Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet Chewable, Oral:
Emverm: 100 mg [contains corn starch, fd&c yellow #6 (sunset yellow), saccharin sodium]
Pharmacology
Mechanism of Action
Inhibits the formation of helminth microtubules; selectively and irreversibly blocks glucose uptake and other nutrients in susceptible adult intestine-dwelling helminths
Pharmacokinetics/Pharmacodynamics
Absorption
Oral: Poor; 5% to 10%; increased with food (Dayan 2003)
Distribution
Vd: 1 to 2 L/kg
Metabolism
Extensively hepatic
Excretion
Primarily feces (as unchanged drug and primary metabolite); urine (<2%)
Half-Life Elimination
3 to 6 hours
Protein Binding
90% to 95%
Use in Specific Populations
Special Populations: Hepatic Function Impairment
Plasma levels may be increased.
Use: Labeled Indications
Intestinal nematode infection: Treatment of patients ≥2 years of age with GI infections caused by Ancylostoma duodenale or Necator americanus (hookworms), Ascaris lumbricoides (roundworms), Enterobius vermicularis (pinworms), and Trichuris trichiura (whipworms).
Use: Off Label
Capillariasisc
Data from case reports suggest that mebendazole may be beneficial for the treatment of capillariasis Chunlertrith 1992. Clinical experience also suggests the utility of mebendazole in the treatment of capillariasis CDC 2012.
Echinococcosis, cystic (Echinococcus granulosus)c
Data from a case series suggest that mebendazole may be beneficial in the treatment of cystic echinococcosis Franchi 1999. Clinical experience also suggests the utility of mebendazole in the treatment of cystic echinococcosis CDC 2014.
Toxocariasisc
Data from a small, randomized trial and an observational study support the use of mebendazole in the treatment of toxocariasis Magnaval 1995, Wisniewska-Ligier 2012. Clinical experience also suggests the utility of mebendazole in the treatment of toxocariasis CDC 2013a.
Trichinellosis (Trichinella spiralis)c
Data from a limited number of patients studied suggest that mebendazole may be beneficial in the treatment of trichinellosis Horstmann 1982. Clinical experience also suggests the utility of mebendazole in the treatment of trichinellosis CDC 2018c.
Trichostrongyliasisb
Data from a randomized trial support the use of mebendazole in the treatment of trichostrongyliasis Farahmandian 1977.
Contraindications
Hypersensitivity to mebendazole or any component of the formulation
Dosage and Administration
Dosing: Adult
Ancylostoma duodenale or Necator americanus (hookworm): Oral: 100 mg twice daily for 3 days (manufacturer's labeling; CDC 2018b) or 500 mg as a single dose (CDC 2018b). Repeat in 3 weeks if not cured with initial treatment.
Ascariasis (roundworm): Oral: 100 mg twice daily for 3 days (manufacturer's labeling; CDC 2018a) or 500 mg as a single dose (CDC 2018a). Repeat in 3 weeks if not cured with initial treatment.
Capillariasis (off-label use): Oral: 200 mg twice daily for 20 days (CDC 2012).
Echinococcus, cystic (alternative agent) (off-label use): Oral: 40 to 50 mg/kg/day in 3 divided doses for 3 to 6 months (CDC 2014; Franchi 1999).
Enterobiasis (pinworm): Oral: 100 mg as a single dose (manufacturer's labeling); repeat in 2 weeks (CDC 2016a).
Toxocariasis (off-label use): Oral: 100 to 200 mg twice daily for 5 days (CDC 2013a).
Trichinellosis (Trichinella spiralis) (off-label use): Oral: 200 to 400 mg 3 times daily for 3 days, followed by 400 to 500 mg 3 times daily for 10 days (CDC 2018c).
Trichostrongyliasis (off-label use): Oral: 100 mg twice daily for 3 days (Farahmandian 1977).
Trichuriasis (whipworm): Oral: 100 mg twice daily for 3 days; repeat in 3 weeks if not cured with initial treatment.
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Ancylostoma duodenale or Necator americanus (hookworm): Children and Adolescents (Limited data in children <2 years): Oral: 100 mg twice daily for 3 days or 500 mg once as a single dose; repeat in 3 weeks if not cured with initial treatment (CDC 2018b; Red Book [AAP 2018])
Ascariasis (roundworm): Children and Adolescents (Limited data in children < 2 years): Oral: 100 mg twice daily for 3 days or 500 mg once as a single dose; repeat in 3 weeks if not cured with initial treatment (CDC 2018a; Red Book [AAP 2018])
Capillariasis: Limited data available: Children and Adolescents: Oral: 200 mg twice daily for 20 to 30 days (CDC 2012; Red Book [AAP 2018])
Enterobiasis (pinworm): Children and Adolescents (Limited data in children <2 years): Oral: 100 mg as a single dose, repeat in 2 weeks. (Red Book [AAP 2018]).
