/kg/dose twice daily; maximum dose: 200 mg/dose; duration determined by severity and response; usual duration for mild to moderate disease is 6 to 12 months; for moderately severe to severe disease a total duration of 12 months including 1 to 2 weeks of amphotericin B (Bradley 2018; IDSA [Chapman 2008]; Red Book [AAP 2018])
Candidiasis (HIV-exposed/-positive patients) (HHS [OI adult 2018]; HHS [OI pediatric 2016]): Limited data available:
Oropharyngeal, treatment:
Infants and Children: Fluconazole-refractory: Oral solution: 2.5 mg/kg/dose twice daily for 7 to 14 days; maximum daily dose range: 200 to 400 mg/day
Adolescents: Oral solution: 200 mg once daily for 7 to 14 days
Esophageal, treatment:
Infants and Children: Fluconazole-refractory: Oral solution: 2.5 mg/kg/dose twice daily for at least 21 days and at least 2 weeks following resolution of symptoms.
Adolescents: Oral solution: 200 mg once daily for 14 to 21 days
Vulvovaginal, uncomplicated: Adolescents: Oral solution: 200 mg once daily for 3 to 7 days
Secondary prophylaxis: Infants and Children: Oral solution: 2.5 mg/kg/dose twice daily
Coccidioidomycosis: Limited data available:
Treatment:
Bone and/or joint infection:
Infants and Children: Independent of HIV status: Oral solution: 5 mg/kg/dose twice daily for ≥12 months (Bradley 2018; HHS [OI pediatric 2016]; Homans 2010)
Adolescents: HIV-exposed/-positive: Oral: 200 mg twice daily (HHS [OI adult 2018])
Meningitis: HIV-exposed/-positive (HHS [OI adult 2018]): Adolescents:
Initial: Oral: 200 mg 3 times daily for 3 days
Maintenance: 200 mg twice daily
Pneumonia, focal (mild disease): HIV-exposed/-positive:
Infants and Children: Oral:
Initial: 2 to 5 mg/kg/dose 3 times daily for 3 days; maximum dose: 200 mg/dose
Maintenance: 2 to 5 mg/kg/dose twice daily; maximum dose: 200 mg/dose; duration of treatment determined by rate of clinical response (HHS [OI pediatric 2016])
Adolescents: Oral: 200 mg twice daily (HHS [OI adult 2018])
Secondary prophylaxis/Chronic suppressive therapy: HIV-exposed/-positive:
Infants and Children: Oral: 2 to 5 mg/kg/dose twice daily; maximum dose: 200 mg/dose (HHS [OI pediatric 2016])
Adolescents: Oral: 200 mg twice daily (HHS [OI adult 2018])
Cryptococcal meningitis (HIV-exposed/-positive) (HHS [OI adult 2018]; HHS [OI pediatric 2016]): Limited data available:
Consolidation treatment:
Infants and Children: Oral solution (preferred):
Initial load: 2.5 to 5 mg/kg/dose 3 times daily for 3 days; maximum dose: 200 mg/dose
Maintenance dose: 5 to 10 mg/kg/day divided once or twice daily for a minimum of 8 weeks; maximum daily dose: 400 mg/day
Adolescents: Oral: 200 mg twice daily for a minimum of 8 weeks
Secondary prophylaxis/Relapse prevention: Infants and Children: Oral solution: 5 mg/kg/dose once daily; maximum daily dose: 200 mg/day
Histoplasmosis: Limited data available:
Treatment:
Pulmonary, acute primary disease:
HIV-exposed/-positive (HHS [OI pediatric 2016]): Infants and Children: Oral solution (preferred):
Initial load: 2 to 5 mg/kg/dose 3 times daily for 3 days; maximum dose: 200 mg/dose
Maintenance dose: 2 to 5 mg/kg/dose twice daily for 12 months; maximum dose: 200 mg/dose. Treatment duration of 12 weeks may be adequate in children with functional cellular immunity (CD4 percentage >20% or if age ≥6 years, CD4 cell count >300 cells/mm3) if clinically improved and urine antigen concentrations decreased.
Non-HIV-exposed/-positive: Infants, Children, and Adolescents: Oral solution (preferred): 2.5 to 5 mg/kg/dose twice daily for 6 to 12 weeks; maximum dose: 200 mg/dose (IDSA [Wheat 2007])
Disseminated disease, mild to moderate:
HIV-exposed/-positive (HHS [OI adult 2018]; HHS [OI pediatric 2016]):
Infants and Children: Oral solution (preferred):
Initial load: 2 to 5 mg/kg/dose 3 times daily for 3 days; maximum dose: 200 mg/dose
Maintenance dose: 2 to 5 mg/kg/dose twice daily for 12 months; maximum dose: 200 mg/dose
Adolescents: Oral solution (preferred):
Initial load: 200 mg 3 times daily for 3 days
Maintenance dose: 200 mg twice daily for at least 12 months
Non-HIV-exposed/-positive: Infants, Children, and Adolescents: Oral solution (preferred): 2.5 to 5 mg/kg/dose twice daily for 3 to 12 months (IDSA [Wheat 2007]; Red Book [AAP 2018])
Disseminated disease, moderately severe to severe: Consolidation treatment following appropriate induction treatment:
HIV-exposed/positive (HHS [OI adult 2018]; HHS [OI pediatric 2016]):
Infants and Children: Oral solution:
Initial load: 2 to 5 mg/kg/dose 3 times daily for 3 days; maximum dose: 200 mg/dose
Maintenance dose: 2 to 5 mg/kg/dose twice daily for 12 months; maximum dose: 200 mg/dose
Adolescents: Oral solution (preferred):
Initial load: 200 mg 3 times daily for 3 days
Maintenance dose: 200 mg twice daily for ≥12 months
Non HIV-exposed/positive, step-down: Infants, Children, and Adolescents: Oral solution (preferred): 2.5 to 5 mg/kg/dose twice daily for 3 to 12 months based on severity of disease; maximum dose: 200 mg/dose (IDSA [Wheat 2007]; Red Book [AAP 2018])
Prophylaxis:
Primary: HIV-exposed/-positive: Adolescents: Oral: 200 mg once daily (HHS [OI adult 2018])
Secondary prophylaxis/chronic suppressive therapy:
HIV-exposed/-positive:
Infants and Children: Oral solution: 5 to 10 mg/kg/dose once daily; maximum dose: 200 mg/dose (HHS [OI pediatric 2016])
Adolescents: Oral: 200 mg once daily (HHS [OI adult 2018])
Non HIV-exposed/positive: Infants, Children, and Adolescents: Oral: 5 mg/kg/dose once daily; maximum dose: 200 mg/dose (IDSA [Wheat 2007])
Microsporidiosis, disseminated disease caused by Trachipleistophora or Anncaliia, treatment (HIV-exposed/-positive): Limited data available: Adolescents: Oral: 400 mg once daily in conjunction with albendazole (HHS [OI adult 2018])
Penicilliosis (HIV-exposed/-positive) (HHS [OI adult 2018]): Limited data available: Adolescents:
Primary prophylaxis: Oral: 200 mg once daily for patients with a CD4 count <100 cells/mm3 who spend extensive time in northern Thailand, Vietnam, and Southern China, especially rural areas
Acute infection (severely ill), treatment: Oral: 200 mg twice daily for 10 weeks; initiate after completion of 2 weeks induction therapy with amphotericin B
Mild disease, treatment: Oral: 200 mg twice daily for 8 weeks
Secondary prophylaxis/chronic maintenance therapy: Oral: 200 mg once daily
Sporotrichosis (IDSA [Kauffman 2007]; Red Book [AAP 2018]): Limited data available: Infants, Children, and Adolescents:
Lymphocutaneous or localized cutaneous: Oral solution (preferred): 3 to 5 mg/kg/dose twice daily; continue 2 to 4 weeks after all lesions have resolved, usual total duration: 3 to 6 months; maximum dose: 200 mg/dose
Step down therapy, visceral or disseminated (after initial treatment and clinical response with amphotericin B): Oral: 3 to 5 mg/kg/dose twice daily; continue for at least 12 months; maximum dose: 200 mg/dose
Tinea capitis, Microsporum canis and trichophyton sp: Limited data available: Infants, Children, and Adolescents: Oral: 5 mg/kg/dose once daily; maximum dose: 100 mg/dose; duration of therapy dependent on organism: Microsporum sp: 4 to 8 weeks; trichophyton sp: 2 to 3 weeks; up to 12 weeks of treatment may be required (Binder 2009; Fuller 2014; Ginter-Hanselmayer 2004; Gupta 2001a; Gupta 2001b). Alternatively, a pulse regimen may be used: 1 week treatment pulses with at least 2 weeks off between pulses (Gupta 1997; Gupta 2001b; Kakourou 2010)
Extemporaneously Prepared
Note: Commercial oral solution is available (10 mg/mL)
A 20 mg/mL oral suspension may be made with capsules. Empty the contents of forty 100 mg capsules and add 15 mL of Alcohol, USP. Let stand for 5 minutes. Crush the beads in a mortar and reduce to a fine powder. Mix while adding a 1:1 mixture of Ora-Sweet and Ora-Plus in incremental proportions to almost 200 mL; transfer to a calibrated bottle, rinse mortar with vehicle, and add quantity of vehicle sufficient to make 200 mL. Label "shake well" and "refrigerate". Stable for 56 days refrigerated.
Nahata MC, Pai VB, and Hipple TF, Pediatric Drug Formulations, 5th ed, Cincinnati, OH: Harvey Whitney Books Co, 2004.
