Boxed Warning
Monitoring:
Lithium toxicity is closely related to serum lithium levels, and can occur at doses close to therapeutic levels. Facilities for prompt and accurate serum lithium determinations should be available before initiating therapy.
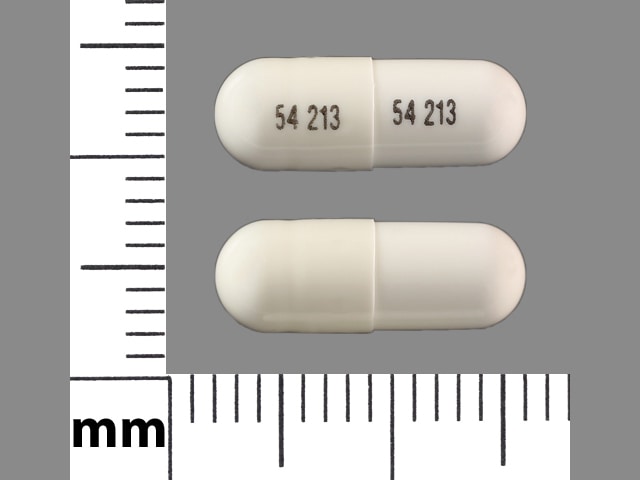
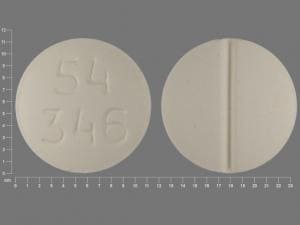
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Capsule, Oral, as carbonate:
Generic: 150 mg, 300 mg, 600 mg
Solution, Oral, as citrate:
Generic: 8 mEq/5 mL (5 mL [DSC], 500 mL)
Tablet, Oral, as carbonate:
Generic: 300 mg
Tablet Extended Release, Oral, as carbonate:
Lithobid: 300 mg [contains fd&c blue #2 aluminum lake, fd&c red #40 aluminum lake, fd&c yellow #6 aluminum lake]
Generic: 300 mg, 450 mg
Pharmacology
Mechanism of Action
The precise mechanism of action in mood disorders is unknown. Traditionally thought to alter cation transport across cell membranes in nerve and muscle cells, influence the reuptake of serotonin and/or norepinephrine, and inhibit second messenger systems involving the phosphatidylinositol cycle (Ward 1994). May also provide neuroprotective effects by increasing glutamate clearance, inhibiting apoptotic glycogen synthase kinase activity, increasing the levels of antiapoptotic protein Bcl-2 and, enhancing the expression of neurotropic factors, including brain-derived neurotrophic factor (Sanacora 2008).
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid and complete
Distribution
Vd: Initial: 0.307 L/kg; Vdss: 0.7 to 1 L/kg; decreased in elderly patients (Ward 1994)
Metabolism
Not metabolized (Ward 1994)
Excretion
Urine (primarily; unchanged drug); sweat, saliva and feces (negligible amounts)
Clearance: 80% of filtered lithium is reabsorbed in the proximal convoluted tubules; decreased in elderly patients secondary to age-related decreases in renal function (Ward 1994)
Time to Peak
Serum: Nonsustained release: ~0.5 to 3 hours; Extended release: 2 to 6 hours; Solution: 15 to 60 minutes (Ward 1994)
Half-Life Elimination
Pediatric patients 7 to 17 years: t1/2 (beta): 27 hours (Findling 2010)
Adults: 18 to 36 hours; prolonged in elderly patients (28.5 hours) (Ward 1994)
Protein Binding
Not protein bound (Ward 1994)
Use in Specific Populations
Special Populations: Elderly
Elderly patients receiving lithium may have a decreased glomerular filtration rate and decrease in renal plasma clearance (13.7 mL/minute) (Ward 1994).
Special Populations: Children
In pediatric patients, great variability in clearance was found across subjects with linear pharmacokinetics correlated to fat-free mass (Findling 2010).
Use: Labeled Indications
Bipolar disorder: Treatment of manic episodes and maintenance treatment in patients ≥7 years of age with a diagnosis of bipolar disorder
Use: Off Label
Bipolar depressionyes
Based on the American Psychiatric Association (APA) practice guideline for the treatment of patients with bipolar disorder, the World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the biological treatment of bipolar disorders, and the Canadian Network for Mood and Anxiety Treatments (CANMAT)/International Society for Bipolar Disorders (ISBD) guidelines for the management of patients with bipolar disorder, lithium given for bipolar depression is effective and recommended for acute and maintenance treatment of this condition.
