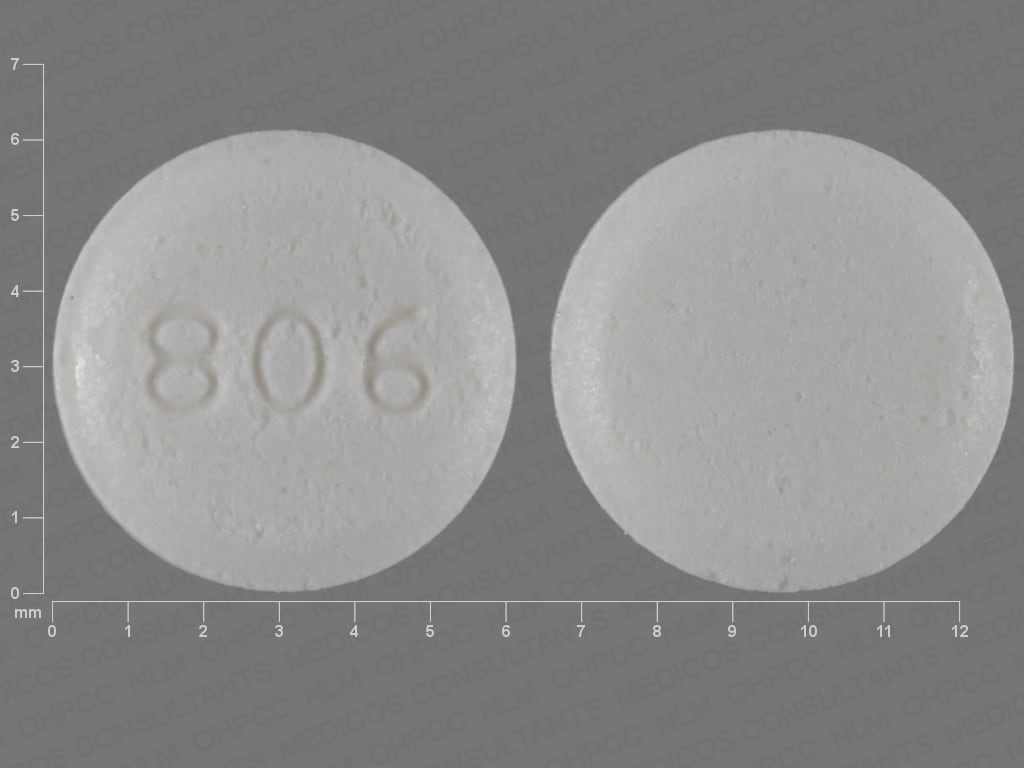
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral:
Stromectol: 3 mg
Generic: 3 mg
Pharmacology
Mechanism of Action
Ivermectin is a semisynthetic anthelminthic agent; it binds selectively and with strong affinity to glutamate-gated chloride ion channels which occur in invertebrate nerve and muscle cells. This leads to increased permeability of cell membranes to chloride ions then hyperpolarization of the nerve or muscle cell, and death of the parasite.
Pharmacokinetics/Pharmacodynamics
Absorption
Well absorbed (Gonzalez Canga 2008)
Distribution
Vd: 3.1 to 3.5 L/kg (healthy males); high concentration in the liver and adipose tissue; does not readily cross the blood-brain barrier (Gonzalez Canga 2008)
Metabolism
Hepatic via CYP3A4 (major), CYP2D6 (minor), and CYP2E1 (minor)
Excretion
Feces; urine (<1%)
Time to Peak
~4 hours
Half-Life Elimination
18 hours
Protein Binding
~93% primarily to albumin (Gonzalez Canga 2008)
Use: Labeled Indications
Onchocerciasis: Treatment of onchocerciasis due to the immature form of Onchocerca volvulus.
Limitations of use: Ivermectin has no activity against adult Onchocerca volvulus parasites. The adult parasites reside in subcutaneous nodules which are infrequently palpable. Surgical excision may be considered as removal of these nodules will eliminate the microfilariae-producing adult parasites.
Strongyloidiasis, intestinal: Treatment of intestinal (eg, nondisseminated) strongyloidiasis due to Strongyloides stercoralis.
Use: Off Label
Ascariasisb
Data from two clinical trials in patients with intestinal helminths supports the use of ivermectin in the treatment of Ascaris lumbricoides infection Marti 1996, Naquira 1989. Additional trials may be necessary to further define the role of ivermectin in this condition.