Administration
Oral: Formulations are not interchangeable; generally, oral solution is the preferred formulation because of improved absorption (IDSA [Kauffman 2007]; HHS [OI adult 2017; OI pediatric 2013]). Administer capsule and tablet with a full meal. Oral solution should be taken on an empty stomach; when treating oropharyngeal and esophageal candidiasis, solution should be swished vigorously in mouth (10 mL at a time), then swallowed. Swallow capsule whole; do not crush, chew, or break.
Dietary Considerations
Capsule (100 mg [Sporanox] and 65 mg [Tolsura]), tablet: Take with food.
Solution: Take without food, if possible.
Storage
Capsule: Store at room temperature of 15°C to 25°C (59°F to 77°F). Protect from light and moisture.
Oral solution: Store at ≤25°C (77°F); do not freeze.
Tablet: Store at room temperature 15°C to 25°C (59°F to 77°F); excursions permitted between 15°C and 30°C (59°F and 86°F). Protect from light and moisture.
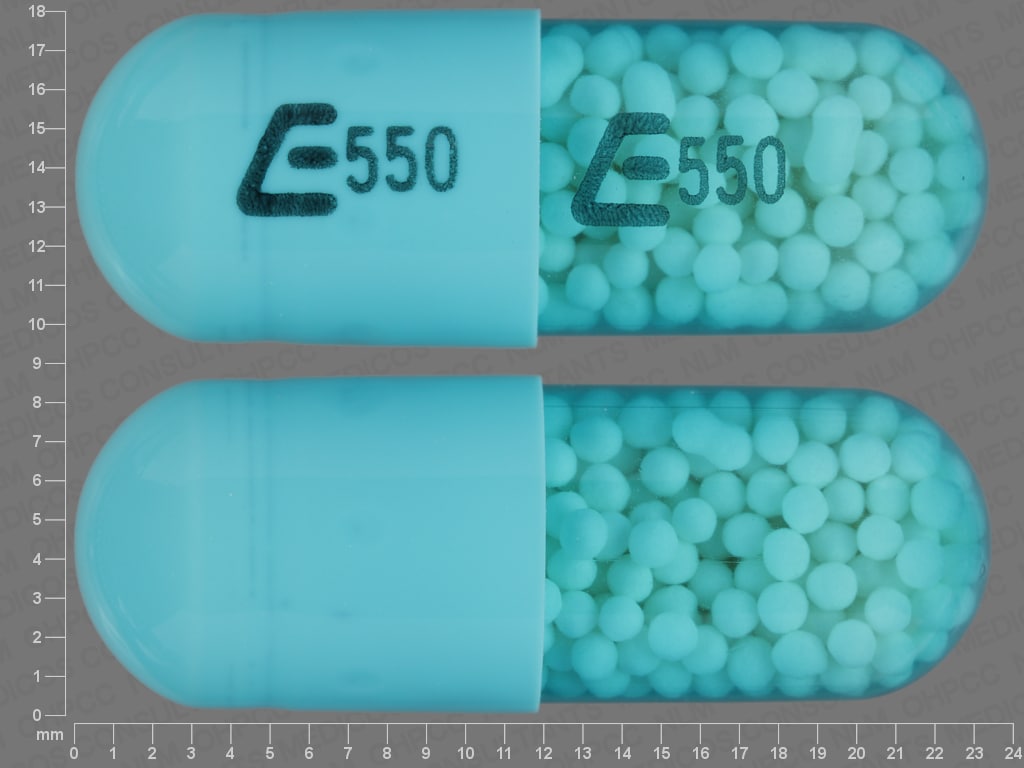
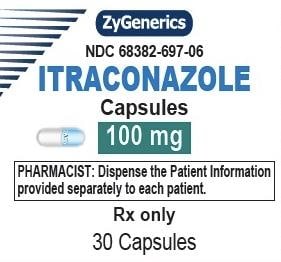
Itraconazole Images
Drug Interactions
Abemaciclib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Abemaciclib. Management: In patients taking abemaciclib at a dose of 200 mg or 150 mg twice daily, reduce the dose to 100 mg twice daily when combined with strong CYP3A4 inhibitors. In patients taking abemaciclib 100 mg twice daily, decrease the dose to 50 mg twice daily. Consider therapy modification
Acalabrutinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Acalabrutinib. Avoid combination
Ado-Trastuzumab Emtansine: CYP3A4 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of Ado-Trastuzumab Emtansine. Specifically, strong CYP3A4 inhibitors may increase concentrations of the cytotoxic DM1 component. Avoid combination
Afatinib: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Afatinib. Management: Reduce afatinib by 10 mg if not tolerated. Some non-US labeling recommends avoiding combination if possible. If used, administer the P-gp inhibitor simultaneously with or after the dose of afatinib. Consider therapy modification
Alfuzosin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Alfuzosin. Avoid combination
Aliskiren: Itraconazole may increase the serum concentration of Aliskiren. Avoid combination
Alitretinoin (Systemic): CYP3A4 Inhibitors (Strong) may increase the serum concentration of Alitretinoin (Systemic). Management: Consider reducing the alitretinoin dose to 10 mg when used together with strong CYP3A4 inhibitors. Monitor for increased alitretinoin effects/toxicities if combined with a strong CYP3A4 inhibitor. Consider therapy modification
Almotriptan: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Almotriptan. Management: Limit initial almotriptan adult dose to 6.25 mg and maximum adult dose to 12.5 mg/24-hrs when used with a strong CYP3A4 inhibitor. Avoid concurrent use in patients with impaired hepatic or renal function. Consider therapy modification
Alosetron: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Alosetron. Monitor therapy
ALPRAZolam: Itraconazole may increase the serum concentration of ALPRAZolam. Avoid combination
Amphotericin B: Antifungal Agents (Azole Derivatives, Systemic) may diminish the therapeutic effect of Amphotericin B. Monitor therapy
Antacids: May decrease the serum concentration of Itraconazole. Antacids may increase the serum concentration of Itraconazole. Management: Administer Sporanox brand itraconazole at least 2 hours before or 2 hours after administration of any antacids. Exposure to Tolsura brand itraconazole may be increased by antacids; consider itraconazole dose reduction. Consider therapy modification
Apixaban: Inhibitors of CYP3A4 (Strong) and P-glycoprotein may increase the serum concentration of Apixaban. Management: US labeling recommends a 50% apixaban dose reduction in patients who would otherwise receive 5 or 10 mg twice daily, and avoiding in patients who would otherwise receive 2.5 mg twice daily. Canadian labeling lists any combined use as contraindicated. Consider therapy modification
Aprepitant: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Aprepitant. Avoid combination
ARIPiprazole: CYP3A4 Inhibitors (Strong) may increase the serum concentration of ARIPiprazole. Management: See full interaction monograph for details. Consider therapy modification
ARIPiprazole Lauroxil: CYP3A4 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of ARIPiprazole Lauroxil. Management: Please refer to the full interaction monograph for details concerning the recommended dose adjustments. Consider therapy modification
Astemizole: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Astemizole. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Avoid combination
Asunaprevir: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Asunaprevir. Avoid combination
AtorvaSTATin: Itraconazole may increase the serum concentration of AtorvaSTATin. Management: Limit atorvastatin to a maximum adult dose of 20 mg/day in patients receiving itraconazole. Assess clinical response to ensure that the lowest necessary dose of atorvastatin is used. Consider use of fluva-, rosuva-, pitava-, or pravastatin when possible. Consider therapy modification
Avanafil: Itraconazole may increase the serum concentration of Avanafil. Avoid combination
Avapritinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Avapritinib. Avoid combination
Axitinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Axitinib. Management: Avoid concurrent use of axitinib with any strong CYP3A inhibitor whenever possible. If a strong CYP3A inhibitor must be used with axitinib, a 50% axitinib dose reduction is recommended. Consider therapy modification
Barnidipine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Barnidipine. Avoid combination
Bedaquiline: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Bedaquiline. Management: Limit duration of concurrent use of bedaquiline with CYP3A4 inhibitors to no more than 14 days, unless the benefit of continued use outweighs the possible risks. Monitor for toxic effects of bedaquiline. Exceptions discussed in separate monographs. Consider therapy modification
Benperidol: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Benperidol. Monitor therapy
Benzhydrocodone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Benzhydrocodone. Specifically, the concentration of hydrocodone may be increased. Monitor therapy
Betamethasone (Ophthalmic): CYP3A4 Inhibitors (Strong) may increase the serum concentration of Betamethasone (Ophthalmic). Monitor therapy
Betrixaban: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Betrixaban. Management: Decrease the adult betrixaban dose to an initial single dose of 80 mg followed by 40 mg once daily if combined with a P-glycoprotein inhibitor. Consider therapy modification
Bictegravir: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Bictegravir. Monitor therapy
Bilastine: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Bilastine. Management: Consider alternatives when possible; bilastine should be avoided in patients with moderate to severe renal insufficiency who are receiving p-glycoprotein inhibitors. Consider therapy modification
Blonanserin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Blonanserin. Avoid combination
Bortezomib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Bortezomib. Monitor therapy
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Bosentan: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Bosentan. Management: Concomitant use of both a CYP2C9 inhibitor and a CYP3A inhibitor or a single agent that inhibits both enzymes with bosentan is likely to cause a large increase in serum concentrations of bosentan and is not recommended. See monograph for details. Monitor therapy
Bosutinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Bosutinib. Avoid combination
Brentuximab Vedotin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Brentuximab Vedotin. Specifically, concentrations of the active monomethyl auristatin E (MMAE) component may be increased. Monitor therapy
Brentuximab Vedotin: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Brentuximab Vedotin. Specifically, concentrations of the active monomethyl auristatin E (MMAE) component may be increased. Monitor therapy
Brexpiprazole: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Brexpiprazole. Management: Reduce brexpiprazole dose 50% with strong CYP3A4 inhibitors; reduce to 25% of usual if used with both a moderate CYP3A4 inhibitor and a CYP2D6 inhibitor in patients not being treated for MDD, or strong CYP3A4 inhibitor used in a CYP2D6 poor metabolizer. Consider therapy modification
Brigatinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Brigatinib. Management: Avoid concurrent use of brigatinib with strong CYP3A4 inhibitors when possible. If combination cannot be avoided, reduce the brigatinib dose by approximately 50%, rounding to the nearest tablet strength (ie, from 180 mg to 90 mg, or from 90 mg to 60 mg). Consider therapy modification
Brinzolamide: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Brinzolamide. Monitor therapy
Bromocriptine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Bromocriptine. Avoid combination
Bromperidol: Itraconazole may increase the serum concentration of Bromperidol. Monitor therapy
Budesonide (Nasal): CYP3A4 Inhibitors (Strong) may increase the serum concentration of Budesonide (Nasal). Monitor therapy
Budesonide (Oral Inhalation): CYP3A4 Inhibitors (Strong) may increase the serum concentration of Budesonide (Oral Inhalation). Monitor therapy
Budesonide (Systemic): CYP3A4 Inhibitors (Strong) may increase the serum concentration of Budesonide (Systemic). Avoid combination
Budesonide (Topical): CYP3A4 Inhibitors (Strong) may increase the serum concentration of Budesonide (Topical). Management: Per US prescribing information, avoid this combination. Canadian product labeling does not recommend strict avoidance. If combined, monitor for excessive glucocorticoid effects as budesonide exposure may be increased. Consider therapy modification
Buprenorphine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Buprenorphine. Monitor therapy
BusPIRone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of BusPIRone. Management: Limit the buspirone dose to 2.5 mg daily and monitor patients for increased buspirone effects/toxicities if combined with strong CYP3A4 inhibitors. Consider therapy modification
Busulfan: Antifungal Agents (Azole Derivatives, Systemic) may increase the serum concentration of Busulfan. Isavuconazonium considerations are addressed in separate monographs. Monitor therapy
Cabazitaxel: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Cabazitaxel. Management: Concurrent use of cabazitaxel with strong inhibitors of CYP3A4 should be avoided when possible. If such a combination must be used, consider a 25% reduction in the cabazitaxel dose. Consider therapy modification
Cabozantinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Cabozantinib. Management: Avoid use of a strong CYP3A4 inhibitor with cabozantinib if possible. If combined, cabozantinib dose adjustments are recommended and vary based on the cabozantinib product used and the indication for use. See monograph for details. Consider therapy modification
Calcifediol: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Calcifediol. Monitor therapy
