Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Solution, Oral [preservative free]:
Corlanor: 5 mg/5 mL (5 mL)
Tablet, Oral:
Corlanor: 5 mg [scored]
Corlanor: 7.5 mg
Pharmacology
Mechanism of Action
Selective and specific inhibition of the hyperpolarization-activated cyclic nucleotide-gated (HCN) channels (f-channels) within the sinoatrial (SA) node of cardiac tissue resulting in disruption of If ion current flow prolonging diastolic depolarization, slowing firing in the SA node, and ultimately reducing heart rate. Has not demonstrated effects on myocardial contractility or relaxation, ventricular repolarization, or conduction apart from the sinus node effects. Partial inhibition of the retinal Ih current (similar to the cardiac If current) may explain visual disturbances (eg, phosphenes) (Nawarskas 2015).
Pharmacokinetics/Pharmacodynamics
Distribution
Vd: ~100 L
Metabolism
Extensively intestinal and hepatic via CYP3A4; major active metabolite equipotent to ivabradine is the N-desmethylated derivative (S 18982) which is also metabolized by CYP3A4
Excretion
Feces and urine (~4% as unchanged drug)
Time to Peak
Plasma: ~1 hour (fasting); ~2 hours (with food)
Half-Life Elimination
Distribution half-life: 2 hours; Effective half-life: ~6 hours
Protein Binding
~70%
Use: Labeled Indications
Heart failure: To reduce the risk of hospitalization for worsening heart failure in adult patients with stable, symptomatic (NYHA class II to III according to the ACC/AHA/HFSA heart failure guidelines [Yancy 2016]) chronic heart failure with left ventricular ejection fraction ≤35%, who are in sinus rhythm with resting heart rate ≥70 beats per minute (bpm) and either are on maximally tolerated doses of beta blockers or have a contraindication to beta-blocker use.
Use: Off Label
Inappropriate sinus tachycardiacyes
Data from a small, prospective, randomized, placebo-controlled, crossover trial demonstrated that ivabradine significantly reduced daytime heart rate and improved exercise tolerance and symptoms in patients with inappropriate sinus tachycardia (IST) Cappato 2012. In addition, ivabradine may be combined with beta-blocker therapy in patients who are refractory to monotherapy Ptaszynski 2013. Additional data may be necessary to further define the role of ivabradine in this condition.
Based on the American College of Cardiology/American Heart Association/Heart Rhythm Society guidelines for the management of patients with supraventricular arrhythmias, ivabradine may be a reasonable treatment option for ongoing management of symptomatic IST.
Stable anginabyes
A multicenter, placebo-controlled trial evaluating the addition of ivabradine to current stable angina therapy demonstrated no significant differences in the incidence of primary end points (composite of death from cardiovascular events or nonfatal myocardial infarction) or incidence of primary end point components. In a single-center, placebo-controlled trial, ivabradine in combination with atenolol significantly improved total exercise endurance compared with atenolol alone in patients with stable angina. The long-term clinical and cost effectiveness of adding ivabradine to beta-blocker or calcium channel blocker therapy is unknown.
According to European and UK guidelines, ivabradine is recommended as second-line therapy (or as first-line therapy in select patients) for treatment of adults with chronic stable angina. Ivabradine is approved in Europe for symptomatic treatment of patients with chronic stable angina, normal sinus rhythm, and a heart rate of at least 70 bpm, specifically as monotherapy in cases unresponsive to or intolerant of beta-blockers, or as add-on therapy in cases uncontrolled by beta-blockers alone. US guidelines provide pharmacology and evidence for ivabradine; however, because ivabradine was not approved in the United States when the guidelines were published, no specific recommendation was made regarding its use.
