Boxed Warning
Exacerbations of hepatitis B:
Severe acute exacerbations of hepatitis B have been reported in patients who are coinfected with hepatitis B virus (HBV) and HIV-1 and have discontinued lamivudine or discontinued anti-hepatitis B therapy (including lamivudine-HBV). Hepatic function should be monitored closely with both clinical and laboratory follow-up for at least several months in patients who discontinue lamivudine and are coinfected with HIV-1 and HBV or who discontinue anti-hepatitis B therapy. If appropriate, initiation of anti-HBV therapy may be warranted.
Important differences among lamivudine-containing products:
Lamivudine tablets and oral solution (used to treat HIV-1 infection) contain a higher dose of lamivudine than lamivudine-HBV tablets and oral solution (used to treat chronic hepatitis B infection). Patients with HIV-1 infection should receive only dosage forms appropriate for treatment of HIV-1.
Risk of HIV-1 resistance if lamivudine-HBV is used in patients with unrecognized or untreated HIV-1:
Lamivudine-HBV is not approved for the treatment of HIV-1 infection because the lamivudine dosage in lamivudine-HBV is subtherapeutic and monotherapy is inappropriate for the treatment of HIV-1 infection. HIV-1 resistance may emerge in chronic hepatitis B-infected patients with unrecognized or untreated HIV-1 infection. HIV counseling and testing should be offered to all patients before beginning treatment with lamivudine-HBV and periodically during treatment.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Solution, Oral:
Epivir: 10 mg/mL (240 mL) [contains methylparaben, propylene glycol, propylparaben; strawberry-banana flavor]
Epivir HBV: 5 mg/mL (240 mL) [contains methylparaben, propylene glycol, propylparaben; strawberry-banana flavor]
Generic: 10 mg/mL (240 mL)
Tablet, Oral:
Epivir: 150 mg [scored]
Epivir: 300 mg
Epivir HBV: 100 mg
Generic: 100 mg, 150 mg, 300 mg
Pharmacology
Mechanism of Action
Lamivudine is a cytosine analog. In vitro, lamivudine is triphosphorylated, the principle mode of action is inhibition of HIV reverse transcription via viral DNA chain termination; inhibits RNA- and DNA-dependent DNA polymerase activities of reverse transcriptase. In hepatitis B, the monophosphate form of lamivudine is incorporated into the viral DNA by hepatitis B virus polymerase, resulting in DNA chain termination.
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid
Distribution
Into extravascular spaces
Children (n=38): CSF concentrations were 14.2 ± 7.9% of the serum concentration
Vd: 1.3 ± 0.4 L/kg
Metabolism
Minor; only known metabolite is trans-sulfoxide metabolite
Excretion
Primarily urine (majority as unchanged drug); weight-corrected oral clearance is highest at age 2 years, then declines from age 2 to 12 years, where values then remain comparable to adult values
Time to Peak
Pediatric patients 0.5 to 17 years: Median: 1.5 hours (range: 0.5 to 4 hours) (Lewis 1996)
Adolescents 13 to 17 years: 0.5 to 1 hour
Adults: Fed: 3.2 hours; Fasted: 0.9 hours
Half-Life Elimination
Intracellular: 10 to 15 hours
Elimination:
Children 4 months to 14 years: 2 ± 0.6 hours
Adults: 5 to 7 hours; increased with renal impairment
Protein Binding
Plasma: <36%
Use in Specific Populations
Special Populations: Renal Function Impairment
AUC and Cmax are increased.
Use: Labeled Indications
Chronic hepatitis B (Epivir HBV): Treatment of chronic hepatitis B associated with evidence of hepatitis B viral replication and active liver inflammation
Limitations of use: Use only when an alternative antiviral agent with a higher genetic barrier to resistance is not available or appropriate. Lamivudine-HBV has not been evaluated in patients coinfected with HIV, hepatitis C virus, or hepatitis delta virus; with decompensated liver disease; or in liver transplant recipients.
HIV-1 infection, treatment (Epivir): Treatment of HIV-1 in combination with other antiretroviral agents
Use: Off Label
HIV-1 nonoccupational postexposure prophylaxisyes
Based on the Centers for Disease Control and Prevention, US Department of Health and Human Services updated guidelines for antiretroviral postexposure prophylaxis after sexual, injection drug use, or other nonoccupational exposure to HIV, lamivudine (in conjunction with other antiretrovirals) is an effective and recommended treatment option for postexposure prophylaxis of HIV-1 infection following nonoccupational exposure (nPEP) in individuals exposed to blood, genital secretions, or other potentially infectious body fluids that may contain HIV when that exposure represents a substantial risk for HIV transmission.