Calcium Channel Blockers: Antifungal Agents (Azole Derivatives, Systemic) may enhance the adverse/toxic effect of Calcium Channel Blockers. Specifically, itraconazole may enhance the negative inotropic effects of verapamil or diltiazem. Antifungal Agents (Azole Derivatives, Systemic) may decrease the metabolism of Calcium Channel Blockers. Fluconazole and isavuconazonium likely exert weaker effects than other azoles and are addressed in separate monographs. Management: Concurrent use of felodipine or nisoldipine with itraconazole is specifically contraindicated. Frequent monitoring is warranted with any such combination; calcium channel blocker dose reductions may be required. Exceptions: Clevidipine. Consider therapy modification
Cannabidiol: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Cannabidiol. Monitor therapy
Cannabis: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Cannabis. More specifically, tetrahydrocannabinol and cannabidiol serum concentrations may be increased. Monitor therapy
Cardiac Glycosides: Itraconazole may increase the serum concentration of Cardiac Glycosides. Management: Consider preemptive cardiac glycoside dose adjustments with initiation / changes / discontinuation of itraconazole. Consider therapy modification
Cariprazine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Cariprazine. Management: Cariprazine dose reductions of 50% are required; specific recommended management varies slightly for those stable on cariprazine versus those just starting cariprazine. See prescribing information or full interaction monograph for details. Consider therapy modification
Celiprolol: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Celiprolol. Monitor therapy
Ceritinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Ceritinib. Management: If such combinations cannot be avoided, the ceritinib dose should be reduced by approximately one-third (to the nearest 150 mg). Resume the prior ceritinib dose after cessation of the strong CYP3A4 inhibitor. Exceptions discussed in separate monographs. Consider therapy modification
Cilostazol: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Cilostazol. Management: Consider reducing the cilostazol dose to 50 mg twice daily in adult patients who are also receiving strong inhibitors of CYP3A4. Consider therapy modification
Cinacalcet: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Cinacalcet. Monitor therapy
Cisapride: Itraconazole may increase the serum concentration of Cisapride. Avoid combination
Clobetasone: Itraconazole may increase the serum concentration of Clobetasone. Avoid combination
Clofazimine: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CloZAPine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of CloZAPine. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Cobicistat: Itraconazole may increase the serum concentration of Cobicistat. Cobicistat may increase the serum concentration of Itraconazole. Management: Limit itraconazole to a maximum adult dose of 200 mg/day in patients treated with the elvitegravir/cobicistat/emtricitabine/tenofovir combination product. Dosing recommendations for other cobicistat-containing products are not available. Consider therapy modification
Cobimetinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Cobimetinib. Avoid combination
Codeine: CYP3A4 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of Codeine. Monitor therapy
Colchicine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Colchicine. Management: Colchicine is contraindicated in patients with impaired renal or hepatic function who are also receiving a strong CYP3A4 inhibitor. In those with normal renal and hepatic function, reduce colchicine dose as directed. See full monograph for details. Consider therapy modification
Colchicine: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Colchicine. Colchicine distribution into certain tissues (e.g., brain) may also be increased. Management: Colchicine is contraindicated in patients with impaired renal or hepatic function who are also receiving a p-glycoprotein inhibitor. In those with normal renal and hepatic function, reduce colchicine dose as directed. See full monograph for details. Consider therapy modification
Conivaptan: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Conivaptan. Avoid combination
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Copanlisib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Copanlisib. Management: If concomitant use of copanlisib and strong CYP3A4 inhibitors cannot be avoided, reduce the copanlisib dose to 45 mg. Monitor patients for increased copanlisib effects/toxicities. Consider therapy modification
Corticosteroids (Orally Inhaled): CYP3A4 Inhibitors (Strong) may increase the serum concentration of Corticosteroids (Orally Inhaled). Management: Orally inhaled fluticasone propionate with a strong CYP3A4 inhibitor is not recommended. Exceptions: Beclomethasone (Oral Inhalation); Triamcinolone (Systemic). Monitor therapy
Corticosteroids (Systemic): CYP3A4 Inhibitors (Strong) may increase the serum concentration of Corticosteroids (Systemic). Exceptions: MethylPREDNISolone; PrednisoLONE (Systemic); PredniSONE. Monitor therapy
Crizotinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Crizotinib. Management: Avoid concomitant use of crizotinib and strong CYP3A4 inhibitors whenever possible. If combined use cannot be avoided, decrease the crizotinib dose to 250 mg daily. Exceptions are discussed in separate monographs. Consider therapy modification
CycloSPORINE (Systemic): Antifungal Agents (Azole Derivatives, Systemic) may decrease the metabolism of CycloSPORINE (Systemic). Fluconazole and isavuconazonium considerations are addressed in separate monographs. Consider therapy modification
CycloSPORINE (Systemic): CYP3A4 Inhibitors (Strong) may increase the serum concentration of CycloSPORINE (Systemic). Consider therapy modification
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May decrease the serum concentration of Itraconazole. Avoid combination
CYP3A4 Inhibitors (Moderate): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CYP3A4 Inhibitors (Strong): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Consider therapy modification
CYP3A4 Substrates (High risk with Inhibitors): CYP3A4 Inhibitors (Strong) may decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Exceptions: Alitretinoin (Systemic); AmLODIPine; Benzhydrocodone; Buprenorphine; Gefitinib; HYDROcodone; Mirtazapine; Praziquantel; Telithromycin; Vinorelbine. Consider therapy modification
Dabigatran Etexilate: P-glycoprotein/ABCB1 Inhibitors may increase serum concentrations of the active metabolite(s) of Dabigatran Etexilate. Monitor therapy
Dabrafenib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Dabrafenib. Avoid combination
Daclatasvir: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Daclatasvir. Management: Decrease the daclatasvir dose to 30 mg once daily if combined with a strong CYP3A4 inhibitor. No dose adjustment is needed when daclatasvir is used with darunavir/cobicistat. Consider therapy modification
Dapoxetine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Dapoxetine. Avoid combination
Darolutamide: Inhibitors of CYP3A4 (Strong) and P-glycoprotein may increase the serum concentration of Darolutamide. Monitor therapy
Darunavir: May increase the serum concentration of Itraconazole. Itraconazole may increase the serum concentration of Darunavir. Management: Limit the adult maximum itraconazole dose to 200 mg/day in patients receiving darunavir/ritonavir. Consider therapy modification
Dasatinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Dasatinib. Management: This combination should be avoided if possible. If combined, dasatinib dose reductions are recommended. See full monograph for details. Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Consider therapy modification
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Deflazacort: CYP3A4 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of Deflazacort. Management: Administer one third of the recommended deflazacort dose when used together with a strong or moderate CYP3A4 inhibitor. Consider therapy modification
Delamanid: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Delamanid. Management: Increase ECG monitoring frequency if delamanid is combined with strong CYP3A4 inhibitors due to the risk for QTc interval prolongation. Continue frequent ECG assessments throughout full delamanid treatment period. Exceptions discussed separately. Consider therapy modification
DexAMETHasone (Ophthalmic): CYP3A4 Inhibitors (Strong) may increase the serum concentration of DexAMETHasone (Ophthalmic). Monitor therapy
Dichlorphenamide: Antifungal Agents (Azole Derivatives, Systemic) may enhance the hypokalemic effect of Dichlorphenamide. Monitor therapy
Didanosine: May decrease the absorption of Antifungal Agents (Azole Derivatives, Systemic). Enteric coated didanosine capsules are not expected to affect these antifungals. Consider therapy modification
Dienogest: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Dienogest. Monitor therapy
Dihydroergotamine: Itraconazole may increase the serum concentration of Dihydroergotamine. Avoid combination
Disopyramide: Itraconazole may increase the serum concentration of Disopyramide. Avoid combination
DOCEtaxel: CYP3A4 Inhibitors (Strong) may increase the serum concentration of DOCEtaxel. Management: Avoid the concomitant use of docetaxel and strong CYP3A4 inhibitors when possible. If combined use is unavoidable, consider a 50% docetaxel dose reduction and monitor for increased docetaxel toxicities. Consider therapy modification
Dofetilide: Itraconazole may increase the serum concentration of Dofetilide. Avoid combination
Domperidone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Domperidone. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Avoid combination
Doxercalciferol: CYP3A4 Inhibitors (Strong) may decrease serum concentrations of the active metabolite(s) of Doxercalciferol. Monitor therapy
DOXOrubicin (Conventional): CYP3A4 Inhibitors (Strong) may increase the serum concentration of DOXOrubicin (Conventional). Management: Seek alternatives to strong CYP3A4 inhibitors in patients treated with doxorubicin whenever possible. One U.S. manufacturer (Pfizer Inc.) recommends that these combinations be avoided. Consider therapy modification
DOXOrubicin (Conventional): P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of DOXOrubicin (Conventional). Management: Seek alternatives to P-glycoprotein inhibitors in patients treated with doxorubicin whenever possible. One U.S. manufacturer (Pfizer Inc.) recommends that these combinations be avoided. Consider therapy modification
Dronabinol: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Dronabinol. Monitor therapy
Dronedarone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Dronedarone. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Avoid combination
Drospirenone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Drospirenone. Management: Drospirenone use is contraindicated specifically when the strong CYP3A4 inhibitors atazanavir and cobicistat are administered concurrently. Caution should be used when drospirenone is coadministered with other strong CYP3A4 inhibitors. Consider therapy modification
Dutasteride: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Dutasteride. Monitor therapy