Depression, augmentation of antidepressantb
Data from a meta-analysis of 9 randomized, controlled trials support antidepressant augmentation with lithium in the treatment of depression Nelson 2014. Additional trials may be necessary to further define the role of lithium in this condition.
Headache, cluster (episodic and chronic, prevention)cyes
Data from a randomized, double-blind, active comparator crossover study suggest that lithium may be beneficial for decreasing headache severity and analgesic consumption when used prophylactically in patients with chronic cluster headaches Bussone 1990. Data from a limited number of patients in other studies suggest that lithium may be beneficial for decreasing headache severity and duration when used prophylactically in patients with episodic or chronic cluster headaches Ekbom 1981, Kudrow 1977, Mathew 1978.
Based on the American Headache Society (AHS) evidence-based guidelines for the treatment of cluster headache, lithium is possibly effective and may be considered as an alternative to first-line options for headache prophylaxis in patients with cluster headaches AHS [Robbins 2016] .
Contraindications
Hypersensitivity to lithium or any component of the formulation
Immediate-release capsule, solution and tablet: Severe cardiovascular or renal disease, severe debilitation, dehydration, sodium depletion, concurrent use with diuretics
Dosage and Administration
Dosing: Adult
Note: Monitor serum concentrations and clinical response (efficacy and toxicity) to determine proper dose. Each 5 mL of lithium citrate oral solution contains 8 mEq of lithium ion, equivalent to the amount of lithium in 300 mg of lithium carbonate immediate release capsules/tablets. When tolerated, lithium dosage may be consolidated to a single dose given at bedtime (APA 2002; Carter 2013; Grandjean 2009).
Bipolar disorder:
Acute manic episodes or bipolar major depression (off-label use) (monotherapy or adjunctive therapy): Oral: Initial: 600 to 900 mg/day in 2 to 3 divided doses; may increase gradually (eg, 300 to 600 mg every 1 to 5 days) based on response and tolerability; usual dosage: 900 to 1,800 mg/day in 1 to 3 divided doses (Janicak 2018; WFSBP [Grunze 2009]; WFSBP [Grunze 2010])
Maintenance treatment to prevent manic or depressed episodes (monotherapy or adjunctive therapy) (off-label use): Oral: Continue dose and combination regimen that was used to achieve control of the acute episode (CANMAT [Yatham 2018]).
Depression, augmentation of antidepressant (off-label use): Oral: Initial: Initiate at a low dose (eg, 300 mg once daily or 300 mg twice daily); increase gradually based on response and tolerability; usual dosage: 600 to 1200 mg daily in divided doses (Bauer 2003a; Bauer 2003b; Nelson 2014)
Headache, cluster (episodic and chronic, prevention) (alternative agent) (off-label use): Oral: Initial: 300 to 900 mg/day in 1 to 3 divided doses; may increase gradually in 300 to 600 mg increments every 1 to 7 days based on response and tolerability; doses up to 1.2 g/day have been studied (AHS [Robbins 2016]; Bussone 1990; Kudrow 1977; Manzoni 1983; Mathew 1978).
Dosing: Geriatric
Bipolar disorder (acute mania, acute depression [off-label use], and maintenance): Initiate therapy with lower doses; refer to adult dosing.
Dosing: Pediatric
Note: Monitor serum concentrations and clinical response (efficacy and toxicity) to determine proper dose. Each 5 mL of lithium oral solution contains 8 mEq of lithium ion, equivalent to the amount of lithium in 300 mg of lithium carbonate immediate-release capsules/tablets.
Bipolar disorder: Oral:
Immediate release: Children ≥7 years and Adolescents: Limited data available in weight <20 kg: Note: Dosing in weight <20 kg extrapolated from clinical experience (Kliegman 2007).
Lithium carbonate capsule or tablet:
Patient weight <30 kg: Initial: 300 mg twice daily, increase dose at weekly intervals in 300 mg/day increments as tolerated to clinical response and goals based on type of therapy (acute or maintenance).
