Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral:
Generic: 200 mg, 400 mg
Pharmacology
Mechanism of Action
Affects the thalamus and limbic system; also appears to inhibit multineuronal spinal reflexes
Pharmacokinetics/Pharmacodynamics
Metabolism
Hepatic
Excretion
Urine (8% to 20% as unchanged drug); feces (10% as metabolites)
Onset of Action
Sedation: ~1 hour
Half-Life Elimination
10 hours
Use: Labeled Indications
Anxiety: Management of anxiety disorders
Limitations of use: Meprobamate is not a preferred treatment option for anxiety disorders per the American Psychiatric Association, World Federation of Societies of Biological Psychiatry, and British Association for Psychopharmacology guidelines (APA [Stein 2009]; BAP [Baldwin 2014]; WFSBP [Bandelow 2012]).
Contraindications
Hypersensitivity to meprobamate, related compounds (including carisoprodol), or any component of the formulation; acute intermittent porphyria
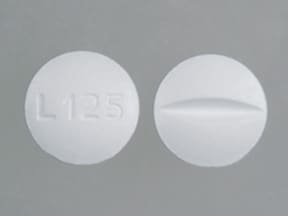
Meprobamate Images
Dosage and Administration
Dosing: Adult
Anxiety: Oral: 1,200 to 1,600 mg/day in 3 to 4 divided doses; maximum: 2,400 mg/day
Discontinuation: In patients with excessive dosage continued for weeks or months, meprobamate should be tapered off gradually over 1 to 2 weeks to avoid withdrawal symptoms such as anxiety, anorexia, or insomnia.
Dosing: Geriatric
Avoid use (Beers Criteria [AGS 2019]).
Dosing: Pediatric
Anxiety: Oral:
Children ≥6 years: 200 to 600 mg/day in 2 to 3 divided doses
Discontinuation: In patients with excessive dosage continued for weeks or months, meprobamate should be tapered off gradually over 1 to 2 weeks to avoid withdrawal symptoms such as anxiety, anorexia, or insomnia.
Adolescents: Refer to adult dosing.
Drug Interactions
Alcohol (Ethyl): CNS Depressants may enhance the CNS depressant effect of Alcohol (Ethyl). Monitor therapy
Alizapride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Azelastine (Nasal): CNS Depressants may enhance the CNS depressant effect of Azelastine (Nasal). Avoid combination
Blonanserin: CNS Depressants may enhance the CNS depressant effect of Blonanserin. Consider therapy modification
Brexanolone: CNS Depressants may enhance the CNS depressant effect of Brexanolone. Monitor therapy
Brimonidine (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromopride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromperidol: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Buprenorphine: CNS Depressants may enhance the CNS depressant effect of Buprenorphine. Management: Consider reduced doses of other CNS depressants, and avoiding such drugs in patients at high risk of buprenorphine overuse/self-injection. Initiate buprenorphine at lower doses in patients already receiving CNS depressants. Consider therapy modification
Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Cannabis: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Chlormethiazole: May enhance the CNS depressant effect of CNS Depressants. Management: Monitor closely for evidence of excessive CNS depression. The chlormethiazole labeling states that an appropriately reduced dose should be used if such a combination must be used. Consider therapy modification
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
CNS Depressants: May enhance the adverse/toxic effect of other CNS Depressants. Monitor therapy
Dimethindene (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Doxylamine: May enhance the CNS depressant effect of CNS Depressants. Management: The manufacturer of Diclegis (doxylamine/pyridoxine), intended for use in pregnancy, specifically states that use with other CNS depressants is not recommended. Monitor therapy
Dronabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Droperidol: May enhance the CNS depressant effect of CNS Depressants. Management: Consider dose reductions of droperidol or of other CNS agents (eg, opioids, barbiturates) with concomitant use. Exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Consider therapy modification
Esketamine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Flunitrazepam: CNS Depressants may enhance the CNS depressant effect of Flunitrazepam. Consider therapy modification
HYDROcodone: CNS Depressants may enhance the CNS depressant effect of HYDROcodone. Management: Avoid concomitant use of hydrocodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