Duvelisib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Duvelisib. Management: Reduce the dose of duvelisib to 15 mg twice a day when used together with a strong CYP3A4 inhibitor. Consider therapy modification
Edoxaban: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Edoxaban. Management: See full monograph for details. Reduced doses are recommended for patients receiving edoxaban for venous thromboembolism in combination with certain P-gp inhibitors. Similar dose adjustment is not recommended for edoxaban use in atrial fibrillation. Consider therapy modification
Efavirenz: May decrease the serum concentration of Itraconazole. Avoid combination
Elagolix: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Elagolix. Management: Use of the elagolix 200 mg twice daily dose with a strong CYP3A4 inhibitor for longer than 1 month is not recommended. Limit combined use of the elagolix 150 mg once daily dose with a strong CYP3A4 inhibitor to a maximum of 6 months. Consider therapy modification
Eletriptan: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Eletriptan. Avoid combination
Elexacaftor, Tezacaftor, and Ivacaftor: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Elexacaftor, Tezacaftor, and Ivacaftor. Management: When combined with strong CYP3A4 inhibitors, administer two elexacaftor/tezacaftor/ivacaftor tablets (100 mg/50 mg/75 mg) in the morning, twice a week, approximately 3 to 4 days apart. No evening doses of ivacaftor (150 mg) alone should be administered. Consider therapy modification
Eliglustat: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Eliglustat. Management: Use should be avoided under some circumstances. See full drug interaction monograph for details. Consider therapy modification
Elvitegravir: Itraconazole may increase the serum concentration of Elvitegravir. Management: Limit itraconazole to a maximum dose of 200 mg/day in patients who are being treated with the elvitegravir-containing products. Consider therapy modification
Encorafenib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Encorafenib. Management: Avoid concomitant use of encorafenib and strong CYP3A4 inhibitors whenever possible. If concomitant administration is unavoidable, decrease the encorafenib dose. See monograph for details. Consider therapy modification
Enfortumab Vedotin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Enfortumab Vedotin. Specifically, concentrations of the active monomethyl auristatin E (MMAE) component may be increased. Monitor therapy
Entrectinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Entrectinib. Management: Avoid strong CYP3A4 inhibitors during treatment with entrectinib. Reduce dose to 100 mg/day if combination cannot be avoided in adults and those 12 yrs of age or older with a BSA of at least 1.5 square meters. No alternative dosing provided for others. Consider therapy modification
Eplerenone: Itraconazole may increase the serum concentration of Eplerenone. Avoid combination
Erdafitinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Erdafitinib. Management: Avoid concomitant use of erdafitinib and strong CYP3A4 inhibitors when possible. If combined, monitor closely for erdafitinib adverse reactions and consider dose modifications accordingly. Consider therapy modification
Ergoloid Mesylates: Itraconazole may increase the serum concentration of Ergoloid Mesylates. Avoid combination
Ergonovine: Itraconazole may increase the serum concentration of Ergonovine. Avoid combination
Ergotamine: Itraconazole may increase the serum concentration of Ergotamine. Avoid combination
Erlotinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Erlotinib. Management: Avoid use of this combination when possible. When the combination must be used, monitor the patient closely for the development of severe adverse reactions, and if such severe reactions occur, reduce the erlotinib dose (in 50 mg decrements). Consider therapy modification
Estazolam: Itraconazole may increase the serum concentration of Estazolam. Avoid combination
Estrogen Derivatives: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Estrogen Derivatives. Monitor therapy
Eszopiclone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Eszopiclone. Management: Limit the eszopiclone dose to 2 mg daily when combined with strong CYP3A4 inhibitors and monitor for increased eszopiclone effects and toxicities (eg, somnolence, drowsiness, CNS depression). Consider therapy modification
Etizolam: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Etizolam. Management: Consider use of lower etizolam doses when using this combination; specific recommendations concerning dose adjustment are not available. Monitor clinical response to the combination closely. Consider therapy modification
Etravirine: Antifungal Agents (Azole Derivatives, Systemic) may increase the serum concentration of Etravirine. Applicable Isavuconazonium considerations are addressed in separate monographs. Etravirine may decrease the serum concentration of Antifungal Agents (Azole Derivatives, Systemic). This would be anticipated with itraconazole or ketoconazole. Etravirine may increase the serum concentration of Antifungal Agents (Azole Derivatives, Systemic). This would be anticipated with voriconazole. Management: Monitor for increased effects/toxicity of etravirine. Antifungal dose adjustment may be needed for ketoconazole, itraconazole, or posaconazole but specific dosing guidelines are lacking. Consider therapy modification
Everolimus: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Everolimus. Avoid combination
Evogliptin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Evogliptin. Monitor therapy
Fedratinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Fedratinib. Management: Consider alternatives when possible. If used together, decrease fedratinib dose to 200 mg/day. After the inhibitor is stopped, increase fedratinib to 300 mg/day for the first 2 weeks and then to 400 mg/day as tolerated. Consider therapy modification
Felodipine: Itraconazole may increase the serum concentration of Felodipine. Avoid combination
FentaNYL: CYP3A4 Inhibitors (Strong) may increase the serum concentration of FentaNYL. Management: Monitor patients closely for several days following initiation of this combination, and adjust fentanyl dose as necessary. Consider therapy modification
Fesoterodine: CYP3A4 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of Fesoterodine. Management: Avoid fesoterodine doses greater than 4 mg daily in adult patients who are also receiving strong CYP3A4 inhibitors. Consider therapy modification
Fexofenadine: Itraconazole may increase the serum concentration of Fexofenadine. Monitor therapy
Flibanserin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Flibanserin. Avoid combination
Fluticasone (Nasal): CYP3A4 Inhibitors (Strong) may increase the serum concentration of Fluticasone (Nasal). Avoid combination
Fluticasone (Oral Inhalation): CYP3A4 Inhibitors (Strong) may increase the serum concentration of Fluticasone (Oral Inhalation). Management: Use of orally inhaled fluticasone propionate with strong CYP3A4 inhibitors is not recommended. Use of orally inhaled fluticasone furoate with strong CYP3A4 inhibitors should be done with caution. Monitor patients using such a combination more closely. Consider therapy modification
Fosamprenavir: Itraconazole may increase serum concentrations of the active metabolite(s) of Fosamprenavir. Specifically, amprenavir concentrations may be increased. Fosamprenavir may increase the serum concentration of Itraconazole. Management: Limit the adult maximum itraconazole dose to 200 mg/day with fosamprenavir/ritonavir. In patients receiving fosamprenavir without ritonavir, patients receiving greater than 400 mg/day itraconazole may also require dose reduction. Consider therapy modification
Fosaprepitant: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Fosaprepitant. Avoid combination
Fosnetupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fostamatinib: CYP3A4 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of Fostamatinib. Monitor therapy
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Galantamine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Galantamine. Monitor therapy
Gefitinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Gefitinib. Monitor therapy
Gilteritinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Gilteritinib. Management: Consider alternatives to the use of a strong CYP3A4 inhibitor with gilteritinib. If the combination cannot be avoided, monitor more closely for evidence of gilteritinib toxicities. Consider therapy modification
Glasdegib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Glasdegib. Management: Consider alternatives to this combination when possible. If the combination must be used, monitor closely for evidence of QT interval prolongation and other adverse reactions to glasdegib. Consider therapy modification
Grapefruit Juice: May decrease the serum concentration of Itraconazole. Grapefruit Juice may increase the serum concentration of Itraconazole. Monitor therapy
GuanFACINE: CYP3A4 Inhibitors (Strong) may increase the serum concentration of GuanFACINE. Management: Reduce the guanfacine dose by 50% when initiating this combination. Consider therapy modification
Halofantrine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Halofantrine. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Avoid combination
Histamine H2 Receptor Antagonists: May increase the serum concentration of Itraconazole. Histamine H2 Receptor Antagonists may decrease the serum concentration of Itraconazole. Management: Administer Sporanox brand itraconazole at least 2 hours before or 2 hours after administration of any histamine H2 receptor antagonists (H2RAs). Exposure to Tolsura brand itraconazole may be increased by H2RAs; consider itraconazole dose reduction. Consider therapy modification
HYDROcodone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of HYDROcodone. Monitor therapy
Ibrutinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Ibrutinib. Management: Avoid concomitant use of ibrutinib and strong CYP3A4 inhibitors. If a strong CYP3A4 inhibitor must be used short-term (eg, anti-infectives for 7 days or less), interrupt ibrutinib therapy until the strong CYP3A4 inhibitor is discontinued. Avoid combination
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Ifosfamide: CYP3A4 Inhibitors (Strong) may decrease serum concentrations of the active metabolite(s) of Ifosfamide. Monitor therapy
Iloperidone: CYP3A4 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of Iloperidone. Specifically, concentrations of the metabolites P88 and P95 may be increased. CYP3A4 Inhibitors (Strong) may increase the serum concentration of Iloperidone. Management: Reduce iloperidone dose by half when administered with a strong CYP3A4 inhibitor. Consider therapy modification
Imatinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Imatinib. Monitor therapy
Imidafenacin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Imidafenacin. Monitor therapy
Indinavir: Itraconazole may increase the serum concentration of Indinavir. Indinavir may increase the serum concentration of Itraconazole. Management: Reduce the normal indinavir adult dose to 600 mg every 8 hours when given with itraconazole. Monitor for increased systemic effects (including adverse/toxic effects) of itraconazole. Consider therapy modification
