What is Lotronex?
Lotronex is a prescription medicine used only for some women with severe chronic irritable bowel syndrome (IBS) whose:
- main problem is diarrhea and
- IBS symptoms have not been helped enough by other treatments.
Lotronex does not cure IBS, and it may not help every person who takes it. For those who are helped, Lotronex reduces lower stomach area (abdominal) pain and discomfort, the sudden need to have a bowel movement (bowel urgency), and diarrhea from IBS. If you stop taking Lotronex, your IBS symptoms may return within 1 or 2 weeks to what they were before you started taking Lotronex.
It is not known if Lotronex is safe and effective in men with IBS.
It is not known if Lotronex is safe and effective in children.
What is the most important information I should know about Lotronex?
Lotronex is a medicine only for some women with severe chronic irritable bowel syndrome (IBS) whose:
- main problem is darrhea and
- IBS symptoms have not been helped enough by other treatments.
Some people have developed serious bowel side effects while taking Lotronex. Serious bowel (intestine) side effects can happen suddenly, including the following:
Serious complications of constipation:
These complications may lead to a hospital stay and, in rare cases, blood transfusions, surgery, and death. People who are older, who are weak from illness, or who take other constipating medicines may be more likely to have serious complications of constipation with Lotronex.
To lower your chances of getting serious complications of constipation, do the following:
- If you are constipated, do not start taking Lotronex.
- If you get constipated while taking Lotronex, stop taking it right away and call your doctor.
- If your constipation does not get better after stopping Lotronex, call your doctor again.
- If you stopped taking Lotronex, do not start taking Lotronex again unless your doctor tells you to do so.
- Inflammation and injury of the intestines caused by reduced blood flow (ischemic colitis): Ischemic colitis is caused by reduced blood flow to parts of the large bowel. The chance of getting ischemic colitis when you take Lotronex for more than 6 months is not known. Ischemic colitis may lead to a hospital stay and, in rare cases, blood transfusions, surgery, and death.
Stop taking Lotronex and call your doctor or get medical help if you have symptoms of ischemic colitis such as new or worsening stomach-area (abdominal) pain, bloody diarrhea or blood in the stool.
Who should not take Lotronex?
Do not take Lotronex if you:
- have constipation or you are constipated most of the time.
- have had a serious problem from constipation. If you are constipated now, do not start taking Lotronex.
- have had serious bowel blockages.
- have had blood flow problems to your bowels, such as ischemic colitis.
- have had blood clots.
- have had Crohn's disease, ulcerative colitis, diverticulitis, or severe liver disease.
- are taking fluvoxamine (Luvox).
What should I tell my healthcare provider before taking Lotronex?
Talk with your doctor:
- about the possible benefits and risks of Lotronex.
- about how much of a problem IBS is in your life and what treatments you have tried.
- about any other illnesses you have and medicines you take or plan to take. These include prescription and non-prescription medicines, supplements, and herbal remedies. Certain illnesses and medicines can increase your chance of getting serious side effects while taking Lotronex. Other medicines may interact with how the body handles Lotronex.
- any allergies that you have. See the end of the Medication Guide for a complete list of ingredients in Lotronex.
- if you have liver problems.
- if you are pregnant or planning to become pregnant. It is not known if Lotronex can harm your unborn baby.
- if you are breastfeeding or plan to breastfeed. It is not known if Lotronex can harm your baby. Talk to your doctor about the best way to feed your baby if you take Lotronex.
How should I take Lotronex?
- Take Lotronex exactly as your doctor prescribes it. You can take Lotronex with or without food.
- Begin with 0.5 mg two times a day for 4 weeks to see how Lotronex affects you. You and your doctor may decide that you should keep taking this dose if you are doing well.
- Check with your doctor 4 weeks after starting Lotronex:
- If you try 0.5 mg two times a day for 4 weeks, it may not control your symptoms. If you do not get constipation or other side effects from Lotronex, your doctor may increase your dose up to 1 mg two times a day.
- If 1 mg two times a day does not work after 4 weeks, Lotronex is not likely to help you. You should stop taking it and call your doctor.
- Follow the instructions in the section “What is the most important information I should know about Lotronex?” about when you must stop taking the medicine and when you should call your doctor.
What are the possible side effects of Lotronex?
Lotronex may cause serious side effects, including:
See "What is the most important information I should know about Lotronex?"
The most common side effects of Lotronex include:
- constipation
- stomach (abdominal) discomfort and pain
- nausea
- intestinal discomfort and pain
These are not all the possible side effects of Lotronex.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
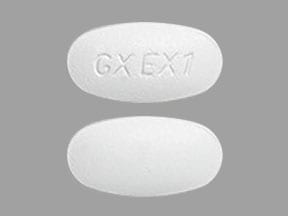
Lotronex Images
General information about the safe and effective use of Lotronex
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use Lotronex for a condition for which it was not prescribed. Do not give Lotronex to other people, even if they have the same symptoms that you have. It may harm them. You can ask your pharmacist or healthcare provider for information about Lotronex that is written for healthcare professionals.
How should I store Lotronex?
- Store Lotronex at room temperature between 68°F to 77°F (20°C to 25°C).
- Protect Lotronex from light and moisture.
Keep Lotronex and all medicines out of the reach of children.
What are the ingredients in Lotronex?
Active Ingredient: alosetron hydrochloride
Inactive Ingredients: lactose (anhydrous), magnesium stearate, microcrystalline cellulose, and pregelatinized starch. The white film-coat for the 0.5 mg tablet contains hypromellose, titanium dioxide, and triacetin. The blue film-coat for the 1 mg tablet contains hypromellose, titanium dioxide, triacetin, and indigo carmine.