Prevention of perinatal HIV transmissionyes
Based on the Health and Human Services (HHS) Perinatal HIV Guidelines, lamivudine, in combination with zidovudine and nevirapine, is a recommended regimen for empiric therapy to reduce the risk of perinatal transmission of HIV in HIV-exposed infants at higher risk of HIV-acquisition, including those born to HIV-infected women who did not receive antepartum or intrapartum antiretroviral drugs (ARV), who received only intrapartum ARV drugs, or who received antepartum and intrapartum ARV drugs but had a detectable viral load near delivery (particularly if delivery was vaginal), or mothers with acute HIV infection during pregnancy or breastfeeding. Empiric therapy with this combination provides prophylaxis against HIV acquisition and provides early treatment if HIV infection is later confirmed.
Contraindications
Hypersensitivity to lamivudine or any component of the formulation
Dosage and Administration
Dosing: Adult
Note: The formulation and dosage of Epivir HBV are not appropriate for patients infected with both HBV and HIV; tenofovir and lamivudine are a preferred nucleoside reverse transcriptase inhibitor (NRTI) backbone in a fully suppressive antiretroviral regimen and for the treatment of HBV coinfection (HHS [adult] 2017).
HIV-1 infection, treatment (Epivir, 3TC [Canadian product]): Oral (use in combination with other antiretroviral agents): 150 mg twice daily or 300 mg once daily
Note: Lamivudine is a component of recommended initial regimens for any ART-naive patient (when coadministered with tenofovir plus dolutegravir or with tenofovir plus raltegravir) or for ART-naive patients who are HLA-B*5701 negative (when coadministered with abacavir plus dolutegravir) (HHS [adult] 2017).
HIV-1 nonoccupational postexposure prophylaxis (nPEP) (Epivir) (off-label use) (HHS [nPEP] 2016): Oral: Note: Initiate therapy within 72 hours of exposure and continue for 28 days; use in combination with other antiretroviral agents.
CrCl ≥60 mL/minute: Lamivudine is not a component of the recommended antiretroviral regimens for these patients.
CrCl <60 mL/minute: Dose should be adjusted based on renal function.
Treatment of hepatitis B (Epivir HBV, Heptovir [Canadian product]): Oral: 100 mg once daily
Treatment duration (AASLD practice guidelines): Treatment duration for nucleos(t)ide analog-based therapy (eg, lamivudine) is variable and influenced by HBeAg status, duration of HBV suppression, and presence of cirrhosis/decompensation (AASLD [Terrault 2016):
Patients without cirrhosis:
Hepatitis B e antigen (HBeAg) positive immune-active chronic hepatitis: Treat until HBeAg seroconversion; after seroconversion, prolonged duration of therapy is often required in patients treated with nucleos(t)ide analogues. Optimal duration is unknown; however, consolidation therapy is generally a minimum of 12 months of persistently normal ALT and undetectable serum HBV DNA levels after HBeAg seroconversion
HBeAg-negative immune-active chronic hepatitis: Indefinite antiviral therapy is suggested unless there is competing rationale for discontinuation (risk/benefit decision); treatment discontinuation may be considered in patients with loss of HBsAg; however, there is insufficient evidence to guide decisions in these patients.
Patients with cirrhosis:
HBeAg-positive immune-active chronic hepatitis: In patients who seroconvert on therapy, continue antiviral therapy indefinitely due to concerns with decompensation and death, unless there is a strong competing rationale for discontinuation.
HBeAg-negative immune-active chronic hepatitis: Treatment discontinuation is not recommended due to potential for decompensation and death (limited data).
Viral breakthrough (AASLD practice guidelines): Patients with confirmed viral breakthrough (HBV DNA ≥100 units/mL with previously undetectable levels [<10 units/mL] or >1 log increase in HBV DNA) should either be switched to an alternative antiviral monotherapy agent with a high genetic barrier to resistance or receive a second antiviral agent with a complementary resistance profile; consult current clinical practice guidelines for recommended agents (AASLD [Terrault 2016]).