Irinotecan Products: CYP3A4 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of Irinotecan Products. Specifically, serum concentrations of SN-38 may be increased. CYP3A4 Inhibitors (Strong) may increase the serum concentration of Irinotecan Products. Avoid combination
Isavuconazonium Sulfate: CYP3A4 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of Isavuconazonium Sulfate. Specifically, CYP3A4 Inhibitors (Strong) may increase isavuconazole serum concentrations. Management: Combined use is considered contraindicated per US labeling. Lopinavir/ritonavir (and possibly other uses of ritonavir doses less than 400 mg every 12 hours) is treated as a possible exception to this contraindication despite strongly inhibiting CYP3A4. Avoid combination
Isoniazid: May decrease the serum concentration of Itraconazole. Monitor therapy
Istradefylline: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Istradefylline. Management: Limit the maximum istradefylline dose to 20 mg daily when combined with strong CYP3A4 inhibitors and monitor for increased istradefylline effects/toxicities. Consider therapy modification
Ivabradine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Ivabradine. Avoid combination
Ivacaftor: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Ivacaftor. Management: Ivacaftor dose reductions are required; consult full monograph content for age- and weight-specific recommendations. Consider therapy modification
Ivosidenib: Itraconazole may increase the serum concentration of Ivosidenib. Ivosidenib may decrease the serum concentration of Itraconazole. Avoid combination
Ixabepilone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Ixabepilone. Consider therapy modification
Lacosamide: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Lacosamide. Monitor therapy
Lapatinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Lapatinib. Management: If an overlap in therapy cannot be avoided, consider reducing lapatinib adult dose to 500 mg/day during, and within 1 week of completing, treatment with the strong CYP3A4 inhibitor. Avoid combination
Larotrectinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Larotrectinib. Management: Avoid use of strong CYP3A4 inhibitors with larotrectinib. If this combination cannot be avoided, reduce the larotrectinib dose by 50%. Increase to previous dose after stopping the inhibitor after a period of 3 to 5 times the inhibitor half-life. Consider therapy modification
Lefamulin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Lefamulin. Management: Avoid concomitant use of lefamulin tablets and strong inhibitors of CYP3A4. Avoid combination
Lemborexant: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Lemborexant. Avoid combination
Lercanidipine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Lercanidipine. Avoid combination
Levobupivacaine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Levobupivacaine. Monitor therapy
Levomilnacipran: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Levomilnacipran. Management: Do not exceed a maximum adult levomilnacipran dose of 80 mg/day in patients also receiving strong CYP3A4 inhibitors. Consider therapy modification
Lomitapide: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Lomitapide. Avoid combination
Lopinavir: May increase the serum concentration of Itraconazole. Management: Limit the adult maximum itraconazole dose to 200 mg/day in patients receiving lopinavir/ritonavir. Consider therapy modification
Lorlatinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Lorlatinib. Management: Avoid use of lorlatinib with strong CYP3A4 inhibitors. If the combination cannot be avoided, reduce the lorlatinib dose from 100 mg once daily to 75 mg once daily, or from 75 mg once daily to 50 mg once daily. Consider therapy modification
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Losartan: Antifungal Agents (Azole Derivatives, Systemic) may decrease the metabolism of Losartan. Applicable Isavuconazonium considerations are addressed in separate monographs. Monitor therapy
Lovastatin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Lovastatin. Avoid combination
Lumateperone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Lumateperone. Avoid combination
Lumefantrine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Lumefantrine. Monitor therapy
Lurasidone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Lurasidone. Avoid combination
Macitentan: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Macitentan. Avoid combination
Manidipine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Manidipine. Management: Consider avoiding concomitant use of manidipine and strong CYP3A4 inhibitors. If combined, monitor closely for increased manidipine effects and toxicities. Manidipine dose reductions may be required. Consider therapy modification
Maraviroc: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Maraviroc. Management: Reduce the adult dose of maraviroc to 150 mg twice daily when used with a strong CYP3A4 inhibitor. Do not use maraviroc with strong CYP3A4 inhibitors in patients with Clcr less than 30 mL/min. Consider therapy modification
MedroxyPROGESTERone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of MedroxyPROGESTERone. Monitor therapy
Meloxicam: Itraconazole may decrease the serum concentration of Meloxicam. Monitor therapy
Meperidine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Meperidine. Monitor therapy
Methadone: Itraconazole may increase the serum concentration of Methadone. Avoid combination
Methylergonovine: Itraconazole may increase the serum concentration of Methylergonovine. Avoid combination
MethylPREDNISolone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of MethylPREDNISolone. Management: Consider methylprednisolone dose reduction in patients receiving strong CYP3A4 inhibitors and monitor for increased steroid related adverse effects. Consider therapy modification
Midazolam: Itraconazole may increase the serum concentration of Midazolam. Management: Oral midazolam is contraindicated. Use intravenous midazolam with great caution in patients receiving itraconazole, employing reduced initial doses whenever possible and monitoring closely for enhanced and prolonged effects. Avoid combination
Midostaurin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Midostaurin. Management: Seek alternatives to the concomitant use of midostaurin and strong CYP3A4 inhibitors if possible. If concomitant use cannot be avoided, monitor patients for increased risk of adverse reactions. Exceptions are discussed in separate monographs. Consider therapy modification
MiFEPRIStone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of MiFEPRIStone. Management: Limit mifepristone adult dose, when used for treatment of hyperglycemia in Cushing's syndrome, to a maximum of 900 mg/day when combined with a strong CYP3A4 inhibitor. Monitor for increased mifepristone toxicity regardless of dose or indication. Consider therapy modification
MiFEPRIStone: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Minimize doses of CYP3A4 substrates, and monitor for increased concentrations/toxicity, during and 2 weeks following treatment with mifepristone. Avoid cyclosporine, dihydroergotamine, ergotamine, fentanyl, pimozide, quinidine, sirolimus, and tacrolimus. Consider therapy modification
Mirodenafil: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Mirodenafil. Management: Consider using a lower dose of mirodenafil when used with strong CYP3A4 inhibitors. Monitor for increased mirodenafil effects/toxicities with the use of this combination. Consider therapy modification
Mirtazapine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Mirtazapine. Monitor therapy
Mizolastine: Antifungal Agents (Azole Derivatives, Systemic) may increase the serum concentration of Mizolastine. Avoid combination
Naldemedine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Naldemedine. Monitor therapy
Naldemedine: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Naldemedine. Monitor therapy
Nalfurafine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Nalfurafine. Monitor therapy
Naloxegol: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Naloxegol. Avoid combination
Neratinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Neratinib. Avoid combination
Netupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Nevirapine: May decrease the serum concentration of Itraconazole. Avoid combination
Nilotinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Nilotinib. Management: Avoid if possible. If combination needed, decrease nilotinib to 300 mg once/day for patients with resistant or intolerant Ph+ CML or to 200 mg once/day for patients with newly diagnosed Ph+ CML in chronic phase. Exceptions discussed in separate monograph. Consider therapy modification
NiMODipine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of NiMODipine. Avoid combination
Nintedanib: Combined Inhibitors of CYP3A4 and P-glycoprotein may increase the serum concentration of Nintedanib. Monitor therapy
Nisoldipine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Nisoldipine. Avoid combination
Olaparib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Olaparib. Management: Avoid use of strong CYP3A4 inhibitors in patients being treated with olaparib, if possible. If such concurrent use cannot be avoided, the dose of olaparib should be reduced to 100 mg twice daily. Consider therapy modification
Ospemifene: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Ospemifene. Monitor therapy
Oxybutynin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Oxybutynin. Monitor therapy
OxyCODONE: CYP3A4 Inhibitors (Strong) may enhance the adverse/toxic effect of OxyCODONE. CYP3A4 Inhibitors (Strong) may increase the serum concentration of OxyCODONE. Serum concentrations of the active metabolite oxymorphone may also be increased. Consider therapy modification
Palbociclib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Palbociclib. Avoid combination
Paliperidone: Itraconazole may enhance the QTc-prolonging effect of Paliperidone. Itraconazole may decrease the metabolism of Paliperidone. Consider therapy modification
Panobinostat: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Panobinostat. Management: Reduce the panobinostat dose to 10 mg when it must be used with a strong CYP3A4 inhibitor. Consider therapy modification
Parecoxib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Parecoxib. Monitor therapy
Paricalcitol: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Paricalcitol. Monitor therapy
PAZOPanib: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of PAZOPanib. Avoid combination
Pexidartinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Pexidartinib. Management: Avoid use of pexidartinib with strong CYP3A4 inhibitors if possible. If combined use cannot be avoided, the pexidartinib dose should be reduced. Decrease 800 mg or 600 mg daily doses to 200 mg twice daily. Decrease doses of 400 mg/day to 200 mg/day. Consider therapy modification
P-glycoprotein/ABCB1 Substrates: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inhibitors may also enhance the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Exceptions: Loperamide. Monitor therapy
Pimavanserin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Pimavanserin. Management: Decrease the pimavanserin dose to 10 mg daily when combined with strong CYP3A4 inhibitors. Consider therapy modification