Acute therapy: Titrate dose to 600 to 1,500 mg/day in divided doses and target serum lithium concentration of 0.8 to 1.2 mEq/L; a maximum dose is not described in the manufacturer labeling; in trials, weight-dependent maximum daily doses were reported: Patients <23 kg: 900 mg/day; patients ≥23 kg: 40 mg/kg/day and doses were not further increased if serum lithium concentration was ≥1.4 mEq/L. In a multicenter, double-blind, placebo-controlled efficacy trial for treatment of acute mania, the mean effective daily dose was 956 ± 225 mg/day. For all patients in the trial (regardless of weight) the mean final dose was: 30.5 ± 8.7 mg/kg/day (Findling 2011; Findling 2013; Findling 2015).
Maintenance therapy: Titrate dose to 600 to 1,200 mg/day in divided doses and target serum trough concentration of 0.8 to 1 mEq/L as tolerated.
Patient weight ≥30 kg: Initial: 300 mg 3 times daily, increase dose in 300 mg/day increments every 3 days as tolerated to clinical response and goals based on type of therapy (acute or maintenance).
Acute therapy: Titrate dose to 600 mg twice or 3 times daily and target serum lithium concentration of 0.8 to 1.2 mEq/L; a maximum dose is not described in the manufacturer labeling; in trials, reported doses did not exceed a maximum daily dose of 40 mg/kg/day and doses were not further increased if serum lithium concentration was ≥1.4 mEq/L. In a multicenter, double-blind, placebo-controlled efficacy trial for treatment of acute mania, the mean effective daily dose was 1,583 ± 524 mg/day. For all patients in the trial (regardless of weight) the mean final dose was 30.5 ± 8.7 mg/kg/day (Findling 2011; Findling 2013; Findling 2015).
Maintenance therapy: Titrate dose to 300 to 600 mg twice or 3 times daily and target serum trough concentration of 0.8 to 1 mEq/L as tolerated; in a long-term trial, doses were not further increased if serum lithium concentration was ≥1.4 mEq/L (Findling 2013).
Lithium oral solution:
Patient weight <30 kg: Initial: 8 mEq twice daily, increase dose at weekly intervals in 8 mEq increments as tolerated to clinical response and goals based on type of therapy (acute or maintenance).
Acute therapy: Titrate dose to 16 to 40 mEq/day in divided doses and target serum lithium concentration of 0.8 to 1.2 mEq/L; a maximum dose is not described in the manufacturer labeling; in trials, weight-dependent maximum daily doses were reported: Patients <23 kg: 900 mg of lithium carbonate/day; patients ≥23 kg: 40 mg of lithium carbonate/kg/day and doses were not further increased if serum lithium concentration was ≥1.4 mEq/L (Findling 2011; Findling 2013; Findling 2015).
Maintenance therapy: Titrate dose to 16 to 32 mEq/day in divided doses and target serum trough concentration of 0.8 to 1 mEq/L as tolerated and doses were not further increased if serum lithium concentration was ≥1.4 mEq/L (Findling 2011; Findling 2013; Findling 2015).
Patient weight ≥30 kg: Initial: 8 mEq 3 times daily, increase dose in 8 mEq increments every 3 days as tolerated to clinical response and goals based on type of therapy (acute or maintenance).
Acute therapy: Titrate dose to 16 mEq twice or 3 times daily and target serum lithium concentration of 0.8 to 1.2 mEq/L; maximum doses are not described in the manufacturer labeling; in trials, reported doses did not exceed a maximum daily dose of: 40 mg of lithium carbonate/kg/day and doses were not further increased if serum lithium concentration was ≥1.4 mEq/L (Findling 2011; Findling 2013; Findling 2015).
Maintenance therapy: Titrate dose to 8 to 16 mEq twice or 3 times daily and target serum trough concentration of 0.8 to 1 mEq/L as tolerated; in a long-term trial, doses were not further increased if serum lithium concentration was ≥1.4 mEq/L (Findling 2013).
Extended release: Children ≥12 years and Adolescents: Weight-based usual daily dosing administered in 2 divided doses: <22 kg: 600 mg/day; 22 to 41 kg: 900 mg/day, and >41 kg: 1,200 mg/day (Kliegman 2016). In an open-label trial of 27 subjects (age range: 12 to 18 years), an initial dose of 15 mg/kg/dose twice daily, maximum initial dose: 600 mg/dose, with dose titration at weekly intervals as tolerated to target serum lithium concentration of 1 to 1.2 mEq/L was used (Patel 2006). In adults, therapy is initiated at a low dose (eg, 450 mg 2 times daily or less); increased gradually based on response and tolerability (APA 2002); the usual adult dosage is 900 to 1,800 mg/day in 2 divided doses.