Contraindications
Acute decompensated heart failure; clinically significant hypotension; sick sinus syndrome, sinoatrial block, or third-degree AV block (unless a functioning demand pacemaker is present); clinically significant bradycardia; severe hepatic impairment; pacemaker dependence (heart rate maintained exclusively by the pacemaker); concomitant use with strong CYP3A4 inhibitors
Canadian labeling: Additional contraindications (not in US labeling): Hypersensitivity to ivabradine or any component of the formulation; resting heart rate <70 bpm prior to treatment; prolonged QT interval (eg, congenital long QT syndrome); cardiogenic shock; acute myocardial infarction; concomitant use of verapamil or diltiazem; pregnancy, breastfeeding, or women of child-bearing potential not using appropriate contraception; hereditary problems of galactose intolerance, glucose-galactose malabsorption, or the Lapp lactase deficiency
Dosage and Administration
Dosing: Adult
Heart failure: Oral: Initial: 5 mg twice daily or 2.5 mg twice daily in patients with a history of conduction defects or who may experience hemodynamic compromise due to bradycardia. After 2 weeks, adjust dose to achieve a resting heart rate between 50 and 60 beats per minute (bpm). Thereafter, adjust dose as needed based on resting heart rate and tolerability. Maximum dose: 7.5 mg twice daily.
Dosage adjustment based on resting heart rate:
If heart rate >60 bpm: Increase dose by 2.5 mg twice daily (maximum dose: 7.5 mg twice daily)
If heart rate 50 to 60 bpm: Maintain dose
If heart rate <50 bpm or signs and symptoms of bradycardia: Decrease dose by 2.5 mg twice daily; if current dose is 2.5 mg twice daily, discontinue therapy
Inappropriate sinus tachycardia (off-label use): Oral: Initial: 5 mg twice daily; maintenance: 7.5 mg twice daily (ACC/AHA/HRS [Page 2015]; Cappato 2012). May also use in combination with a beta-blocker (eg, metoprolol) in patients who are refractory to monotherapy (Ptaszynski 2013).
Stable angina (off-label use): Adults <75 years: Oral: Initial: 2.5 to 5 mg twice daily; titrate up in increments of 2.5 mg after 3 to 4 weeks if symptoms persist and heart rate is greater than 60 bpm to a maximum dose of 7.5 mg twice daily. Discontinue therapy if angina symptoms do not improve within 3 months of initiation. Also consider discontinuation if improvement of angina symptoms is limited and no clinically significant heart rate reduction occurs in the first 3 months. If heart rate is lower than 50 bpm at rest or patient experiences symptomatic bradycardia (eg, dizziness, fatigue, hypotension) during therapy, decrease dose by 2.5 mg per dose, or discontinue if already at the minimum dose of 2.5 mg twice daily. Monitor heart rate carefully after dosage reduction. If heart rate continues to be lower than 50 bpm or symptoms of bradycardia persist, discontinue ivabradine (Corlentor 2015).
If symptoms are not controlled on beta-blocker or calcium channel blocker monotherapy, addition of ivabradine can be considered. If combined with a calcium channel blocker, use of a dihydropyridine (such as slow-release nifedipine, amlodipine, or felodipine) is suggested (Montalescot 2013; NICE 2012).
Dosing: Geriatric
Heart failure: Refer to adult dosing.
Stable angina (off-label use): Adults ≥75 years: Initial: Oral: Consider 2.5 mg twice daily. Titration and maintenance: Refer to adult dosing.
Dosing: Pediatric
Heart failure, dilated cardiomyopathy:
Infants ≥6 months, Children, and Adolescents <18 years:
<40 kg: Oral: Initial: 0.05 mg/kg/dose twice daily; may increase dose every 2 weeks by 0.05 mg/kg/dose as tolerated to achieve a 20% reduction in heart rate without inducing bradycardia.
Maximum dose: Age-dependent:
≥6 months to <1 year: 0.2 mg/kg/dose twice daily.
≥1 year: 0.3 mg/kg/dose twice daily, not to exceed 7.5 mg/dose twice daily.
Dosage adjustment for bradycardia:
Initial dose: Decrease dose to 0.02 mg/kg/dose twice daily.
During titration: Decrease dose to previous dose.
≥40 kg: Oral: Initial: 2.5 mg twice daily; may increase dose every 2 weeks by 2.5 mg as tolerated to achieve a 20% reduction in heart rate without inducing bradycardia; maximum dose: 7.5 mg/dose twice daily.
Dosage adjustment for bradycardia: Decrease dose to previous dose.