Treatment of hepatitis B/HIV coinfection (in patients with both infections requiring treatment) (Epivir): Note: The formulation and dosage of Epivir HBV are not appropriate for patients infected with both HBV and HIV. Tenofovir and lamivudine are a preferred NRTI backbone in a fully suppressive antiretroviral regimen for the treatment of HIV/HBV coinfection (HHS [adult] 2017).
Oral: 150 mg twice daily or 300 mg once daily, in combination with other antiretrovirals in an antiretroviral (ARV) regimen (HHS [adult] 2017)
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Oral solution is available in 2 concentrations (10 mg/mL [eg, Epivir] and 5 mg/mL [Epivir-HBV]); use extra precaution during calculations to ensure accurate mg of lamivudine administered (HHS [pediatric] 2018). Gene mutation and antiretroviral resistance patterns should be evaluated (refer www.IASUSA.org for more information) when necessary.
HIV-1 infection, treatment: Use in combination with other antiretroviral agents: Oral:
Infants <3 months: Limited data available: Oral solution: 4 mg/kg/dose twice daily (HHS [pediatric] 2018; HHS [perinatal] 2018; Tremoulet 2007)
Infants ≥3 months to Children <3 years: Oral solution: 5 mg/kg/dose twice daily; maximum dose: 150 mg/dose (HHS [pediatric] 2018)
Children ≥3 years and Adolescents: Note: Scored tablet is preferred formulation in patients weighing ≥14 kg who are able to swallow a solid oral dosage form.
Twice-daily dosing:
Oral solution: 5 mg/kg/dose twice daily; maximum dose: 150 mg/dose
Oral tablet: Weight-band dosing for patients weighing ≥14 kg who are able to swallow tablets (using scored 150 mg tablets):
14 to <20 kg: 75 mg (1/2 tablet) twice daily
20 to <25 kg: 75 mg (1/2 tablet) in the morning and 150 mg (1 tablet) in the evening
≥25 kg: 150 mg (1 tablet) twice daily
Once-daily dosing: Note: Not recommended as initial therapy in children. Patients can be transitioned to once daily treatment with the oral solution or tablet after stable on twice-daily treatment for ≥36 weeks with an undetectable viral load and stable CD4 count (HHS [pediatric] 2018).
Oral solution: 10 mg/kg/dose once daily; maximum dose: 300 mg/dose
Oral tablet: Weight-band dosing for patients ≥14 kg who are able to swallow tablets (scored 150 mg tablets):
14 to <20 kg: 150 mg (1 tablet) once daily
20 to <25 kg: 225 mg (1 + 1/2 tablet) once daily
≥25 kg: 300 mg (2 tablets) once daily
HIV-1 nonoccupational postexposure prophylaxis (nPEP): Note: Initiate therapy within 72 hours of exposure and continue for 28 days in combination with other retroviral agents (HHS [nPEP] 2016): Oral:
Infants, Children, and Adolescents <16 years:
Weight-directed dosing: Oral solution: 4 mg/kg (maximum dose: 150 mg/dose) twice daily has been recommended (HHS [nPEP] 2016); however, based on newer pharmacokinetic data, a higher dose of 5 mg/kg/dose twice daily has been recommended for HIV treatment in patients ≥3 months of age (HHS [pediatric] 2018)
Weight-band dosing: Oral tablet: For patients ≥14 kg who are able to swallow tablets (scored 150 mg tablets):
14 to <20 kg: 75 mg (1/2 tablet) twice daily
20 to <25 kg: 75 mg (1/2 tablet) in the morning and 150 mg (1 tablet) in the evening
≥25 kg: 150 mg (1 tablet) twice daily
Adolescents ≥16 years: Oral solution or tablet:
<50 kg: 4 mg/kg twice daily; maximum dose: 150 mg/dose
≥50 kg: 150 mg twice daily or 300 mg once daily
HIV-1 perinatal transmission, empiric therapy in neonates at high risk of transmission (HHS [perinatal] 2018): Note: Dosing addresses completion of courses initiated at birth; if the neonate is diagnosed as HIV positive, discontinue empiric dosing and transition to a treatment regimen and monitoring (see HIV-1 infection, treatment). Recommended in combination with zidovudine and either raltegravir or nevirapine for empiric treatment of HIV in neonates at higher risk of perinatal transmission; see guidelines for additional information on high-risk definitions (HHS [perinatal] 2018). Duration of therapy undefined; some experts suggest a full 6 weeks of therapy, and others suggest that lamivudine can be discontinued once a negative nucleic acid test (NAT) is returned.