Administration
Oral: Administer with meals to decrease GI upset. Extended release tablets must be swallowed whole; do not crush or chew.
Dietary Considerations
May be taken with meals to avoid GI upset; maintain adequate salt and fluid intake.
Storage
Store between 15°C and 30°C (59°F to 86°F). Protect tablets and capsules from moisture.
Lithium Images
Drug Interactions
Almotriptan: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Alosetron: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Amphetamines: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Angiotensin II Receptor Blockers: May increase the serum concentration of Lithium. Management: Lithium dosage reductions will likely be needed following the addition of an angiotensin II receptor antagonist. Consider therapy modification
Angiotensin-Converting Enzyme Inhibitors: May increase the serum concentration of Lithium. Management: Lithium dosage reductions will likely be needed following the addition of an ACE inhibitor. Monitor patient response to lithium closely following addition or discontinuation of concurrent ACE inhibitor treatment. Consider therapy modification
Antiemetics (5HT3 Antagonists): May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Exceptions: Alosetron; Ondansetron; Ramosetron. Monitor therapy
Antipsychotic Agents: Lithium may enhance the neurotoxic effect of Antipsychotic Agents. Lithium may decrease the serum concentration of Antipsychotic Agents. Specifically noted with chlorpromazine. Monitor therapy
BusPIRone: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Caffeine and Caffeine Containing Products: May decrease the serum concentration of Lithium. Monitor therapy
Calcitonin: May decrease the serum concentration of Lithium. Monitor therapy
Calcium Channel Blockers (Nondihydropyridine): May enhance the neurotoxic effect of Lithium. Calcium Channel Blockers (Nondihydropyridine) may increase the serum concentration of Lithium. Decreased or unaltered lithium concentrations have also been reported with this combination. Exceptions: Bepridil. Monitor therapy
Calcium Polystyrene Sulfonate: May decrease the serum concentration of Lithium. Management: Consider separating administration of lithium from administration of oral calcium polystyrene sulfonate by at least 6 hours. Consider therapy modification
CarBAMazepine: May enhance the adverse/toxic effect of Lithium. Monitor therapy
Carbonic Anhydrase Inhibitors: May decrease the serum concentration of Lithium. Exceptions: Brinzolamide; Dorzolamide. Monitor therapy
Cyclobenzaprine: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Dapoxetine: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Do not use serotonergic agents (high risk) with dapoxetine or within 7 days of serotonergic agent discontinuation. Do not use dapoxetine within 14 days of monoamine oxidase inhibitor use. Dapoxetine labeling lists this combination as contraindicated. Avoid combination
Desmopressin: Lithium may diminish the therapeutic effect of Desmopressin. Desmopressin may increase the serum concentration of Lithium. Monitor therapy
Dexmethylphenidate-Methylphenidate: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Dextromethorphan: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Eletriptan: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Eplerenone: May increase the serum concentration of Lithium. Monitor therapy
Ergot Derivatives: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Exceptions: Nicergoline. Monitor therapy
Fexinidazole [INT]: Lithium may enhance the QTc-prolonging effect of Fexinidazole [INT]. Avoid combination
Fosphenytoin: May enhance the adverse/toxic effect of Lithium. Monitor therapy
Haloperidol: QT-prolonging Agents (Indeterminate Risk - Caution) may enhance the QTc-prolonging effect of Haloperidol. Monitor therapy
Lasmiditan: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Linezolid: May enhance the serotonergic effect of Lithium. This could result in serotonin syndrome. Management: Consider alternatives to this drug combination. If combined, monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes). Consider therapy modification
Loop Diuretics: May decrease the serum concentration of Lithium. Loop Diuretics may increase the serum concentration of Lithium. Monitor therapy
Lorcaserin: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Metaxalone: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Methyldopa: May enhance the adverse/toxic effect of Lithium. This may occur without notable changes in serum lithium concentrations. Monitor therapy