Demodicosisc
Data from a limited number of patients (one case report) with an abscessing nodular demodicosis due to hair follicle mites Demodex folliculorum and Demodex brevis, suggest that ivermectin may be beneficial for the treatment of this condition Eismann 2010. Additional trials may be necessary to further define the role of ivermectin in this condition.
Clinical experience also suggests the utility of ivermectin in the treatment of demodicosis (Elston 2010).
Gnathostomiasisc
Data from two randomized, open-label trials in patients with gnathostomiasis due to Gnathostoma spinigerum supports the use of ivermectin for this condition Kraivichian 2004, Nontasut 2000. Additional trials may be necessary to further define the role of ivermectin in this condition.
Hookworm-related cutaneous larva migransc
Data from a retrospective study in patients with hookworm-related cutaneous larva migrans (HrCLM) supports the use of a single dose of ivermectin in the treatment of this condition Vanhaecke 2013. Additional trials may be necessary to further define the role of ivermectin in this condition.
Licebyes
Data from one multicenter, cluster-randomized, double-blind, double-dummy, controlled trial Chosidow 2010 and one nonrandomized, open-label study Foucault 2006 supports the use of ivermectin in patients with lice due to Pediculus humanus capitis, Pediculus humanus corporis, and Phthirus pubis (pediculosis pubis; pubic lice). Additional trials may be necessary to further define the role of ivermectin in this condition.
Based on the Centers for Disease Control and Prevention (CDC) sexually transmitted diseases treatment guidelines, ivermectin is an effective and recommended alternative agent for the treatment of pediculosis pubis (pubic lice).
Mansonella ozzardi infectionb
Data from a double-blind, placebo-controlled study in patients with Mansonella ozzardi infections supports the use of ivermectin for the treatment of this condition Gonzales 1999. Additional trials may be necessary to further define the role of ivermectin in this condition.
Mansonella streptocerca infectionb
Data from a double-blind, placebo-controlled study in patients with Mansonella streptocerca infections supports the use of ivermectin for the treatment of this condition Fischer 1997. Additional trials may be necessary to further define the role of ivermectin in this condition.
Scabies, prevention and controlb
Data from a randomized population-based study support the use of oral ivermectin for scabies prevention and control Romani 2015. Additional trials may be necessary to further define the role of ivermectin in this condition.
Scabies, treatmentbyes
Data from an open-label study in patients with scabies due to Sarcoptes scabiei (with or without human immunodeficiency virus infection), support the use of ivermectin in the treatment of scabies Meinking 1995. Additional trials may be necessary to further define the role of ivermectin in this condition.
Based on the Centers for Disease Control and Prevention (CDC) sexually transmitted diseases treatment guidelines, ivermectin is an effective and recommended agent for the treatment of scabies. Scabies in adults is frequently sexually acquired as opposed to scabies in children which is usually not.
Trichuriasisb
Data from one clinical study in patients with strongyloidiasis and enterobiasis with concurrent intestinal infection due to Trichuris trichiura supports the use of ivermectin in this condition Naquira 1989. Additional trials may be necessary to further define the role of ivermectin in this condition.
Wucheria bancrofti infectionb
Data from a randomized controlled study in pediatric patients (aged 5 to 11 years) and a randomized study of male asymptomatic microflaraemic subjects with Wuchereria bancrofti infection supports the use of ivermectin for this condition Addiss 1997, Ismail 2001. Additional trials may be necessary to further define the role of ivermectin in this condition.