Pimecrolimus: CYP3A4 Inhibitors (Strong) may decrease the metabolism of Pimecrolimus. Monitor therapy
Pimozide: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Pimozide. Avoid combination
Piperaquine: CYP3A4 Inhibitors (Strong) may enhance the QTc-prolonging effect of Piperaquine. CYP3A4 Inhibitors (Strong) may increase the serum concentration of Piperaquine. Management: Avoid concomitant use of piperaquine and strong CYP3A4 inhibitors when possible. If the combination cannot be avoided, frequent ECG monitoring is recommended due to the risk for QTc prolongation. Exceptions are discussed separately. Consider therapy modification
Polatuzumab Vedotin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Polatuzumab Vedotin. Exposure to unconjugated MMAE, the cytotoxic small molecule component of polatuzumab vedotin, may be increased. Monitor therapy
PONATinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of PONATinib. Management: Per ponatinib U.S. prescribing information, the adult starting dose of ponatinib should be reduced to 30 mg daily during treatment with any strong CYP3A4 inhibitor. Consider therapy modification
Pranlukast: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Pranlukast. Monitor therapy
Pravastatin: Itraconazole may increase the serum concentration of Pravastatin. Monitor therapy
Praziquantel: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Praziquantel. Monitor therapy
PrednisoLONE (Systemic): CYP3A4 Inhibitors (Strong) may increase the serum concentration of PrednisoLONE (Systemic). Monitor therapy
PredniSONE: CYP3A4 Inhibitors (Strong) may increase the serum concentration of PredniSONE. Monitor therapy
Propafenone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Propafenone. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Proton Pump Inhibitors: May increase the serum concentration of Itraconazole. Proton Pump Inhibitors may decrease the serum concentration of Itraconazole. Management: Exposure to Tolsura brand itraconazole may be increased by PPIs; consider itraconazole dose reduction. Exposure to Sporanox brand itraconazole capsules may be decreased by PPIs. Give Sporanox brand itraconazole at least 2 hrs before or 2 hrs after PPIs Consider therapy modification
Prucalopride: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Prucalopride. Monitor therapy
QT-prolonging Agents (Highest Risk): QT-prolonging Agents (Indeterminate Risk - Caution) may enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QUEtiapine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of QUEtiapine. Management: In quetiapine treated patients, reduce quetiapine to one-sixth of regular dose after starting strong CYP3A4 inhibitor. In those on strong CYP3A4 inhibitors, start quetiapine at lowest dose and up-titrate as needed. Exceptions discussed separately. Consider therapy modification
QuiNIDine: Itraconazole may increase the serum concentration of QuiNIDine. Avoid combination
Radotinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Radotinib. Avoid combination
Ramelteon: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Ramelteon. Monitor therapy
Ranolazine: Antifungal Agents (Azole Derivatives, Systemic) may decrease the metabolism of Ranolazine. Fluconazole and isavuconazonium considerations are addressed in separate monographs. Avoid combination
Ranolazine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Ranolazine. Avoid combination
Reboxetine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Reboxetine. Consider therapy modification
Red Yeast Rice: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Red Yeast Rice. Specifically, concentrations of lovastatin and related compounds found in Red Yeast Rice may be increased. Avoid combination
Regorafenib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Regorafenib. Avoid combination
Repaglinide: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Repaglinide. Management: The addition of a CYP2C8 inhibitor to this drug combination may substantially increase the magnitude of increase in repaglinide exposure. Monitor therapy
Retapamulin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Retapamulin. Management: Avoid this combination in patients less than 2 years old. No action is required in other populations. Monitor therapy
Ribociclib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Ribociclib. Management: Avoid use of ribociclib with strong CYP3A4 inhibitors when possible; if combined use cannot be avoided, reduce ribociclib dose to 400 mg once daily. Exceptions are discussed in separate monographs. Consider therapy modification
Rifamycin Derivatives: Antifungal Agents (Azole Derivatives, Systemic) may increase the serum concentration of Rifamycin Derivatives. Only rifabutin appears to be affected. Rifamycin Derivatives may decrease the serum concentration of Antifungal Agents (Azole Derivatives, Systemic). Management: Avoid these combinations when possible. Voriconazole and isavuconazonium are considered contraindicated. Consider therapy modification
RifAXIMin: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of RifAXIMin. Monitor therapy
Rilpivirine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Rilpivirine. Monitor therapy
Riociguat: Itraconazole may increase the serum concentration of Riociguat. Management: Consider starting with a reduced riociguat dose of 0.5 mg three times a day. Patients receiving such a combination should also be monitored extra closely for signs or symptoms of hypotension. Consider therapy modification
Ritonavir: May increase the serum concentration of Itraconazole. Management: Limit the adult maximum itraconazole dose to 200 mg/day in patients receiving ritonavir. Consider therapy modification
Rivaroxaban: Inhibitors of CYP3A4 (Strong) and P-glycoprotein may increase the serum concentration of Rivaroxaban. Avoid combination
RomiDEPsin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of RomiDEPsin. Monitor therapy
Rosuvastatin: Itraconazole may increase the serum concentration of Rosuvastatin. Monitor therapy
Rupatadine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Rupatadine. Avoid combination
Ruxolitinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Ruxolitinib. Management: This combination should be avoided under some circumstances. See monograph for details. Consider therapy modification
Saccharomyces boulardii: Antifungal Agents (Systemic, Oral) may diminish the therapeutic effect of Saccharomyces boulardii. Avoid combination
Salmeterol: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Salmeterol. Avoid combination
Saquinavir: Itraconazole may increase the serum concentration of Saquinavir. Saquinavir may increase the serum concentration of Itraconazole. Management: Limit the adult maximum itraconazole dose to 200 mg/day in patients receiving saquinavir/ritonavir. Consider therapy modification
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
SAXagliptin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of SAXagliptin. Management: Limit the saxagliptin dose to 2.5 mg daily when combined with strong CYP3A4 inhibitors. When using the saxagliptin combination products saxagliptin/dapagliflozin or saxagliptin/dapagliflozin/metformin, avoid use with strong CYP3A4 inhibitors. Consider therapy modification
Sibutramine: CYP3A4 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of Sibutramine. CYP3A4 Inhibitors (Strong) may increase the serum concentration of Sibutramine. Monitor therapy
Sildenafil: Itraconazole may increase the serum concentration of Sildenafil. Management: Concurrent itraconazole is not recommended when sildenafil is used for treatment of pulmonary arterial hypertension. If sildenafil is used to treat erectile dysfunction, an initial dose of 25 mg is recommended with concurrent itraconazole. Consider therapy modification
Silodosin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Silodosin. Avoid combination
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Simeprevir. Avoid combination
Simvastatin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Simvastatin. Avoid combination
Sirolimus: Itraconazole may increase the serum concentration of Sirolimus. Management: Sirolimus dose adjustments will likely be needed when starting/stopping any azole antifungal. Clinical data suggest sirolimus (adult) dose reductions of 50-90% will be needed when starting an azole antifungal, but specific guidelines are lacking. Consider therapy modification
Solifenacin: Itraconazole may increase the serum concentration of Solifenacin. Management: Limit solifenacin doses to 5 mg daily when combined with itraconazole. Do not use solifenacin with itraconazole, or for 2 weeks after itraconazole discontinuation, in patients with moderate to severe hepatic impairment or severe renal impairment. Consider therapy modification
Sonidegib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Sonidegib. Avoid combination
SORAfenib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of SORAfenib. Monitor therapy
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
SUFentanil: CYP3A4 Inhibitors (Strong) may increase the serum concentration of SUFentanil. Management: If a strong CYP3A4 inhibitor is initiated in a patient on sufentanil, consider a sufentanil dose reduction and monitor for increased sufentanil effects and toxicities (eg, respiratory depression). Consider therapy modification
SUNItinib: Itraconazole may increase the serum concentration of SUNItinib. Management: Avoid when possible. If such a combination cannot be avoided, sunitinib dose decreases are recommended, and vary by indication. See full monograph for details. Consider therapy modification
Suvorexant: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Suvorexant. Avoid combination
Tacrolimus (Systemic): Itraconazole may increase the serum concentration of Tacrolimus (Systemic). Management: Monitor tacrolimus concentrations closely and adjust dose as necessary when concomitantly administered with itraconazole. Tacrolimus dose reductions will likely be required. The magnitude of this interaction may be greater in older patients. Consider therapy modification
Tacrolimus (Topical): Antifungal Agents (Azole Derivatives, Systemic) may decrease the metabolism of Tacrolimus (Topical). Applicable Isavuconazonium considerations are addressed in separate monographs. Monitor therapy
Tadalafil: Itraconazole may increase the serum concentration of Tadalafil. Consider therapy modification
Talazoparib: Itraconazole may increase the serum concentration of Talazoparib. Management: If concurrent use cannot be avoided, reduce talazoparib dose to 0.75 mg once daily. After a period of 3 to 5 times the half-life of itraconazole, increase the talazoparib dose to the dose used before initiation of itraconazole. Consider therapy modification
Tamsulosin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Tamsulosin. Avoid combination
Tasimelteon: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Tasimelteon. Monitor therapy
Tazemetostat: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Tazemetostat. Avoid combination
Tegaserod: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Tegaserod. Monitor therapy
Telithromycin: Itraconazole may increase the serum concentration of Telithromycin. Telithromycin may increase the serum concentration of Itraconazole. Avoid combination