Methylene Blue: May enhance the serotonergic effect of Lithium. This could result in serotonin syndrome. Management: Consider alternatives to this drug combination. If combined, monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes). Consider therapy modification
MetroNIDAZOLE (Systemic): May enhance the adverse/toxic effect of Lithium. MetroNIDAZOLE (Systemic) may increase the serum concentration of Lithium. Monitor therapy
Monoamine Oxidase Inhibitors (Antidepressant): May enhance the serotonergic effect of Lithium. This could result in serotonin syndrome. Management: Consider alternatives to this drug combination. If combined, monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes). Consider therapy modification
Monoamine Oxidase Inhibitors (Type B): May enhance the serotonergic effect of Serotonergic Agents (High Risk, Miscellaneous). This could result in serotonin syndrome. Avoid combination
Nefazodone: May enhance the serotonergic effect of Serotonergic Agents (High Risk, Miscellaneous). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Neuromuscular-Blocking Agents: Lithium may enhance the neuromuscular-blocking effect of Neuromuscular-Blocking Agents. Monitor therapy
Nonsteroidal Anti-Inflammatory Agents: May increase the serum concentration of Lithium. Exceptions: Sulindac. Consider therapy modification
Ondansetron: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Opioid Agonists: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Exceptions: FentaNYL; Meperidine; TraMADol. Monitor therapy
Oxitriptan: Serotonergic Agents (High Risk) may enhance the serotonergic effect of Oxitriptan. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Phenytoin: May enhance the adverse/toxic effect of Lithium. Monitor therapy
Potassium Iodate: Lithium may enhance the hypothyroid effect of Potassium Iodate. Monitor therapy
Potassium Iodide: May enhance the hypothyroid effect of Lithium. Monitor therapy
QT-prolonging Agents (Highest Risk): QT-prolonging Agents (Indeterminate Risk - Caution) may enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Ramosetron: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Sargramostim: May enhance the adverse/toxic effect of Lithium. Specifically, the myeloproliferative effects may be increased. Monitor therapy
Selective Serotonin Reuptake Inhibitors: Serotonergic Agents (High Risk, Miscellaneous) may enhance the serotonergic effect of Selective Serotonin Reuptake Inhibitors. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Exceptions: Dapoxetine. Monitor therapy
Serotonergic Non-Opioid CNS Depressants: Serotonergic Agents (High Risk, Miscellaneous) may enhance the serotonergic effect of Serotonergic Non-Opioid CNS Depressants. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Serotonergic Opioids (High Risk): May enhance the serotonergic effect of Serotonergic Agents (High Risk, Miscellaneous). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) if these agents are combined. Monitor therapy
Serotonin 5-HT1D Receptor Agonists (Triptans): May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Exceptions: Almotriptan; Eletriptan. Monitor therapy
Serotonin/Norepinephrine Reuptake Inhibitors: May enhance the serotonergic effect of Serotonergic Agents (High Risk, Miscellaneous). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Sodium Bicarbonate: May increase the excretion of Lithium. Monitor therapy
Sodium Chloride: May increase the excretion of Lithium. Monitor therapy
Sodium Polystyrene Sulfonate: May decrease the serum concentration of Lithium. Management: Consider separating administration of lithium from administration of oral sodium polystyrene sulfonate by at least 6 hours. Consider therapy modification
St John's Wort: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. St John's Wort may decrease the serum concentration of Serotonergic Agents (High Risk). Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Syrian Rue: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Theophylline Derivatives: May decrease the serum concentration of Lithium. Monitor therapy
Thiazide and Thiazide-Like Diuretics: May decrease the excretion of Lithium. Consider therapy modification
Topiramate: May increase the serum concentration of Lithium. Monitor therapy
Tricyclic Antidepressants: May enhance the serotonergic effect of Serotonergic Agents (High Risk, Miscellaneous). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Tryptophan: Lithium may enhance the serotonergic effect of Tryptophan. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Adverse Reactions
Frequency not always defined.