HydrOXYzine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Kava Kava: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Lemborexant: May enhance the CNS depressant effect of CNS Depressants. Management: Dosage adjustments of lemborexant and of concomitant CNS depressants may be necessary when administered together because of potentially additive CNS depressant effects. Close monitoring for CNS depressant effects is necessary. Consider therapy modification
Lofexidine: May enhance the CNS depressant effect of CNS Depressants. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Magnesium Sulfate: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Methotrimeprazine: CNS Depressants may enhance the CNS depressant effect of Methotrimeprazine. Methotrimeprazine may enhance the CNS depressant effect of CNS Depressants. Management: Reduce adult dose of CNS depressant agents by 50% with initiation of concomitant methotrimeprazine therapy. Further CNS depressant dosage adjustments should be initiated only after clinically effective methotrimeprazine dose is established. Consider therapy modification
MetyroSINE: CNS Depressants may enhance the sedative effect of MetyroSINE. Monitor therapy
Minocycline (Systemic): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Nabilone: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Opioid Agonists: CNS Depressants may enhance the CNS depressant effect of Opioid Agonists. Management: Avoid concomitant use of opioid agonists and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Orphenadrine: CNS Depressants may enhance the CNS depressant effect of Orphenadrine. Avoid combination
Oxomemazine: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
OxyCODONE: CNS Depressants may enhance the CNS depressant effect of OxyCODONE. Management: Avoid concomitant use of oxycodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Paraldehyde: CNS Depressants may enhance the CNS depressant effect of Paraldehyde. Avoid combination
Perampanel: May enhance the CNS depressant effect of CNS Depressants. Management: Patients taking perampanel with any other drug that has CNS depressant activities should avoid complex and high-risk activities, particularly those such as driving that require alertness and coordination, until they have experience using the combination. Consider therapy modification
Piribedil: CNS Depressants may enhance the CNS depressant effect of Piribedil. Monitor therapy
Pramipexole: CNS Depressants may enhance the sedative effect of Pramipexole. Monitor therapy
ROPINIRole: CNS Depressants may enhance the sedative effect of ROPINIRole. Monitor therapy
Rotigotine: CNS Depressants may enhance the sedative effect of Rotigotine. Monitor therapy
Rufinamide: May enhance the adverse/toxic effect of CNS Depressants. Specifically, sleepiness and dizziness may be enhanced. Monitor therapy
Selective Serotonin Reuptake Inhibitors: CNS Depressants may enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk of psychomotor impairment may be enhanced. Monitor therapy
Sodium Oxybate: May enhance the CNS depressant effect of CNS Depressants. Management: Consider alternatives to combined use. When combined use is needed, consider minimizing doses of one or more drugs. Use of sodium oxybate with alcohol or sedative hypnotics is contraindicated. Consider therapy modification
Suvorexant: CNS Depressants may enhance the CNS depressant effect of Suvorexant. Management: Dose reduction of suvorexant and/or any other CNS depressant may be necessary. Use of suvorexant with alcohol is not recommended, and the use of suvorexant with any other drug to treat insomnia is not recommended. Consider therapy modification
Tapentadol: May enhance the CNS depressant effect of CNS Depressants. Management: Avoid concomitant use of tapentadol and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Tetrahydrocannabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Thalidomide: CNS Depressants may enhance the CNS depressant effect of Thalidomide. Avoid combination
Trimeprazine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Yohimbine: May diminish the therapeutic effect of Antianxiety Agents. Monitor therapy
Zolpidem: CNS Depressants may enhance the CNS depressant effect of Zolpidem. Management: Reduce the Intermezzo brand sublingual zolpidem adult dose to 1.75 mg for men who are also receiving other CNS depressants. No such dose change is recommended for women. Avoid use with other CNS depressants at bedtime; avoid use with alcohol. Consider therapy modification
Adverse Reactions
Frequency not defined.