Three-drug combination (with zidovudine and either raltegravir or nevirapine): Limited data available: Infants ≤6 weeks: Oral: Oral solution: 4 mg/kg/dose every 12 hours to complete up to a total duration of lamivudine therapy of 6 weeks.
Hepatitis B, treatment (non-HIV-exposed/-positive): Note: Use in HBV treatment is discouraged due to rapid resistance development; consider use only if other anti-HBV antiviral regimens with more favorable resistance patterns cannot be used.
Epivir HBV: Children ≥2 years and Adolescents: Oral: 3 mg/kg/dose once daily; maximum daily dose: 100 mg/day
Heptovir [Canadian product]: Adolescents ≥16 years: Oral: 100 mg once daily
AASLD practice guidelines (Lok 2009): Treatment duration:
Hepatitis Be antigen (HBeAg) positive chronic hepatitis: Treat ≥1 year until HBeAg confirmed seroconversion and undetectable serum HBV DNA; continue therapy for ≥6 months after HBeAg seroconversion
HBeAg negative chronic hepatitis: Treat >1 year until hepatitis B surface antigen (HBsAg) clearance
Note: Patients not achieving <2 log decrease in serum HBV DNA after at least 6 months of therapy should either receive additional treatment or be switched to an alternative therapy (Lok 2009)
Hepatitis B/HIV coinfection, treatment of both infections: Infants, Children, and Adolescents: Dosing should be based on recommendations for treatment of HIV infection (higher dose) not hepatitis B, as part of an appropriate cART regimen (HHS [pediatric] 2018; HHS [OI pediatric] 2018).
Administration
Oral: May be administered without regard to meals.
Dietary Considerations
Some products may contain sucrose.
Storage
Oral solution:
Epivir: Store at 25°C (77°F) tightly closed.
Epivir HBV: Store at 20°C to 25°C (68°F to 77°F) tightly closed.
Tablet: Store at 25°C (77°F); excursions are permitted between 15°C and 30°C (59°F and 86°F).
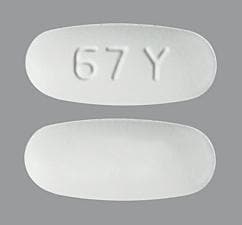
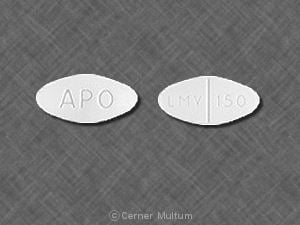
LamiVUDine Images
Drug Interactions
Cabozantinib: MRP2 Inhibitors may increase the serum concentration of Cabozantinib. Monitor therapy
Cladribine: Agents that Undergo Intracellular Phosphorylation may diminish the therapeutic effect of Cladribine. Avoid combination
Emtricitabine: LamiVUDine may enhance the adverse/toxic effect of Emtricitabine. Avoid combination
Orlistat: May decrease the serum concentration of Antiretroviral Agents. Monitor therapy
Sorbitol: May decrease the serum concentration of LamiVUDine. Management: When possible, avoid chronic coadministration of sorbitol-containing solutions with lamivudine, but if this combination cannot be avoided, monitor patients more closely for possible therapeutic failure associated with decreased lamivudine exposure. Consider therapy modification
Trimethoprim: May increase the serum concentration of LamiVUDine. Monitor therapy
Adverse Reactions
Incidence data include patients on combination therapy with other antiretroviral agents.