Cardiovascular: Abnormal T waves on ECG, bradycardia, cardiac arrhythmia, chest tightness, circulatory shock, cold extremities, edema, hypotension, myxedema, sinus node dysfunction, startled response, syncope
Dermatologic: Acne vulgaris, alopecia, blue-gray skin pigmentation, dermal ulcer, dry or thinning of hair, exacerbation of psoriasis, folliculitis, pruritus, psoriasis, skin rash, xerosis
Endocrine & metabolic: Hypothyroidism (females 14%; males 5% [Johnston 1999]; children and adolescents: <1% [Findling 2015]), albuminuria, dehydration, diabetes insipidus, euthyroid goiter, glycosuria, hypercalcemia (secondary to hyperparathyroidism [McKnight 2012]), hyperglycemia, hyperparathyroidism, hyperthyroidism, increased radioactive iodine uptake, increased thirst, polydipsia, weight gain, weight loss
Gastrointestinal: Abdominal pain, anorexia, dental caries, diarrhea, dysgeusia, dyspepsia, excessive salivation, flatulence, gastritis, nausea, vomiting, sialadenitis, sialorrhea, swelling of lips, xerostomia
Genitourinary: Impotence, incontinence, oliguria
Hematologic & oncologic: Leukocytosis
Hypersensitivity: Angioedema
Nervous system: Ataxia, blackout spells, cogwheel rigidity, coma, confusion, dizziness, drowsiness, dystonia, EEG pattern changes, extrapyramidal reaction, fatigue, hallucination, headache, hyperactive deep tendon reflex, hypertonia, involuntary choreoathetoid movements, lethargy, local anesthesia, memory impairment, loss of consciousness, metallic taste, myasthenia gravis (rare), pseudotumor cerebri, psychomotor retardation, reduced intellectual ability, restlessness, salty taste, sedation, seizure, slowed intellectual functioning, slurred speech, stupor, tics, vertigo, worsening of organic brain syndromes
Neuromuscular & skeletal: Joint swelling, muscle hyperirritability, neuromuscular excitability, polyarthralgia, tremor
Ophthalmic: Blurred vision, exophthalmos, nystagmus, transient scotoma
Otic: Tinnitus
Renal: Decreased creatinine clearance, polyuria
Miscellaneous: Fever
Postmarketing: Intracranial hypertension (Tan 2019), lupus-like syndrome (Shukla 1982)
Warnings/Precautions
Concerns related to adverse effects:
- CNS depression: May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks that require mental alertness (eg, operating machinery, driving).
- Heart failure: In a scientific statement from the American Heart Association, lithium has been determined to be an agent that may cause direct myocardial toxicity that is reversible upon discontinuation (magnitude: major) (AHA [Page 2016]).
- Hypercalcemia: Hypercalcemia with or without hyperparathyroidism has been reported. Risks are greater in women and possibly in older patients; symptom onset does not appear to be related to therapy duration (Lehmann 2013). Serum calcium levels typically range from slightly above normal to over 15 mg/dL and PTH levels may range from high normal to several times the upper limit of normal (Lehmann 2013); magnesium levels are often elevated; serum phosphate levels may be either normal or low (Grandjean 2009). Monitor calcium and PTH levels as clinically indicated. Consider discontinuation if clinical manifestations of hypercalcemia are present (fatigue, weakness, abdominal pain, constipation, nephrolithiasis, bone pain) or if calcium levels are >11.4 mg/dL. Following discontinuation, check serum calcium levels weekly for one month for return to baseline. Changes are usually reversible if lithium is discontinued; however, sustained hypercalcemia and parathyroid gland enlargement has been reported (Lehmann 2013).
- Hypothyroidism: May cause hypothyroidism, generally within 6 to 18 months of initiating treatment. Women may be at an increased risk. If hypothyroidism develops and symptoms of bipolar disorder are well-controlled, consider continuing lithium and treating hypothyroidism (APA 2002).
- Pseudotumor cerebri: Pseudotumor cerebri (increased intracranial pressure and papilledema) has been reported with use; undetected cases may result in blind spot enlargement, visual field constriction, and blindness secondary to optic atrophy. Discontinue therapy, if clinically possible, if syndrome occurs.
- Renal effects: Chronic therapy results in diminished renal concentrating ability (nephrogenic diabetes insipidus); this is usually reversible when lithium is discontinued. Monitor for changes in renal function and avoid dehydration; re-evaluation of treatment may be necessary. Morphologic changes with glomerular and interstitial fibrosis and nephron atrophy have been reported in patients on chronic lithium therapy; morphologic changes have also been reported in patients with bipolar disorder never exposed to lithium. The relationship between morphologic changes and renal function, and the association with lithium therapy, have not been established. If polyuria develops during lithium therapy, consolidating to once-daily dosing may decrease urine output (APA 2002; Carter 2013).
- Serotonin syndrome: Lithium can precipitate a potentially life-threatening serotonin syndrome, particularly when used in combination with other serotonergic agents (eg, SSRIs, SNRIS, triptans, TCAs, fentanyl, tramadol, buspirone, St. John's wort, tryptophan) or agents that impair metabolism of serotonin (eg, MAOIs). Monitor patients closely for signs of serotonin syndrome, such as mental status changes (eg, agitation, hallucinations, delirium, coma), autonomic instability (eg, tachycardia, labile blood pressure, dizziness, diaphoresis, flushing, hyperthermia), neuromuscular changes (eg, tremor, rigidity, myoclonus, hyperreflexia, incoordination), GI symptoms (eg, nausea, vomiting, diarrhea), and/or seizures. Discontinue treatment (and any concomitant serotonergic agent) immediately if signs/symptoms arise and initiate supportive therapy.