Cardiovascular: Abnormal electroencephalogram, cardiac arrhythmia, peripheral edema, palpitations, severe hypotension, syncope, tachycardia
Central nervous system: Ataxia, chills, dizziness, drowsiness, euphoria, headache, overstimulation, paradoxical excitation, paresthesia, slurred speech, vertigo
Dermatologic: Dermatitis, erythema multiforme, skin rash, Stevens-Johnson syndrome
Endocrine & metabolic: Exacerbation of porphyria
Gastrointestinal: Diarrhea, nausea, proctitis, stomatitis, vomiting
Genitourinary: Anuria, oliguria
Hematologic & oncologic: Agranulocytosis, aplastic anemia, bruise, eosinophilia, immune thrombocytopenia, leukopenia, petechia, purpura
Hypersensitivity: Anaphylaxis, angioedema, hypersensitivity reaction
Neuromuscular & skeletal: Weakness
Ophthalmic: Accommodation disturbance
Respiratory: Bronchospasm
Miscellaneous: Fever
Warnings/Precautions
Concerns related to adverse effects:
- Allergic reactions: May occur in patients with history of dermatological condition (usually by fourth dose).
- CNS depression: May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks which require mental alertness (eg, operating machinery or driving). Effects may be potentiated when used with other sedative drugs or ethanol.
Disease-related concerns:
- Depression: Use with caution in patients with depression or suicidal tendencies.
- Drug abuse: Use with caution in patients with a history of drug abuse or acute alcoholism; potential for drug dependency exists. Tolerance, psychological and physical dependence may occur with prolonged use.
- Hepatic impairment: Use with caution in patients with hepatic impairment.
- Renal impairment: Use with caution in patients with renal impairment.
- Seizure disorder: Use with caution in patients with a history of seizure disorder.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Other warnings/precautions:
- Withdrawal: Abrupt discontinuation may precipitate withdrawal. In patients with excessive dosage continued for weeks or months, meprobamate should be tapered off gradually over 1 to 2 weeks to avoid withdrawal symptoms such as anxiety, anorexia, or insomnia.
Monitoring Parameters
Anxiety symptoms, mental status, abuse/overuse
Pregnancy
Pregnancy Considerations
Meprobamate crosses the placenta and is found in cord blood in concentrations similar to those in the maternal plasma. Maternal use may be associated with congenital malformations; avoid use during pregnancy.
Patient Education
- Discuss specific use of drug and side effects with patient as it relates to treatment. (HCAHPS: During this hospital stay, were you given any medicine that you had not taken before? Before giving you any new medicine, how often did hospital staff tell you what the medicine was for? How often did hospital staff describe possible side effects in a way you could understand?)
- Patient may experience headache, nausea, vomiting, diarrhea, fatigue, or anxiety. Have patient report immediately to prescriber signs of infection, enlarged lymph nodes, swelling of arms or legs, bruising, bleeding, unable to pass urine, change in amount of urine passed, difficulty breathing, severe loss of strength and energy, thoughts of suicide, seizures, dysarthria, fast heartbeat, arrhythmia, behavioral changes, burning or numbness feeling, change in balance, vision changes, severe dizziness, passing out, or signs of Stevens-Johnson syndrome/toxic epidermal necrolysis (red, swollen, blistered, or peeling skin [with or without fever]; red or irritated eyes; or sores in mouth, throat, nose, or eyes) (HCAHPS).
- Educate patient about signs of a significant reaction (eg, wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat). Note: This is not a comprehensive list of all side effects. Patient should consult prescriber for additional questions.
Intended Use and Disclaimer: Should not be printed and given to patients. This information is intended to serve as a concise initial reference for healthcare professionals to use when discussing medications with a patient. You must ultimately rely on your own discretion, experience and judgment in diagnosing, treating and advising patients.