Toxocariasis (roundworm, ocular larva migrans, visceral larva migrans): Limited data available: Children and Adolescents: Oral: 100 to 200 mg twice daily for 5 days (CDC 2013a; Red Book [AAP 2018])
Trichinellosis (trichinosis; Trichinella species): Limited data available: Children and Adolescents: Oral: 200 to 400 mg 3 times daily for 3 days, then 400 to 500 mg 3 times daily for 10 days (CDC 2018c; Red Book [AAP 2018])
Trichuriasis (whipworm): Children and Adolescents (Limited data in children <2 years): Oral: 100 mg twice daily for 3 days; repeat in 3 weeks if not cured with initial treatment (CDC 2013b; Red Book [AAP 2018]).
Administration
Oral: Administer with or without food. Tablets may be chewed, swallowed whole, or crushed and mixed with food.
Storage
Store at 20°C to 25°C (68°F to 77°F).
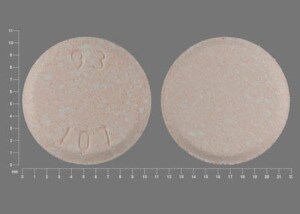
Mebendazole Images
Drug Interactions
CarBAMazepine: May decrease the serum concentration of Mebendazole. Monitor therapy
Cimetidine: May increase the serum concentration of Mebendazole. Monitor therapy
Fosphenytoin: May decrease the serum concentration of Mebendazole. Monitor therapy
MetroNIDAZOLE (Systemic): Mebendazole may enhance the adverse/toxic effect of MetroNIDAZOLE (Systemic). Particularly the risk for Stevens-Johnson syndrome or toxic epidermal necrolysis may be increased. Avoid combination
Phenytoin: May decrease the serum concentration of Mebendazole. Monitor therapy
Ritonavir: May decrease the serum concentration of Mebendazole. Monitor therapy
Adverse Reactions
Frequency not defined.
Gastrointestinal: Abdominal pain, anorexia, diarrhea, flatulence, nausea, vomiting
Hepatic: Hepatitis
<1%, postmarketing, and/or case reports: Abnormal hepatic function tests, agranulocytosis, alopecia, anaphylaxis, angioedema, decreased ejaculate volume (Parasitic Infections 2013), dizziness, glomerulonephritis, hepatitis, hypersensitivity reaction, leukopenia (Parasitic Infections 2013), neutropenia, seizure, skin rash, Stevens-Johnson syndrome, toxic epidermal necrolysis, urticaria
Warnings/Precautions
Concerns related to adverse effects:
- Bone marrow suppression: Neutropenia and agranulocytosis have been reported with high doses and prolonged use. Monitor CBC if used at higher doses or for a prolonged duration.
Disease-related concerns:
- Hepatic impairment: Use with caution; systemic exposure may be increased with hepatic impairment.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Pediatric: Experience with use in children <2 years of age is limited; convulsions have been reported postmarketing in pediatric patients <1 year.
Monitoring Parameters
Periodic hematologic, hepatic, and renal function; check for helminth ova in feces within 3-4 weeks following the initial therapy
Pregnancy
Pregnancy Considerations
Information following first trimester exposure to mebendazole is limited; however, an increased risk of birth defects has not been observed in the available studies (Gyorkos 2019). Most pregnancy outcome information is available from studies using mebendazole during the second or third trimester (Akpan 2018; Gyorkos 2019).
Untreated soil-transmitted helminth infections during pregnancy are associated with adverse maternal outcomes (eg, maternal iron deficiency anemia, low birth weight, neonatal and maternal death).
The World Health Organization (WHO) recommends preventive therapy with a benzimidazole, such as mebendazole, in pregnant women after the first trimester who live in areas where the baseline prevalence of soil-transmitted helminth infections is ≥20% (WHO 2017). The WHO also recommends treatment of soil-transmitted helminthiases (such as hookworm) in pregnant patients after the first trimester (WHO 1996).
WHO recommends preventive therapy with a benzimidazole, such as mebendazole, in females of reproductive potential who live in areas where the baseline prevalence of soil-transmitted helminth infections is ≥20% (WHO 2017).
Patient Education
What is this drug used for?
- It is used to treat infections caused by worms.
Frequently reported side effects of this drug
- Abdominal pain
- Lack of appetite
- Passing gas
- Nausea
- Vomiting
- Diarrhea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Seizures
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.