>10%:
Central nervous system: Headache (35%), fatigue (≤27%), malaise (≤27%), paresthesia (≤15%), peripheral neuropathy (≤15%), neuropathy (12%), insomnia (≤11%), sleep disorder (≤11%)
Dermatologic: Skin rash (9% to 12%)
Gastrointestinal: Nausea (≤33%), diarrhea (adults: 14% to 18%, children: 8%), pancreatitis (≤18%; higher percentage in pediatric patients), sore throat (13%), vomiting (≤13%)
Hematologic & oncologic: Neutropenia (7% to 15%)
Hepatic: Increased serum alanine aminotransferase (adults: 4% to 27%, children: 1%), hepatomegaly (children: 11%, adults: <1%)
Infection: infection (25%; includes ear, nose, and throat)
Neuromuscular & skeletal: Musculoskeletal pain (12%)
Respiratory: Nasal signs and symptoms (8% to 20%), cough (15% to 18%)
Miscellaneous: Fever (children: 25%, adults: ≤10%)
1% to 10%:
Central nervous system: Dizziness (10%), chills (≤10%), depression (9%)
Endocrine & metabolic: Increased amylase (2% to 4%)
Gastrointestinal: Increased serum lipase (adults: 10%, children: 3%), anorexia (≤10%), decreased appetite (≤10%), abdominal pain (9%), abdominal cramps (6%), stomatitis (children: 6%, adults: <1%), dyspepsia (5%)
Hematologic & oncologic: Lymphadenopathy (children: 9%), splenomegaly (children 5%, adults <1%), thrombocytopenia (adults: 4%, children: 1%), decreased hemoglobin (2% to 4%)
Hepatic: Increased serum aspartate aminotransferase (2% to 4%)
Neuromuscular & skeletal: Increased creatine phosphokinase (9%), myalgia (8%), arthralgia (5%)
Otic: Ear disease (children: 7%)
Respiratory: Abnormal breath sounds (children: ≤7%; adults: <1%), wheezing (children: ≤7%, adults: <1%)
<1%, postmarketing, and/or case reports: Alopecia, anaphylaxis, anemia, asthenia, cramps, exacerbation of hepatitis B, hyperbilirubinemia, hyperglycemia, immune reconstitution syndrome, lactic acidosis, liver steatosis, muscle cramps, myasthenia, pruritus, pure red cell aplasia, redistribution of body fat, rhabdomyolysis, urticaria
Warnings/Precautions
Concerns related to adverse effects:
- Immune reconstitution syndrome: Patients may develop immune reconstitution syndrome resulting in the occurrence of an inflammatory response to an indolent or residual opportunistic infection during initial HIV treatment or activation of autoimmune disorders (eg, Graves disease, polymyositis, Guillain-Barré syndrome) later in therapy; further evaluation and treatment may be required.
- Lactic acidosis/hepatomegaly: Lactic acidosis and severe hepatomegaly with steatosis have been reported with nucleoside analogues, including fatal cases; suspend treatment in any patient who develops clinical or laboratory findings suggestive of lactic acidosis or pronounced hepatotoxicity. Use with caution in patients with risk factors for liver disease (risk may be increased with female gender or obesity) and discontinue in any patient who develops clinical or laboratory findings suggestive of lactic acidosis or hepatotoxicity (transaminase elevation may/may not accompany hepatomegaly and steatosis).
- Pancreatitis: Has been reported, particularly in HIV-infected pediatric patients with a history of nucleoside use. Discontinue treatment if signs of symptoms of pancreatitis occur.
Disease-related concerns:
- Chronic hepatitis B: [US Boxed Warning]: Severe acute exacerbations of hepatitis B (some fatal) have been reported in patients with HBV or HIV/HBV coinfection who have discontinued lamivudine; hepatic function should be monitored closely with both clinical and laboratory follow-up for at least several months after discontinuation. Initiate antihepatitis B (HBV) medications if clinically appropriate.
- Renal impairment: Use with caution in patients with renal impairment; dosage reduction recommended.
- Resistance:
- HIV: [US Boxed Warning]: HIV-1 resistance may emerge in chronic hepatitis B-infection patients with unrecognized or untreated HIV-1 infection. Counseling and HIV testing should be offered to all patients before beginning treatment with lamivudine for hepatitis B and then periodically during treatment. Lamivudine dosing for hepatitis B is subtherapeutic if used for HIV-1 infection treatment. Lamivudine monotherapy is not appropriate for HIV-1 infection treatment. Lamivudine resistant HIV-1 can develop rapidly and limit treatment options if used in unrecognized or untreated HIV-1 infection or if a patient becomes coinfected during HBV treatment. Lamivudine dosing for hepatitis B is also subtherapeutic if used for HIV-1/HBV coinfection treatment. If lamivudine is chosen as part of a HIV-1 treatment regimen in coinfected patients, the higher lamivudine dosage indicated for HIV-1 therapy should be used, with other drugs, in an appropriate combination regimen.
- HBV: Patients treated with lamivudine-HBV with YMDD-mutant HBV showed diminished treatment response (lower rates of HBeAg seroconversion and HBeAg loss, more frequent return of positive HBV DNA, more frequent ALT elevations) compared to patients without evidence of YMDD substitutions. Emergence of lamivudine resistant HBV variants has also been reported in HIV-1/HBV coinfected patients who have received lamivudine-containing antiretroviral regimens.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Pediatric: Use with caution in pediatric patients with a history of prior antiretroviral nucleoside exposure or pancreatitis, or other significant risk factors for development of pancreatitis.