Temsirolimus: Itraconazole may increase serum concentrations of the active metabolite(s) of Temsirolimus. Avoid combination
Terfenadine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Terfenadine. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Avoid combination
Tetrahydrocannabinol: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Tetrahydrocannabinol. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Tetrahydrocannabinol and Cannabidiol. Monitor therapy
Tezacaftor and Ivacaftor: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Tezacaftor and Ivacaftor. Management: When combined with strong CYP3A4 inhibitors, tezacaftor/ivacaftor should be administered in the morning, twice a week, approximately 3 to 4 days apart. No evening doses of ivacaftor alone should be administered. Consider therapy modification
Thiotepa: CYP3A4 Inhibitors (Strong) may decrease serum concentrations of the active metabolite(s) of Thiotepa. CYP3A4 Inhibitors (Strong) may increase the serum concentration of Thiotepa. Management: Thiotepa prescribing information recommends avoiding concomitant use of thiotepa and strong CYP3A4 inhibitors. If concomitant use is unavoidable, monitor for adverse effects and decreased efficacy. Consider therapy modification
Ticagrelor: CYP3A4 Inhibitors (Strong) may decrease serum concentrations of the active metabolite(s) of Ticagrelor. CYP3A4 Inhibitors (Strong) may increase the serum concentration of Ticagrelor. Avoid combination
Tipranavir: May increase the serum concentration of Itraconazole. Management: Limit itraconazole adult maximum dose to 200 mg/day in patients treated with tipranavir. Consider therapy modification
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Tofacitinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Tofacitinib. Management: Tofacitinib dose reductions are recommended when combined with strong CYP3A4 inhibitors. Recommended dose adjustments vary by tofacitinib formulation and therapeutic indication. See full monograph for details. Consider therapy modification
Tolterodine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Tolterodine. Management: The maximum recommended adult dose of tolterodine is 2 mg/day when used together with a strong CYP3A4 inhibitor. Consider therapy modification
Tolvaptan: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Tolvaptan. Avoid combination
Topotecan: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Topotecan. Avoid combination
Toremifene: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Toremifene. Management: Use of toremifene with strong CYP3A4 inhibitors should be avoided if possible. If coadministration is necessary, monitor for increased toremifene toxicities, including QTc interval prolongation. Exceptions are discussed in separate monograph. Consider therapy modification
Trabectedin: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Trabectedin. Avoid combination
TraMADol: CYP3A4 Inhibitors (Strong) may increase the serum concentration of TraMADol. Monitor therapy
TraZODone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of TraZODone. Management: Consider the use of a lower trazodone dose and monitor for increased trazodone effects (eg, sedation, QTc prolongation) if combined with strong CYP3A4 inhibitors. Consider therapy modification
Triazolam: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Triazolam. Avoid combination
Ubrogepant: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Ubrogepant. Avoid combination
Udenafil: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Udenafil. Avoid combination
Ulipristal: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Ulipristal. Management: This is specific for when ulipristal is being used for signs/symptoms of uterine fibroids (Canadian indication). When ulipristal is used as an emergency contraceptive, patients receiving this combo should be monitored for ulipristal toxicity. Avoid combination
Upadacitinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Upadacitinib. Monitor therapy
Valbenazine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Valbenazine. Management: Reduce the valbenazine dose to 40 mg daily when combined with strong CYP3A4 inhibitors. Consider therapy modification
Vardenafil: Itraconazole may increase the serum concentration of Vardenafil. Management: Limit vardenafil to a max of 5 mg/24 hours in patients receiving itraconazole 200 mg/day, and a max of 2.5 mg/24 hours in patients receiving itraconazole 400 mg/day. Itraconazole labeling and Staxyn brand of vardenafil both recommend avoiding this combo. Consider therapy modification
Vemurafenib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Vemurafenib. Management: Avoid concurrent use of vemurafenib with strong CYP3A4 inhibitors when possible. Consider use of an alternative that is not a strong inhibitor of CYP3A4 as clinically appropriate. Consider therapy modification
Venetoclax: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Venetoclax. Management: This combination is contraindicated during venetoclax initiation and ramp-up in patients with CLL/SLL. Reduced venetoclax doses are required during ramp-up for patients with AML, and reduced doses are required for all patients during maintenance therapy. Consider therapy modification
Venetoclax: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Venetoclax. Management: Consider a venetoclax dose reduction by at least 50% in patients requiring concomitant treatment with P-glycoprotein (P-gp) inhibitors. Consider therapy modification
Vilanterol: May increase the serum concentration of CYP3A4 Inhibitors (Strong). Monitor therapy
Vilazodone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Vilazodone. Management: Limit maximum adult vilazodone dose to 20 mg daily in patients receiving strong CYP3A4 inhibitors. The original vilazodone dose can be resumed following discontinuation of the strong CYP3A4 inhibitor. Consider therapy modification
VinBLAStine: Itraconazole may increase the serum concentration of VinBLAStine. Monitor therapy
VinCRIStine: Itraconazole may enhance the adverse/toxic effect of VinCRIStine. Itraconazole may increase the serum concentration of VinCRIStine. Consider therapy modification
VinCRIStine (Liposomal): CYP3A4 Inhibitors (Strong) may increase the serum concentration of VinCRIStine (Liposomal). Avoid combination
VinCRIStine (Liposomal): P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of VinCRIStine (Liposomal). Avoid combination
Vindesine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Vindesine. Monitor therapy
Vinflunine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Vinflunine. Avoid combination
Vinorelbine: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Vinorelbine. Monitor therapy
Vitamin K Antagonists (eg, warfarin): Itraconazole may increase the serum concentration of Vitamin K Antagonists. Monitor therapy
Vorapaxar: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Vorapaxar. Avoid combination
Voxelotor: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Voxelotor. Management: Avoid concomitant use of voxelotor and strong CYP3A4 inhibitors. If concomitant use is unavoidable, reduce the voxelotor dose to 1,000 mg once daily. Consider therapy modification
Zanubrutinib: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Zanubrutinib. Management: Decrease the zanubrutinib dose to 80 mg once daily during coadministration with a strong CYP3A4 inhibitor. Further dose adjustments may be required for zanubrutinib toxicities, refer to prescribing information for details. Consider therapy modification
Zolpidem: Itraconazole may increase the serum concentration of Zolpidem. Monitor therapy
Zopiclone: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Zopiclone. Management: The initial starting adult dose of zopiclone should not exceed 3.75 mg if combined with a strong CYP3A4 inhibitor. Monitor patients for signs and symptoms of zopiclone toxicity if these agents are combined. Consider therapy modification
Zuclopenthixol: CYP3A4 Inhibitors (Strong) may increase the serum concentration of Zuclopenthixol. Management: Consider zuclopenthixol dosage reduction with concomitant use of a strong CYP3A4 inhibitor (eg, ketoconazole) in poor CYP2D6 metabolizers or with strong CYP2D6 inhibitors (eg, paroxetine). Monitor for increased zuclopenthixol levels/toxicity. Consider therapy modification
Adverse Reactions
>10%: Gastrointestinal: Diarrhea (3% to 11%), nausea (3% to 11%)
1% to 10%:
Cardiovascular: Edema (4%), chest pain (3%), hypertension (2% to 3%),
Central nervous system: Headache (1% to 10%), dizziness (2% to 4%), anxiety (3%), depression (2% to 3%), fatigue (2% to 3%), pain (2% to 3%), malaise (1% to 3%), abnormal dreams (2%)
Dermatologic: Skin rash (3% to 9%), pruritus (≤5%), diaphoresis (3%)
Endocrine & metabolic: Hypertriglyceridemia (≤3%), hypokalemia (2%)
Gastrointestinal: Vomiting (5% to 7%), abdominal pain (2% to 6%), dyspepsia (≤4%), flatulence (≤4%), gastrointestinal disease (≤4%), gingivitis (3%), aphthous stomatitis (≤3%), constipation (2% to 3%), gastritis (2%), gastroenteritis (2%), increased appetite (2%)
Genitourinary: Cystitis (2%), urinary tract infection (2%)
Hepatic: Abnormal hepatic function tests (3%), increased liver enzymes (4%)
Infection: Herpes zoster (2%)
Neuromuscular & skeletal: Bursitis (3%), myalgia (≤3%), tremor (2%)
Respiratory: Rhinitis (5% to 9%), upper respiratory tract infection (8%), sinusitis (2% to 7%), cough (4%), dyspnea (2%), pneumonia (2%), pharyngitis (≤2%)
Miscellaneous: Fever (2% to 7%)
<2%, postmarketing, and/or case reports: Abnormal urinalysis, acute generalized exanthematous pustulosis, adrenocortical insufficiency, albuminuria, alopecia, anaphylactoid reaction, anaphylaxis, angioedema, anorexia, arthralgia, blurred vision, cardiac arrhythmia, cardiac failure, chills, confusion, decreased libido, dehydration, diplopia, drowsiness, dysgeusia, dysphagia, erectile dysfunction, erythema multiforme, erythematous rash, exfoliative dermatitis, facial edema, gynecomastia, hearing loss, hematuria, hepatic failure, hepatitis, hepatotoxicity, hot flash, hyperbilirubinemia, hyperglycemia, hyperhidrosis, hyperkalemia, hypersensitivity angiitis, hypersensitivity reaction, hypoesthesia, hypomagnesemia, hypotension, impotence, increased blood urea nitrogen, increased creatine phosphokinase, increased gamma-glutamyl transferase, increased lactate dehydrogenase, increased serum alkaline phosphatase, increased serum ALT, increased serum AST, insomnia, jaundice, left heart failure, leukopenia, menstrual disease, mucosal inflammation, neutropenia, orthostatic hypotension, pancreatitis, paresthesia, peripheral edema, peripheral neuropathy, pharyngolaryngeal pain, pollakiuria, pulmonary edema, renal insufficiency, rigors, serum sickness, sinus bradycardia, skin photosensitivity, Stevens-Johnson syndrome, tachycardia, thrombocytopenia, tinnitus, toxic epidermal necrolysis, urinary incontinence, urticaria, vasculitis, vertigo, voice disorder
Warnings/Precautions
Concerns related to adverse effects:
- CNS depression: May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks that require mental alertness (eg, operating machinery, driving)
- Hearing loss: Transient or permanent hearing loss has been reported. Quinidine (a contraindicated drug) was used concurrently in several of these cases. Hearing loss usually resolves after discontinuation, but may persist in some patients.