Adolescents ≥18 years: Oral: Initial: 5 mg twice daily or 2.5 mg twice daily in patients with a history of conduction defects or who may experience hemodynamic compromise due to bradycardia; after 2 weeks, adjust dose to achieve a resting heart rate between 50 and 60 beats per minute (bpm); adjust dose as needed based on resting heart rate and tolerability; maximum dose: 7.5 mg/dose twice daily.
Dosage adjustment based on resting heart rate:
If heart rate >60 bpm: Increase dose by 2.5 mg twice daily; maximum dose: 7.5 mg/dose twice daily.
If heart rate 50 to 60 bpm: Maintain dose.
If heart rate <50 bpm or signs and symptoms of bradycardia: Decrease dose by 2.5 mg twice daily; if current dose is 2.5 mg twice daily, discontinue therapy.
Administration
Oral: Administer with food. Oral solution can be used for adults unable to swallow tablets. For oral solution, empty entire contents of ampule(s) into a medication cup; use a calibrated oral syringe to measure prescribed dose from the medication cup. Discard any unused oral solution.
Storage
Store at 25ºC (77ºF); excursions are permitted between 15ºC and 30ºC (59ºF and 86ºF). To protect from light, keep oral solution ampules in original foil pouches until use.
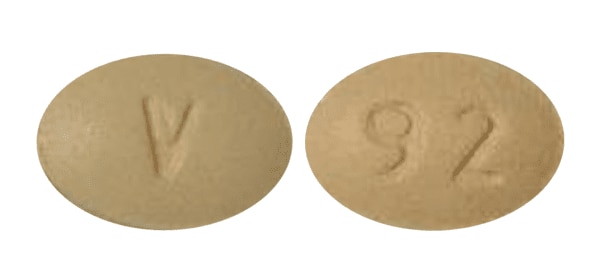
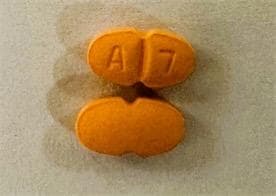
Ivabradine Images
Drug Interactions
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Bradycardia-Causing Agents: May enhance the bradycardic effect of Ivabradine. Monitor therapy
Calcium Channel Blockers (Nondihydropyridine): May enhance the bradycardic effect of Ivabradine. Ivabradine may enhance the QTc-prolonging effect of Calcium Channel Blockers (Nondihydropyridine). Specifically, the QTc prolonging effects of bepridil may be enhanced. Calcium Channel Blockers (Nondihydropyridine) may increase the serum concentration of Ivabradine. Specifically, verapamil or diltiazem may increase serum ivabradine concentrations. Avoid combination
Clofazimine: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May decrease the serum concentration of Ivabradine. Avoid combination
CYP3A4 Inhibitors (Moderate): May increase the serum concentration of Ivabradine. Avoid combination
CYP3A4 Inhibitors (Strong): May increase the serum concentration of Ivabradine. Avoid combination
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fexinidazole [INT]: Bradycardia-Causing Agents may enhance the arrhythmogenic effect of Fexinidazole [INT]. Avoid combination
Fosaprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Grapefruit Juice: May increase the serum concentration of Ivabradine. Avoid combination
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Lacosamide: Bradycardia-Causing Agents may enhance the AV-blocking effect of Lacosamide. Monitor therapy
Larotrectinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Loop Diuretics: May enhance the arrhythmogenic effect of Ivabradine. Monitor therapy
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Midodrine: May enhance the bradycardic effect of Bradycardia-Causing Agents. Monitor therapy
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Regorafenib: May enhance the bradycardic effect of Ivabradine. Monitor therapy
Ruxolitinib: May enhance the bradycardic effect of Bradycardia-Causing Agents. Management: Ruxolitinib Canadian product labeling recommends avoiding use with bradycardia-causing agents to the extent possible. Monitor therapy
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Siponimod: Bradycardia-Causing Agents may enhance the bradycardic effect of Siponimod. Management: Avoid coadministration of siponimod with drugs that may cause bradycardia. Consider therapy modification
St John's Wort: May decrease the serum concentration of Ivabradine. Avoid combination
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
Terlipressin: May enhance the bradycardic effect of Bradycardia-Causing Agents. Monitor therapy
Thiazide and Thiazide-Like Diuretics: May enhance the arrhythmogenic effect of Ivabradine. Monitor therapy
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Tofacitinib: May enhance the bradycardic effect of Bradycardia-Causing Agents. Monitor therapy
Adverse Reactions
1% to 10%:
Cardiovascular: Bradycardia (4% to 10%), hypertension (9%), atrial fibrillation (8%)
Central nervous system: Phosphene (3%)
Frequency not defined: Cardiovascular: Heart block, sinoatrial arrest
<1%, postmarketing, and/or case reports: Angioedema, diplopia, erythema, hypotension, pruritus, skin rash, syncope, torsades de pointes, urticaria, ventricular fibrillation, ventricular tachycardia, vertigo, visual impairment
Warnings/Precautions
Concerns related to adverse events:
- Atrial fibrillation: Use increases the risk of atrial fibrillation; monitor cardiac rhythm. Discontinue if atrial fibrillation develops.