Disease-related concerns:
- Cardiovascular disease: Generally avoid use in patients with significant cardiovascular disease due to an increased risk of lithium toxicity; if use is unavoidable, use with extreme caution and monitor serum lithium levels closely. Lithium may unmask Brugada syndrome; avoid use in patients with or suspected of having Brugada syndrome. Consult with a cardiologist if a patient is suspected of having Brugada syndrome or has risk factors for Brugada syndrome (eg, unexplained syncope, a family history of Brugada syndrome, a family history of sudden death before the age of 45 years), or if unexplained syncope or palpitations develop after starting therapy.
- Dehydration: Generally avoid use in patients with significant fluid loss or sodium depletion due to an increased risk of lithium toxicity. If use is unavoidable, use extreme caution and monitor serum lithium levels closely. Decreased tolerance to lithium has been reported with sweating or diarrhea and, if such occur, supplemental fluid and salt should be administered under careful medical supervision and lithium intake reduced or suspended until the condition is resolved. In addition, concomitant infection with elevated temperatures may also necessitate a temporary reduction or cessation of therapy.
- Depression/suicidal ideation: Use with caution in patients at risk of suicide (suicidal thoughts or behavior) by drug overdose; lithium has a narrow therapeutic index (APA 2002).
- Renal impairment: Generally avoid use in patients with significant renal disease due to an increased risk of lithium toxicity. If use is unavoidable, use extreme caution and monitor serum lithium levels closely.
- Thyroid disease: Use with caution in patients with thyroid disease; hypothyroidism may occur with treatment (APA 2002).
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Debilitated: Generally avoid use in severely debilitated patients due to an increased risk of lithium toxicity; if use is unavoidable, use extreme caution and monitor serum lithium levels closely.
- Elderly: Use with caution in elderly patients due to an increased risk of lithium toxicity.
Dosage form specific issues:
- Benzyl alcohol and derivatives: Some dosage forms may contain benzyl alcohol; large amounts of benzyl alcohol (≥99 mg/kg/day) have been associated with a potentially fatal toxicity ("gasping syndrome") in neonates; the "gasping syndrome" consists of metabolic acidosis, respiratory distress, gasping respirations, CNS dysfunction (including convulsions, intracranial hemorrhage), hypotension, and cardiovascular collapse (AAP ["Inactive" 1997]; CDC 1982); some data suggest that benzoate displaces bilirubin from protein binding sites (Ahlfors 2001); avoid or use dosage forms containing benzyl alcohol with caution in neonates. See manufacturer's labeling.
- Propylene glycol: Some dosage forms may contain propylene glycol; large amounts are potentially toxic and have been associated with hyperosmolality, lactic acidosis, seizures and respiratory depression; use caution (AAP 1997; Zar 2007). See manufacturer's labeling.
Other warnings/precautions:
- Acute manic phase: Higher serum concentrations may be required and tolerated during an acute manic phase; however, the tolerance decreases when symptoms subside.
- Lithium toxicity: [US Boxed Warning]: Lithium toxicity is closely related to serum concentrations and can occur at doses close to therapeutic levels. Facilities for prompt and accurate serum lithium determinations should be available before initiating therapy. Normal fluid and salt intake must be maintained during therapy. Lithium should generally not be given to patients with significant renal or cardiovascular disease, severe debilitation or dehydration, or sodium depletion due to risk of lithium toxicity, or concomitant medications affecting renal function (such as ACE inhibitors, ARBs, loop and thiazide diuretics, and NSAIDs); if use is unavoidable, lithium may be undertaken with extreme caution, including frequent serum lithium determinations and possibly hospitalization. Discontinue therapy if such clinical signs of lithium toxicity occur (eg, diarrhea, vomiting, tremor, mild ataxia, drowsiness, muscular weakness).