Dosage form specific issues:
- Appropriate product selection: Epivir HBV: [US Boxed Warning]: Do not use Epivir HBV tablets or Epivir HBV oral solution for the treatment of HIV.
- Oral solution: Use of lamivudine oral solution has been associated with lower rates of virologic suppression, lower plasma lamivudine exposure, and increased rates of resistance when compared to lamivudine tablets in pediatric clinical trials. Lamivudine scored tablet is the preferred formulation for HIV-1 infected pediatric patients weighing ≥14 kg and for whom a solid dosage form is appropriate; consider more frequent monitoring of HIV-1 viral load if oral solution is used.
- Sucrose: Lamivudine oral solutions contains 3 g of sucrose/15 mL; advise diabetic patients of sucrose content.
- Propylene glycol: Some dosage forms may contain propylene glycol; large amounts are potentially toxic and have been associated hyperosmolality, lactic acidosis, seizures and respiratory depression; use caution (AAP 1997; Zar 2007).
Other warnings/precautions:
- Appropriate use:
-HIV: Do not use as monotherapy in treatment of HIV. Treatment of HIV in patients with unrecognized/untreated HBV may lead to rapid HBV resistance; HIV-infected patients should be screened for hepatitis B prior to starting lamivudine HIV therapy. Lamivudine combined with emtricitabine is not recommended as a dual-nucleoside reverse transcriptase inhibitor (NRTI) combination due to similar resistance patterns and negligible additive antiviral activity. Do not use lamivudine/abacavir (plus efavirenz or plus atazanavir/ritonavir) in adolescent and adult HIV-1 patients with a pre-ART HIV RNA >100,000 copies/mL (HHS [adult] 2017).
- HBV: Current clinical hepatitis B practice guidelines do not recommend lamivudine for initial use in the management of chronic HBV due to low barrier to resistance; other antiviral agents with a high genetic barrier to drug resistance are preferred (eg, tenofovir or entecavir) (AASLD [Terrault 2016]).
- HIV/HBV coinfection: Lamivudine and tenofovir is a recommended NRTI backbone in a fully suppressive antiretroviral regimen to provide activity against both HIV and HBV (HHS [adult] 2017).
Monitoring Parameters
Manufacturer’s labeling:
All patients: Hepatic function, signs/symptoms of lactic acidosis; signs/symptoms of pancreatitis
HIV patients: Coinfection with HBV (prior to therapy); HIV viral load and CD4 count; immune reconstitution syndrome
Hepatitis B patients: Coinfection with HIV (prior to therapy); following discontinuation, monitor hepatic function closely with both clinical and laboratory follow/up for signs/symptoms of HBV relapse/exacerbation (continue for at least several months after stopping treatment)
Alternate recommendations:
Chronic Hepatitis B: HBV DNA and ALT (HBV DNA usually done every 3 months until undetectable and then every 3 to 6 months thereafter); HBeAg; anti-HBe (in patients who are HBeAg-positive to monitor for seroconversion); HBsAg; during therapy, consider monitoring amylase (if symptoms of pancreatitis) and lactic acid levels (if clinical concern); following discontinuation, monitor for recurrent viremia, ALT flares, seroreversion, and clinical decompensation every 3 months for at least 1 year (AASLD [Terrault 2016]). As antivirals do not eliminate the risk of hepatocellular carcinoma, continued monitoring for this complication is recommended in at-risk patients.
Pregnancy
Pregnancy Considerations
Lamivudine has a high level of transfer across the human placenta.
No increased risk of overall birth defects has been observed following first trimester exposure according to data collected by the antiretroviral pregnancy registry. Maternal antiretroviral therapy (ART) may be associated with adverse pregnancy outcomes, including preterm delivery, stillbirth, low birth weight, and small for gestational age infants. Actual risks may be influenced by maternal factors such as disease severity, gestational age at initiation of therapy, and specific ART regimen; therefore, close fetal monitoring is recommended. Based on data collected by the antiretroviral pregnancy registry, the risk of spontaneous abortions, induced abortions, and preterm birth is less in lamivudine-containing regimens compared with regimens without lamivudine. Because there is clear benefit to appropriate treatment, maternal ART should not be withheld due to concerns for adverse neonatal outcomes. Long-term follow-up is recommended for all infants exposed to antiretroviral medications; children without HIV but who were exposed to ART in utero and develop significant organ system abnormalities of unknown etiology (particularly of the CNS or heart) should be evaluated for potential mitochondrial dysfunction. Cases of lactic acidosis and hepatic steatosis have been reported in pregnant women with use of nucleoside reverse transcriptase inhibitors (NRTIs).