Contraindications
Hypersensitivity to ivermectin or any component of the formulation
Dosage and Administration
Dosing: Adult
Onchocerciasis: Oral: 150 mcg/kg as a single dose; retreatment may be required every 3 to 12 months until asymptomatic
Strongyloidiasis, intestinal: Oral: 200 mcg/kg/day for 1 to 2 days (CDC 2016)
Manufacturer's labeling: Dosing in the prescribing information may not reflect current clinical practice. 200 mcg/kg as a single dose
Ascariasis due to Ascaris lumbricoides (off-label use): Oral: 200 mcg/kg as a single dose (Marti 1996; Naquira 1989)
Demodicosis due to Demodex folliculorum and Demodex brevis (off-label use): Oral: 200 mcg/kg as a single dose, followed by topical permethrin (Eismann 2010) or 200 mcg/kg as 2 doses, 1 week apart (Salem 2013)
Gnathostomiasis due to Gnathostoma spinigerum (off-label use): Oral: 200 mcg/kg as a single dose (Kraivichian 2004; Nontasut 2000)
Hookworm-related cutaneous larva migrans (off-label use): Oral: 200 mcg/kg as a single dose; patients with hookworm folliculitis will require additional doses (Vanhaecke 2013)
Lice (off-label use): Oral: Note: Treatment generally requires >1 dose; number of doses and dosage intervals have not been established
Pediculus humanus capitis: Oral: 400 mcg/kg/dose every 7 days for 2 doses (Chosidow 2010)
Pediculus humanus corporis: Oral: 200 mcg/kg/dose every 7 days for 3 doses (Foucault 2006)
Pediculosis pubis (due to Phthirus pubis; pubic lice): Oral: 250 mcg/kg/dose every 7 days for 2 doses (Burkhart 2004) or 250 mcg/kg/dose every 14 days for 2 doses (CDC [Workowski 2015])
Mansonella ozzardi infection (off-label use): Oral: 6 mg as a single dose (Gonzales 1999)
Mansonella streptocerca infection (off-label use): Oral: 150 mcg/kg as a single dose (Fischer 1997)
Scabies due to Sarcoptes scabiei (off-label use):
Classic scabies, treatment-resistant or unable to tolerate topical medications, treatment: Oral: 200 mcg/kg as a single dose (CDC [Workowski 2015]; Meinking 1995); repeat dose in 7 to 14 days (CDC 2017; CDC [Workowski 2015])
Crusted scabies (Norwegian Scabies), treatment: Oral: 200 mcg/kg as a single dose on days 1, 2, 8, 9, and 15 in combination with topical permethrin 5% cream. Severe cases may require additional ivermectin treatment on days 22 and 29 (CDC 2017; CDC [Workowski 2015]).
Prevention and control: Oral: 200 mcg/kg as a single dose (Romani 2015)
Trichuriasis due to Trichuris trichiura (off-label use): Oral: 200 mcg/kg/day for 3 days (CDC 2013)
Wucheria bancrofti infection (off-label use): Oral: 200 to 400 mcg/kg as a single dose in combination with albendazole (Addiss 1997; Ismail 2001)
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Following the indication-specific dosing information are weight-band dosing tables to assist with calculation and rounding of doses.
Ascariasis due to Ascaris lumbricoides (roundworm): Limited data available: Children ≥15 kg and Adolescents: Oral: 150 to 200 mcg/kg/dose as a single dose (Red Book [AAP 2015])
Cutaneous larva migrans (dog and cat hookworm): Limited data available: Children ≥15 kg and Adolescents: Oral: 200 mcg/kg once daily for 1 to 2 days (Red Book [AAP 2015])
Filariasis:
Mansonella ozzardi: Limited data available: Children ≥15 kg and Adolescents: Oral: 200 mcg/kg/dose as a single dose (Red Book [AAP 2015])
Mansonella streptocerca: Limited data available: Children ≥15 kg and Adolescents: Oral: 150 mcg/kg/dose as a single dose (Red Book [AAP 2015])
Wuchereria bancrofti: Limited data available: Children ≥15 kg and Adolescents: Oral: 200 mcg/kg/dose as a single dose given in combination with albendazole (Red Book [AAP 2015])
Gnathostomiasis due to Gnathostoma spinigerum: Limited data available: Children ≥15 kg and Adolescents: Oral: 200 mcg/kg once daily for 2 days (Red Book [AAP 2015])
Onchocerciasis (Onchocerca volvulus, river blindness): Children ≥15 kg and Adolescents: Oral: 150 mcg/kg/dose as a single dose; may repeat every 6 to 12 months until asymptomatic; for prevention of blindness due to ocular onchocerciasis, doses repeated every 3 to 12 months are suggested (Red Book [AAP 2015])
Pediculosis (lice): Limited data available: Note: Ivermectin is not ovicidal; therefore, repeat doses are necessary to eradicate infestation:
Head lice: Children ≥15 kg and Adolescents: Oral: 400 mcg/kg/dose on days 1 and 8 (Chosidow 2010) or 200 mcg/kg/dose repeated once after 10 days (Jones 2003) have been shown to be effective (AAP [Devore 2015]; Red Book [AAP 2015])
Pubic lice: Children ≥15 kg and Adolescents: Oral: 250 mcg/kg/dose for 2 doses administered 14 days apart (CDC [Workowski 2015])
Scabies due to Sarcoptes scabiei: Limited data available: Children ≥15 kg and Adolescents: Oral: 200 mcg/kg/dose for 2 doses administered at least 7 days apart (Red Book [AAP 2015]); others suggest doses be separated by 14 days (CDC [Workowski 2015])
Strongyloidiasis: Children ≥15 kg and Adolescents: Oral: 200 mcg/kg once daily for 2 days (Red Book [AAP 2015]). Immunocompromised patients or patients with disseminated disease may need to repeat therapy.