Monitoring Parameters
Renal function including BUN and SrCr (baseline, every 2 to 3 months during the first 6 months of treatment, then once a year in stable patients or as clinically indicated); pediatric patients may require more frequent checks); serum electrolytes (baseline, then periodically), serum calcium (baseline, 2 to 6 weeks after initiation, then every 6 to 12 months; repeat as clinically indicated) (Broome 2011); thyroid (baseline, 1 to 2 times with in the first 6 months of treatment, then once a year in stable patients or as clinically indicated); beta-hCG pregnancy test for all females not known to be sterile (baseline); ECG with rhythm strip (baseline for all patients over 40 years or if underlying cardiac risk factors, repeat as clinical indicated), CBC with differential (baseline, repeat as clinically indicated); serum lithium levels (twice weekly until both patient's clinical status and levels are stable, then repeat levels every 1 to 3 months or as clinically indicated); weight (baseline, then periodically) (APA 2002; Mehta 2017); polyuria.
Pregnancy
Pregnancy Considerations
Lithium crosses the placenta in concentrations similar to those in the maternal plasma (Newport 2005).
Cardiac malformations in the infant, including Ebstein anomaly, are associated with use of lithium during the first trimester of pregnancy. Other adverse events including polyhydramnios, fetal/neonatal cardiac arrhythmias, hypoglycemia, diabetes insipidus, changes in thyroid function, premature delivery, floppy infant syndrome, or neonatal lithium toxicity are associated with lithium exposure when used later in pregnancy (ACOG 2008). The incidence of adverse events may be associated with higher maternal doses (Newport 2005). Fetal echocardiography should be considered if first trimester exposure occurs (ACOG 2008).
Due to pregnancy-induced physiologic changes, women who are pregnant may require dose adjustments of lithium to achieve euthymia and avoid toxicity (ACOG 2008; Grandjean 2009; Yonkers 2011).
For planned pregnancies, use of lithium during the first trimester should be avoided if possible (Grandjean 2009). However, the absolute risk of Ebstein anomaly is small and treatment for bipolar disorder should not be withheld when clinically indicated (Larsen 2015). If lithium is needed during pregnancy, the minimum effective dose should be used, maternal serum concentrations should be monitored, and consideration should be given to start therapy after the period of organogenesis; lithium should be suspended 24 to 48 hours prior to delivery or at the onset of labor when delivery is spontaneous, then restarted when the patient is medically stable after delivery (ACOG 2008; Grandjean 2009; Newport 2005).
Patient Education
What is this drug used for?
- It is used to treat bipolar problems.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Dizziness
- Loss of strength and energy
- Nausea
- Lack of appetite
- Abdominal pain
- Increased saliva
- Passing gas
- Dry mouth
- Change in taste
- Joint pain
- Dry hair
- Thin hair
- Hair loss
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- High blood sugar like confusion, fatigue, increased thirst, increased hunger, passing a lot of urine, flushing, fast breathing, or breath that smells like fruit
- Acidosis like confusion, fast breathing, fast heartbeat, abnormal heartbeat, severe abdominal pain, nausea, vomiting, fatigue, shortness of breath, or loss of strength and energy
- Thyroid problems like change in weight without trying, anxiety, agitation, feeling very weak, hair thinning, depression, neck swelling, difficulty focusing, inability handling heat or cold, menstrual changes, tremors, or sweating
- Fluid and electrolyte problems like mood changes, confusion, muscle pain or weakness, abnormal heartbeat, severe dizziness, passing out, fast heartbeat, increased thirst, seizures, loss of strength and energy, lack of appetite, not able to pass urine or change in amount of urine passed, dry mouth, dry eyes, or nausea or vomiting
- Kidney problems like not able to pass urine, blood in the urine, change in amount of urine passed, or weight gain
- Serotonin syndrome like dizziness, severe headache, agitation, sensing things that seem real but are not, fast heartbeat, abnormal heartbeat, flushing, tremors, sweating a lot, change in balance, severe nausea, or severe diarrhea
- Bloating
- Mood changes
- Abnormal movements
- Sexual dysfunction
- Fatigue
- Excitability
- Diarrhea
- Noise or ringing in the ears
- Shortness of breath
- Swelling of arms or legs
- Leaking of stool
- Leaking of urine
- Muscle weakness
- Twitching
- Involuntary eye movements
- Change in balance
- Trouble swallowing
- Trouble speaking
- Sensing things that seem real but are not
- Trouble with memory
- Severe headache
- Blurred vision
- Double vision
- Blindness
- Restlessness
- Abnormal gait
- Weight gain or loss
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.