The Health and Human Services (HHS) perinatal HIV guidelines consider lamivudine a preferred NRTI for pregnant females living with HIV who are antiretroviral-naive, who have had ART therapy in the past but are restarting, who require a new ART regimen (due to poor tolerance or poor virologic response of current regimen), and who are not yet pregnant but are trying to conceive. In addition, females who become pregnant while taking lamivudine may continue if viral suppression is effective and the regimen is well tolerated. The pharmacokinetics of lamivudine during pregnancy are not significantly altered, and dosage adjustment is not required.
The HHS perinatal HIV guidelines consider lamivudine in combination with either abacavir or tenofovir disoproxil fumarate to be a preferred NRTI backbone for initial therapy in antiretroviral-naive pregnant females. The lamivudine/abacavir backbone is not recommended with atazanavir/ritonavir or efavirenz if pretreatment HIV RNA is >100,000 copies/mL. In addition, the HHS perinatal HIV guidelines consider lamivudine in combination with abacavir and dolutegravir to be a preferred INSTI regimen for initial therapy in antiretroviral-naive pregnant females. The guidelines consider lamivudine with zidovudine to be an alternative NRTI backbone for initial therapy in antiretroviral-naive pregnant females. The guidelines also consider lamivudine plus tenofovir disoproxil fumarate a recommended dual NRTI backbone in regimens for HIV/hepatitis B virus (HBV)-coinfected pregnant females. Use caution with hepatitis B coinfection; hepatitis B flare may occur if lamivudine is discontinued.
In general, ART is recommended for all pregnant females living with HIV to keep the viral load below the limit of detection and reduce the risk of perinatal transmission. Therapy should be individualized following a discussion of the potential risks and benefits of treatment during pregnancy. Monitoring of pregnant females is more frequent than in nonpregnant adults. ART should be continued postpartum for all females living with HIV and can be modified after delivery.
In hepatitis B-infected women (not coinfected with HIV), the American Association for the Study of Liver Diseases (AASLD) chronic hepatitis B treatment guidelines suggest antiviral therapy to reduce the risk of perinatal transmission of hepatitis B in HBsAg-positive pregnant women with an HBV DNA >200,000 units/mL. There are limited data on the level of HBV DNA for when antiviral therapy is routinely recommended (>200,000 units/mL is a conservative recommendation); however, the AASLD recommends against antiviral therapy to reduce the risk of perinatal transmission in HBsAg-positive pregnant women with an HBV DNA ≤200,000 units/mL. Lamivudine is one of the antivirals that has been studied in pregnant women, with most studies initiating antiviral therapy at 28 to 32 weeks gestation and discontinuing antiviral therapy between birth to 3 months postpartum (monitor for ALT flares every 3 months for 6 months following discontinuation). There are insufficient long-term safety data in infants born to mothers who took antiviral agents during pregnancy (AASLD [Terrault 2016]).
Health care providers are encouraged to enroll pregnant females exposed to antiretroviral medications as early in pregnancy as possible in the Antiretroviral Pregnancy Registry (1-800-258-4263 or http://www.APRegistry.com). Health care providers caring for pregnant females living with HIV and their infants may contact the National Perinatal HIV Hotline (888-448-8765) for clinical consultation (HHS [perinatal] 2019).
Patient Education
What is this drug used for?
- It is used to treat hepatitis B infection.
- It is used to treat HIV infection.
Frequently reported side effects of this drug
- Headache
- Nausea
- Diarrhea
- Loss of strength and energy
- Stuffy nose
- Dizziness
- Sore throat
- Ear irritation
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Lactic acidosis like fast breathing, fast heartbeat, abnormal heartbeat, vomiting, fatigue, shortness of breath, severe loss of strength and energy, severe dizziness, feeling cold, or muscle pain or cramps.
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Pancreatitis like severe abdominal pain, severe back pain, severe nausea, or vomiting.
- Depression
- Burning or numbness feeling
- Infection
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.