Trichuriasis due to Trichuris trichiura (whipworm): Limited data available: Children ≥15 kg and Adolescents: Oral: 200 mcg/kg once daily for 3 days (Red Book [AAP 2015])
Weight-band dosing tables:
|
Patient Weight (kg) |
Single Oral Dose |
|---|---|
|
15 to 25 |
3 mg |
|
26 to 44 |
6 mg |
|
45 to 64 |
9 mg |
|
65 to 84 |
12 mg |
|
≥85 |
150 mcg/kg |
Table has been converted to the following text:
Weight-Band Dosing to Provide ~150 mcg/kg
Patient weight 15 to 25 kg: 3 mg as a single oral dose
Patient weight 26 to 44 kg: 6 mg as a single oral dose
Patient weight 45 to 64 kg: 9 mg as a single oral dose
Patient weight 65 to 84 kg: 12 mg as a single oral dose
Patient weight ≥85 kg: 150 mcg/kg as a single oral dose
|
Patient Weight (kg) |
Single Oral Dose |
|---|---|
|
15 to 24 |
3 mg |
|
25 to 35 |
6 mg |
|
36 to 50 |
9 mg |
|
51 to 65 |
12 mg |
|
66 to 79 |
15 mg |
|
≥80 |
200 mcg/kg |
Table has been converted to the following text:
Weight-Band Dosing to Provide ~200 mcg/kg
Patient weight 15 to 24 kg: 3 mg as a single oral dose
Patient weight 25 to 35 kg: 6 mg as a single oral dose
Patient weight 36 to 50 kg: 9 mg as a single oral dose
Patient weight 51 to 65 kg: 12 mg as a single oral dose
Patient weight 66 to 79 kg: 15 mg as a single oral dose
Patient weight ≥80 kg: 200 mcg/kg as a single oral dose
Administration
Oral: Administer on an empty stomach with water.
Pediculosis pubis and scabies treatment: To increase bioavailability in the epidermis, ivermectin is recommended to be taken with food (CDC [Workowski 2015]; Currie 2010).
Storage
Store at temperatures below 30°C (86°F).
Ivermectin (Systemic) Images
Drug Interactions
Azithromycin (Systemic): May increase the serum concentration of Ivermectin (Systemic). Monitor therapy
BCG (Intravesical): Antibiotics may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCG Vaccine (Immunization): Antibiotics may diminish the therapeutic effect of BCG Vaccine (Immunization). Monitor therapy
Cholera Vaccine: Antibiotics may diminish the therapeutic effect of Cholera Vaccine. Management: Avoid cholera vaccine in patients receiving systemic antibiotics, and within 14 days following the use of oral or parenteral antibiotics. Avoid combination
Erdafitinib: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Lactobacillus and Estriol: Antibiotics may diminish the therapeutic effect of Lactobacillus and Estriol. Monitor therapy
Lasmiditan: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Avoid combination
Lumacaftor and Ivacaftor: May decrease the serum concentration of P-glycoprotein/ABCB1 Substrates. Lumacaftor and Ivacaftor may increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
P-glycoprotein/ABCB1 Inducers: May decrease the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inducers may also further limit the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Monitor therapy
P-glycoprotein/ABCB1 Inhibitors: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inhibitors may also enhance the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Monitor therapy
Ranolazine: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Sodium Picosulfate: Antibiotics may diminish the therapeutic effect of Sodium Picosulfate. Management: Consider using an alternative product for bowel cleansing prior to a colonoscopy in patients who have recently used or are concurrently using an antibiotic. Consider therapy modification
Typhoid Vaccine: Antibiotics may diminish the therapeutic effect of Typhoid Vaccine. Only the live attenuated Ty21a strain is affected. Management: Vaccination with live attenuated typhoid vaccine (Ty21a) should be avoided in patients being treated with systemic antibacterial agents. Use of this vaccine should be postponed until at least 3 days after cessation of antibacterial agents. Consider therapy modification
Vitamin K Antagonists (eg, warfarin): Ivermectin (Systemic) may enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Adverse Reactions
>10%:
Dermatologic: Pruritus (3%; Mazzotti reaction, associated with onchocerciasis: 28%), dermatological reaction (Mazzotti reaction, associated with onchocerciasis: 23%; includes edema, urticarial rash)
Hematologic & oncologic: Lymphadenitis (Mazzotti reaction, associated with onchocerciasis: 1% to 14%)
Neuromuscular & skeletal: Arthralgia (Mazzotti reaction, associated with onchocerciasis: ≤9%), synovitis (Mazzotti reaction, associated with onchocerciasis: ≤9%)
Miscellaneous: Fever (Mazzotti reaction, associated with onchocerciasis: 23%)
1% to 10%:
Cardiovascular: Tachycardia (4%), peripheral edema (3%), facial edema (1%), orthostatic hypotension (1%)
Central nervous system: Dizziness (3%)
Gastrointestinal: Diarrhea (2%), nausea (2%)
Hematologic & oncologic: Eosinophilia (3%), decreased white blood cell count (3%), increased hemoglobin (1%)
Hepatic: Increased serum ALT (2%), increased serum AST (2%)
<1%, postmarketing, and/or case reports: Abdominal distention, abdominal pain, abnormal gait, abnormal sensation in eyes, anemia, anorexia, anterior uveitis, ataxia, back pain, brain disease (rare; associated with loiasis), chest discomfort, chorioretinitis, coma, confusion, conjunctival hemorrhage (associated with onchocerciasis), conjunctivitis, constipation, drowsiness, dyspnea, exacerbation of asthma, eye redness, eyelid edema, fatigue, fecal incontinence, headache, hepatitis, hypotension, increased serum bilirubin, keratitis, lethargy, leukopenia, mental status changes, myalgia, neck pain, posterior uveitis, seizure, skin rash, Stevens-Johnson syndrome, stupor, temporary vision loss, toxic epidermal necrolysis, tremor, urinary incontinence, urticaria, vertigo, vomiting, weakness
Warnings/Precautions
Concerns related to adverse effects:
- Cutaneous/systemic reactions: Data have shown that antihelmintic drugs like ivermectin may cause cutaneous and/or systemic reactions (Mazzoti reaction) of varying severity including ophthalmological reactions in patients with onchocerciasis. These reactions are probably due to allergic and inflammatory responses to the death of microfilariae. Patients treated with ivermectin for onchocerciasis may experience these reactions. Treatment of severe Mazzoti reactions is not definitive, but includes supportive care (eg, hydration and/or parenteral corticosteroids) to treat postural hypotension. Antihistamines and/or aspirin have been used for most mild to moderate reactions.
Disease-related concerns:
- Loiasis: Pretreatment assessment and post-treatment follow up for Loa loa infection is recommended in any patient with significant exposure to endemic areas (West and Central Africa); serious and/or fatal encephalopathy has been reported (rarely) during treatment in onchocerciasis patients with concomitant loiasis.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Immunocompromised patients: Repeated treatment may be required in immunocompromised patients (eg, HIV); control of extraintestinal strongyloidiasis may necessitate suppressive (once monthly) therapy.
Other warnings/precautions:
- Appropriate use: Onchocerca volvulus: Ivermectin has no activity against adult O. volvulus parasites.
Monitoring Parameters
Skin and eye microfilarial counts, periodic ophthalmologic exams; follow up stool examinations
Pregnancy
Pregnancy Considerations
Adverse events have been observed in animal reproduction studies. Although use in pregnancy is likely low risk, other agents are currently recommended for the treatment of pediculosis pubis or scabies in pregnant women (CDC [Workowski 2015]).
Patient Education
What is this drug used for?
- It is used to treat infections caused by worms.
Frequently reported side effects of this drug
- Itching
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Severe dizziness
- Passing out
- Vision changes
- Eye pain
- Severe eye irritation
- Severe skin irritation
- Joint pain
- Edema
- Enlarged lymph nodes
- Severe brain problems in patients with Loa-Loa infection (rare).
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.