- Heart failure: [US Boxed Warning]: Itraconazole can cause or exacerbate heart failure (HF). Negative inotropic effects have been observed following intravenous administration. Use with caution in patients with risk factors for HF (COPD, renal failure, edematous disorders, ischemic or valvular disease). Inform such patients of the signs and symptoms of HF and monitor carefully during treatment. If signs or symptoms of HF occur or worsen during administration of itraconazole, discontinue use or reassess the risk-benefit of continuing treatment. In postmarketing experience, HF was more frequently reported in patients receiving a total daily dose of 400 mg, although there were also cases reported among those receiving lower total daily doses. In a scientific statement from the American Heart Association, itraconazole has been determined to be an agent that may exacerbate underlying myocardial dysfunction (magnitude: major); may consider use when treating life-threatening fungal infections (AHA [Page 2016]).
- Hepatotoxicity: Rare cases of serious hepatotoxicity (including liver failure and death) have been reported (including some cases occurring within the first week of therapy); hepatotoxicity was reported in some patients without preexisting liver disease or risk factors. Discontinue treatment if signs or symptoms of hepatotoxicity develop.
- Hypersensitivity: Hypersensitivity reactions have been reported; discontinue use and institute appropriate supportive care if a hypersensitivity reaction occurs. Use with caution in patients with a history of hypersensitivity to other azoles.
- Neuropathy: Cases of peripheral neuropathy have occurred in patients on long-term itraconazole. Monitor for and discontinue if signs or symptoms of neuropathy occur during treatment.
Disease-related concerns:
- Cystic fibrosis: Large differences in itraconazole pharmacokinetic parameters have been observed in cystic fibrosis patients receiving the oral solution; if a patient with cystic fibrosis does not respond to therapy, alternate therapies should be considered.
- Hepatic impairment: Use with caution in patients with hepatic impairment; monitor liver function closely. Not recommended for use in patients with active liver disease, elevated liver enzymes, or prior hepatotoxic reactions to other drugs unless the expected benefit exceeds the risk of hepatotoxicity.
- Onychomycosis: [US Boxed Warning]: Use is contraindicated for treatment of onychomycosis in patients with ventricular dysfunction such as heart failure (HF) or a history of HF. Cases of HF, peripheral edema, and pulmonary edema have occurred in this patient population. The manufacturer recommends confirmation of diagnosis testing of nail specimens prior to treatment of onychomycosis.
- Renal impairment: Use with caution in patients with renal impairment; limited information is available; dosage adjustment may be needed.
Concurrent drug therapy issues:
- Drug-drug interactions: Additional potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
- High potential for interactions: Life-threatening cardiac dysrhythmias and/or sudden death have occurred in patients taking CYP 3A inhibitors such as cisapride, pimozide, methadone or quinidine. [US Boxed Warning]: Coadministration with itraconazole can cause elevated plasma concentrations of certain drugs and can lead to QT prolongation and ventricular tachyarrhythmias, including torsades de pointes. Coadministration with methadone, disopyramide, dofetilide, dronedarone, quinidine, isavuconazole, ergot alkaloids, irinotecan, lurasidone, oral midazolam, pimozide, triazolam, felodipine, nisoldipine, ivabradine, ranolazine, eplerenone, cisapride, naloxegol, lomitapide, lovastatin, simvastatin, avanafil, ticagrelor and, in subjects with varying degrees of renal or hepatic impairment, colchicine, fesoterodine, and solifenacin is contraindicated. Coadministration with eliglustat is contraindicated in poor or intermediate metabolizers of CYP2D6 and in patients taking strong or moderate CYP2D6 inhibitors.
Dosage form specific issues:
- Oral capsules (100 mg [Sporanox])/tablets: Absorption of itraconazole capsules is reduced when gastric acidity is reduced (eg, achlorhydria, acid suppressive therapy) administer capsules or tablets with an acidic beverage (eg, non-diet cola) in patients with reduced gastric acidity and separate administration from acid suppressive therapy (refer to drug interactions section). Monitor for response.
- Oral capsules (65 mg [Tolsura]): Absorption of itraconazole capsules is increased when gastric acidity is reduced (eg, acid suppressive therapy). Monitor for adverse reactions; itraconazole dose reduction may be necessary.
- Oral solution: Only the oral solution has proven efficacy in oral/esophageal candidiasis; mucosal exposure may vary between the oral solution and capsules. Initiation of treatment with oral solution is not recommended in patients at immediate risk for systemic candidiasis (eg, patients with severe neutropenia). Oral solution contains the excipient cyclodextrin.
- Product interchangeability: Due to differences in bioavailability, formulations cannot be used interchangeably.
- Propylene glycol: Some dosage forms may contain propylene glycol; large amounts are potentially toxic and have been associated hyperosmolality, lactic acidosis, seizures and respiratory depression; use caution (AAP 1997; Zar 2007).
Other warnings/precautions:
- Appropriate use: Itraconazole should NOT be used for voriconazole-refractory aspergillosis because the same antifungal and/or resistance mechanism(s) may be shared by both agents.
Monitoring Parameters
Liver function in patients with preexisting hepatic dysfunction, and in all patients as clinically indicated; renal function; signs/symptoms of HF
For invasive aspergillosis (treatment or prolonged prophylaxis), guidelines recommend monitoring serum trough concentrations (IDSA [Patterson 2016]). Consider monitoring serum trough concentrations for other infections; itraconazole has a variable pharmacokinetic profile and high concentrations may increase the risk of adverse events (Lestner 2009).
Pregnancy
Pregnancy Considerations
Congenital abnormalities (eg, skeletal, genitourinary tract, cardiovascular and ophthalmic malformations, chromosomal abnormalities, and multiple malformations) have been reported during postmarketing surveillance; however, a causal relationship has not been established.
Itraconazole is contraindicated for the treatment of onychomycosis during pregnancy. Although itraconazole is approved for the treatment of various fungal infections, when treatment of a systemic fungal infection is needed in pregnant females, itraconazole should be avoided, especially during the first trimester (Chapman 2008; Galgiani 2016; HHS [OI adult 2017]; Pappas 2016; Perfect 2010; Wheat 2007).
Use is contraindicated in females planning a pregnancy. The manufacturer recommends that when used for the treatment of onychomycosis in females of reproductive potential, effective contraception should be used during treatment and for 2 months following treatment. Therapy should begin on the second or third day following menses.
Patient Education
What is this drug used for?
- It is used to treat fungal infections.
Frequently reported side effects of this drug
- Abdominal pain
- Nausea
- Vomiting
- Diarrhea
- Lack of appetite
- Loss of strength and energy
- Fatigue
- Runny nose
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Electrolyte problems like mood changes, confusion, muscle pain or weakness, abnormal heartbeat, seizures, lack of appetite, or severe nausea or vomiting.
- High blood sugar like confusion, fatigue, increased thirst, increased hunger, passing a lot of urine, flushing, fast breathing, or breath that smells like fruit.
- Heart problems like cough or shortness of breath that is new or worse, swelling of the ankles or legs, abnormal heartbeat, weight gain of more than five pounds in 24 hours, dizziness, or passing out.
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Burning or numbness feeling
- Difficulty urinating
- Chest pain
- Severe headache
- Severe dizziness
- Passing out
- Chills
- Vision changes
- Confusion
- Edema
- Loss of sex drive
- Sexual dysfunction
- Hearing loss
- Trouble hearing
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.