- Bradycardia and conduction disturbances: Bradycardia, sinus arrest, and heart block may occur; monitor heart rate prior to initiation and with any dosage adjustment. Bradycardia may increase the risk of QT prolongation, which may lead to severe ventricular arrhythmias, including torsade de pointes, especially in patients with risk factors such as use of QTc prolonging drugs. Risk factors for bradycardia include sinus node dysfunction, conduction defects (eg, first- or second-degree AV block, bundle branch block), ventricular dyssynchrony, and use of other negative chronotropes (eg, digoxin, diltiazem, verapamil, amiodarone). Avoid concurrent use with verapamil and diltiazem. Avoid use in patients with second-degree AV block (unless a functioning demand pacemaker is present). Use is contraindicated in patients with sick sinus syndrome, sinoatrial block, third-degree AV block (unless a functioning demand pacemaker is present), or pacemaker dependence. Decrease dose or discontinue use if heart rate <50 bpm persists during therapy or signs and symptoms of bradycardia occur. Use is contraindicated in patients with clinically significant bradycardia. In patients with history of conduction defects or in whom bradycardia could lead to hemodynamic compromise, initial dosage reduction is recommended. Heart rate reduction may prolong the uncorrected QT interval while QTc interval remains unchanged (Camm 2003; Murat 2009). At concentrations slightly higher than that achieved with therapeutic dosing, ivabradine prolonged ventricular repolarization in perfused guinea-pig hearts (Melgari 2015). Torsades de pointes has been reported when used with other drugs that produce bradycardia or prolong the QT interval (Cocco 2015; Mittal 2014).
- Visual function: Phosphenes (described as transient enhanced brightness in a limited area of the visual field, halos, image decomposition, colored bright lights, or multiple images) may occur with use. Onset is generally within the first 2 months of therapy and is reported to be of mild to moderate intensity; most cases resolve during or after treatment discontinuation.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Monitoring Parameters
Heart rate (prior to initiation, prior to increasing dose, or after decreasing dose); monitor heart rate more closely if receiving other negative chronotropes (eg, amiodarone, beta-blockers, digoxin); blood pressure; regularly monitor cardiac rhythm (assessing for atrial fibrillation)
Pregnancy
Pregnancy Considerations
Adverse events have been observed in animal reproduction studies, and fetal harm may occur if ivabradine is administered to pregnant women. Effective contraception is recommended in women of reproductive potential. If treatment is needed during pregnancy, closely monitor for destabilization of heart failure that could potentially result from heart rate slowing caused by ivabradine, especially during the first trimester. Pregnant women with chronic heart failure should also be monitored for preterm birth.
Patient Education
What is this drug used for?
- It is used to treat heart failure (weak heart).
- It is used in certain patients with heart failure to lower the chance of having to go to the hospital for heart failure that gets worse.
- It may be given to you for other reasons. Talk with the doctor.
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Slow heartbeat
- Abnormal heartbeat
- Dizziness
- Passing out
- Chest pain
- Shortness of breath
- Loss of strength and energy
- Vision changes
- Severe headache
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.